Abstract
Results of studies published since 2002 reveal that T cells and antigen-presenting cells (APCs) produce complement proteins. The immune cell-derived, alternative pathway complement components activate spontaneously, yielding local, but not systemic, production of C3a and C5a. These anaphylatoxins to bind their respective G-protein coupled receptors, C3aR and C5aR, expressed on both partners. The resultant complement-induced T cell and APC activation drives T cell differentiation, expansion and survival. Complement deficiency or blockade attenuates T cell mediated autoimmunity and delays allograft rejection in mice. Increasing complement activation, achieved by genetic removal of the complement regulatory protein decay accelerating factor (DAF), enhances murine T cell immunity and accelerates allograft rejection. The findings support the need for design and testing of complement inhibitors in humans.
Keywords: T cells, allograft rejection, complement, costimulation, autoimmunity
Introduction
Complement activation is traditionally considered a component of the innate immune response required for host defense against invading pathogens and the clearance of immune complexes (1). The complement cascade also has an established role as a pathogenic effector pathway in autoimmunity and transplant rejection. Antibody-mediated activation of serum complement underlies some forms of vascular allograft injury (2, 3). C6 deficient animals, which cannot form the membrane attack complex, are resistant to antibody-mediated rejection (4). C4d deposition, an activation-product resulting from antibody-mediated complement activation, is used to diagnose human antibody-mediated vascular rejection (2, 5). Blockade of complement activation using anti-C5 mAb limits antibody-mediated kidney transplant injury in humans (6).
Several unexpected observations since 2002, including the finding that C3 deficient mouse kidneys are accepted by wild type allogeneic hosts with normal serum complement activity (7), have resulted in paradigm-shifting insights into how the complement cascade can influence tissue inflammation and adaptive immunity. Several research groups showed that complement produced and activated by parenchymal cells modulates ischemia reperfusion injury (8) and can contribute to the development of tissue fibrosis (9). This review will focus on findings that T cells and antigen presenting cells (APCs) produce complement components and upregulate expression of complement receptors during cognate interactions. The local expression and activation of complement provides critical signals that promote T cell activation and maturation. We provide perspective for how these mechanisms apply to the pathogenesis of autoimmunity and transplant rejection, and how targeting these pathways could potentially benefit clinical outcomes.
Overview of the complement cascade
Complement activation is initiated through the classical, alternative or mannose binding lectin pathways which converge at the formation of C3 convertases, multimeric protein complexes with enzymatic activity (Fig 1a). Cleavage of C3 yields C3a and C3b, the latter of which triggers formation of the C5 convertase. Subsequent C5 cleavage initiates formation of the membrane attack complex (MAC, C5b-9). Soluble and surface bound split products, including C3a, C3b, iC3b, C3dg and C5a mediate inflammation by directly lysing target cells, serving as chemoattractants, functioning as opsonins, and activating innate immune cells such as macrophages and neutrophils (1).
Fig. 1. Schematic representation of complement activation pathways.


a. Three pathways lead to complement activation: classical, mannose-binding lectin (MBL), and alternative. Binding of immune complexes to C1q,r,s activates the classical pathway whereas binding of mannose associated serine protease (MASPs) to mannose motifs expressed on bacteria activate the MBL pathway. Subsequent cleavage and assembly of C2 and C4 proteins form the C3 convertase. The spontaneous hydrolysis of C3 on cell surfaces leads to an alternative pathway C3 convertase dependent on fB, fD, and properdin. C3 convertases cleave C3 into C3a and C3b. C3b permits the formation of C5 convertase. C3b has further roles in opsonization and immune complex clearance. C3a and C5a have inflammatory and chemotactic properties. C5b, in conjunction with C6-C9, allows formation of the membrane attack complex (MAC) and subsequent pathogen lysis. b. Decay accelerating factor (DAF, CD55), is a cell surface expressed complement regulator that accelerates the decay of all surface-assembled C3 convertases, thereby limiting amplification of the downstream cascade.
Complement activation is a tightly regulated cascade designed to prevent bystander damage to host cells (1). This regulation is accomplished through secretion and expression of multiple soluble and membrane-bound complement regulatory proteins. Decay accelerating factor (DAF or CD55) is a glycophosphatidylinositol-anchored, membrane bound, complement regulatory protein that accelerates the decay of cell-surface assembled C3 convertases. DAF limits downstream complement activation and restricts production of the aforementioned cleavage products (10). Notably, DAF only functions intrinsically, limiting complement activation on the cell surface upon which it is expressed, but not proximally located pathogens, which lack DAF expression (Fig 1b). Human CD46 (murine homologue Crry) has similar decay accelerating function but additionally exhibits cofactor activity: in conjunction with soluble Factor I, these membrane bound regulators inactivate C3b to iC3b, thereby preventing re-formation of the C3 convertase. Other examples of complement regulators include CD59 (protectin), a cell surface expressed regulator that inhibits formation of the MAC at the C9 step and factor H, a soluble complement regulatory protein that exhibits both decay accelerating and cofactor activity. Through these various checkpoints, complement regulators naturally restrict the deleterious effects of complement activation on self cells.
Complement as a modulator of adaptive immunity including T cell immunity
Interactions between complement and adaptive immunity were initially described in the 1970s when Pepys observed that complement depleted mice failed to mount potent antibody responses (11). Subsequent mechanistic studies have shown that C3dg, a cleavage product of C3b, binds to the B cell-expressed complement receptor 2 (CR2, CD21) and through this interaction, lowers the threshold for B cell activation (1, 12). The effect of complement on B cell immune responses raised the possibility that complement/C3dg might be used as an adjuvant to enhance the efficacy of vaccines aimed at inducing protective pathogen-specific antibodies.
Work from several groups since the mid-2000s, including ours in collaboration with the Medof laboratory, demonstrated a previously unanticipated role for complement as a regulator of T cell immunity. Our joint group observed that during cognate interactions between T cells and APCs (macrophages and DCs), both partners upregulate and secrete alternative pathway complement components C3, fB, and fD, as well as the common pathway protein C5. We also observed upregulated surface expression of C3a receptor (C3aR) and C5a receptor (C5aR) on both partners during cognate interactions (13, 14). These in vitro experiments were performed in serum free medium such that the only source of complement was the cells added to the cultures. Experiments later showed that these changes are in part a consequence of costimulatory molecule signaling via CD28/CD80/CD86 and CD154/CD40 (14).
Costimulation also resulted in a transient, downregulation of cell surface expressed DAF. These changes in complement gene and protein expression promoted local complement activation on the interacting immune cells, yielding C3a and C5a which stimulate the T cell and the APC in both an autocrine and paracrine manner via the C3aR and C5aR (13, 14). We showed that signaling via these G-protein coupled receptors in T cells activates phosphoinositide 3-kinase gamma (PI-3Kγ), and induces phosphorylation of the central intracellular signaling molecule AKT (14, 15) (Fig 2). AKT phosphorylation upregulates the anti-apoptotic protein Bcl2 and downregulates expression of the pro-apoptotic molecule Fas. We showed that together, C3a and C5a enhance T cell proliferation and diminish T cell apoptosis (Fig 2), explaining the complement-mediated expansion of the effector T cell repertoire following antigenic stimulation (15). The evidence also indicates that C3aR and C5aR signaling is required for T cell homeostasis, as T cells deficient in both receptors spontaneously undergo accelerated cell death in vitro and in vivo (14).
Fig. 2. Schematic representation of complement mediated effects on T cells and APCs.
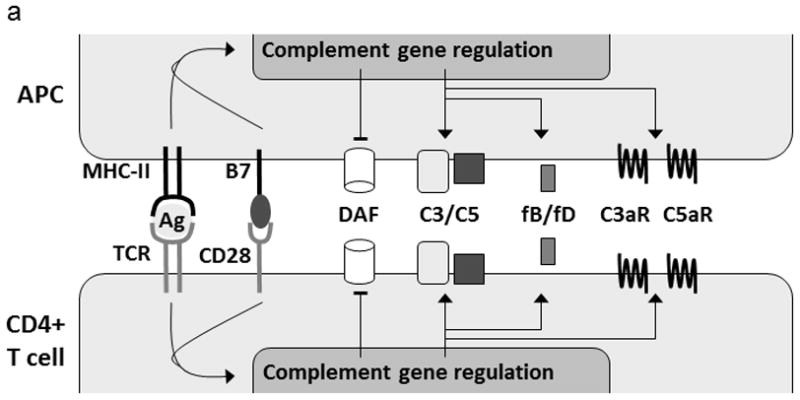
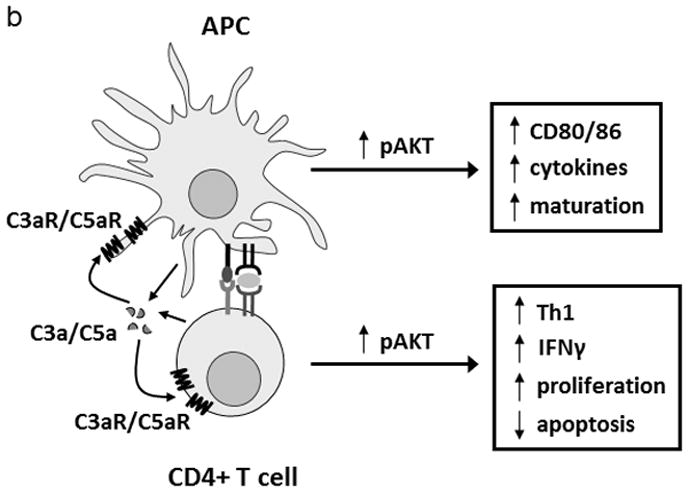
a. During a cognate interaction between APC and T cell, signaling through B7 costimulatory moleules and CD28 triggers local complement component production and release by both cells (~1000 fold more is produced by the APC) along with a transient downregulation of cell surface DAF and upregulation of C3aR/C5aR. These conditions favor the local, spontaneous, activation of complement by the alternative pathway. Consequently, local levels of C3a and C5a increase which stimulate both partners through their respective receptors. b. C3aR/C5aR signaling on both APC and T cells activates the AKT pathway by phosphorylation (among other pathways). AKT activation on the APC stimulates maturation, cytokine production, and B7 costimulatory molecule expression. AKT activation on the T cell directly promotes IFNγ secretion, reduces susceptibility to apoptosis, and promotes cell proliferation. In this manner, C3aR/C5aR stimulation directly and indirectly promotes T cell maturation with an expanded effector repertoire.
The immune cell-derived and locally produced C3a and C5a also bind to C3aR/C5aR on APCs, including dendritic cells and macrophages (14, 16–18) (Fig 2). We showed that C5aR/C3aR ligation activates the APCs via PI-3Kγ/AKT, and others demonstrated the downstream inhibition of cAMP/phosphokinase A, together activate NFκB. Our studies showed that the C3aR/C5aR signals induce upregulation and release of innate cytokines (e.g IL-12, IL-23) and upregulation of APC costimulatory molecules (e.g., CD80, CD86) further amplifying the immune response and modulating the phenotype toward IFNγ-producing Th1 immunity (14, 16). Importantly, in vitro findings supporting these conclusions derived from our group and others are that C5aR/C3aR−/− or C3−/− APCs produce less IL-12, express lower levels of CD80 and are weaker T cell stimulators than WT APCs. Conversely, DCs and macrophages obtained from mice genetically deficient in DAF (Daf1−/−, in which restraint on local complement activation is diminished) produce more IL-12 and induce stronger T cell responses than cells from WT animals (14, 16–18). Regardless of the phenotype of the APC, we showed that T cells deficient in C3aR and C5aR signaling (genetically deficient or blocked) respond poorly to WT and Daf1−/− APCs, and undergo accelerated cell death (14, 15).
To test whether local, immune cell derived complement or systemic, liver-derived complement regulates T cell immunity in vivo we used a bone marrow chimera strategy. T cells in chimeric mice with C3−/− BM-derived cells did not respond to alloantigenic stimuli despite having normal serum complement, while C3 deficient chimeras with WT (C3+) BM exhibited normal T cell alloreactivity (15, 19). Analogously, BM chimeras produced using C5aR deficient donors or recipients confirmed that T cell immunity is dependent on C5aR expression on BM-derived cells (15, 19).
Complement and DAF regulate both pathogenic and protective T cell immunity
The effects of immune cell-derived complement are relevant to multiple disease models. Work by others showed that C3−/− mice exhibit enhanced susceptibility to viral infection (20), Conversely, Daf1−/− mice are better protected and produce stronger T cell responses to lymphocytic choriomeningitis virus infection than WT controls (21). Animals deficient in both C3aR and C5aR are highly susceptible to herpes keratitis and to toxoplasma gondii infection, in the latter case, producing little IL-12 and weak T cell immunity required for protection from this pathogen (14).
Complement regulates T cell-dependent autoimmunity as well. Experimental allergic encephalomyelitis (EAE) is one model of T cell mediated autoimmunity that mimics aspects of human multiple sclerosis. In response to immunization with myelin oligodendrocyte glycoprotein, Daf1−/− mice develop more severe paralysis than wild type animals, which is associated with stronger autoreactive T cell immunity, enhanced IL-17 production, and diffuse T cell epitope spreading (14, 22, 23). These effects are C5aR- and C3aR-dependent as mice deficient in either or both of these G-protein coupled receptors develop weaker T cell responses and are resistant to EAE, regardless of DAF expression (14, 22). Additional recent studies published by others indicate that complement activation drives autoreactive pathogenic T cells in a model of autoimmune focal and segmental glomerulosclerosis (FSGS) in Daf1−/− mice (24), and that serum-derived C5a interacting with immune cell-expressed C5aR is an essential mediator in an IL-17-dependent model of autoimmune arthritis (25).
In 2010 our research group reported that immune cell-derived C3 is required for the induction of T cell dependent, autoimmune diabetes in mice (26). After documenting that multiple low dose, streptozotocin-induced diabetes is a T cell dependent, autoimmune disease, we showed that coincident with the induced elevations in blood glucose levels, alternative pathway complement component gene expression was upregulated within the islets of the diabetic WT animals. When we repeated the experiments with C3 deficient mice we observed complete resistance to disease, as assessed by the absence of histological insulitis and the absence of T cell reactivity to islet antigens. Studies of WT chimeras bearing C3 deficient bone marrow cells confirmed that bone marrow cell-derived C3 and not serum C3 is involved in the induction of diabetes in this model (26).
Complement and T cell immunity following transplantation
Complement dependent effects on alloreactive T cell immunity regulate the phenotypic expression of immune-mediated transplant injury in animal models. In addition to the aforementioned observation that wild type mice do not reject allogeneic C3 deficient kidneys (7), we showed that wild type mice reject Daf1−/− heart allografts (enhances local complement activation) with accelerated kinetics compared to wild type grafts (19). The accelerated rejection of Daf1−/− heart transplants is associated with augmented anti-donor T cell reactivity and is notable in animals devoid of B cells, confirming that local complement activation accelerates graft rejection through a T cell-dependent mechanism. Moreover, the effect is complement dependent because heart grafts deficient in DAF and C3 exhibit prolonged survival and stimulate weak T cell responses (19). Using bone marrow chimeras we then determined that immune cell-derived and/or donor graft-derived complement, but not serum complement, regulate expansion of naïve and primed effector, alloreactive, CD4+ and CD8+ T cells following transplantation. In other work, our joint group showed that donor or recipient DAF deficiency accelerates skin graft rejection (13) and overcomes the immune privilege of the eye (27), enhancing pathogenic T cell alloimmunity induced by normally tolerogenic corneal transplants, and results in rapid rejection. We also presented results at the 2011 American Transplant Congress (Phila., PA) showing that immune cell derived complement plays a critical role in driving graft versus host disease in mice.
Current concepts regarding how CD4 cells help alloreactive CD8 cells required for allograft rejection CD4 deficient mice do not reject cardiac allografts (28)] are that during cognate TCR/APC interactions, CD154 expressed on CD4+ T cells transmits activating signals to APCs through ligation with CD40 (29, 30). This in turn upregulates costimulatory molecule (CD80/86) and MHC expression on the APC, and induces proinflammatory cytokines (e.g. IL-12) which together facilitate optimal CD8+ T cell activation, expansion, differentiation and survival. Based on our above described findings that downstream effects of costimulatory signals are in part complement-dependent we tested the hypothesis that one molecular mechanism through which CD4+ T cells provide help in the induction of alloreactive CD8 T cells engaging a transplant is through stimulating local complement production/activation on the APC. We hypothesized that the resultant C3a/C5a would then activate the CD8 cell through C5aR/C3aR signaling. We indeed found that in vitro, CD4 help to CD8 cells (as measured by CD8 cell proliferation/cytokine production) required complement production by DCs and CD8 cell expression of C3aR and C5aR (31). In vivo, recipient DAF deficiency (and specifically DAF deficiency on BM-derived cells) bypassed the need for CD4 cell help, facilitated activation of alloreactive CD8 T cells and induced cardiac allograft rejection in CD4-depleted or CD4−/− recipients (31)(Fig 3). The effects required complement production by immune cells because CD4 depleted mice deficient in both DAF and factor D did not reject allografts. Our work also showed that DAF deficiency bypassed the requirement for CD40 costimulation to induce CD8 T cell dependent allograft rejection (31). Together these findings support the conclusion that immune cell-derived complement is a molecular intermediary underlying CD4 help to alloreactive CD8 T cells.
Fig. 3. Recipient Daf1 deficiency results in cardiac allograft rejection despite CD4 depletion.

Survival of BALB/c hearts transplanted into B6 WT (n=12), Daf1−/− (n=5), CD4 depleted WT (n=5), CD4 depleted Daf1−/− (n=6). * p< 0.05 versus CD4-depleted Daf1−/−, ** p< 0.05 versus WT controls. Reprinted from Vierya et al (31).
In other work we demonstrated that local complement production influences effector CD8 T cell responses to allogeneic vascular endothelial cells (EC). Following stimulation with IFNγ, TNFα, and IL-1, murine EC produce alternative pathway complement components which activate locally yielding C5a (32). Experiments performed using in vitro culture systems and in vivo heart transplantation models showed that this EC-produced and locally activated complement regulates T cell expansion and function. Consistent with the aforementioned in vitro studies, the effects of EC-derived complement are in part transmitted through C5aR signaling on T cells, as C5aR deficiency or blockade abrogates responsiveness (32).
Studies published by others showed that C5a/C5aR interactions are pathogenic mediators of T cell dependent kidney transplant rejection in rodents. C5aR blockade prolonged kidney transplant survival in rodents, a result associated with an abrogation of intragraft mononuclear cell infiltration and a diminution in T cell alloreactivity (33). We showed in 2011 that a blocking anti-C5 mAb synergizes with CTLA4-Ig to prevent T cell priming, limit T cell trafficking to an allograft and prolong heart transplant survival in mice (34). Together with observations by others that C5aR blockade prolongs rodent kidney allograft survival (33) these findings support the conclusion that complement is a physiologically important regulator of alloreactive T cell immunity.
Therapeutic approaches/data in humans
Selected reports suggest that immune cell-derived and/or graft-derived complement contributes to human transplant rejection. The quantity of RNA message for alternative pathway complement components and complement receptors, including C5aR and C3aR, is higher in human transplant tissue with histologic evidence of rejection compared to non-injured control tissue (33, 35). Gene expression profiling of human kidney transplants reveals higher expression of several complement genes in deceased donor grafts with longer ischemic times, and interestingly, the complement gene upregulation correlates inversely with early and late renal function (36). In vitro studies performed by others showed that analogous to the murine findings, human DCs produce complement and C5aR and C3aR signaling seems to be important in DC activation and function (37).
In another report, donor kidney expression of a specific polymorphic variant of C3 is associated with worse posttransplant outcomes (38). The precise mechanism through which this mutation alters allograft injury in human transplant recipients remains unclear and an independent study of a disparate and larger patient population could not verify these initial findings (39).
Conclusion
While the complement system was originally defined as a serum component that “complemented” antibodies in the killing of bacteria, it is now appreciated that complement has a multitude of other functions. Emerging data indicate that immune cell derived complement activation physiologically regulates immune cell survival and proliferation, modulating the strength and phenotype of adaptive T cell immune responses induced by infection, autoimmunity and alloimmune transplant rejection. Among the unanswered questions are how to best exploit these complement-dependent mechanisms to treat and or prevent disease in humans, and whether and how complement signaling affects other aspects of cellular immune responses, including memory and regulatory T cells.
Acknowledgments
This work was supported by NIH grants AI43578 and AI071185 to PSH. WK is a recipient of a fellowship grant from the American Society of Transplantation.
References
- 1.Ricklin D, Hajishengallis G, Yang K, Lambris JD. Complement: a key system for immune surveillance and homeostasis. Nat Immunol. 2010;11:785–97. doi: 10.1038/ni.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baldwin WM, Ota H, Rodriguez ER. Complement in transplant rejection: diagnostic and mechanistic considerations. Springer Semin Immunopathol. 2003;25:181–97. doi: 10.1007/s00281-003-0133-3. [DOI] [PubMed] [Google Scholar]
- 3.Wehner J, Morrell CN, Reynolds T, Rodriguez ER, Baldwin WM., 3rd Antibody and complement in transplant vasculopathy. Circ Res. 2007;100:191–203. doi: 10.1161/01.RES.0000255032.33661.88. [DOI] [PubMed] [Google Scholar]
- 4.Qian Z, Wasowska BA, Behrens E, Cangello DL, Brody JR, Kadkol SS, et al. C6 produced by macrophages contributes to cardiac allograft rejection. Am J Pathol. 1999;155:1293–302. doi: 10.1016/S0002-9440(10)65231-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins AB, Schneeberger EE, Pascual MA, Saidman SL, Williams WW, Tolkoff-Rubin N, et al. Complement activation in acute humoral renal allograft rejection: diagnostic significance of C4d deposits in peritubular capillaries. J Am Soc Nephrol. 1999;10:2208–14. doi: 10.1681/ASN.V10102208. [DOI] [PubMed] [Google Scholar]
- 6.Stegall M, Tayyab D, Lynn C, Justin B, Patrick D, JMG Terminal Complement Inhibition Decreases Early Acute Humoral Rejection in Sensitized Renal Transplant Recipients. Am J Transplant. 2010;10(s4):39. [Google Scholar]
- 7.Pratt JR, Basheer SA, Sacks SH. Local synthesis of complement component C3 regulates acute renal transplant rejection. Nat Med. 2002;8:582–7. doi: 10.1038/nm0602-582. [DOI] [PubMed] [Google Scholar]
- 8.Sheerin NS, Risley P, Abe K, Tang Z, Wong W, Lin T, et al. Synthesis of complement protein C3 in the kidney is an important mediator of local tissue injury. FASEB J. 2008;22:1065–72. doi: 10.1096/fj.07-8719com. [DOI] [PubMed] [Google Scholar]
- 9.Tang Z, Lu B, Hatch E, Sacks SH, Sheerin NS. C3a mediates epithelial-to-mesenchymal transition in proteinuric nephropathy. J Am Soc Nephrol. 2009;20:593–603. doi: 10.1681/ASN.2008040434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medof ME, Kinoshita T, Nussenzweig V. Inhibition of complement activation on the surface of cells after incorporation of decay-accelerating factor (DAF) into their membranes. J Exp Med. 1984;160:1558–78. doi: 10.1084/jem.160.5.1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pepys MB. Role of complement in the induction of immunological responses. Transplant Rev. 1976;32:93–120. doi: 10.1111/j.1600-065x.1976.tb00230.x. [DOI] [PubMed] [Google Scholar]
- 12.Dempsey PW, Allison ME, Akkaraju S, Goodnow CC, Fearon DT. C3d of complement as a molecular adjuvant: bridging innate and acquired immunity. Science. 1996;271:348–50. doi: 10.1126/science.271.5247.348. [DOI] [PubMed] [Google Scholar]
- 13.Heeger PS, Lalli PN, Lin F, Valujskikh A, Liu J, Muqim N, et al. Decay-accelerating factor modulates induction of T cell immunity. J Exp Med. 2005;201:1523–30. doi: 10.1084/jem.20041967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strainic MG, Liu J, Huang D, An F, Lalli PN, Muqim N, et al. Locally produced complement fragments C5a and C3a provide both costimulatory and survival signals to naive CD4+ T cells. Immunity. 2008;28:425–35. doi: 10.1016/j.immuni.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lalli PN, Strainic MG, Yang M, Lin F, Medof ME, Heeger PS. Locally produced C5a binds to T cell-expressed C5aR to enhance effector T-cell expansion by limiting antigen-induced apoptosis. Blood. 2008;112:1759–66. doi: 10.1182/blood-2008-04-151068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lalli PN, Strainic MG, Lin F, Medof ME, Heeger PS. Decay accelerating factor can control T cell differentiation into IFN-gamma-producing effector cells via regulating local C5a-induced IL-12 production. J Immunol. 2007;179:5793–802. doi: 10.4049/jimmunol.179.9.5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li K, Anderson KJ, Peng Q, Noble A, Lu B, Kelly AP, et al. Cyclic AMP plays a critical role in C3a-receptor-mediated regulation of dendritic cells in antigen uptake and T-cell stimulation. Blood. 2008;112:5084–94. doi: 10.1182/blood-2008-05-156646. [DOI] [PubMed] [Google Scholar]
- 18.Peng Q, Li K, Wang N, Li Q, Asgari E, Lu B, et al. Dendritic cell function in allostimulation is modulated by C5aR signaling. J Immunol. 2009;183:6058–68. doi: 10.4049/jimmunol.0804186. [DOI] [PubMed] [Google Scholar]
- 19.Pavlov V, Raedler H, Yuan S, Leisman S, Kwan WH, Lalli PN, et al. Donor deficiency of decay-accelerating factor accelerates murine T cell-mediated cardiac allograft rejection. J Immunol. 2008;181:4580–9. doi: 10.4049/jimmunol.181.7.4580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suresh M, Molina H, Salvato MS, Mastellos D, Lambris JD, Sandor M. Complement component 3 is required for optimal expansion of CD8 T cells during a systemic viral infection. J Immunol. 2003;170:788–94. doi: 10.4049/jimmunol.170.2.788. [DOI] [PubMed] [Google Scholar]
- 21.Fang C, Miwa T, Shen H, Song WC. Complement-dependent enhancement of CD8+ T cell immunity to lymphocytic choriomeningitis virus infection in decay-accelerating factor-deficient mice. J Immunol. 2007;179:3178–86. doi: 10.4049/jimmunol.179.5.3178. [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Lin F, Strainic MG, An F, Miller RH, Altuntas CZ, et al. IFN-gamma and IL-17 production in experimental autoimmune encephalomyelitis depends on local APC-T cell complement production. J Immunol. 2008;180:5882–9. doi: 10.4049/jimmunol.180.9.5882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu J, Miwa T, Hilliard B, Chen Y, Lambris JD, Wells AD, et al. The complement inhibitory protein DAF (CD55) suppresses T cell immunity in vivo. J Exp Med. 2005;201:567–77. doi: 10.1084/jem.20040863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bao L, Haas M, Pippin J, Wang Y, Miwa T, Chang A, et al. Focal and segmental glomerulosclerosis induced in mice lacking decay-accelerating factor in T cells. J Clin Invest. 2009;119:1264–74. doi: 10.1172/JCI36000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hashimoto M, Hirota K, Yoshitomi H, Maeda S, Teradaira S, Akizuki S, et al. Complement drives Th17 cell differentiation and triggers autoimmune arthritis. J Exp Med. 2010;207:1135–43. doi: 10.1084/jem.20092301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin M, Yin N, Murphy B, Medof ME, Segerer S, Heeger PS, et al. Immune Cell Derived C3 is Required for Autoimmune Diabetes Induced by Multiple Low Doses of Streptozotocin. Diabetes. 2010;59:2247–52. doi: 10.2337/db10-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Esposito A, Suedekum B, Liu J, An F, Lass J, Strainic MG, et al. Decay accelerating factor is essential for successful corneal engraftment. Am J Transplant. 2010;10:527–34. doi: 10.1111/j.1600-6143.2009.02961.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krieger NR, Yin DP, Fathman CG. CD4+ but not CD8+ cells are essential for allorejection. J Exp Med. 1996;184:2013–8. doi: 10.1084/jem.184.5.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ridge JP, Di Rosa F, Matzinger P. A conditioned dendritic cell can be a temporal bridge between a CD4+ T-helper and a T-killer cell. Nature. 1998;393:474–8. doi: 10.1038/30989. [DOI] [PubMed] [Google Scholar]
- 30.Schoenberger SP, Toes RE, van der Voort EI, Offringa R, Melief CJ. T-cell help for cytotoxic T lymphocytes is mediated by CD40-CD40L interactions. Nature. 1998;393:480–3. doi: 10.1038/31002. [DOI] [PubMed] [Google Scholar]
- 31.Vieyra M, Leisman S, Raedler H, Kwan WH, Yang M, Strainic MG, et al. Complement regulates CD4 T-cell help to CD8 T cells required for murine allograft rejection. Am J Pathol. 2011;179:766–74. doi: 10.1016/j.ajpath.2011.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raedler H, Yang M, Lalli PN, Medof ME, Heeger PS. Primed CD8(+) T-cell responses to allogeneic endothelial cells are controlled by local complement activation. Am J Transplant. 2009;9:1784–95. doi: 10.1111/j.1600-6143.2009.02723.x. [DOI] [PubMed] [Google Scholar]
- 33.Gueler F, Rong S, Gwinner W, Mengel M, Brocker V, Schon S, et al. Complement 5a receptor inhibition improves renal allograft survival. J Am Soc Nephrol. 2008;19:2302–12. doi: 10.1681/ASN.2007111267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raedler H, Vieyra MB, Leisman S, Lakhani P, Kwan W, Yang M, et al. Anti-complement component C5 mAb synergizes with CTLA4Ig to inhibit alloreactive T cells and prolong cardiac allograft survival in mice. Am J Transplant. 2011;11:1397–406. doi: 10.1111/j.1600-6143.2011.03561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keslar K, Rodriguez ER, Tan CD, Starling RC, Heeger PS. Complement gene expression in human cardiac allograft biopsies as a correlate of histologic grade of injury. Transplantation. 2008;86:1319–21. doi: 10.1097/TP.0b013e3181889831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naesens M, Li L, Ying L, Sansanwal P, Sigdel TK, Hsieh SC, et al. Expression of complement components differs between kidney allografts from living and deceased donors. J Am Soc Nephrol. 2009;20:1839–51. doi: 10.1681/ASN.2008111145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li K, Fazekasova H, Gomes C, Wang N, Sagoo P, Peng Q, et al. Expression of compement compoents, receptors and regulators by human dendritic cells and the role of C3a and C5a in modulation of dendritic cell function. Molecular Immunology. 2010;47:2232. doi: 10.1016/j.molimm.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brown KM, Kondeatis E, Vaughan RW, Kon SP, Farmer CK, Taylor JD, et al. Influence of donor C3 allotype on late renal-transplantation outcome. N Engl J Med. 2006;354:2014–23. doi: 10.1056/NEJMoa052825. [DOI] [PubMed] [Google Scholar]
- 39.Varagunam M, Yaqoob MM, Dohler B, Opelz G. C3 polymorphisms and allograft outcome in renal transplantation. N Engl J Med. 2009;360:874–80. doi: 10.1056/NEJMoa0801861. [DOI] [PubMed] [Google Scholar]


