Summary
Objective
This cross-sectional study examined the association of limb length inequality (LLI) with chronic joint symptoms at the hip and knee in a large, community-based sample, adjusting for the presence of radiographic osteoarthritis (OA) and other confounders.
Methods
The total study group comprised 3012 participants with complete knee symptoms data, 3007 participants with complete hip symptoms data, and 206 with LLI ≥ 2 cm. Presence of chronic knee symptoms was defined as report of pain, aching, or stiffness (symptoms) of the knee on most days. Presence of chronic hip symptoms was defined as hip pain, aching, or stiffness on most days or groin pain. Multiple logistic regression models were used to examine the relationship of LLI with knee and hip symptoms, while adjusting for demographic and clinical factors, radiographic knee or hip OA and history of knee or hip problems (joint injury, fracture, surgery, or congenital anomalies).
Results
Participants with LLI were more likely than those without LLI to have knee symptoms (56.8% vs 43.0%, P < 0.001), and hip symptoms (49.5% vs 40.0%, P = 0.09). In adjusted models, knee symptoms were significantly associated with presence of LLI (adjusted odds ratio [aOR] = 1.41, 95% confidence interval, [95% CI] 1.02 –1.97), but the relationship between hip symptoms and LLI (aOR = 1.20, 95% CI 0.87–1.67) was not statistically significant.
Conclusion
LLI was moderately associated with chronic knee symptoms and less strongly associated with hip symptoms. LLI may be a new modifiable risk factor for therapy of people with knee or hip symptoms.
Keywords: Leg length inequality, Joint pain, Osteoarthritis
Introduction
Chronic joint symptoms, including joint pain, aching, and stiffness, may contribute to impaired daily function and quality of life. The prevalence of chronic joint symptoms is high in the United States adult population (18 years and older). In 2005, an estimated 30.7% of the civilian non-institutionalized adult population, after adjusting for age, reported joint pain during the 30 days prior to interview1. Among adults with chronic joint symptoms, 43.3–57.9% have reported associated activity limitations2. While joint symptoms can often result from injuries or joint disorders, these symptoms can also be caused or exacerbated by injuries, chronic joint disorders, and mechanical factors, such as obesity, joint malalignment, and joint instability3-6. Limb length inequality (LLI), a condition in which paired lower extremities are of unequal length, is another mechanical factor that may also contribute to abnormal lower limb joint loading and symptoms7-10. LLI alters gait symmetry and joint mechanics during weight bearing, potentially contributing to atypical compressive and tensile stresses on the joint structures of the lower limb7,11,12. Increased pressure on a joint structure or pulling of soft tissues around a joint may then result in joint symptoms. Five reports suggest an association between LLI and knee or hip pain, but four of these studies examined only athletes and one was primarily based on observations in a clinical setting7–9,13,14.
In the Johnston County Osteoarthritis Project (JoCo OA), a community-based sample of African American and Caucasian men and women, we recently reported that LLI was associated with radiographic knee and hip osteoarthritis (OA), a chronic degenerative disorder of the joints that can result in pain, aching, and stiffness15. Because the presence of chronic joint symptoms is an outcome that can result from other conditions in addition to OA, we examined the association of LLI with chronic joint symptoms in this cohort, adjusting for the presence of radiographic OA. Additionally, we examined whether the associations of LLI with chronic symptoms were modified by other potential risk factors to help identify high risk subgroups (i.e., gender, race, and body mass index (BMI)) that may require particular attention. This information will expand our understanding of the clinical importance of LLI in the population and suggest potential areas for intervention.
Methods
Study Participants
JoCo OA is an ongoing, community-based study of knee and hip OA in African American and Caucasian residents in a rural county in North Carolina. Details of this study have been reported previously16,17. This study involved civilian, non-institutionalized adults aged 45 years and older who resided in six townships in Johnston County. Participants were recruited by probability sampling, with over-sampling of African Americans. A total of 3187 individuals were recruited between May 1991 and December 1997, and all participants completed a baseline clinical evaluation17. A total of 3012 participants with complete knee symptoms data and 3007 participants with complete hip or groin symptoms data were included in this cross-sectional analysis.
Limb Length Measurement
With the participant in the supine position, right and left lower extremity lengths were measured with a tape measure in centimeters (cm) between two defined bony landmarks: the anterior superior iliac spine (ASIS) and the distal medial malleolus. Inter-tester reliability of r = 0.98 and an intra-tester reliability from r = 0.89–0.95 have been reported for this measurement technique18. Friberg et al.19 reported that the mean difference in tape measured LLI was 8.6 mm (1.1 mm intra-tester mean error) compared with a gold standard of radiographs. LLI was defined conservatively as a 2.0 cm or greater difference in length between limbs to account for this potential measurement error.
Chronic Knee and Hip Symptoms
Participants completed an interviewer-administered questionnaire in which they answered “Yes” or “No,” separately for left and right knees and left and right hips, to the question: “On most days do you have pain, aching or stiffness in your [left/right] [knee/hip]?” The presence of groin pain was recorded for right and left sides. Participants were considered to have chronic knee symptoms if they answered affirmatively to the knee symptoms question and to have chronic hip symptoms if they answered affirmatively to the hip symptoms question or reported groin pain. Participants with knee or hip symptoms were categorized into mild, moderate, and severe symptoms based on their response to the question: “Is the pain, aching or stiffness in your [left/right] [knee/hip] mild, moderate, or severe?”
Radiographic Assessment of OA
All participants completed bilateral anteroposterior radiography of the knee with weight bearing. Women over 50 years of age and all men completed supine anteroposterior pelvic radiography. By protocol, 28 women under the age of 50 years did not complete pelvic radiographs to limit radiation exposure to their reproductive tissues, and thus, were excluded from hip analyses controlling for radiographic hip OA. Radiographs were rated by a single radiologist (JBR) using the Kellgren–Lawrence (K/L) radiographic atlas for overall knee and hip radiographic grades20. As previously described, inter-rater and intra-rater reliability for the radiologist were high (weighted kappa for inter-rater reliability 0.86; kappa for intra-rater reliability 0.89)17. Radiographs without the features of OA were defined as K/L grade of 0 (normal findings). A minute radiographic osteophyte of doubtful pathologic significance was assigned a K/L grade of 1 (questionable). Radiographs showing an osteophyte without joint space narrowing were assigned a K/L grade of 2 (mild). A moderate decrease of the joint space was assigned a K/L grade of 3 (moderate). K/L grade 4 (severe) was defined as severe joint space narrowing with subchondral bone sclerosis20. The presence of radiographic OA was defined as a K/L grade ≥2.
Demographic and Clinical Characteristics
The following participant characteristics were examined as covariates in our analyses because they may be associated with knee and hip symptoms: presence of radiographic OA in the joint of interest (K/L grade ≥2), as described above; gender; self-reported race (African American or Caucasian); age; history of knee joint problems (i.e., either knee injury [“Have you ever injured your right/left knee?”] or knee fracture [“Has a doctor ever told you that you had broken or fractured your right/left knee?”] or and knee surgery [“Have you ever had surgery on your right/left knee?”]); history of hip joint problems (i.e., either congenital hip problem [“Has a doctor ever told you that you had a problem with your right/left hip from birth or childhood?”] or hip injury [“Have you ever injured your right/left hip?”] or hip fracture [“Has a doctor ever told you that you had broken or fractured your right/left hip?”] or hip surgery [“Have you ever had surgery on your right/left hip?”]); and BMI(calculated as weight in kilograms/height in meters squared). Our questionnaire did not include items about fractures located in parts of the limb other than the knee or hip. History of joint injuries, fractures, and surgeries was combined into one category (history of joint problems) for both the knee and hip due to smaller numbers of observations. Height without shoes was measured in cm and weight was measured in kilograms (kg) using a balance beam scale.
Analysis
Chi-square and t-tests were used to compare all demographic and clinical characteristics (radiographic OA in the joint of interest, gender, race, age, BMI, and history of knee/hip joint problems) by LLI status. Among participants with LLI, we used Chi-square tests to compare the presence of chronic symptoms in the right longer vs left longer limb. Separate multiple logistic regression models were used to examine the relationship of knee and hip symptoms to LLI, while controlling for knee or hip OA in the joint of interest, age, gender, race, BMI, and history of knee or hip problems. Using a forward strategy, we included any statistically significant interaction terms of LLI with the other covariates. Multiple logistic regression models were used to estimate the prevalence odds ratio (POR) of LLI with the outcomes of chronic knee and hip symptoms, controlling for confounders. Additionally, separate models were used to estimate the POR of LLI for chronic symptoms in any knee, any hip, right knee, left knee, right hip, and left hip. In analyses examining left or right knee or hip symptoms, we examined one limb per person. At least one limb per person was examined in analyses with any knee or hip symptoms, without clustering by participant. Lastly, the relationship of LLI with severity of symptoms (i.e., mild, moderate–severe, none) in the any, right, or left knee or hip was explored. Statistical significance was evaluated at the P < 0.05 level. All statistical computations were performed using SAS Version 9.1 software (SAS Institute, Cary, NC).
Results
Among participants with complete knee or hip symptoms data, few data for other variables were missing (nearly 5%), and thus, we conducted a complete-case analysis. The analytic groups for knee (3012 participants with a response to knee symptom question) and hip (3007 participants with a response to hip and/or groin symptom questions) were similar in age (mean 62.6 years), sex (61.7% female), race (68.1% Caucasian), and BMI (29.0) (Table I). Among both samples, 206 (6.8%) participants had LLI ≥ 2 cm (Table I). Compared to those without LLI, participants with LLI in both the knee and hip analyses were significantly more likely to be older, have a higher mean BMI, report symptoms most days in the knee or hip, have radiographic knee or hip OA, and report a history of joint problems (Table I).
Table I. Selected characteristics of the knee and hip samples, overall and by LLI.
| Participants with response to knee symptom questions | Participants with response to hip/groin symptom questions | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Overall knee sample (N = 3012) | With LLI (N = 206) | Without LLI (N = 2806) | P-value | Overall hip sample (N = 3007) | With LLI (N = 206) | Without LLI (N=2801) | P-value | |
| Presence of joint symptoms (%) | 44.0 | 56.8 | 43.0 | <0.01 | 40.6 | 49.5 | 40.0 | 0.09 |
| Age (mean (SD)) years | 62.6 (±11.1) | 65.0 (±11.2) | 62.4 (±11.0) | <0.01 | 62.6 (±11.1) | 65.0 (±11.2) | 62.4 (±11.0) | <0.01 |
| Female (%) | 61.7 | 62.1 | 61.7 | 0.90 | 61.7 | 62.1 | 61.7 | 0.90 |
| Caucasian (%) | 68.1 | 64.6 | 68.3 | 0.26 | 68.0 | 64.6 | 68.3 | 0.27 |
| BMI (mean kg/m2 (SD)) | 29.0 (±6.0) | 30.0 (±7.3) | 28.9 (±5.9) | <0.01 | 29.0 (±6.0) | 30.0 (±7.3) | 28.9 (±5.9) | <0.01 |
| OA in joint (%) | 29.7 | 46.8 | 28.4 | <0.01 | 28.8 | 35.1 | 28.3 | 0.04 |
| History of joint problems (%) | 18.1 | 26.5 | 17.5 | <0.01 | 8.4 | 16.8 | 7.8 | <0.01 |
Among all participants, 37.1% reported chronic symptoms for the right knee, 32.3% for the left knee, 31.2% for the right hip, and 29.7% for the left hip. The left limb was the longer limb in 65.5% of the 206 participants. There were no statistically significant differences in the frequency of whether the right or the left limb was longer according to location of knee or hip symptoms (Fig. 1).
Fig. 1.
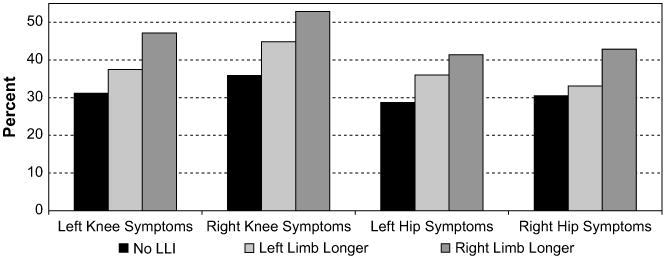
Proportion of sample with knee and hip symptoms, by laterality of joint site and LLI. No statistically significant differences in the frequency of left or right knee or hip symptoms based on whether the left or right limb is longer.
There were no statistically significant interaction terms between LLI and radiographic OA, age, BMI, gender, race, and history of problems in the knee or hip models. In adjusted knee models controlling for covariates, participants with LLI were 41% more likely than those without LLI to have knee symptoms (adjusted POR (aPOR) = 1.41, 95% confidence interval [CI] 1.02–1.97) (Table II). In adjusted hip models, participants with LLI were more likely than those without LLI to have hip symptoms (Table II), although these differences were not statistically significant. Adjusting for other covariates, moderate-to-severe symptoms of either knee or hip were more prevalent in participants with LLI than without LLI, but these differences were not statistically significant (Table II).
Table II. POR of symptoms among participants with and without LLI, by site and severity of symptoms, adjusting for age, BMI, gender, race, and radiographic OA and history of problems in joint of interest.
| LLI (N = 206) | No LLI (N = 2806) | Adjusted POR | 95% CI | |
|---|---|---|---|---|
| Any knee symptoms (%) | 56.8 | 43.0 | 1.41 | 1.02–1.97 |
| Mild (%) | 15.3 | 13.1 | 1.32 | 0.86–2.00 |
| Moderate–severe (%) | 41.4 | 29.9 | 1.29 | 0.90–1.84 |
| Left knee symptoms (%) | 40.8 | 31.2 | 1.25 | 0.90–1.74 |
| Mild (%) | 11.2 | 9.9 | 1.03 | 0.65–1.64 |
| Moderate–severe (%) | 29.6 | 21.3 | 1.13 | 0.80–1.61 |
| Right knee symptoms (%) | 47.8 | 35.9 | 1.28 | 0.93–1.76 |
| Mild (%) | 14.1 | 12.4 | 1.06 | 0.70–1.62 |
| Moderate–severe (%) | 33.7 | 23.5 | 1.25 | 0.90–1.74 |
| N = 206 | N = 2801 | |||
| Any hip symptoms (%) | 49.5 | 40.0 | 1.20 | 0.87–1.67 |
| Mild (%) | 13.3 | 11.0 | 1.16 | 0.72–1.85 |
| Moderate–severe (%) | 36.2 | 29.0 | 1.17 | 0.82–1.67 |
| Left hip symptoms (%) | 37.9 | 28.7 | 1.18 | 0.83–1.64 |
| Mild (%) | 8.3 | 7.4 | 1.11 | 0.58–2.11 |
| Moderate–severe (%) | 29.6 | 21.3 | 1.07 | 0.73–1.58 |
| Right hip symptoms (%) | 36.4 | 30.5 | 1.06 | 0.76–1.49 |
| Mild (%) | 7.8 | 7.9 | 0.91 | 0.48–1.74 |
| Moderate–severe (%) | 28.6 | 22.1 | 0.88 | 0.60–1.30 |
All models were adjusted for age, gender, race, BMI, radiographic OA at the joint of interest and history of problems in the joint of interest. The sum of the percents with mild, moderate, and severe symptoms may be less than total for that joint due to missing values.
Discussion
In this community-based study, participants with LLI were significantly more likely to have knee symptoms compared to participants without LLI, even when controlling for age, BMI, gender, race, radiographic knee OA, and history of knee joint problems. There was a similar but non-significant trend for hip symptoms. Additionally, comparable but nonsignificant trends were observed for left knee, right knee, left hip, and right hip symptoms. Moderate-to-severe symptoms were more common in participants with LLI than without LLI, though this was not statistically significant in either knee or hip joint. We cannot determine causality from this cross-sectional study. Potentially, individuals with LLI could functionally minimize the inequality by increasing knee flexion or hip adduction of the longer limb or hyperextending the knee of the shorter limb21. The altered movement pattern may amplify forces across lower extremity joints, and the increased forces may contribute to or exacerbate symptoms in the joint. Alternatively, patients with joint symptoms may modify their functional movements, resulting in shortening of tissues around the joints, contractures, or limitations in range of motion that could appear as a functional LLI.
Others studies have reported greater prevalence of knee and hip symptoms in individuals with LLI, but these studies did not adjust for radiographic OA or joint problems (i.e., injury, fracture, or surgery)11,13,14. Gofton14 noted the occurrence of cartilage degeneration and pain in the medial compartment of the knee of the longer leg. In the present study, we did not find a statistically significant relationship between which limb was longer and the presence of knee or hip symptoms. Brunet et al.13 reported that hip pain was twice as common in male and female runners with LLI compared to runners without LLI. McCaw11 also reported that hip pain was linked to LLI in their study of runners. Our results add to this literature by showing that the association between LLI and joint symptoms may be independent of radiographic OA. In addition, this study confirms the association of LLI with joint symptoms in a larger and more general population of individuals than prior studies. For some patients, correction of LLI may reduce joint symptoms and associated disability. Since there were no interactions between OA and LLI for right or left knee or hip joints in our analyses, our findings may be applicable to all groups (i.e., males and females, African Americans and Caucasians, and obese and normal weight).
Strengths of this study include that it is community-based, consists of African American and Caucasian men and women, includes information on radiographic knee and hip OA and the presence of knee and hip symptoms for each study participant, and has a larger sample size than other studies7–9,13,14.Our method for measuring LLI is a limitation. Tape measurement is highly accurate between testers when compared to supine radiography, but is less reliable compared to standing radiographs21,22. Sources of error with tape measurement include difficulty with accurately placing the tape measure on identical bilateral bony landmarks, lower extremity girth differences affecting LLI measurements, masking of LLIs observed in weight bearing by measuring in the supine position, and exclusion of the contributions of the foot and ankle to limb length22. We defined LLI categorically as discrepancies ≥2 cm to account for these potential sources of error. In a prior report, ASIS to medial malleolus measurements differed from standing radiographic measurements by a mean difference of 0.73 ± .01 cm23. The use of an LLI of ≥1.5 cm with the tape measurement technique has moderate inter-tester reliability (post-standardization prevalence-adjusted bias-adjusted kappa = 0.72)24. Accordingly, we believe our definition of LLI is conservative and clinically relevant since subjects with supine tape measurement differences between limbs ≥2 cm would likely demonstrate a LLI in standing. Misclassification of LLI is possible with our measurement technique, and with our conservative definition, those who truly had LLI may have been misclassified as having no LLI in our analyses. This misclassification would have resulted in an underreporting of true LLI, biasing estimates towards the null.
Results of this community-based study may have important clinical implications for patients seeking treatment for knee or hip symptoms. Our results suggest a notable association between knee and hip symptoms and LLI, even when controlling for the presence of OA and history of joint problems. Physical examinations of patients reporting knee or hip symptoms should include evaluation of LLI. Shoe inserts may be simple, non-invasive, and inexpensive treatment options for patients with knee or hip symptoms. Previous studies have shown that shoe lifts appear to reduce pain and disability in patients with LLI and chronic pain conditions, such as low back pain and hip pain7,14,25–27. Studies are needed to examine whether shoe lifts may be a helpful intervention for relief of pain and improvement in physical function in patients with LLI and knee symptoms.
Acknowledgments
Center for Disease Control and Prevention/Association of Schools of Public Health co-operative agreements S1734 and S3486 (JMJ, JBR), the NIAMS Multipurpose Arthritis and Musculoskeletal Disease Center grant 5-P60-AR30701 (JMJ), the NIAMS Multidisciplinary Clinical Research Center grant 5 P60 AR49465-03 (JMJ), and NIH National Research Service Award Institutional Research Training Grant (T32) – Arthritis and Immunology AR07416 (YMG).
Footnotes
Conflict of interest: The authors have no competing interests, financial or otherwise, to declare.
References
- 1.Health, United States, 2007, with chartbook on trends in the health of Americans. [accessed 14.12.07]; www.cdc.gov/nchs/data/hus/hus07.pdf. [PubMed]
- 2.Prevalence and impact of chronic joint symptoms – seven states, 1996. MMWR CDC Surveill Summ. 1998;47(17):345–51. [PubMed] [Google Scholar]
- 3.Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–6. doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 4.Sharma L. The role of proprioceptive deficits, ligamentous laxity, and malalignment in development and progression of knee osteoarthritis. J Rheumatol. 2004;31:87–92. [PubMed] [Google Scholar]
- 5.Sharma L, Lou C, Felson DT, Dunlopp DD, Kirwan-Mellis G, Hayes KW, et al. Laxity in healthy and osteoarthritis knees. Arthritis Rheum. 1999;42:861–70. doi: 10.1002/1529-0131(199905)42:5<861::AID-ANR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 6.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–95. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 7.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine Sep. 1983;8(6):643–51. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Kujala UM, Friberg O, Aalto T, Kvist M, Osterman K. Lower limb asymmetry and patellofemoral joint incongruence in the etiology of knee exertion injuries in athletes. Int J Sports Med Jun. 1987;8(3):214–20. doi: 10.1055/s-2008-1025658. [DOI] [PubMed] [Google Scholar]
- 9.Kujala UM, Osterman K, Kvist M, Aalto T, Friberg O. Factors predisposing to patellar chondropathy and patellar apicitis in athletes. Int Orthop. 1986;10(3):195–200. doi: 10.1007/BF00266208. [DOI] [PubMed] [Google Scholar]
- 10.Swezey RL. Pseudo-radiculopathy in subacute trochanteric bursitis of the subgluteus maximus bursa. Arch Phys Med Rehabil. 1976 Aug;57(8):387–90. [PubMed] [Google Scholar]
- 11.McCaw ST. Leg length inequality. Implications for running injury prevention. Sports Med. 1992 Dec;14(6):422–9. doi: 10.2165/00007256-199214060-00008. [DOI] [PubMed] [Google Scholar]
- 12.Morscher E. Etiology and pathophysiology of leg length discrepancies. Prog Orthop Surg. 1977;1:9–19. [Google Scholar]
- 13.Brunet ME, Cook SD, Brinker MR, Dickinson JA. A survey of running injuries in 1505 competitive and recreational runners. J Sports Med Phys Fitness. 1990 Sep;30(3):307–15. [PubMed] [Google Scholar]
- 14.Gofton JP. Persistent low back pain and leg length disparity. J Rheumatol. 1985 Aug;12(4):747–50. [PubMed] [Google Scholar]
- 15.Golightly YM, Allen KD, Renner JB, Helmick CG, Salazar A, Jordan JM. Relationship of limb length inequality with radiographic knee and hip osteoarthritis. Osteoarthritis Cartilage. 2007;15(7):824–9. doi: 10.1016/j.joca.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;35(3):543–4. [PubMed] [Google Scholar]
- 17.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8(4):242–50. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 18.Hoyle DA, Latour M, Bohannon RW. Intraexaminer, interexaminer, and interdevice comparability of leg length measurements obtained with measuring tape and metrecom. J Orthop Sports Phys Ther. 1991;14(6):263–8. doi: 10.2519/jospt.1991.14.6.263. [DOI] [PubMed] [Google Scholar]
- 19.Friberg O, Nurminen M, Korhonen K, Soininen E, Manttari T. Accuracy and precision of clinical estimation of leg length inequality and lumbar scoliosis: comparison of clinical and radiological measurements. Int Disabil Stud. 1988;10(2):49–53. doi: 10.3109/09638288809164098. [DOI] [PubMed] [Google Scholar]
- 20.Kellgren JH, Lawrence JS. Atlas of standard radiographs: the epidemiology of chronic rheumatism. Vol. 2. Oxford: Blackwell Scientific; 1963. [Google Scholar]
- 21.Brady RJ, Dean JB, Skinner TM, Gross MT. Limb length inequality: clinical implications for assessment and intervention. J Orthop Sports Phys Ther. 2003 May;33(5):221–34. doi: 10.2519/jospt.2003.33.5.221. [DOI] [PubMed] [Google Scholar]
- 22.Gogia PP, Braatz JH. Validity and reliability of leg length measurements. J Orthop Sports Phys Ther. 1986;8(10):185–8. doi: 10.2519/jospt.1986.8.4.185. [DOI] [PubMed] [Google Scholar]
- 23.Woerman AL, Binder-Macleod SA. Leg length discrepancy assessment: accuracy and precision in five clinical methods of evaluation. J Orthop Sports Phys Ther. 1984;5(5):230–9. doi: 10.2519/jospt.1984.5.5.230. [DOI] [PubMed] [Google Scholar]
- 24.Cibere J, Thorne A, Bellamy N, Greidanus N, Chalmers A, Mahomed N, et al. Reliability of the hip examination in osteoarthritis: effect of standardization. Arthritis Rheum. 2008;59(3):373–81. doi: 10.1002/art.23310. [DOI] [PubMed] [Google Scholar]
- 25.Defrin R, Benyamin S, Aldubi R, Pick C. Conservative correction of leg-length discrepancies of 10 mm or less for the relief of chronic low back pain. Arch Phys Med Rehabil. 2005;86(1):2075–80. doi: 10.1016/j.apmr.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Giles LG, Taylor JR. Low-back pain associated with leg length inequality. Spine. 1981 Sep-Oct;6(5):510–21. doi: 10.1097/00007632-198109000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Helliwell M. Leg length inequality and low back pain. Practitioner. 1985 May;229(1403):483–5. [PubMed] [Google Scholar]


