Abstract
Objectives:
To assess the prevalence, location and anatomical course of accessory canals of the jaws using cone beam CT.
Methods:
A retrospective analysis of 4200 successive cone beam CT scans, for patients of both genders and ages ranging from 7 to 88 years, was performed. They were exposed at the School of Dentistry, University of Michigan, Ann Arbor, MI. After applying the exclusion criteria (the presence of severe ridge resorption, pre-existing implants, a previously reported history of craniofacial malformations or syndromes, a previous history of trauma or surgery, inadequate image quality and subsequent scans from the same individuals), 4051 scans were ultimately included in this study.
Results:
Of the 4051 scans (2306 females and 1745 males) that qualified for inclusion in this study, accessory canals were identified in 1737 cases (42.9%; 1004 females and 733 males). 532 scans were in the maxilla (13.1%; 296 females and 236 males) and 1205 in the mandible (29.8%; 708 females and 497 males).
Conclusions:
A network of accessory canals bringing into communication the inner and outer cortical plates of the jaws was identified. In light of these findings, clinicians should carefully assess for the presence of accessory canals prior to any surgical intervention to decrease the risk for complications.
Keywords: accessory canals, incisive canal, lingual vascular canals, interforaminal, CBCT
Introduction
Cone beam CT (CBCT) permits finely detailed visualization of the osseous architecture with high contrast and without burn out. By offering tomographic slices down to 0.08 mm, a true volumetric presentation of the arch is obtained. In addition, fine osseous architecture can be visualized without data loss.1
Numerous unnamed accessory foramina have been described in the jaws, especially on the lingual aspect of the mandible,2 midline of the mandible, lateral to the lingual foramina and in the canine–premolar region. Additionally, the size and morphology of the incisive canal and the incisive foramen are extremely variable.3–6
A thorough understanding of the prevalence and distribution of these accessory canals is clinically important. Several reports have documented sensory disturbances caused by direct trauma to the mandibular incisive canal bundle in the interforaminal region as a result of surgical implant placement.4,5 Moreover, following transection or compression, intraosseous nerves may undergo Wallerian degeneration, resulting in post-operative pain or a persistent sensation of burning. This may even occur in the absence of paraesthesia of the lip or chin when the injury is anterior to the sensory division of these areas.7
Blood vessels can be inadvertently resected during implant placement or following other surgical procedures. When this occurs, the artery may prolapse into the floor of the mouth, permitting the sublingual space to fill with blood and raising the tongue until the airway is compromised. In this potentially life-threatening situation, an emergency tracheostomy may be required until blood flow can be controlled.8–10 In addition, at least one case of haematoma-induced sensory disturbance, developing as a result of indirect trauma to the mandibular incisive canal, affecting the incisive canal bundle with extension to the main mental branch, has been described.4 Other reports have detailed trauma and pathology associated with accessory canals of the nasopalatine canal region.11
It is hypothesized that these accessory canals, with their widely differing morphology, position and size, could also potentially be misinterpreted as fracture lines by a clinician unaware of their existence.
As the demand for the placement of osseointegrated dental implants and grafting procedures in the rehabilitation of edentulous areas of the jaws increases, the pre-operative evaluation of anatomical variations, with respect to both the distribution and morphology of these canals, will be of even greater importance.
The aim of this study was to investigate the prevalence, distribution and anatomy of accessory canals in the jaws.
Methods and materials
A retrospective analysis of 4200 successive CBCT scans, exposed at the School of Dentistry, University of Michigan, Ann Arbor, MI, was performed. Patients were both male and female, with ages ranging from 7 to 88 years. After applying the exclusion criteria (the presence of severe ridge resorption, pre-existing implants, a previously reported history of craniofacial malformations or syndromes, a previous history of trauma or surgery, inadequate image quality and subsequent scans from the same individuals), 4051 scans were included in this study.
Images were acquired using the i-CAT® Imaging system (Next Generation; Imaging Sciences International, Hatfield, PA). The patients were exposed in the sitting position and immobilized using a headband to adjust the head against the headrest and chin cup. The mid-sagittal plane was aligned perpendicular to the horizontal plane using vertical and horizontal alignment beams, as recommended by the manufacturer. A single 360° scan collected the projection data for reconstruction. As the scans were performed for various diagnostic purposes, the field of view, voxel size (0.2, 0.3 and 0.4 mm) and other scan parameters varied, depending on the reason for exposing the scan. i-CAT Vision software (Imaging Sciences International) was used for image manipulation and analysis.
Scans were examined for the presence, morphology and anatomical course of accessory canals in the maxilla and mandible. The scans were examined by one of the authors (ME), who has 17 years of experience as an oral radiologist. Any observed radiolucent line meeting the following criteria was considered to represent an accessory canal: not previously reported as a known anatomical landmark in the oral radiology literature, was not present in all patients scanned and was not related to any kind of pathology. Descriptive statistics of the resulting data was performed and the percentages of the observed canals were calculated manually.
This research was approved by the University of Michigan Institutional Review Board. Examiners were blinded to all potentially identifiable personal information other than patient age and gender.
Results
Of the 4051 scans that qualified for inclusion in this study, accessory canals were identified in 1737 scans (42.9%; 1004 females and 733 males). 532 of these accessory canals were in the maxilla (13.1%; 296 females and 236 males) and 1205 were in the mandible (29.8%; 708 females and 497 males) (Table 1; Figure 1).12
Table 1.
Types, number and percentage of accessory canals found in the maxilla and mandible sorted by frequency
| Classification of accessory canals identified | Abbreviation | Total number of cases (percentage) | Number of cases in females | Number of cases in males |
|---|---|---|---|---|
| Accessory canal in the region of canine to lateral incisor and extends to the alveolar crest (maxilla) | Mx-alv-crest | 279 (6.89) | 149 | 130 |
| Two canals appearing bilaterally in the area of lateral incisors (maxilla) | Mx-2bilateral | 253 (6.25) | 147 | 106 |
| Total maxillary cases | 532 (13.13) | 296 | 236 | |
| Two lingual canals at midline (mandible) | Md-2LatM | 510 (12.59) | 310 | 200 |
| One canal opening lingually (mandible) | Md-1L | 229 (5.65) | 129 | 100 |
| One canal opening buccally (mandible) | Md-1B | 181 (4.47) | 98 | 83 |
| Two canals opening lingually (mandible) | Md-2L | 137 (3.38) | 88 | 49 |
| Three lingual canals at midline (mandible) | Md-3LatM | 76 (1.88) | 50 | 26 |
| Two canals opening buccally (mandible) | Md-2B | 41 (1.01) | 21 | 20 |
| Three canals opening lingually (mandible) | Md-3L | 13 (0.32) | 6 | 7 |
| Accessory canal going upwards and opening in the alveolar crest (mandible) | Md-alv-crest | 7 (0.17) | 2 | 5 |
| Four lingual canals at midline (mandible) | Md-4LatM | 6 (0.15) | 3 | 3 |
| Two mental canals opening buccally (mandible) | Md-2Bmental | 5 (0.12) | 1 | 4 |
| Total mandibular cases | 1205 (29.75) | 708 | 497 | |
| Total number of cases | 1737 of 4051 cases (42.88) |
Md-1B, one canal opening buccally (mandible); Md-1L, one canal opening lingually (mandible); Md-2B, two canals opening buccally (mandible); Md-2Bmental, two mental canals opening buccally (mandible); Md-2L, two canals opening lingually (mandible); Md-2LatM, two lingual canals at midline (mandible); Md-3L, three canals opening lingually (mandible); Md-3LatM, three lingual canals at midline (mandible); Md-4LatM, four lingual canals at midline (mandible); Md-alv-crest, accessory canal travelling upwards and opening onto the alveolar crest (mandible); Mx-2bilateral, two canals appearing bilaterally in the area of lateral incisors (maxilla); Mx-alv-crest, accessory canal in the region of canine to lateral incisor, extending to the alveolar crest (maxilla).
Note that the values denoted here are calculated as a percentage of the 1737 cases with accessory canals.
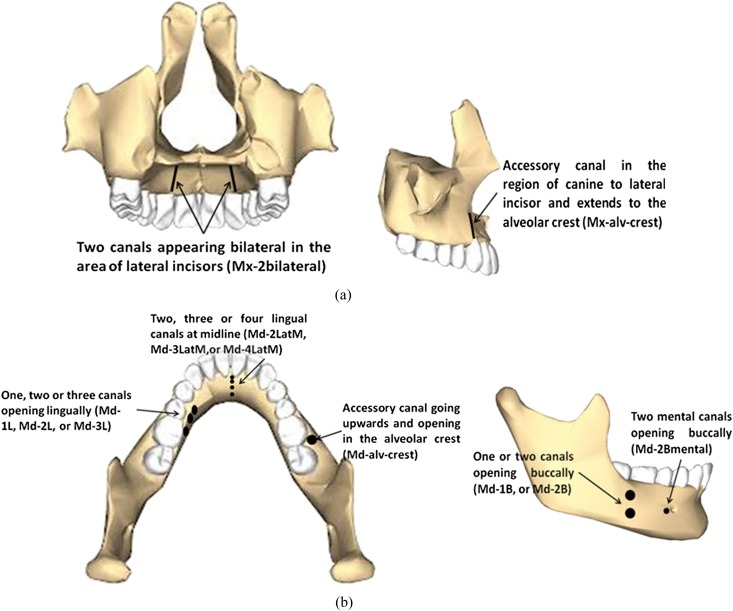
Figure 1.
Schematic drawings of the maxilla (a) and mandible (b) illustrating the various positions of accessory canals identified in this study. Md-1B, one canal opening buccally (mandible); Md-1L, one canal opening lingually (mandible); Md-2B, two canals opening buccally (mandible); Md-2Bmental, two mental canals opening buccally (mandible); Md-2L, two canals opening lingually (mandible); Md-2LatM, two lingual canals at midline (mandible); Md-3L, three canals opening lingually (mandible); Md-3LatM, three lingual canals at midline (mandible); Md-4LatM, four lingual canals at midline (mandible); Md-alv-crest, accessory canal travelling upwards and opening onto the alveolar crest (mandible); Mx-2bilateral, two canals appearing bilaterally in the area of lateral incisors (maxilla); Mx-alv-crest, accessory canal in the region of canine to lateral incisor, extending to the alveolar crest (maxilla). (Template from Anatomography.12)
The most common accessory canal presentations were the presence of two lingual canals at the midline of the mandible (12.6%), an accessory canal in the region of the canine to the lateral incisor extending to the alveolar crest of the maxilla (6.9%), and the presence of two canals appearing bilaterally in the area of the maxillary lateral incisors (6.3%). The prevalence of other presentations of accessory canals ranged from 5.7% to 0.1%, all of which were in the mandible (Figures 2–7).
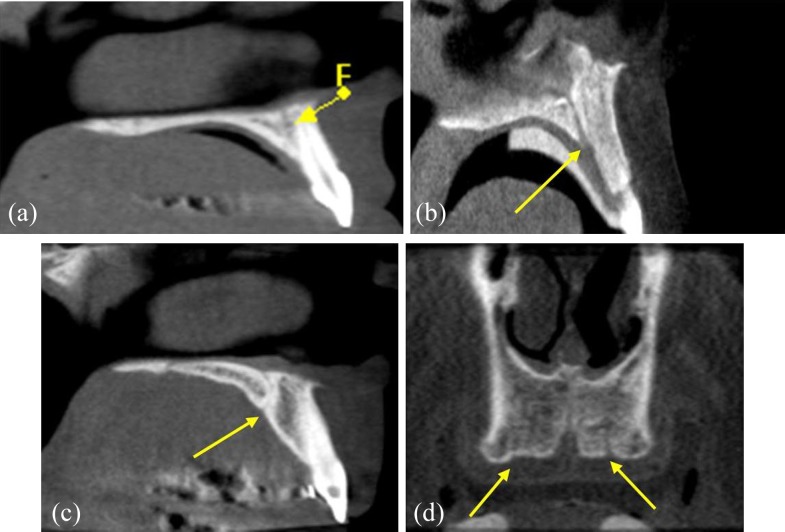
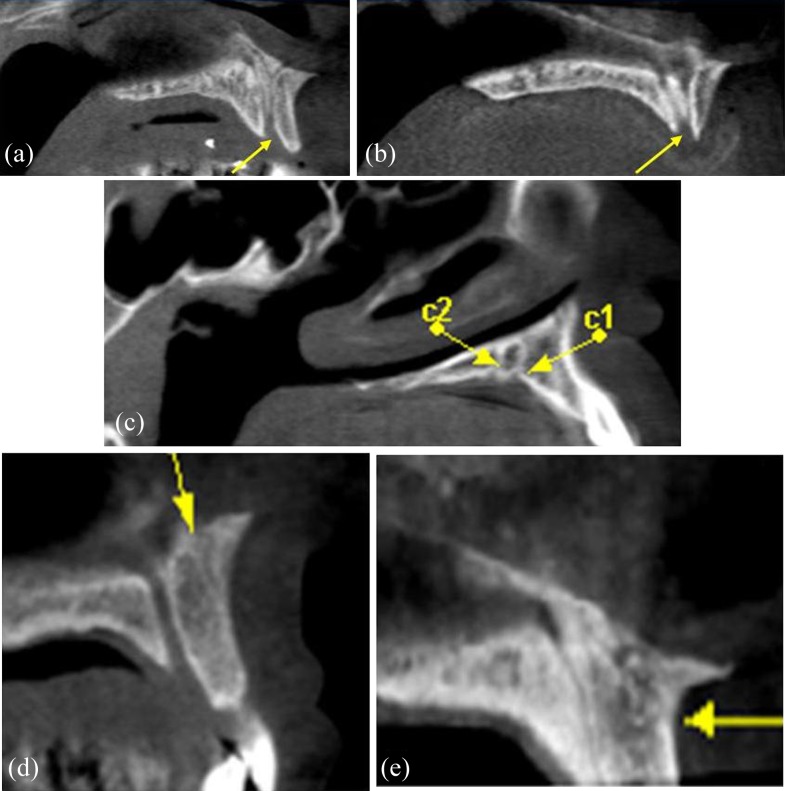
Figure 2.
Cone beam CT images showing two canals appearing bilaterally in the area of the maxillary lateral incisors (denoted by arrows). (a–c) Sagittal cuts (visualizing the canal present at one side of the patient); (d) coronal cut (visualizing the two canals bilaterally; note that the right canal is at a different coronal level in relation to the left canal, therefore is less evident in this cut). F, foramina.
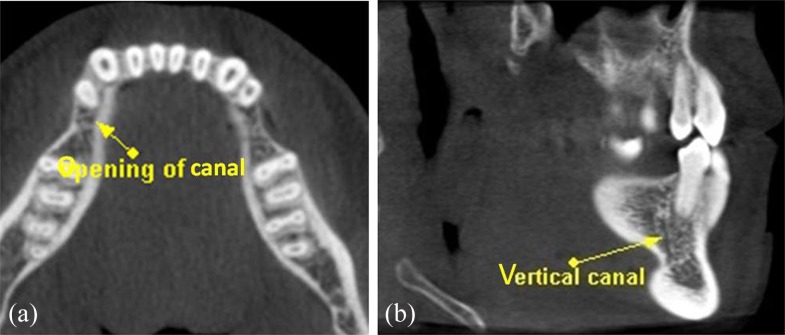
Figure 7.
Cone beam CT images showing an accessory canal travelling upwards and opening on the alveolar crest (mandible): (a) axial cut revealing the canal opening at the alveolar crest; (b) sagittal cut revealing the vertical course of the canal in the alveolar process.
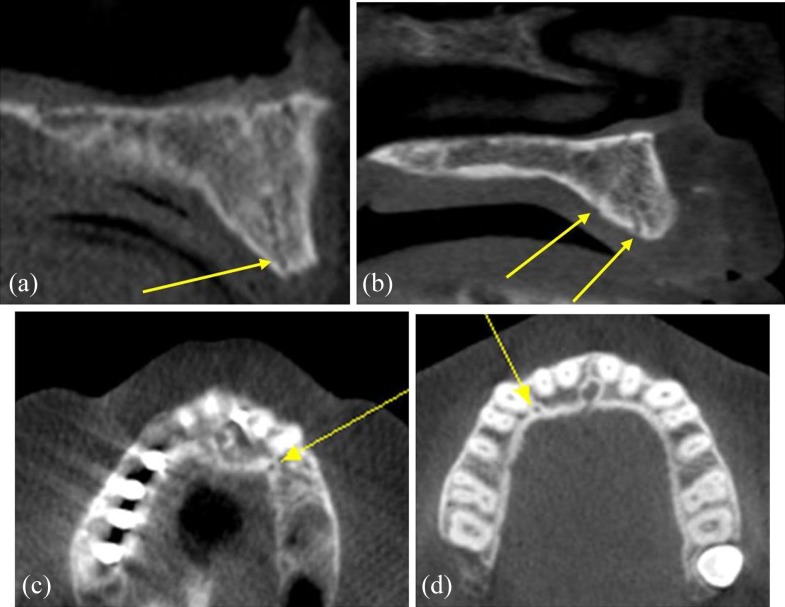
Figure 3.
Cone beam CT images showing a maxillary accessory canal in the region of the canine to lateral incisor, extending to the alveolar crest (denoted by arrows). (a, b) Sagittal cuts; (c, d) axial cuts.
Figure 4.
Cone beam CT images showing: (a, b) sagittal cuts of a bifid incisive canal (this was not considered an accessory canal). Note that this appears different from (c) sagittal cut of two accessory canals at the maxillary lateral incisor area; (d, e) sagittal cuts of accessory canals in the midline, opening buccally (denoted by arrows).
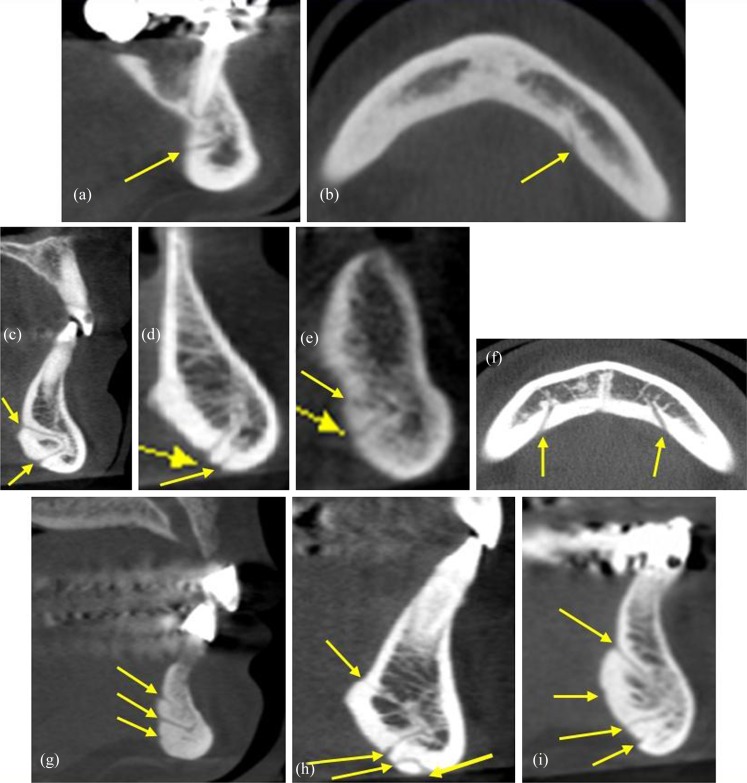
Figure 5.
Cone beam CT images showing mandibular lingual accessory canals (denoted by arrows): (a) sagittal cut and (b) axial cut revealing the presence of one canal opening lingually; (c–e) sagittal cuts and (f) axial cut revealing the presence of two canals opening lingually; (g) sagittal cut revealing the presence of three accessory canals opening lingually; (h) sagittal cut revealing the presence of three accessory canals opening lingually and one opening at the base of the inferior border; (i) sagittal cut revealing the presence of four accessory canals opening lingually.
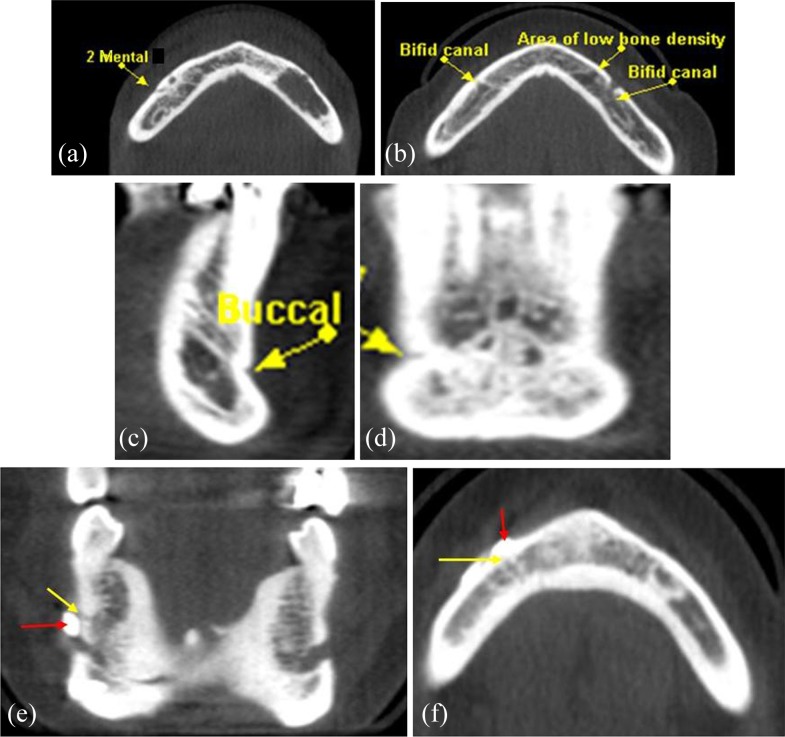
Figure 6.
Cone beam CT images showing mandibular buccal accessory canals (denoted by arrows): (a) axial cut revealing the presence of two mental canals; (b) axial cut revealing the presence of bilateral bifid mental canal and an area of low bone density (this was not considered an accessory canal; note that the left canal is at a different axial level in relation to the right canal, therefore is less evident on this cut); (c) sagittal cut and (d) coronal cut revealing the presence of an accessory canal opening buccally at the canine area; (e) coronal cut and (f) axial cut revealing the presence of an accessory canal opening buccally at a level superior to the mental foramen [note the presence of a radiopaque marker denoted by the inferior arrow in (e) and the superior arrow in (f)].
Discussion
Images produced by CBCT are high-resolution cross-sectional slices of varying thickness that offer high-resolution visualization of the structures of the jaws.13 Sherrard et al14 reported that tooth-length and root-length measurements obtained by CBCT were not significantly different from the true measured lengths; the mean difference was <0.3 mm. Mean differences between 0.2-, 0.3- and 0.4-mm voxel sizes were each <0.25 mm, with errors greatest at the 0.4-mm voxel size. The mean absolute difference in volumetric measurements of lateral defects was significantly less at 0.2-mm resolution than at 0.4 mm, compared with micro-CT images,15 demonstrating that high-resolution CBCT scans afford more accurate volumetric quantifications of lateral resorption defects than low-resolution scans. However, CBCT images at 0.2-mm voxel size can be used to accurately determine endodontic working length.16 Furthermore, no significant differences were observed between CBCT and periapical radiography in the detection of vertical root fractures, except for teeth with metallic posts in images from CBCT at 0.125-mm voxel size. Voxel size did not significantly influence the diagnosis of vertical root fractures.17 By extension, CBCT permits detailed visualization of the accessory canals of the jaws within the standard range of voxel sizes used in this study.
Despite the consensus that areas such as the intraforaminal region of the mandibular arch are relatively low-risk surgical sites, as evidenced by the relative scarcity of post-surgical complications, such as sensory deficits to the lip and chin after dental implant placement, additional consideration must still be given during pre-surgical assessment in these areas.1,4 Two-thirds of the neurovascular bundle of the inferior alveolar nerve, comprising the neurovascular supply to the lip and chin on the same side, exits at the mental foramen. The remaining one-third of the inferior alveolar nerve continues through the incisive canal and anastomoses with its opposing counterpart as well as with other vascular structures from the lingual foramen, which houses the lingual artery. Moreover, the submental artery, which is a branch of the facial artery, anastomoses with the incisive canal at or adjacent to the symphyseal midline. This vessel runs medial to the mandible and may insert into the mandibular symphysis at its inferior border.1,11
Most anatomy texts state that the mandibular canal gives off two small canals: the mental canal, which courses superiorly, posteriorly and laterally to the mental foramen, and the incisive canal, which continues medially below the incisor teeth. Tomographic imaging, by providing the ability to perform three-dimensional reconstruction, allows for highly detailed visualization of the mandibular canal.18–21
Superior and inferior genial foramina, spinal foramina and their bony canals are anatomical landmarks found at the interforaminal region. The superior genial foramina are at the level of or superior to the genial spine, whereas their inferior counterparts are below the genial spine. Combined, these foramina are reported in 85–99% of mandibles. These canals are corticated, so they can be readily visualized radiographically. Their existence is reported in texts focusing on dental radiographic anatomy but are seldom described in general anatomy and dental anatomy texts.11,22–26
In this study, we noted the presence of two lingual canals at the midline of the mandible in 12.6% of CBCT scans. Three lingual accessory canals opening in the midline were noted in 1.9% of cases and four accessory canals in 0.15% of cases.
Previous studies have shown, based on dissection, that the superior genial spinal foramen contains a branch of the lingual artery, vein and nerve, whereas the inferior genial spinal foramen contains a branch of the mylohyoid nerve, with or anastomosing with the sublingual and/or submental artery and vein.27–32 The mylohyoid artery generally courses from the lingual cortex at the bicuspid region to anastomose with the incisive canal in the cuspid area. As a branch of the facial artery, this artery runs anteromedially below the mandible and superficial to the mylohyoid muscle, terminating near the midline. Some authors described these foramina as nutrient canals, as a result of reports of substantial bleeding in the symphysis area following the raising of a flap in this region. Paraesthesia of the midline chin area has been reported following block graft harvesting, attributed to transection of this anterior neurovascular component.1 In our study, there were two mental foramina opening on the buccal side of the mandible in 1.0% of cases, while one accessory canal opening buccally on the mandible was noted in 4.5% of cases. An accessory mental foramen was defined as a buccal foramen showing continuity with the mandibular canal, excluding the mental foramen. A buccal foramen was defined as a canal penetrating the buccal cortical plate from the buccal bone surface not showing continuity with the mandibular canal.11
The submental artery supplies the floor of the mouth, submandibular lymph nodes and salivary gland, the mylohyoid and digastric muscles and the skin of the chin. The submental artery runs medial to the mandible and may insert into the mandibular symphysis at the inferior border.1,11 The submental vein drains the tissues of the chin, as well as the submandibular region.
Accessory foramina anterior to the mental foramen were reported in previous studies as being of varying number, size and location.29 The higher prevalence of foramina reported in this study, which we identified as a variety of accessory canals with openings on the lingual or buccal aspect of the mandible lateral to the canine area, numbering two or three canals, was attributable to advances in imaging technique using CBCT, especially at the lowest axial slice thickness. Some researchers found that in 80% of scans additional anterior foramina could be identified and their anastomoses with the incisive canal traced.29,30 These foramina can measure up to 2 mm in diameter, indicating the presence of a neurovascular component exiting the mandible to supply the chin. This explains the reported bleeding in the symphysis when tissue flaps are raised in this region. Additionally, paraesthesia of the midline chin area has been reported following block graft harvesting.30,31
In this study, accessory canals were seen adjacent to the nasopalatine canal, represented by two canals appearing bilaterally in the area of the maxillary lateral incisors in 6.3% of cases. 6.9% of cases had accessory canals in the region of the canine–lateral incisor, extending to the alveolar crest. The nasopalatine nerve and terminal branches of the palatine artery may travel through these canals. When the palatine processes of two maxillae are articulated, a funnel-shaped opening is found in the midline, posterior to the central incisor teeth, representing the nasopalatine foramen. The nasal floor contains the orifices of two radiographically visible lateral canals terminating at the nasal floor level at the foramina of Stensen, containing the nasopalatine nerve and terminal branches of the descending palatine artery.33 Moreover, two additional minor canals can be seen (Scarpa's foramina), which may transmit the nasopalatine nerve.
Radlanski et al33 reported that, by the 24th week of gestation, the incisive canal attains its typical pattern of two nasal entrances, in which the nasomaxillary crest separates the two branches of the nasopalatine nerves and arteries, and a common palatal orifice. Only solitary epithelial remnants from the nasopalatine duct remain at this developmental stage. The nasopalatine nerves and arteries run within the incisive canal. The incisive canal is located within the bony mass of the primary palate, away from the border between the primary and secondary palatal bone.
Mraiwa et al34 described nasopalatine canal variability relative to morphological appearance and dimensions. In their study, two canals were identified bilaterally in the maxilla: in the area of the lateral incisors (6.28%) and accessory canals in the region of the canine and lateral incisor (6.87%), extending to the alveolar crest. This is in agreement with reports describing the uncommon presence of nasopalatine canals with oronasal communication and canal openings in the palatal incisive papilla.35,36
In conclusion, CBCT imaging permits visualization of the accessory canals of the jaws with high resolution and accuracy. In this study, a network of accessory canals bringing into communication the inner and outer cortical plates of the jaws was identified radiographically. The presence of these accessory canals should be considered when performing pre-surgical planning for implant placement, bone grafting or other surgical procedures in the jaws, in light of the resulting potential risk of surgical complication. Additionally, the potential for the development of pathological processes associated with these accessory structures and their associated neurovascular bundles should be considered.
References
- 1.Miller RJ, Edwards WC, Boudet C, Cohen JH. Maxillofacial anatomy: the mandibular symphysis. J Oral Implantol 2011; 37: 745–53. doi: 10.1563/AAID-JOI-D-10-00136 [DOI] [PubMed] [Google Scholar]
- 2.Angelopoulos C. Cone beam tomographic imaging anatomy of the maxillofacial region. Dent Clin North Am 2008; 52: 731–52. doi: 10.1016/j.cden.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 3.Monsour PA, Dudhia R. Implant radiography and radiology. Aust Dent J 2008; 53(Suppl. 1): S11–25. doi: 10.1111/j.1834-7819.2008.00037.x [DOI] [PubMed] [Google Scholar]
- 4.Scaravilli MS, Mariniello M, Sammartino G. Mandibular lingual vascular canals (MLVC): evaluation on dental CTs of a case series. Eur J Radiol 2010; 76: 173–6. doi: 10.1016/j.ejrad.2009.06.002 [DOI] [PubMed] [Google Scholar]
- 5.Romanos GE, Greenstein G. The incisive canal. Considerations during implant placement: case report and literature review. Int J Oral Maxillofac Implants 2009; 24: 740–5. [PubMed] [Google Scholar]
- 6.Kohavi D, Bar-Ziv J. Atypical incisive nerve: clinical report. Implant Dent 1996; 5: 281–3. [DOI] [PubMed] [Google Scholar]
- 7.Hall SM. Observations on the progress of Wallerian degeneration in transected peripheral nerves of C57BL/Wld mice in the presence of recruited macrophages. J Neurocytol 1993; 22: 480–90. [DOI] [PubMed] [Google Scholar]
- 8.Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol 2004; 75: 631–45. doi: 10.1902/jop.2004.75.5.631 [DOI] [PubMed] [Google Scholar]
- 9.Givol N, Chaushu G, Halamish-Shani T, Taicher S. Emergency tracheostomy following life-threatening hemorrhage in the floor of the mouth during immediate implant placement in the mandibular canine region. J Periodontol 2000; 71: 1893–5. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs R, Lambrichts I, Liang X, Martens W, Mraiwa N, Adriaensens P, et al. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 683–93. doi: 10.1016/j.tripleo.2006.11.014 [DOI] [PubMed] [Google Scholar]
- 11.Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e25–31. [DOI] [PubMed] [Google Scholar]
- 12.Anatomography. Cited 7 February 2014. Available from: http://commons.wikimedia.org/wiki/File:Maxilla_close-up_posterior.png#; http://commons.wikimedia.org/wiki/File:Maxilla_close-up_lateral.png#; http://commons.wikimedia.org/wiki/File:Mandible_close-up_superior.png#; http://commons.wikimedia.org/wiki/File:Mandible_close-up_lateral.png#
- 13.Gupta R, Cheung AC, Bartling SH, Lisauskas J, Grasruck M, Leidecker C, et al. Flat-panel volume CT: fundamental principles, technology, and applications. Radiographics 2008; 28: 2009–22. doi: 10.1148/rg.287085004 [DOI] [PubMed] [Google Scholar]
- 14.Sherrard JF, Rossouw PE, Benson BW, Carrillo R, Buschang PH. Accuracy and reliability of tooth and root lengths measured on cone-beam computed tomographs. Am J Orthod Dentofacial Orthop 2010; 137: S100–8. doi: 10.1016/j.ajodo.2009.03.040 [DOI] [PubMed] [Google Scholar]
- 15.Ponder SN, Benavides E, Kapila S, Hatch NE. Quantification of external root resorption by low- vs high-resolution cone-beam computed tomography and periapical radiography: a volumetric and linear analysis. Am J Orthod Dentofacial Orthop 2013; 143: 77–91. doi: 10.1016/j.ajodo.2012.08.023 [DOI] [PubMed] [Google Scholar]
- 16.Connert T, Hülber-J M, Godt A, Löst C, Elayouti A. Accuracy of endodontic working length determination using cone beam computed tomography. Int Endod J Oct 2013. Epub ahead of print. doi: 10.1111/iej.12206. [DOI] [PubMed] [Google Scholar]
- 17.Junqueira RB, Verner FS, Campos CN, De vito KL, do Carmo AM. Detection of vertical root fractures in the presence of intracanal metallic post: a comparison between periapical radiography and cone-beam computed tomography. J Endod 2013; 39: 1620–4. doi: 10.1016/j.joen.2013.08.031 [DOI] [PubMed] [Google Scholar]
- 18.White SC, Pharoah MJ. The evolution and application of dental maxillofacial imaging modalities. Dent Clin North Am 2008; 52: 689–705. doi: 10.1016/j.cden.2008.05.006 [DOI] [PubMed] [Google Scholar]
- 19.Jacobs R, Mraiwa N, vanSteenberghe D, Gijbels F, Quirynen M. Appearance, location, course, and morphology of the mandibular incisive canal: an assessment on spiral CT scan. Dentomaxillofac Radiol 2002; 31: 322–7. doi: 10.1038/sj.dmfr.4600719 [DOI] [PubMed] [Google Scholar]
- 20.Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat 2004; 26: 329–33. doi: 10.1007/s00276-004-0242-2 [DOI] [PubMed] [Google Scholar]
- 21.Last RJ. Anatomy, regional and applied. 7th edn. Edinburgh, UK: Churchill Livingstone; 1984. pp. 575–7. [Google Scholar]
- 22.Woodbume RT, Burkel WE. Essentials of human anatomy. 8th edn. New York, NY: Oxford University Press; 1988. pp. 253–5. [Google Scholar]
- 23.Agur AM, Lee MJ, Grant JC. Grant's atlas of anatomy. 9th edn. Baltimore, MD: Lippincott Williams and Wilkins; 1991. p. 501. [Google Scholar]
- 24.Langland OE, Langlais RP. Principles of dental imaging. Baltimore, MD: Lippincott Williams and Wilkins; 1997. pp. 331–55. [Google Scholar]
- 25.Liang X, Jacobs R, Lambrichts I. An assessment on spiral CT scan of the superior and inferior genial spinal foramina and canals. Surg Radiol Anat 2006; 28: 98–104. doi: 10.1007/s00276-005-0055-y [DOI] [PubMed] [Google Scholar]
- 26.Vandewalle G, Liang X, Jacobs R, Lambrichts I. Macroanatomic and radiologic characteristics of the superior genial spinal foramen and its bony canal. Int J Oral Maxillofac Implants 2006; 21: 581–6. [PubMed] [Google Scholar]
- 27.McDonnell D, Reza Nouri M, Todd ME. The mandibular lingual foramen: a consistent arterial foramen in the middle of the mandible. J Anat 1994; 184: 363–9. [PMC free article] [PubMed] [Google Scholar]
- 28.Williams PL, Warwick R, Dyson M, Bannister LH. Gray's anatomy. 37th edn. Edinburgh, UK: Churchill Livingstone; 1989. pp. 368–90, 1106. [Google Scholar]
- 29.Trikeriotis D, Paravalou E, Diamantopoulos P, Nikolaou D. Anterior mandible canal communications: a potential portal of entry for tumour spread. Dentomaxillofac Radiol 2008; 37: 125–9. doi: 10.1259/dmfr/24407623 [DOI] [PubMed] [Google Scholar]
- 30.Langland OE, Sippy FH, Langlais RP. Textbook of dental radiology. 2nd edn. Springfield, IL: Charles C Thomas; 1984. pp. 380–411. [Google Scholar]
- 31.Kawai T, Sato I, Yosue T, Takamori H, Sunohara M. Anastomosis between the inferior alveolar artery branches and submental artery in human mandible. Surg Radiol Anat 2006; 28: 308–10. doi: 10.1007/s00276-006-0097-9 [DOI] [PubMed] [Google Scholar]
- 32.Liang X, Jacobs R, Lambrichts I, Vandewalle G, van Oostveldt D, Schepers E, et al. Microanatomical and histological assessment of the content of superior genial spinal foramen and its bony canal. Dentomaxillofac Radiol 2005; 34: 362–8. doi: 10.1259/dmfr/75895125 [DOI] [PubMed] [Google Scholar]
- 33.Radlanski RJ, Emmerich S, Renz H. Prenatal morphogenesis of the human incisive canal. Anat Embryol (Berl) 2004; 208: 265–71. doi: 10.1007/s00429-004-0389-y [DOI] [PubMed] [Google Scholar]
- 34.Mraiwa N, Jacobs R, van Steenberghe D, Quirynen M. Clinical assessment and surgical implications of anatomic challenges in the anterior mandible. Clin Implant Dent Relat Res 2003; 5: 219–25. [DOI] [PubMed] [Google Scholar]
- 35.Chapple IL, Ord RA. Patent nasopalatine ducts: four case presentations and review of the literature. Oral Surg Oral Med Oral Pathol 1990; 69: 554–8. [DOI] [PubMed] [Google Scholar]
- 36.Edwards PC, Kanjirath PP, Norton NS, McVaney T, Scanlon S, Saini T. Developmental oronasal fistula of the incisive papilla. Gen Dent 2010; 58: 62–7. [PubMed] [Google Scholar]