Abstract
Objectives:
To examine the presence and morphologic characteristics of bifid mandibular canals (BMCs) and retromolar foramens (RFs) using cone beam CT (CBCT) and to determine their visualization on panoramic radiographs (PANs).
Methods:
A sample of 225 CBCT examinations was analysed for the presence of BMCs, as well as length, height, diameter and angle. The diameter of the RF was also determined. Subsequently, corresponding PANs were analysed to determine whether the BMCs and RFs were visible or not.
Results:
The BMCs were observed on CBCT in 83 out of the 225 patients (36.8%). With respect to gender, statistically significant differences were found in the number of BMCs. There were also significant differences in anatomical characteristics of the types of BMCs. Only 37.8% of the BMCs and 32.5% of the RFs identified on CBCT were also visible on PANs. The diameter had a significant effect on the capability of PANs to visualize BMCs and RFs (B = 0.791, p = 0.035; B = 1.900, p = 0.017, respectively).
Conclusions:
PANs are unable to sufficiently identify BMCs and RFs. The diameter of these anatomical landmarks represents a relevant factor for visualization on PANs. Pre-operative images using only PANs may lead to underestimation of the presence of BMCs and to surgical complications and anaesthetic failures, which could have been avoided. For true determination of BMCs, a CBCT device should be considered better than a PAN.
Keywords: inferior alveolar nerve, accessory nerve, endosseous dental implantation, cone beam computed tomography, panoramic radiography
Introduction
Cone beam CT (CBCT) is increasingly being used as a diagnostic tool in the field of dentistry, especially in oral surgery. Its high-resolution three-dimensional images are better than panoramic radiographs (PANs) in that they reveal anatomic structures more clearly.1
Anatomic variations of the mandibular canal have been reported in studies using both PANs and CBCT.2–6 The reported rate of bifid mandibular canals (BMCs) on PAN ranged from 0.08% to 8.30%, whereas on CBCT, it ranged from 10% to 66%.3,7–13 One type of BMC is the retromolar canal, which ends in the retromolar foramen (RF). CBCT studies14,15 have reported rates of RF between 16% and 65%,3,11,13–16 similar to dry mandible studies ranging from 1.7% to 72.0%,17–19 whereas PANs have yielded a lower range.14
Identifying these anatomic structures has important clinical implications. It may help avoid some of the complications resulting from injury of BMCs during surgery, such as paraesthesia, sensory disturbances, traumatic neuromas and unanticipated profuse bleeding.19–21 Moreover, proper identification of BMCs may help adequate planning of anaesthesia.22,23 Worthy of special consideration is the retromolar canal, which is coursed by branches that contribute to innervation and supply the third molar, the most posterior zone of the alveolar process, and buccal gingival of mandibular pre-molars and molars.19 A variety of anatomical structures have been reported to arise from the RF, such as the buccal nerve, fibres innervating muscle temporalis and buccinators.24,25
Considering that PANs are sometimes used as the sole diagnostic tool in oral surgery and implant treatment planning, it is important to determine to what extent BMCs and RFs may go undetected, thus increasing the risk of certain surgical complications.3,8
The aim of the present study was two-fold: firstly, to analyse the presence and morphologic characteristics of BMCs and RFs using CBCT and secondly, to analyse the capability of PANs to visualize BMCs and RFs in comparison to CBCT.
Methods and materials
The overall sample consisted of 233 consecutive patients for whom pre-operative CBCT imaging was performed from July 2008 to March 2012 for various clinical indications, mainly for planning implants and impacted-tooth extractions, in the Radiology Unit of the Medicine and Dentistry School at the University of Santiago de Compostela, Santiago de Compostela, Spain. Ethical approval for the study was obtained from the Galician Ethics Committee of Clinical Research (Ref. 2012/272). Written informed consent was obtained from the participants in the study.
The inclusion criteria were the following: (i) both bilateral mandibular foramens had to be included in the CBCT volume; (ii) patients who had a PAN within a year of CBCT; and (iii) the CBCT voxel size was ≤0.3 mm. The exclusion criteria were the following: (i) patients with a history of mandibular trauma or surgical intervention in the mandible, such as orthognathic surgery, or repositioning of the inferior alveolar nerve; (ii) the presence of pathological findings in the anatomical area, such as osteomyelitis, fibrous dysplasia, tumours or cysts; and (iii) the presence of any artefacts or blurring due to patient movements affecting the image quality.
Imaging systems
CBCT images were obtained using a CBCT unit with a flat panel image detector of amorphous silicon (i-CAT® Model 17-19; Imaging Sciences International Inc., Hatfield, PA). All images were performed using the following protocol for patient position and exposure acquisition parameters: occlusal plane parallel to the floor base, a tube voltage of 120 kVp, a current of 5 mAs and 14.7 s.
PANs were performed using Orthophos® DS (Sirona Dental Systems GmbH, Bensheim, Germany) with a digital charge-coupled device line sensor. Exposure parameters were set at 80 kVp, 7 mAs and 14.1 s and a focus/sensor distance of 497 mm. PANs were processed using a computed radiography system (Sidexis® neXt Generation; Sirona Dental Systems GmbH, Bensheim, Germany). The PANs accepted for the survey met the following criteria: (i) free from any radiolucident or radiopaque lesion in the mandible; (ii) no evidence of current or past jaw fractures; and (iii) devoid of any radiographic exposure or processing artefacts.
Measurement procedure
Multiplanar reconstructions from CBCT were jointly analysed by two experienced researchers to identify any branching of the inferior alveolar canal in the area from the mandibular foramen to 30 mm from the anterior border of the mandibular ramus. For this purpose, digital imaging and communications in medicine files were reconstructed on a computer (Samsung R522; Samsung Electronics, Seoul, Republic of Korea) using i-CAT software (i-CAT Vision v. 1.9; Imaging Sciences International, Inc.). The CBCT slice thickness was ≤0.3 mm. The BMCs were classified into five types: type I, retromolar canal; type II, dental canal; type III, forward canal; type IV, buccolingual canal; and type V, superior canal. The retromolar canal bifurcated from the inferior mandibular canal in the mandibular ramus region and coursed upwards reaching the retromolar region. The dental canal ran forwards with its end in the root apex of the second or third molars. The forward canal coursed towards the front with or without joining the inferior alveolar canal. The buccolingual canals sprouted in a buccal or lingual direction from its origin. The superior canal followed an upward direction and did not meet the criteria for classification into any other group.
The following measurements were made: (i) on cross-sectional images: the width of mandibular bone at the point of bifurcation; (ii) on sagittal images: the height (vertical distance), length (anterioposterior distance) and diameter of BMCs, the angle of the BMCs with the mandibular canal (angle between the main canal and inferior wall of BMCs), and the diameter of the RF. Measurements were taken by one researcher under standard conditions (dimly lit room and a 15.6-inch monitor). 1 month later, the CBCT images for 30 patients were randomly selected, and the same researcher performed a re-measurement of the BMCs and RFs to assess intra-observer variability.
Para-panoramic 1.5-mm slice thickness reconstructions from CBCT obtained using i-CAT Vision and PANs were imported to image processing and evaluation software (Photoshop® v. 7.0; Adobe® Systems, San Jose, CA). Using CBCT images as a reference, two observers jointly analysed the PANs to determine whether or not the BMCs and RFs were visible.
Statistical analysis
Statistical analysis was performed using SPSS® v. 21.0 for Windows (IBM Corporation, Armonk, NY). Descriptive statistics were performed. The level of intra-observer agreement was assessed for anatomical measurements using the intraclass correlation coefficient. The χ2 test and the t-test were used to test differences in frequency and the morphologic characteristic of BMCs between genders. The one-way ANOVA with a post hoc Tukey's multiple comparison test were used to compare the characteristics of the different types of BMCs. The analysis of BMCs and RF visibility on PANs was performed using the Mann–Whitney U-test. The effect of anatomical characteristics of BMCs and RFs on their visibility on PANs was assessed using binary logistic regression, adjusting for possible confounding variables. Differences were considered significant at p < 0.05.
Results
The sample consisted of 225 CBCTs selected out of a total of 233 CBCTs. Of the excluded examinations, three CBCTs presented pathology (one patient had lesions consistent with cherubism, another had multiple dental inclusions and the third had an unspecific radiopaque lesion) and five volumes did not have adequate quality for diagnosis. The study sample consisted of 135 females (60%) and 90 males (40%), with a mean age of 43.87 years (range, 13.00–79.00 years).
Bifid mandibular canals on cone beam CT
BMCs were observed in 83 out of the 225 CBCTs (44 males and 39 females; 36.8% of the population) and in 103 out of 450 sides (22.8%) using CBCT (Figure 1). Out of the 83 patients with BMCs, 39 patients (21 males and 18 females) had unilateral presentation in the right mandible, 24 patients (12 males and 12 females) had presentation in the left mandible, whereas 20 patients (10 males and 10 females) had bilateral presentation. One BMC was observed in 99 sides. Two canals were seen in six sides (one side with lingual and dental canals; one side with lingual and anterior canals; two sides with two retromolar canals; one side with anterior and retromolar canals; and one side with two dental canals). A total of 111 BMCs were depicted. The results by the bifurcation type are shown in Table 1. BMCs were observed more frequently in males than females, both in terms of the total number of patients (48.8% vs 28.8%) and the total number of hemimandibles (30.0% vs 18.1%). Statistically significant differences regarding gender were found in the number of BMCs (p = 0.002 for total patients, and p = 0.006 for hemimandibles; Table 2).
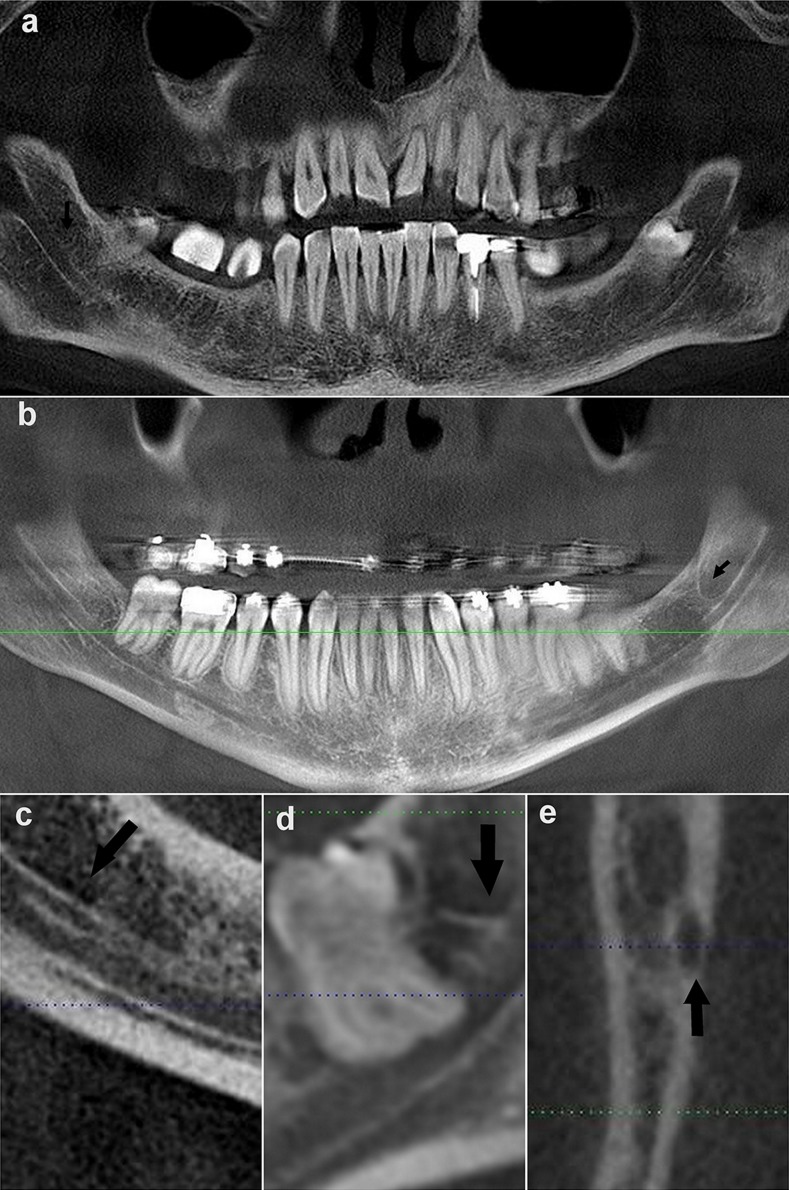
Figure 1.
Bifid mandibular canals on cone beam CT: (a) superior canal on the right mandibular body on panoramic reconstruction, 1.5 mm slice thickness; (b) retromolar canal on left retromolar region on panoramic reconstruction, 1.5 mm slice thickness; (c) forward canal on sagittal reconstruction; (d) dental canal towards the third molar cervical region on sagittal reconstruction; and (e) lingual canal on left ramus towards the lingual cortex on cross-sectional image.
Table 1.
The rate of bifid mandibular canal presence
| Mandibular canal | No. of canals [n (%)] | In all patients (%) | In all sides (%) |
|---|---|---|---|
| Forward canal | 43 (38.7) | 16.8 | 9.1 |
| Retromolar canal | 40 (36.0) | 12.0 | 8.6 |
| Dental canal | 19 (17.1) | 7.5 | 4.0 |
| Buccolingual canal | 6 (5.4) | 2.6 | 1.3 |
| Superior | 3 (2.7) | 0.8 | 0.4 |
Table 2.
The prevalence of bifid mandibular canal (BMC) regarding gender on cone beam CT (CBCT) and panoramic radiographs (PANs)
| Type of image | BMC, n (%) |
||
|---|---|---|---|
| Presence | Absence | p-value | |
| CBCT | |||
| Patients | |||
| Female (n = 135) | 39a (28.89)b | 96 (71.11) | |
| Male (n = 90) | 44 (48.89) | 46 (51.11) | 0.002c |
| Hemimandibles | |||
| Female (n = 270) | 49 (18.15) | 221 (81.85) | |
| Male (n = 180) | 54 (30.00) | 126 (70.00) | 0.006c |
| PAN | |||
| Patients | |||
| Female (n = 135) | 19a (14.00)b | 116 (85.90) | |
| Male (n = 90) | 19 (21.10) | 71 (78.80) | 0.168 |
| Hemimandibles | |||
| Female (n = 270) | 20 (7.40) | 250 (92.50) | |
| Male (n = 180) | 22 (12.22) | 158 (87.78) | 0.085 |
Number of female patients with BMC.
Percentage of female patients with BMC in female patients.
p < 0.05 (χ2 test).
BMCs presented a mean height of 6.3 ± 4.1 mm; a mean length of 7.1 ± 3.7 mm; a mean diameter of 1.6 ± 0.7 mm; and a mean angle of 30.7 ± 23.3°. None of the previous characteristics of BMCs showed statistically significant differences regarding gender. Table 3 summarizes the data according to the type of BMCs, no statistical differences were observed in length, whereas significant statistical differences were found in the height, diameter and angle of the BMCs. The height of forward canals was significantly different as compared with that of retromolar canals (p = 0.000) and buccolingual canals (p = 0.000). The height of retromolar canals was significantly different compared with that of dental canals (p = 0.000). Also, significant differences were found in the height between dental and buccolingual canals (p = 0.000) and between buccolingual and superior canals (p = 0.013). Significant differences in diameter were noted between the dental and superior canals (p = 0.035). The angle of forward canals was significantly different as compared with that of retromolar and superior canals (p = 0.005 and 0.005, respectively). The angle of retromolar canals was significantly different compared with that of buccolingual canals (p = 0.036). Also, the angle of buccolingual canals was significant different compared with that of superior canals (p = 0.004). The intra-observer agreement was calculated with intraclass correlation coefficient and presented values ranging from 0.72 to 0.98 (confidence interval of 95% ranging from 0.50 to 0.99).
Table 3.
Height, length, diameter and angle of bifid mandibular canals (BMCs) by gender and type
| Distribution groups | Height (mm) | Length (mm) | Diameter (mm) | Angle (°) |
|---|---|---|---|---|
| Total sample | 6.3 ± 4.1a | 7.1 ± 3.7a | 1.6 ± 0.7a | 30.7 ± 23.3a |
| Gender | ||||
| Male (n = 57) | 6.9 ± 4.4 | 7.3 ± 3.8 | 1.7 ± 0.6 | 32.6 ± 21.9 |
| Female (n = 54) | 5.6 ± 3.6 | 6.8 ± 3.6 | 1.5 ± 0.8 | 28.9 ± 24.8 |
| Type of BMC | ||||
| Forward canal (n = 43) | 5.0 ± 3.7 | 7.4 ± 4.1 | 1.5 ± 0.4 | 22.0 ± 18.7 |
| Retromolar (n = 40) | 8.4 ± 3.4 | 6.9 ± 2.8 | 1.6 ± 0.7 | 39.0 ± 24.6 |
| Dental (n = 19) | 3.2 ± 1.7 | 6.3 ± 4.0 | 2.0 ± 1.1 | 35.2 ± 20.5 |
| Buccolingual (n = 6) | 12.3 ± 4.6 | 10.1 ± 3.7 | 1.5 ± 0.7 | 12.0 ± 15.1 |
| Superior (n = 3) | 4.5 ± 0.7 | 4.6 ± 1.9 | 0.7 ± 0.2 | 66.8 ± 21.5 |
| p = 0.019b | p = 0.154 | p = 0.000b | p = 0.000b |
Mean ± standard deviation.
p < 0.05 (one-factor analysis of variance).
Bifid mandibular canals on panoramic radiographs
BMCs were identified in 38 out of the 225 PANs (20 males and 18 females between 15 and 71 years of age; 16.8% of the sample) and 42 out of the 450 sides (9.3%). 17 cases (9 males and 8 females) had unilateral presentation in the right mandible and 17 cases (9 males and 8 females) in the left mandible, whereas 4 cases were bilateral (2 males and 2 females). No multiple canals were found on any side. A total of 42 BMCs were found. BMCs were observed more frequently in male hemimandibles (12.2%) than in female hemimandibles (7.4%). No statistical difference was noted in the number of canals with respect to gender (Table 2).
A total of 42 out of the 111 BMCs identified using CBCT were visualized on PANs (37.8%) (Figure 2). With respect to canal type, no statistically significant differences were observed (p = 0.202). BMCs and mandibular bone characteristics with respect to visibility on PANs are shown in Table 4. A significant difference in height and diameter was observed (p = 0.014 and 0.004, respectively) with respect to the visualized and non-visualized BMCs groups on PANs. The binary logistic regression was adjusted for the variables age and gender. The morphological characteristics of BMCs, age and gender were included in the model. Age and gender were not found to be confounding variables. BMCs diameter was found to be statistically significant and did significantly influence the capability of PANs visualization (B = 0.791; p = 0.035) (Table 5).
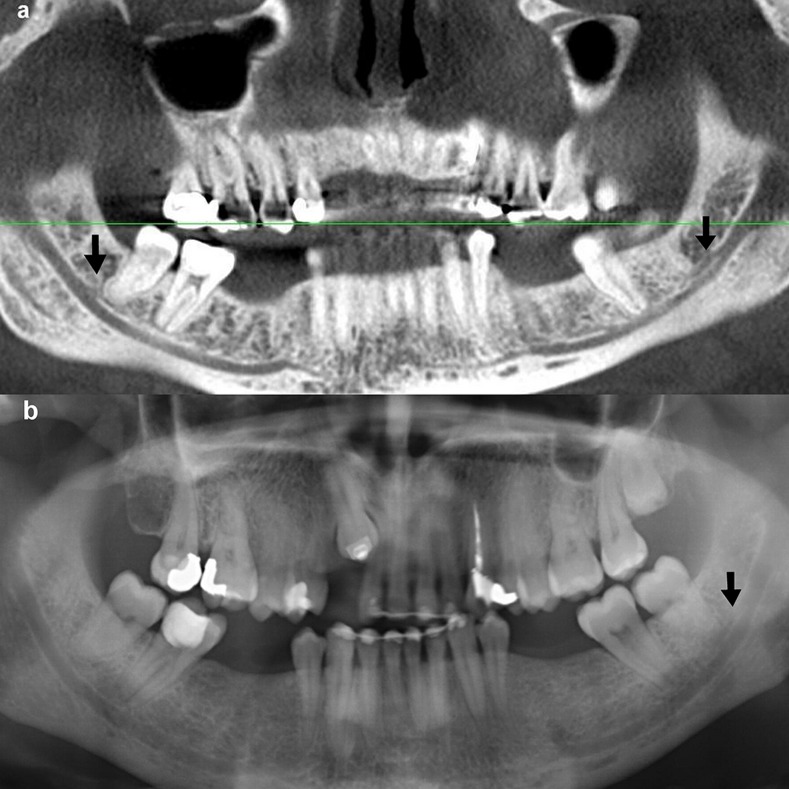
Figure 2.
(a) Dental and forward canal on cone beam CT para-panoramic reconstruction (left and right arrow, respectively). (b) Dental canal could not be identified on panoramic radiography (arrow).
Table 4.
Height, length, diameter and angle of the bifid mandibular canals (BMCs), width of mandibular bone and diameter of the retromolar foramen (RF) for the visualized and non-visualized BMCs groups on panoramic radiographs (mm, °)
| Factor related to visualization | Range | Mean | Standard deviation |
|---|---|---|---|
| Height of BMC | |||
| Visualization (n = 42) | 1.5–19.5 | 7.4a | 4.1 |
| No visualization (n = 69) | 0.0–16.5 | 5.6a | 3.9 |
| Length of BMC | |||
| Visualization (n = 42) | 2.2–16.2 | 7.4 | 3.1 |
| No visualization (n = 69) | 2.1–20.4 | 6.9 | 4.0 |
| Diameter of BMC | |||
| Visualization (n = 42) | 0.7–4.0 | 1.8a | 0.6 |
| No visualization (n = 69) | 0.5–5.5 | 1.5a | 0.7 |
| Angle of BMC | |||
| Visualization (n = 42) | 0.0–84.0 | 30.6 | 24.2 |
| No visualization (n = 69) | 0.0–85.0 | 30.7 | 22.9 |
| Width of mandibular bone | |||
| Visualization (n = 42) | 3.7–11.5 | 7.8 | 1.6 |
| No visualization (n = 69) | 5.2–12.3 | 8.4 | 1.5 |
| RF | |||
| Visualization (n = 13) | 1.0–3.6 | 2.1a | 0.7 |
| No visualization (n = 27) | 0.9–2.5 | 1.4a | 0.4 |
p < 0.05 (Mann–Whitney U-test).
Table 5.
The effect of age, gender and anatomical characteristics of bifid mandibular canals (BMCs) and retromolar foramens (RFs) on their visibility on panoramic radiographs
| Factors related to BMCs | B | SE | p-value | Odds ratio | 95% confidence interval |
||||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Visibility of BMCs | |||||||||
| Age | −0.005 | 0.014 | 0.747 | 0.995 | 0.968 | 1.024 | |||
| Gender | −0.207 | 0.450 | 0.645 | 0.813 | 0.336 | 1.963 | |||
| Width of mandibular bone | −0.221 | 0.141 | 0.119 | 0.802 | 0.608 | 1.058 | |||
| Height of BMC | 0.064 | 0.057 | 0.187 | 1.079 | 0.964 | 1.207 | |||
| Length of BMC | −0.010 | 0.068 | 0.888 | 0.990 | 0.867 | 1.131 | |||
| Diameter of BMC | 0.791 | 0.374 | 0.035a | 2.205 | 1.059 | 4.592 | |||
| Angle of BMC | 0.000 | 0.011 | 0.965 | 1.000 | 0.978 | 1.022 | |||
| Visibility of RFs | |||||||||
| Age | 0.002 | 0.026 | 0.949 | 1.002 | 0.951 | 1.055 | |||
| Gender | −0.233 | 1.045 | 0.823 | 0.792 | 0.102 | 6.140 | |||
| Diameter of RF | 1.900 | 0.799 | 0.017a | 6.685 | 1.397 | 31.980 | |||
SE, standard error.
p < 0.05 (binary logistic regression).
Retromolar foramen on cone beam CT
On CBCT, the RF was observed in 28 out of the total 225 examinations (15 males and 13 females; 12.4% of the sample) and 40 out of the 450 sides (8.8%). No statistically significant differences were found regarding gender. 16 patients had unilateral presentation, and 12 patients had bilateral presentation. A total of 40 RFs were found. The mean diameter of RF was 1.6 mm (standard deviation, 0.6 mm).
Retromolar foramen on panoramic radiographs
On PANs, the RF was identified in 12 out of the 225 examinations (8 males and 4 females; 5.3% of the sample) and in 13 out of the 450 sides (2.8%). One patient showed bilateral RF. Out of the 40 RFs observed on CBCT, 13 were identified using PANs. This represents an RF visualization rate on PANs of 32.5%. No statistical differences in visualization were found by gender (p = 0.106). A significant difference was observed in RF diameter with respect to visualized and non-visualized groups (p = 0.02; Table 4). The diameter of RF, age and gender were included in the model. Age and gender were not found to be confounding variables. There were statistically significant differences regarding the diameter of RF. The diameter of RF did significantly influence the capability of PANs visualization (B = 1.900; p = 0.017) (Table 5).
Discussion
To the best of our knowledge, this is the first study to analyse whether BMC morphologic characteristics influence their visibility on PANs. The only studies available describe the presence of BMCs on PANs without analysing potential influencing factors. Previous research conducted using various populations have described BMCs on multislice CT and CBCT,3,7–13 and have reported a wide variation in frequency, ranging from 10%13 to 65%.3 The present study is in line with Fu et al10 who identified BMCs in 30.6% of patients and 18.5% of total hemimandibles, and Orhan et al12 who observed BMCs in 27% of patients. There is also agreement with Fu et al10 in that BMCs were observed more frequently in males. Nevertheless, other studies found no such gender differences.3,8,9
With respect to the type of bifurcation, Naitoh et al3,26 and Orhan et al8,12 reported that forward and retromolar canals were the most frequent BMCs. The present study found a similar distribution with forward and retromolar types making up 75% of the total canals. We have used the BMC classification developed by Naitoh et al3 and added a previously undescribed canal type called superior canal, which is different in direction and did not meet the criteria for classification into any other group. Other studies using PANs suggest using more classifications.6,27–29 Kuribayashi et al7 reported that the most common BMC type was dental canal (type II classification of Nortjé et al6,29), which constituted 85% of their sample. In addition, Fu et al10 reported that more than half of their BMCs fell into either the retromolaror dental canal types (type IV and II classification of Nortjé et al6,29). Using PANs, Nortjé et al6 reported that forward canals (type I) were the most frequent.
Previous research on the prevalence of BMCs using PANs varies widely. To be of assistance in identifying suspected BMCs, a distinctive radiographic feature has been proposed. Auluck et al30 suggested that the possible presence of BMCs needs to be considered in cases where cortical outlines of different canals join to form triangular islands of bone. Naitoh et al31 reported that the presence of BMCs was suggested on PAN images in only two of five sides observed on CT images, showing that the true incidence of BMCs is underestimated by PAN images. Previously available research reported cases in which PANs failed to demonstrate bilateral BMCs despite their bilateral presence on CBCT.32,33 The present study involves a large sample and found that the rate of visualization of BMCs on PANs as compared with CBCT was similar to the results reported by Naitoh et al.31 Kuribayashi et al7 explained that buccolingual canals can be easily detected on CBCT but might be missed on PANs. However, in the present study, the proportion of buccolingual canals was very low, suggesting that features other than the canal type must also play a role. The overlap of anatomical structures may also interfere in the visualization of neurovascular canals. Owing to the two-dimensional nature of PANs, the upper airway, soft palate and uvula, and opposing side and submandibular fossae may produce ghost shadows and interfere with the visualization of neurovascular canals. The present study found a visualization rate of BMCs using PANs as compared with that using CBCT of 37.8%, which was similar to the rate previously reported by Naitoh et al.31 Neves et al,34 by contrast, reported a 76% visualization rate, but, this may be owing to the low number of BMCs that they detected on CBCT. Bogdán et al35 found 19.6% of BMCs in dry mandibles, but only 0.2% of total cases were visible on PANs.
With respect to the findings on the diameter of BMCs, the present study is in line with previous research, which reported averages of around 1.5 mm (individual cases ranging from 0.8 to 3.6 mm).7,9,10,15 There is also similarity with previous findings in terms of average RF diameter, which range from 0.99 to 2 mm14,15 (individual cases ranging from 0.20 to 4.35 mm).15,18 This variation may be owing to methodological differences; that is, measurement at the origin of the mandibular canal, at the opening of the RF or at 3 mm below.14,15 We found the unilateral location to be the most common, which is similar to previous studies,11,14,18,19 with the exception of Sagne et al36 who reported bilateral location. Like previous research, no significant gender differences were found regarding the presence of RF.14,15,17
The present study found that 32.5% of RFs identified on CBCT were also visualized on PANs. These results were somewhat higher than those of von Arx et al14 who reported a rate of 23%; however, this difference may be owing to the fact that the location of RF on CBCT was known at the time of analysing PANs in the present study. To the best of our knowledge, no further studies have been conducted on this issue.
Regarding visibility of anatomic landmarks, it has been suggested that bone trabeculation in the posterior mandible may affect the visibility of the mandibular canal. Bone trabeculation is known to influence the presence of mandibular canal corticalization, thus affecting its visibility.9 Moreover, the depiction of the mandibular canal has been related to cancellous bone density on PANs.37 Several authors have described factors influencing visualization of BMCs on PANs, such as buccolingual canal direction7 and superposition of anatomical structures.16 In addition, small diameter has been proposed as an explanation for the lower rate of BMC visualization on PANs.14,16 Indeed, we found the diameter to be a main factor in determining both BMCs and RFs on PANs.
Surgical procedures involving the mandible need to consider the clinical implications of BMCs. Considering that the retromolar region represents a frequent donor site for harvesting bone blocks, the identification of retromolar canals should be of primary concern. This is made clear by the observation of sensory disturbances associated with this procedure.38 Moreover, injury to neurovascular content of the retromolar canal during implant surgery can produce sensory disturbances and bleeding, which increases the possibility for peri-implant fibrous tissue formation.24 In addition, the presence of the dental canal has clinical implications for extraction and endodontic treatment because of the potential for lateral canals in the root canal.3,39 Anaesthesia failure in the inferior alveolar nerve may be associated with the presence of BMCs, especially when there are two mandibular foramens. Particularly, the suspicion of an anatomic variation should be taken into account when anaesthesia appears to have reached the ipsilateral lip and chin but not the teeth.22 Furthermore, a retromolar canal may cause difficulty in the anaesthesia of the buccal and retromolar mucosa. In conclusion, as has been observed in this research, we should be warned that PANs are unable to sufficiently identify BMCs and RFs and that the diameter of these anatomical landmarks represents a relevant factor for visualization. For true determination of BMCs, a CBCT device should be considered better than PANs. Further research is necessary to determine other factors that can influence the visibility of anatomic structures in PANs.
Acknowledgments
Acknowledgments
The authors wish to express their gratitude to the radiologist Lilian Sampedro Crujeiras, for her exceptional work in the Radiology Unit, Medicine and Dentistry School of Santiago de Compostela, Santiago de Compostela, Spain, and for the contribution to the development of this research.
References
- 1.Angelopoulos C, Thomas SL, Hechler S, Parissis N, Hlavacek M. Comparison between digital panoramic radiography and cone-beam computed tomography for the identification of the mandibular canal as part of presurgical dental implant assessment. J Oral Maxillofacial Surg 2008; 66: 2130–5. [DOI] [PubMed] [Google Scholar]
- 2.Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res 2012; 23: 1022–30. doi: 10.1111/j.1600-0501.2011.02261.x [DOI] [PubMed] [Google Scholar]
- 3.Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants 2009; 24: 155–9. [PubMed] [Google Scholar]
- 4.Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 289–94. doi: 10.1016/j.tripleo.2008.09.010 [DOI] [PubMed] [Google Scholar]
- 5.Sanchis JM, Penarrocha M, Soler F. Bifid mandibular canal. J Oral Maxillofacial Surg 2003; 61: 422–4. doi: 10.1053/joms.2003.50004 [DOI] [PubMed] [Google Scholar]
- 6.Nortjé CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg 1977; 15: 55–63. [DOI] [PubMed] [Google Scholar]
- 7.Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T. Bifid mandibular canals: cone beam computed tomography evaluation. Dentomaxillofac Radiol 2010; 39: 235–9. doi: 10.1259/dmfr/66254780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orhan K, Aksoy S, Bilecenoglu B, Sakul BU, Paksoy CS. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: a retrospective study. Surg Radiol Anat 2011; 33: 501–7. doi: 10.1007/s00276-010-0761-y [DOI] [PubMed] [Google Scholar]
- 9.de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig 2012; 16: 387–93. doi: 10.1007/s00784-011-0544-9 [DOI] [PubMed] [Google Scholar]
- 10.Fu E, Peng M, Chiang CY, Tu HP, Lin YS, Shen EC. Bifid mandibular canals and the factors associated with their presence: a medical computed tomography evaluation in a Taiwanese population. Clin Oral Implants Res 2014; 25: e64–7. doi: 10.1111/clr.12049 [DOI] [PubMed] [Google Scholar]
- 11.Lizio G, Pelliccioni GA, Ghigi G, Fanelli A, Marchetti C. Radiographic assessment of the mandibular retromolar canal using cone-beam computed tomography. Acta Odontol Scand 2013; 71: 650–5. doi: 10.3109/00016357.2012.704393 [DOI] [PubMed] [Google Scholar]
- 12.Orhan AI, Orhan K, Aksoy S, Ozgul O, Horasan S, Arslan A, et al. Evaluation of perimandibular neurovascularization with accessory mental foramina using cone-beam computed tomography in children. J Craniofac Surg 2013; 24: e365–9. doi: 10.1097/SCS.0b013e3182902f49 [DOI] [PubMed] [Google Scholar]
- 13.Kang JH, Lee KS, Oh MG, Choi NY, Lee SR, Oh SH, et al. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci Dent 2014; 44: 53–60. doi: 10.5624/isd.2014.44.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.von Arx T, Hanni A, Sendi P, Buser D, Bornstein MM. Radiographic study of the mandibular retromolar canal: an anatomic structure with clinical importance. J Endod 2011; 37: 1630–5. doi: 10.1016/j.joen.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 15.Patil S, Matsuda Y, Nakajima K, Araki K, Okano T. Retromolar canals as observed on cone-beam computed tomography: their incidence, course, and characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 115: 692–9. doi: 10.1016/j.oooo.2013.02.012 [DOI] [PubMed] [Google Scholar]
- 16.Kawai T, Asaumi R, Sato I, Kumazawa Y, Yosue T. Observation of the retromolar foramen and canal of the mandible: a CBCT and macroscopic study. Oral Radiol 2012; 28: 10–14. [Google Scholar]
- 17.Ossenberg NS. Retromolar foramen of the human mandible. Am J Phys Anthropol 1987; 73: 119–28. doi: 10.1002/ajpa.1330730112 [DOI] [PubMed] [Google Scholar]
- 18.Narayana K, Nayak UA, Ahmed WN, Bhat JG, Devaiah BA. The retromolar foramen and canal in South Indian dry mandibles. Eur J Anat 2002; 6: 141–6. [Google Scholar]
- 19.Bilecenoglu B, Tuncer N. Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg 2006; 64: 1493–7. doi: 10.1016/j.joms.2006.05.043 [DOI] [PubMed] [Google Scholar]
- 20.Wadhwani P, Mathur RM, Kohli M, Sahu R. Mandibular canal variant: a case report. J Oral Pathol Med 2008; 37: 122–4. doi: 10.1111/j.1600-0714.2007.00573.x [DOI] [PubMed] [Google Scholar]
- 21.Claeys V, Wackens G. Bifid mandibular canal: literature review and case report. Dentomaxillofac Radiol 2005; 34: 55–8. doi: 10.1259/dmfr/23146121 [DOI] [PubMed] [Google Scholar]
- 22.Lew K, Townsen G. Failure to obtain adequate anaesthesia associated with a bifid mandibular canal: a case report. Aust Dent J 2006; 51: 86–90. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman E, Weinstein P, Milgrom P. Difficulties in achieving local anesthesia. J Am Dent Assoc 1984; 108: 205–8. [DOI] [PubMed] [Google Scholar]
- 24.Singh S. Aberrant buccal nerve encountered at third molar surgery. Oral Surg Oral Med Oral Pathol 1981; 52: 142. [DOI] [PubMed] [Google Scholar]
- 25.Anderson LC, Kosinski TF, Mentag PJ. A review of the intraosseous course of the nerves of the mandible. J Oral Implantol 1991; 17: 394–403. [PubMed] [Google Scholar]
- 26.Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 25–31. [DOI] [PubMed] [Google Scholar]
- 27.Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc 1985; 110: 923–6. [DOI] [PubMed] [Google Scholar]
- 28.Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat 1971; 108: 433–40. [PMC free article] [PubMed] [Google Scholar]
- 29.Nortje CJ, Farman AG, de V Joubert JJ. The radiographic appearance of the inferior dental canal: an additional variation. Br J Oral Surg 1977; 15: 171–2. [DOI] [PubMed] [Google Scholar]
- 30.Auluck A, Pai KM, Shetty C. Pseudo bifid mandibular canal. Dentomaxillofac Radiol 2005; 34: 387–8. doi: 10.1259/dmfr/59445082 [DOI] [PubMed] [Google Scholar]
- 31.Naitoh M, Hiraiwa Y, Aimiya H, Gotoh M, Ariji Y, Izumi M, et al. Bifid mandibular canal in Japanese. Implant Dent 2007; 16: 24–32. doi: 10.1097/ID.0b013e3180312323 [DOI] [PubMed] [Google Scholar]
- 32.Fukami K, Shiozaki K, Mishima A, Kuribayashi A, Hamada Y, Kobayashi K. Bifid mandibular canal: confirmation of limited cone beam CT findings by gross anatomical and histological investigations. Dentomaxillofac Radiol 2012; 41: 460–5. doi: 10.1259/dmfr/60245722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mizbah K, Gerlach N, Maal TJ, Berge SJ, Meijer GJ. Bifid and trifid mandibular canal. A coincidental finding. [In Dutch.] Ned Tijdschr Tandheelkd 2010; 117: 616–18. [DOI] [PubMed] [Google Scholar]
- 34.Neves F, Nascimento M, Oliveira M, Almeida S, Bóscolo F. Comparative analysis of mandibular anatomical variations between panoramic radiography and cone beam computed tomography. Oral Maxillofac Surg; in press. Epub ahead of print August 2013. doi: 10.1007/s10006-013-0428-z [DOI] [PubMed] [Google Scholar]
- 35.Bogdán S, Pataky L, Barabas J, Nemeth Z, Huszar T, Szabo G. Atypical courses of the mandibular canal: comparative examination of dry mandibles and x-rays. J Craniofac Surg 2006; 17: 487–91. [DOI] [PubMed] [Google Scholar]
- 36.Sagne S, Olsson G, Hollender L. Retromolar foramina and canals in the human mandible. Studies in a medieval skull material. Dentomaxillofac Radiol 1977; 6: 41–5. [DOI] [PubMed] [Google Scholar]
- 37.Naitoh M, Katsumata A, Kubota Y, Hayashi M, Ariji E. Relationship between cancellous bone density and mandibular canal depiction. Implant Dent 2009; 18: 112–18. doi: 10.1097/ID.0b013e318198da7e [DOI] [PubMed] [Google Scholar]
- 38.Silva FM, Cortez AL, Moreira RW, Mazzonetto R. Complications of intraoral donor site for bone grafting prior to implant placement. Implant Dent 2006; 15: 420–6. doi: 10.1097/01.id.0000246225.51298.67 [DOI] [PubMed] [Google Scholar]
- 39.Rossi AC, Freire AR, Prado BG, Prado FB, Botacin PR, Caria PH. Incidence of retromolar foramen in human mandibles: ethnic and clinical aspects. Int J Morphol 2012; 30: 1074–8. [Google Scholar]