Abstract
Objective: The purpose of this study was to investigate the shear bond strength (SBS) of two different adhesive resin cements used to lute ceramics on laser-etched dentin. Background data: Erbium, chromium: yttrium, scandium, gallium, garnet (Er,Cr:YSGG) laser irradiation has been claimed to improve the adhesive properties of dentin, but results to date have been controversial, and its compatibility with existing adhesive resin cements has not been conclusively determined. Materials and methods: Two adhesive cements, one “etch-and-rinse” [Variolink II (V)] and one “self-etch” [Clearfil Esthetic Cement (C)] luting cement, were used to lute ceramic blocks (Vita Celay Blanks, Vita) onto dentin surfaces. In total, 80 dentin specimens were distributed randomly into eight experimental groups according to the dentin surface-etching technique used Er,Cr:YSGG laser and Er:YAG laser: (1) 37% orthophosphoric acid+V (control group), (2) Er,Cr:YSGG laser+V, (3) Er,Cr:YSGG laser+acid+V, (4) Er:YAG laser+V, (5) Er:YAG laser+acid+V, (6) C, (7) Er,Cr:YSGG laser+C, and (8) Er:YAG laser+C. Following these applications, the ceramic discs were bonded to prepared surfaces and were shear loaded in a universal testing machine until fracture. SBS was recorded for each group in MPa. Shear test values were evaluated statistically using the Mann–Whitney U test. Results: No statistically significant differences were evident between the control group and the other groups (p>0.05). The Er,Cr:YSGG laser+A+V group demonstrated significantly higher SBS than did the Er,Cr:YSGG laser+V group (p=0.034). The Er,Cr:YSGG laser+C and Er:YAG laser+C groups demonstrated significantly lower SBS than did the C group (p<0.05). Conclusions: Dentin surfaces prepared with lasers may provide comparable ceramic bond strengths, depending upon the adhesive cement used.
Introduction
The search for techniques and materials capable of restoring teeth, and recovering aesthetic and functional properties, with the least discomfort for the patient, is constant in dentistry. Over the last few years, new techniques have become available because of advances in dentistry, and as a consequence of the development of other areas of knowledge. Preservation of tooth structure has become an important trend in modern dentistry, with new equipment and techniques available for cavity preparation as well as new or improved restorative materials.1
Ceramic restorations have gained popularity among clinicians and patients, because of their superior aesthetics and the possibility of conservative tooth preparations. Long-term survival of the restoration depends primarily on the strength and durability of the bond between the ceramic and the dental substrates.2 Pretreatment of the tooth surface is essential for establishing a strong bond between the ceramic and both the enamel and dentin. Acid-etching has been the standard approach for enamel pretreatment since the introduction of Buonocore.3 The retention to dentin is based mainly on hybrid layer formation and, to a lesser extent, on the micromechanical retention offered by the resin tags embedded in the dentin. The bonding of resin to enamel is achieved via micromechanical retention on the roughened surface in cavity preparation.4 Therefore, the formation of a hybrid layer and resin tags is essential for the establishment of a strong bond at the dentin level.5 This type of strong bond can be achieved by complete dissolution of the smear layer and demineralization of the intertubular and peritubular dentin by means of acid etching, resulting in an exposed collagen matrix that can be infiltrated by resin.
In recent years, there has been a growing debate about the use of lasers for various applications in dentistry, including carious dentin removal or cavity preparation.6–8 Erbium, chromium: yttrium-scandium-gallium-garnet (Er,Cr:YSGG) and erbium: yttrium-aluminum-garnet (Er:YAG) lasers can ablate enamel and dentin effectively because of the high absorption by water and hydroxyapatite.6 Surfaces irradiated by these lasers showed a characteristic rough surface, clean and without debris, open dentinal tubules, and microirregularities caused by the preferential removal of the intertubular dentin, suggesting that the resultant dentin surface is receptive to adhesive procedures.9,10 However, some studies have shown a decrease in the bond strength values of superficial parts of laser-irradiated surfaces compared with surfaces prepared by conventional instruments.11,12
Apart from laser technology, significant advances in enamel and dentin adhesive systems have been made over the past several years. The development of adhesives has progressed to a single-step approach (e.g., self-etch adhesive), absent the separate etching step used in the conventional adhesive (three step) systems; this shortens the application time and reduces the errors that can occur at each bonding step.13 Several studies have been performed using different adhesive systems, and have produced conflicting results. Because all of the adhesive systems were originally developed to act on tooth substrates prepared by conventional techniques, additional investigation is required into the adhesion performance of various adhesive systems on laser-prepared dental surfaces.
Previous studies have mainly dealt with the bond strength between adhesives and tooth surfaces, or ceramics and resin cements.14–17 However, to date, few studies have investigated the shear bond strength (SBS) between ceramic and laser-etched tooth surfaces.10,18,19 Therefore, the aim of this in vitro study was to measure and compare the bond strength of two adhesive resin cements used to lute ceramics onto Er,Cr:YSGG and Er:YAG laser-etched dentin. Scanning electron microscopy (SEM) analysis was also performed for two specimens in each group after the SBS test was performed, to evaluate the nature of the fractured surface. The null hypotheses tested were (1) that the SBS obtained after Er,Cr:YSGG or Er:YAG laser etching of dentin is similar to that obtained after acid etching and can be an alternative to acid etching, and (2) that there is a significant difference in the SBS to dentin etched with Er,Cr:YSGG or Er:YAG laser in combination with acid etching versus that etched with acid alone, with the adhesive resin cements tested.
Materials and Methods
Sample preparation
Eighty extracted human third molar teeth (gathered after receiving informed written consent from the patients) that were free of caries and restorations were selected. These teeth samples were cleaned of surface debris and stored in 0.5% chloramine T-solution for 24 h. The teeth were then stored in distilled water for <6 months, pending further processing. Each tooth was fixed in a plastic cube with acrylic resin (Panacryl, İnci Dental, Turkey), 2–3 mm below the cementum–enamel junction. The enamel surfaces were ground flat parallel to the tooth surface, using fissure diamond burs (#8, Dia-Burs, MANI Inc., Tochigi, Japan), to expose the superficial dentin surfaces. Prepared dentin surfaces were abraded with 600 grit silicon carbide (SiC) paper for 60 sec to create a standard and clinically relevant smear layer.
In total, 80 standardized ceramic discs were prepared from commercially available porously pre-sintered aluminium oxide (Al2O3) porcelain blocks (VITA In-Ceram ALUMINA for CELAY Blanks, Vita Zahnfabric, Bad Sackingen, Germany). The blocks were sectioned at 8 mm in diameter and 4 mm in height using a precision saw (IsoMet 1000, Buehler, USA) with a diamond blade [6 in (152mm) IsoMet Buehler, USA]. The bonding surfaces of the ceramic discs were subjected to a sandblasting procedure with 50 μm Al2O3. For cementation of the ceramic discs, the 80 dentin specimens were assigned to eight groups of 10 (n=10). The first five groups were luted to the ceramic discs with an etch-and-rinse adhesive resin [Variolink II (V)] cement; the other three groups used a self-etch adhesive resin [Clearfil Esthetic Cement (C)] cement. All of the dentin specimens were prepared with one of the following treatments before the bonding of ceramic discs: (1) 37% orthophosphoric acid (A)+V (control group), (2) Er,Cr:YSGG laser+V, (3) Er,Cr:YSGG laser+A+V, (4) Er:YAG laser+V, (5) Er:YAG laser+A+V, (6) C, (7) Er,Cr:YSGG laser+C, and (8) Er:YAG laser+C.
Dentin surface treatment
In the first group (control), dentin surfaces were exposed to 37% orthophosphoric acid etching gel for 15 sec, then rinsed for 20 sec with a water spray. In the second, third, and seventh groups, the dentin surfaces were prepared using an Er,Cr:YSGG laser (Waterlase MD, Biolase Technologies, Irvine, CA) (wavelength, 2.78 μm; pulse duration, 140 μs; energy, 1.5 W; repetition rate, 20 Hz) with water spray (75% water, 85% air), in accordance with the manufacturer's instructions. The laser beam was used in a noncontact mode 1–2 mm from the target area, and the 600 μm diameter sapphire tip was held perpendicular to the dentin surface and moved in a sweeping fashion by hand during the exposure time (15 sec). In the fourth, fifth, and eighth groups, an Er:YAG laser [Fidelis PLUS, Fotona Medical Lasers, Ljubljana, Slovenia; wavelength, 2.94-μm; laser energy, 120 mJ per pulse; pulse duration, 100 μs (very short pulse); repetition rate, 10 Hz; treatment time, 15 sec; noncontact hand pieces (R02); beam spot size, 0.6 mm; within 1–2 mm of the dentin surface] with continuous water irrigation (40–60 mL/min) was used to irradiate the dentin surfaces, in accordance with previous studies.20–22
Bonding procedures
Following the surface treatments, ceramic discs were cemented to prepared dentin surfaces with Variolink II (conventional etch-and-rinse resin cement) or Clearfil Esthetic Cement (self-etch resin cement). All of the bonding procedures were performed strictly following the manufacturer's instructions.23,24 For the Variolink II groups, the ceramic discs were treated with 10% hydrofluoric acid (CondacPorcelana, FGM, Brazil) for 60 sec. For the Clearfil Esthetic Cement groups, the ceramic disc surfaces were treated with 5% phosphoric acid (K-Etchant gel, Kuraray Medical INC., Okayama, Japan) for 5 sec.
During the ceramic disc cementation, a custom-designed device was used to stabilize the ceramic discs on the prepared dentin surfaces (Fig. 1). After exact positioning and alignment of specimens, the device was top-loaded with 10 N of force for 10 sec, to ensure that pure forces were applied to standardize the cement film thicknesses. Excess cement was removed with a microbrush. The luting agent was polymerized from each direction for 40 sec with a light emitting diode (LED)-curing light, using a previously tested output of 450 mW/cm2 (Bluephase C5, Ivoclar, Vivadent, Schaan, Liechtenstein). The details of the luting cements used in this study, along with their composition, are listed in Table 1.
FIG. 1.
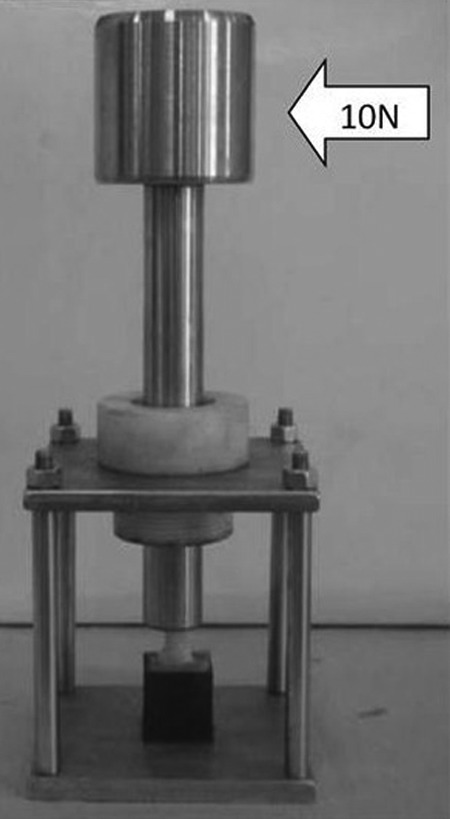
Custom-designed device used to stabilize the ceramic discs on the prepared dentin surfaces.
Table 1.
List of Resin-Luting Cements Tested and their Application Protocol
| Luting cements | Manufacturer | Composition | Application protocol |
|---|---|---|---|
| Variolink II Low Viscosity (incl. ExciTE DSC) | Ivoclar-Vivadent, Schaan, Liechtenstein | Monomer matrix is composed of Bis-GMA, urethane dimethacrylate, and triethylene glycol dimethacrylate. Inorganic fillers are barium glass, ytterbium trifluoride, Ba-Al-fluorosilicate glass and spheroid mixed oxide. Additional contents: catalysts, stabilizers, and pigments. |
Etch dentin for 15 sec and rinse with H3PO4 (Total etch, Ivoclar-Vivadent); apply ExciTE DSC with a brush on the dentin surface, and agitate for at least 10 sec; dry for 1–3 sec; the surface should have a uniform glossy appearance; light cure for 20 sec; mix equal amounts of base and catalyst paste for 10 sec; apply with a brush on dentin and, if necessary, on the restoration; light cure for 20 sec (four times sideways, one time from above, 80 sec in total). |
| Clearfil Esthetic Cement (C) | Kuraray Medical Inc., Tokyo, Japan | ED Primer II Liquid A: HEMA, 10-MDP, 5-NMSA, water, accelerator ED Primer II Liquid B: 5-NMSA, accelerator, water, initiator Clearfil Esthetic Cement Paste A: Bis-GMA, TEGDMA, hydrophobic aromatic dimethacrylate monomers, silanated barium glass filler, colloidal silica, accelerator Clearfil Esthetic Cement Paste B: Bis-GMA, TEGDMA, hydrophobic aromatic dimethacrylate monomers, hydrophilic aliphatic dimethacrylate monomers, silanated barium glass filler, silanated silica, colloidal silica, benzoyl peroxide, dicamphorquinone, pigments |
Dispense equal amounts of ED Primer II Liquid A and B and mix; apply ED primer II and leave for 30 sec; remove any excess of primer using a cotton pellet and dry the primer completely with gentle air flow; apply on dentin; remove excess cement; light cure each surface for 20 sec (four times sideways, one time from above, 80 sec in total) |
HEMA, hydroxyethylmethacrylate; 10-MDP, 10-methacryloyloxi-decyl-dihydrogen-phosphate; 5-NSMA, N-methacryloyl-5-aminosalicylic acid; TEGDMA, triethyleneglycol-dimethacrylate.
Thermocycle procedure
The specimens were stored in distilled water at 37°C for 24 h. They were then subjected to 500 thermal cycles, alternating between 5±2°C and 55±2°C water baths, with a dwell time of 30 sec and transfer time of 3 sec.
SBS test
The SBSs were measured using a Zwick Z010 universal testing machine (Zwick GmbH, Ulm, Germany). A steel L-shaped metal chisel was used as the loading device. All specimens were loaded at a crosshead speed of 0.5 mm/min−1 until fracture occurred. The force at failure was normalized to the bond area by computer calculations, and the results were given in megapascals (MPa). All materials and methods used in this study complied with the recommendations of International Organization for Standardization (ISO).25
Failure mode evaluation
The fractured surfaces were examined using a stereomicroscope (Leica Imaging Systems Ltd., Cambridge, England) at×20 magnification. Failures were classified as adhesive, cohesive within ceramic, mixed, and cohesive within dentin.
SEM examination
The two teeth from each group were used for SEM investigations after the SBS test. Dentin specimens were dehydrated in an incubator for 2 h at 70°C. The specimens were mounted on aluminium stubs, sputter-coated with gold (BioRad-SC 502, Fison, UK), and examined with a scanning electron microscope (Jeol JSM-5200, Tokyo, Japan) at 25 kV.
Statistical analysis
Average values and their standard deviations were obtained for each group. Statistical analysis was performed using the Number Cruncher Statistical System (NCSS) 2007 and the Power Analysis and Sample Size (PASS) 2008 statistical software (Utah, USA). If the data were not normally distributed (according to the Kolmogorov–Smirnov Test), the Kruskal–Wallis test was performed, followed by the Mann–Whitney U test. All tests were performed at a 95% confidence level; a significant difference was defined as p<0.05. Failure mode distributions were analyzed as percentages.
Results
The SBS results for the eight groups are listed in Table 2. Statistically significant differences were evident among the groups, according to the Kruskal–Wallis test (p=0.009). The highest SBS was measured for Acid+Variolink II at 10.71±5.47 MPa (the control group); the lowest bond strength was in the YSGG+Variolink II group, 6.34±1.35 MPa.
Table 2.
Mean and Standard Deviation (SD) Shear Bond Strengths of the Eight Groups Tested
| MPa | |||
|---|---|---|---|
| Groups (n=10) | Mean±SD | KW | p |
| Acid+Variolink II (Control) (A+V) | 10.71±5.47 | 18,404 | 0.009** |
| YSGG+Variolink II (YSGG+V) | 6.34±1.35 | ||
| YSGG+Acid+VariolinkII (YSGG+A+V) | 8.14±1.69 | ||
| YAG+Variolink II (YAG+V) | 7.17±3.08 | ||
| YAG+Acid+Variolink II (YAG+A+V) | 8.33±3.17 | ||
| Clearfil (C) | 10.89±2.70 | ||
| YSGG+Clearfil (YSGG+C) | 6.62±1.81 | ||
| YAG+Clearfil (YAG+C) | 7.45±1.05 | ||
KW, Kruskal–Wallis test was used.
** p<0.01.
Further analysis indicated a statistically significant difference between the following groups: YSGG+V and YSGG+A+V (p=0.034), YSGG+A+V and YSGG+C (p=0.049), C and YSGG+C (p=0.002), and C and YAG+C (p=0.005), according to the Mann–Whitney U test. There were no statistically significant differences among the other groups (Table 3). The YSGG laser+A+V group showed significantly higher SBS than did the YSGG laser+V group (p<0.05). The YSGG laser+C and YAG laser+C groups demonstrated significantly lower SBS than did the C group (p<0.05).
Table 3.
Comparison of the Shear Bond Strengths Among the Groups
| Groups | Groups | Significance level |
|---|---|---|
| A+V (Control) | YSGG+V | 0.104 |
| YSGG+A+V | 0.45 | |
| YAG+V | 0.082 | |
| YAG+A+V | 0.364 | |
| C | 0.623 | |
| YSGG+V | YSGG+A+V | 0.034* |
| YAG+V | 0.762 | |
| YAG+A+V | 0.174 | |
| YSGG+C | 0.97 | |
| YSGG+A+V | YAG+V | 0.364 |
| YAG+A+V | 0.997 | |
| YSGG+C | 0.049* | |
| YAG+V | YAG+A+V | 0.29 |
| YAG+C | 0.545 | |
| C | YSGG+C | 0.002** |
| YAG+C | 0.005** | |
| YSGG+C | YAG+C | 0.112 |
| YAG+A+V | YAG+C | 0.597 |
Mann–Whitney U test was used.
* p<0.05 ** p<0.01
Boldface indicates significant differences.
Results of the fracture analysis are presented in Table 4. Cohesive-within-ceramic failure was observed in the C group. Cohesive-within-dentin failure was the most prevalent type of failure in the A+V (control) and C groups. In the YSGG+C and YAG+C groups, most fractures were adhesive and occurred between the cement and dentin surfaces.
Table 4.
Distribution (as Percentage) of Failure Mode According to Stereomicroscopic Observation
| Groups (n=10) | Adhesive | Cohesive within ceramic | Mixed | Cohesive within dentin |
|---|---|---|---|---|
| Acid+Variolink II (Control) | 20%(2) | _ | 20%(2) | 60%(6) |
| YSGG+Variolink II | 50%(5) | _ | 40%(4) | 10%(1) |
| YSGG+Acid+Variolink II | 40%(4) | _ | 10%(1) | 50%(5) |
| YAG+Variolink II | 50%(5) | _ | 30%(3) | 20%(2) |
| YAG+Acid+Variolink II | 30%(3) | _ | 20%(2) | 50%(5) |
| Clearfil | 20%(2) | 10%(1) | _ | 70%(7) |
| YSGG+Clearfil | 60%(6) | _ | 10%(1) | 30%(3) |
| YAG+Clearfil | 60%(6) | _ | 10%(1) | 30%(3) |
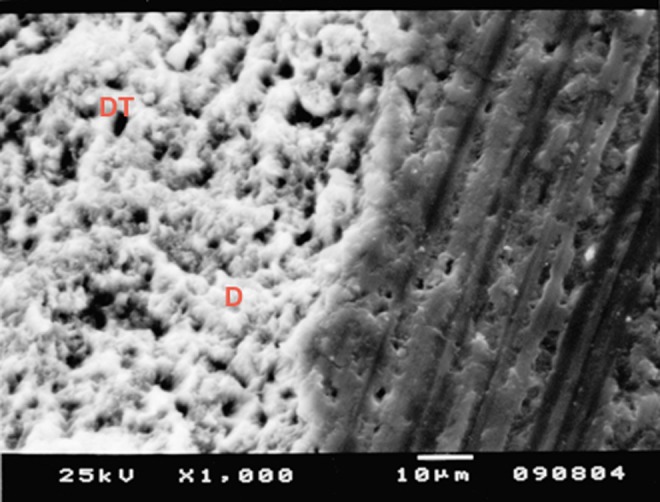
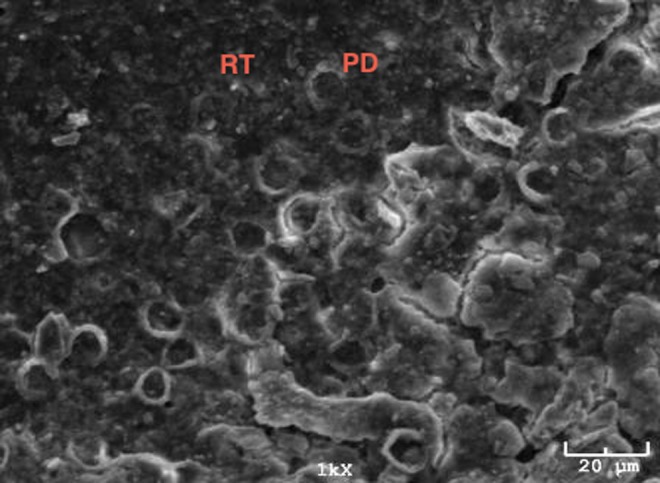
Representative SEM micrographs of the fractured dentin surfaces are shown in Figs. 2–9. The SEM image for the A+V group showed open dentinal tubules and fractured resin tags into dentinal tubules (Fig. 2). Figure 3 shows a scaly appearance or irregular surface because of microirregularities after laser irradiation in the YSGG+V group. The YSGG+A+V group showed open dentinal tubules lined with peritubular dentin and resin tags emerging from dentinal tubules (Fig. 4). Morphologically, dentin after YAG+V application has been characterized as an irregular surface with no cracking and open dentinal tubules (Fig. 5). Figure 6 shows dentinal tubules lined with peritubular dentin and infiltrated resin tags into dentinal tubules in the YAG+A+V group. When self-etch adhesive agent was applied in group C, a smear layer partially covered the surface, and dentinal tubules were not clearly visible (Fig. 7). In the YSGG+C group, SEM images showed protruding peritubular dentin and remaining components of the adhesive cement (Fig. 8). Figure 9 shows the irregular dentin surface, plugged dentin tubules, and protruding peritubular dentin in the YAG+C group.
FIG. 2.
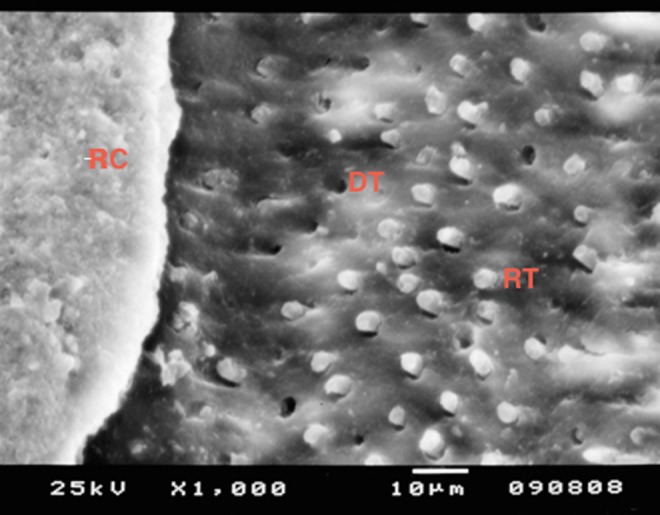
Acid+Variolink II (control) group fractured surface scanning electron micrograph (SEM) (×1000). Resin cement (RC), open dentinal tubules (DT), fractured resin tags (RT).
FIG. 3.
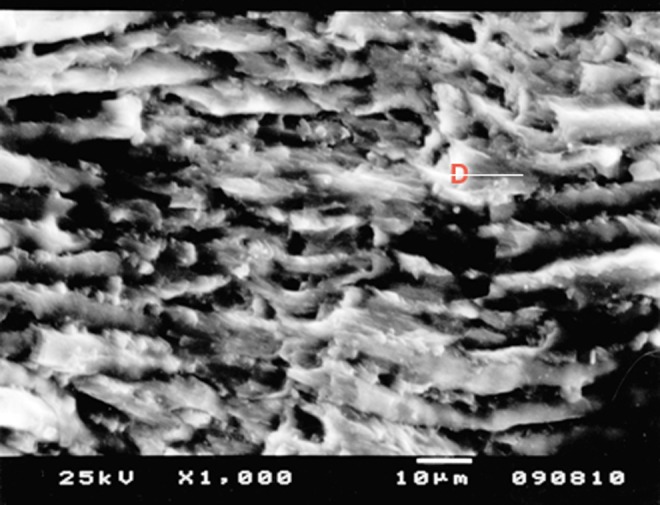
Er,Cr:YSGG+Variolink II group fractured surface scanning electron micrograph (SEM) (×1000). Scaly and irregular dentin surface (D).
FIG. 4.
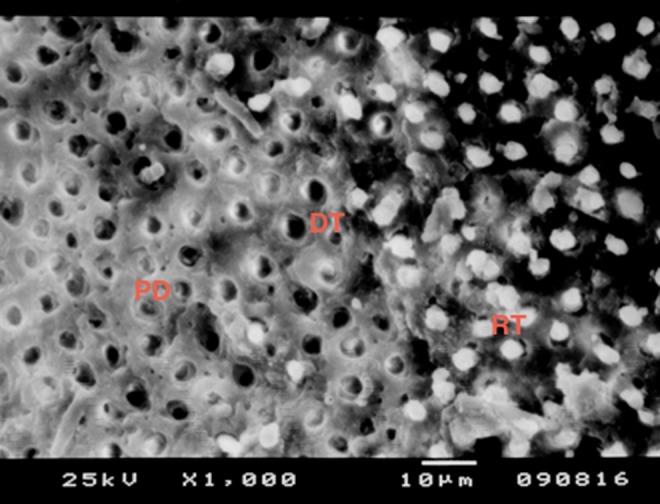
Er,Cr:YSGG+Acid+Variolink II group fractured surface scanning electron micrograph (SEM) (×1000). Open dentinal tubules (DT), peritubular dentin (PD), resin tags (RT).
FIG. 5.
Er:YAG+Variolink II group fractured surface scanning electron micrograph (SEM) (×1000). Scaly and irregular dentin surface (D), open dentinal tubules (DT).
FIG. 6.
Er:YAG+Acid+Variolink II group fractured surface scanning electron micrograph (SEM) (×1000). Peritubular dentin (PD), resin tags (RT).
FIG. 7.
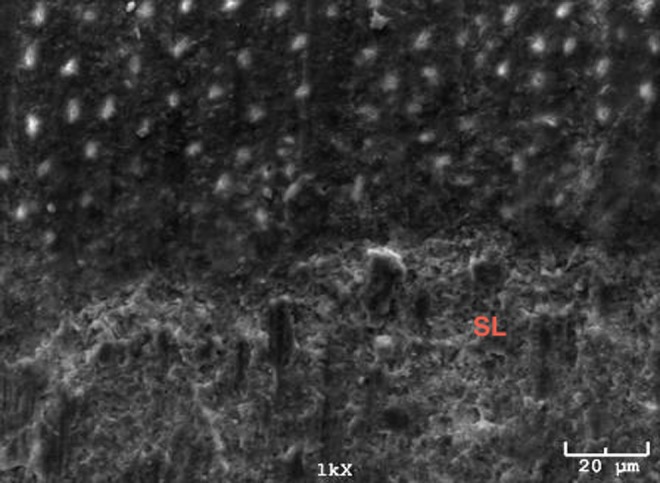
Clearfil group fractured surface scanning electron micrograph (SEM) (×1000). Smear layer (SL).
FIG. 8.
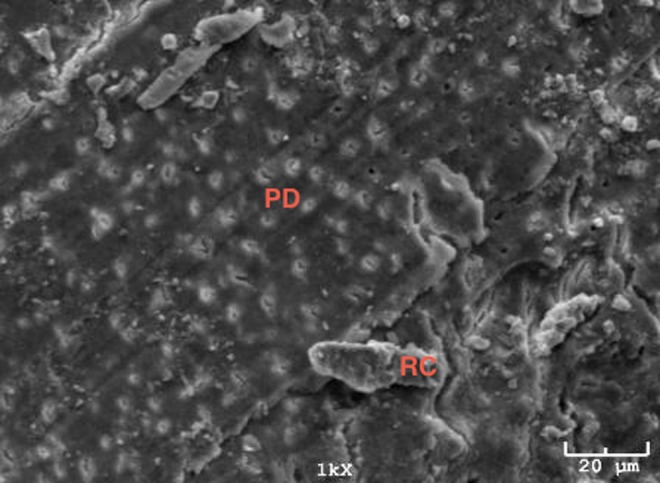
Er,Cr:YSGG+Clearfil group fractured surface scanning electron micrograph (SEM) (×1000). Peritubular dentin (PD), resin cement (RC).
FIG. 9.
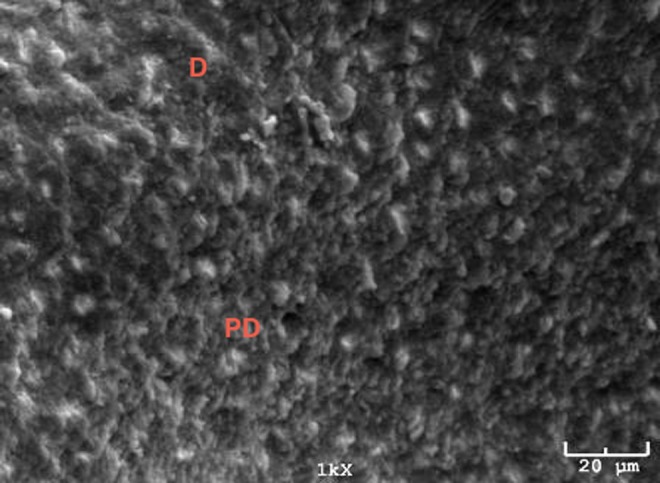
Er:YAG+Clearfil group fractured surface canning electron micrograph (SEM) (×1000). Irregular dentin surface (D), Peritubular dentin (PD).
Discussion
This in vitro study evaluated and compared two adhesive luting systems in terms of the SBS of ceramics to laser-etched and acid-etched dentin surfaces. The null hypothesis that the SBS obtained after Er,Cr:YSGG or Er:YAG laser etching of dentin was similar to that obtained after acid etching, and can be an alternative to acid etching, was accepted. The null hypothesis that there was a significant difference in the SBS to dentin etched with the Er,Cr:YSGG or Er:YAG laser in combination with acid etching versus that etched with acid alone with the adhesive resin cements tested, was rejected.
Clinical studies remain the gold standard when measuring the performance of dental materials; however, by the time useful clinical data are obtained, the materials under investigation may have become outdated.18 Nevertheless, working under variable oral conditions, such as elevated environmental temperatures, high relative humidity, and saliva contamination, can affect the results of the study.26 Therefore, laboratory testing still plays an important role in the evaluation of dental materials.
A number of factors have been related to the adhesion of ceramics to the tooth structure. Bond strengths of bonding agents used with resin cements or resin composites vary among substrates of human enamel, superficial dentin, and deep dentin.27 The preferable ceramic indirect restorations are attached to the dentin surface rather than to the enamel. To evaluate the bond strength, mid-coronal dentin surfaces were used in this study to have all tubuli oriented perpendicular with respect to the surface.
Testing methods are not well standardized, although a number of important recommendations have been made for both the substrate and testing methods. The surface area of the restorative material is an important factor in bond strength tests. As fracture strength is given per unit area, the surface area is extremely important and provides 3, 5, or 10 mm diameters.28 In this study, 8 mm diameter ceramic discs were used to measure the bond strengths.
The luting agent also can affect bonding between the ceramic and dentin. The lack of proper seating pressure during cementation may have contributed to nonstandardized cement film thicknesses, influencing the bond strength results.29 A custom-designed device, having two horizontal platforms and four vertical columns, was used in this study for the application of pure forces, to standardize the results of the ceramic film thicknesses during the cementation process; this approach was based on the study by Goracci et al.30 and ISO requirements. Specifically, in this study, a top-loaded 10 N force was applied for 10 sec during the cementation process.
The adhesion quality of dental materials to tooth tissues is generally investigated by in vitro laboratory tests; the shear and tensile tests are used most commonly.31 To evaluate the strength at the interface, tensile testing seems to be a more appropriate option, and in theory, should provide more uniform stress distributions for proper alignment between the specimen and the adherent. Nevertheless, the tensile strength test is highly sensitive, and stress distributions in such tests have been shown to be nonuniform. Small alterations in the specimen or in the stress distribution during load application have a great influence on the results.32,33 The shear bond test is one of the most commonly used bond strength tests. Shear stresses are believed to be the major stresses involved in in vivo bonding failures of restorative materials. Sano et al. developed the microtensile bond strength (μTBS) test to overcome the limitations of shear and tensile bond strength tests. The μTBS test obtains a uniform distribution of loading stresses across a smaller bonded interface, and the variations among samples are minimized.33 Nevertheless, the difficulty in the technique, the required effort, low bond strength measurement (<5 MPa), and the need for specialized equipment and samples (as well as their rapid dehydration) are disadvantages of the method.28 Therefore, to measure the bond strength, shear and macro-test evaluation were used in this study.
In the present study, high SBS was recorded for the Acid+Variolink II (control) group. Nevertheless the SBS results of Acid+Variolink II were not significantly higher than were those of the Er,Cr:YSGG+Variolink II group. This result is in accordance with the study of Usumez and Aykent, who evaluated the bonding of porcelain veneers to lased enamel surfaces; they determined that porcelain laminate veneers bonded to Er,Cr:YSGG laser-etched tooth surfaces and had a bond strength equivalent to that of orthophosphoric acid-etched tooth surfaces.10
The Er,Cr:YSGG+Acid+Variolink II group showed a significantly higher SBS than did the Er,Cr:YSGG+Variolink II group. These results are in agreement with the findings of Lee et al., who postulated that the acid-etching procedure is essential after laser ablation. That the Er,Cr:YSGG laser could not selectively remove hydroxyapatite crystallites without harmful effects on the collagen fiber network may explain this positive outcome. When the lased dentin was not additionally acid etched, the collagen fiber was not completely exposed. Therefore, the quality of the hybrid layer was not satisfactory in laser-ablated dentin.34 In contrast to this study, Cvikl et al. found the highest shear strength of the bond between dentin and ceramic for the Er,Cr:YSGG laser alone rather than for Er,Cr:YSGG laser+phosphoric acid in the Variolink II/Syntac groups, suggesting that a laser-treated dentin surface provides favorable conditions for bonding, particularly when used with the traditional multistep approach of primer–adhesive bonding. The difference in the results for the laser-treated group was explained by the usage of an irradiation angle of 60 degrees to the dentin surface and different experimental aspects (e.g., the laser setting, storage conditions for the tooth samples, and the source and preparations of the tooth discs).19
This study also compared the SBSs of specimens in the acid and Er:YAG laser-etched dentin surfaces in the Variolink II groups. The results indicated no significant difference in the SBSs among the Acid, Er:YAG, and Er:YAG+Acid groups. However, higher bond strengths were observed for the acid group, and lower bond strengths were obtained for the YAG group. The results of this study are in agreement with the works of Ceballos et al.11 and Schein et al.35 Remnant denatured collagen fibrils were fused and poorly attached to the underlying dentin substrate along the basal part of the laser-modified layer. The presence of this fused layer in which interfibrillar spaces were lacking probably restricted resin diffusion into the subsurface intertubular dentin, resulting in a lower SBS for laser-etched dentin. A substantial increase in SBS caused by the acid-etching application was observed after Er-YAG laser irradiation.11 In contrast, the results of this study are not in agreement with the findings of Visuri et al., in which it was determined that Er:YAG laser-irradiated dentin samples had improved bond strengths compared with handpiece treatments with or without a subsequent acid-conditioning step.7 These differences may be related to the different type of laser used, duration of exposure, and energy applied to the surface.
Tachibana et al. irradiated the surfaces of dentin using an Er,Cr:YSGG laser and evaluated the bond strength of a self-etching system; they observed that laser irradiation was poorest in providing a substrate for bonding with the tested self-etching system. As observed by Tachibana et al. using SEM, irradiated dentin presented opened dentinal tubules, with protruded peritubular dentin distributed on a scaly surface, free of a smear layer.36 These characteristics are considered ideal for bonding to dentin. In this case, the laser irradiation initially vaporizes the water and other hydrated organic components of the tissue. The resulting intertubular dentin was selectively preferable to the peritubular dentin that leaves protruding dentinal tubes with a cuff-like appearance because the intertubular dentin contains more water and has a lower mineral content. The morphology of the dentin surface is significant and it would be expected to have a better bond strength to irradiated dentin. Moreover, the chemical composition of the intertubular dentin is essential for bonding because this dentin is demineralized and then permeated by the hydrophilic monomers during the bonding procedure; the bonding resin can then hybridize with the network of collagen fibers.
The results of this study clearly demonstrate that self-etch adhesive-applied dentin surfaces show significantly higher bond strength than do Er,Cr:YSGG laser-irradiated and self-etch-adhesive-applied Clearfil groups, which is in agreement with the works of Tachibana et al. These results may be related to modification of the composition of the intertubular dentin by laser irradiation. This modification could produce a dentin surface more resistant to demineralization, impairing the action of the mild pH hydrophilic primer used.36
Fracture behavior is another property that defines the bonding of dentin to ceramic. The failure mode with the Acid+Variolink II (control) and Clearfil groups was mainly cohesive in dentin fracture. The YSGG+Variolink II and YAG+Variolink II specimens were predominantly adhesive failures between the ceramic and dentin (50%), and they also showed mixed and cohesive dentin failures. However, 60% of adhesive failures between ceramic and dentin were seen in the YSGG+Clearfil and YAG+Clearfil groups. These results are consistent with those reported by Al Qahtani et al.37 et al and Lee et al.34
The In-Ceram system uses a reinforcing aluminium oxide core to provide enhanced mechanical properties. Very densely stacked alumina particles lead to dispersion strengthening of the ceramic. The aesthetics and strength of In-Ceram have been increased using core materials other than aluminium oxide. For example, by substituting aluminium oxide for magnesium aluminate (MgAl2O4) spinel, the In-Ceram showed improved translucency, partly because of the crystalline nature of the spinel and a lower index of refraction versus alumina. However, the spinel-based core ceramic was not as strong as was the alumina-based material.38,39 In this study, industrially prefabricated aluminium oxide blocks (VITA In-Ceram Alumina) were used. The cohesive-within-ceramic failure mode was seen in only one specimen because of the enhanced mechanical properties of the ceramic system used. Different types of ceramics and additional ceramic surface preparation techniques may change the SBS and fracture behavior. These were not examined in this study and, therefore, can be regarded as a limitation of the study.
Lee et al. reported many protruding resin tags and the obliteration of dentinal tubules on the dentin side of debonded specimens after the bur-cut/acid-etched treatment. Lee et al. also demonstrated a scaly appearance, with dentinal tubules occluded with resin tags on the dentin side of debonded specimens after the laser-ablated/acid-etched treatment, and scaly microstructures and many dentinal tubule orifices incompletely occluded by resin tags at the dentin side of debonded specimens after the laser-ablated treatment. These results are generally consistent with the SEM results34 in the present study.
The diversity of the results from this study may be the result of various factors, including the physical parameters of the laser (type of laser, duration of exposure, and energy applied to the surface), the material used for filling the cavities (composite or ceramic), or the combination of the laser-etched surface with or without acid etching. Other limitations of this study include the lack of an in vivo environment. In vitro studies do not reflect all the variables present in a patient's mouth. Additionally, it is unclear whether the difference in SBS observed would actually translate into clinical benefit for patients. Other experimental conditions, such as different laser parameters or hand-held application of the laser irradiation (i.e., nonuniform irradiation) may change the SBS and fracture behavior. More studies should be conducted to develop new adhesive techniques or systems capable of interacting adequately with the individual characteristics of dentin. Therefore, it is desirable to develop bonding resins and procedures that produce highly uniform bond strengths to laser-etched dentin.36
Conclusions
Dentin surfaces prepared using Er-YAG and Er,Cr:YSGG lasers, with the parameters used herein, may provide comparable ceramic bond strengths, depending upon the adhesive cement used.
Acknowledgments
This study was based on the work performed by Figen Eren Giray for the fulfillment of the degree of Doctor of Philosophy, University of Marmara, Istanbul, Turkey. The study was supported by a research grant from The Marmara University Scientific Research Committee (BAPKO), with project numbers SAG-C-DRP-050608-0119 and SAG-D-110412-0085.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ritter A.V. (2001). Posterior resin-based composite restorations: clinical recommendations for optimal success. J. Esthet. Restor. Dent. 13, 88–99 [DOI] [PubMed] [Google Scholar]
- 2.Cura C., Saracoglu A., and Cötert S. (2003). Effect of different bonding agents on shear bond strength of composite-bonded porcelain to enamel. J. Prosthet. Dent. 89, 394–399 [DOI] [PubMed] [Google Scholar]
- 3.Buonocore M.G. (1955). A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J. Dent. Res. 34, 849–853 [DOI] [PubMed] [Google Scholar]
- 4.Farmakis E.T., Kozyrakis K., Kontakiotis E.G., and Nikolaos K. (2008). Effect of Er,Cr:YSGG laser on human dentin collagen: a preliminary study. J. Laser Dent. 16, 15–20 [Google Scholar]
- 5.Craig G.R., Powers J.M., and O'Brien W.J. (2006). Bonding to dental substrates. In Restoration Dental Material, 11th ed. St. Louis: The C.V. Mosby Co., p. 264 [Google Scholar]
- 6.Hibst R., and Keller U. (1989). Experimental studies of the application of the Er:YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg. Med. 9, 338–344 [DOI] [PubMed] [Google Scholar]
- 7.Visuri S.R., Gilbert J.L., Wright D.D., Wigdor H.A., and Walsh J.T., Jr (1996). Shear strength of composite bonded to Er:YAG laser-prepared dentin. J. Dent. Res. 75, 599–605 [DOI] [PubMed] [Google Scholar]
- 8.Hossain M., Nakamura Y., Yamada Y., Murakami Y., and Matsumoto K. (2002). Compositional and structural changes of human dentin following caries removal by Er,Cr:YSGG laser irradiation in primary teeth. J. Clin. Pediatr. Dent. 26, 377–382 [DOI] [PubMed] [Google Scholar]
- 9.Stiesch–Scholz M., and Hannig M. (2000). In vitro study of enamel and dentin marginal integrity of composite and compomer restorations placed in primary teeth after diamond or Er:YAG laser cavity preparation. J. Adhes. Dent. 2, 213–222 [PubMed] [Google Scholar]
- 10.Usumez A., and Aykent F. (2003). Bond strengths of porcelain laminate veneers to tooth surfaces prepared with acid and Er,Cr:YSGG laser etching. J. Prosthet. Dent. 90, 24–30 [DOI] [PubMed] [Google Scholar]
- 11.Ceballos L., Toledano M., Osorio R., Tay F.R., and Marshall G.W. (2002). Bonding to Er-YAG-laser-treated dentin. J. Dent. Res. 81, 119–122 [PubMed] [Google Scholar]
- 12.Giachetti L., Scaminaci Russo D., Scarpelli F., and Vitale M. (2004). SEM analysis of dentin treated with the Er:YAG laser: a pilot study of the consequences resulting from laser use on adhesion mechanisms. J. Clin. Laser Med. Surg. 22, 35–41 [DOI] [PubMed] [Google Scholar]
- 13.Foong J., Lee K., Nguyen C., et al. (2006). Comparison of microshear bond strengths of four self-etching bonding systems to enamel using two test methods. Aust. Dent. J. 51, 252–257 [DOI] [PubMed] [Google Scholar]
- 14.Stewart G.P., Jain P., and Hodges J. (2002). Shear bond strength of resin cements to both ceramic and dentin. J. Prosthet. Dent. 88, 277–284 [DOI] [PubMed] [Google Scholar]
- 15.Foxton R.M., Nakajima M., Hiraishi N., et al. (2003). Relationship between ceramic primer and ceramic surface pH on the bonding of dual-cure resin cement to ceramic. Dent. Mater. 19, 779–789 [DOI] [PubMed] [Google Scholar]
- 16.de Oyagüe R.C., Monticelli F., Toledano M., Osorio E., Ferrari M., and Osorio R. (2009). Influence of surface treatments and resin cement selection on bonding to densely-sintered zirconium-oxide ceramic. Dent. Mater. 25, 172–179 [DOI] [PubMed] [Google Scholar]
- 17.Akin H., Tugut F., Emine Akin G., Guney U., and Mutaf B. (2012). Effect of Er:YAG laser application on the shear bond strength and microleakage between resin cements and Y-TZP ceramics. Lasers Med. Sci. 27, 333–338 [DOI] [PubMed] [Google Scholar]
- 18.Toman M., Cal E., Türkün M., and Ertuğrul F. (2008). Bond strength of glass-ceramics on the fluorosed enamel surfaces. J. Dent. 36, 281–286 [DOI] [PubMed] [Google Scholar]
- 19.Cvikl B., Moser G., Wernisch J., Raabe M., Gruber R., and Moritz A. (2012). The impact of Er,Cr:YSGG laser on the shear strength of the bond between dentin and ceramic is dependent on the adhesive material. Lasers Med. Sci. 27, 717–722 [DOI] [PubMed] [Google Scholar]
- 20.Jaberi Ansari Z., Fekrazad R., Feizi S., Younessian F., Kalhori K.A., and Gutknecht N. (2012). The effect of an Er,Cr:YSGG laser on the micro-shear bond strength of composite to the enamel and dentin of human permanent teeth. Lasers Med. Sci. 27, 761–765 [DOI] [PubMed] [Google Scholar]
- 21.Gurgan S., Kiremitci A., Yalcin Cakir, F., Yazici E., Gorucu J., and Gutknecht N. (2009). Shear bond strength of composite bonded to erbium:yttrium-aluminum-garnet laser-prepared dentin. Lasers Med. Sci. 24, 117–122 [DOI] [PubMed] [Google Scholar]
- 22.Esteves–Oliveira M., Zezell D.M., Apel C., Turbino M.L., Aranha A.C., Eduardo, Cde P., and Gutknecht N. (2007). Bond strength of self-etching primer to bur cut, Er,Cr:YSGG and Er:YAG lased dental surfaces. Photomed. Laser. Surg. 25, 373–380 [DOI] [PubMed] [Google Scholar]
- 23.Variolink II brochure. Available at: http://www.ivoclarvivadent.com/en/products/luting-material/adhesive-luting-composite/variolink-ii (Last accessed May, 2003)
- 24.Clearfil Esthetic Cement ex brochure. Available at: http://www.kuraraydental.com/product/cements/clearfil-esthetic-cement-ex (Last accessed February2006)
- 25.Technical Specification (2003) Dental materials–Testing of adhesion to tooth structure, 2nd ed. Switzerland: ISO/TS; 11405 [Google Scholar]
- 26.Donmez N., Belli S., Pashley D.H., and Tay F.R. (2005). Ultrastructural correlates of in vivo/in vitro bond degradation in self-etch adhesives. J. Dent. Res. 84, 355–359 [DOI] [PubMed] [Google Scholar]
- 27.Powers J.M., O'Keefe K.L., and Pinzon L.M. (2003). Factors affecting in vitro bond strength of bonding agents to human dentin. Odontology 91, 1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pashley D.H., Sano H., Ciucchi B., Yoshiyama M., and Carvalho R.M. (1995). Adhesion testing of dentin bonding agents: a review. Dent. Mater. 11, 117–125 [DOI] [PubMed] [Google Scholar]
- 29.Chaves C.de A., de Melo R.M., Passos S.P., Camargo F.P., Bottino M.A., and Balducci I. (2009). Bond strength durability of self-etching adhesives and resin cements to dentin. J. Appl. Oral Sci. 17, 155–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goracci C., Cury A.H., Cantoro A., Papacchini F., Tay F.R., and Ferrari M. (2006). Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J. Adhes. Dent. 8, 327–335 [PubMed] [Google Scholar]
- 31.al-Salehi S.K., and Burke F.J. (1997). Methods used in dentin bonding tests: an analysis of 50 investigations on bond strength. Quintessence Int. 28, 717–723 [PubMed] [Google Scholar]
- 32.Cardoso P.E., Braga R.R., and Carrilho M.R. (1998). Evaluation of micro-tensile, shear and tensile tests determining the bond strength of three adhesive systems. Dent. Mater. 14, 394–398 [DOI] [PubMed] [Google Scholar]
- 33.Sano H., Shono T., Sonoda H., et al. (1994). Relationship between surface area for adhesion and tensile bond strength–Evaluation of a micro-tensile bond test. Dent. Mater. 10, 236–240 [DOI] [PubMed] [Google Scholar]
- 34.Lee B.S., Lin P.Y., Chen M.H., et al. (2007). Tensile bond strength of Er,Cr:YSGG laser-irradiated human dentin and analysis of dentin-resin interface. Dent. Mater. 23, 570–578 [DOI] [PubMed] [Google Scholar]
- 35.Schein M.T., Bocangel J.S., Nogueira G.E., and Schein P.A. (2003). SEM evaluation of the interaction pattern between dentin and resin after cavity preparation using Er:YAG laser. J. Dent. 31, 127–135 [DOI] [PubMed] [Google Scholar]
- 36.Tachibana A., Marques M.M., Soler J.M., and Matos A.B. (2008). Erbium, chromium:yttrium scandium gallium garnet laser for caries removal: influence on bonding of a self-etching adhesive system. Lasers Med. Sci. 23, 435–441 [DOI] [PubMed] [Google Scholar]
- 37.Al Qahtani M.Q., Platt J.A., Moore B.K., and Cochran M.A. (2003). The effect on shear bond strength of rewetting dry dentin with two desensitizers. Oper. Dent. 28, 287–296 [PubMed] [Google Scholar]
- 38.Seghi R.R., and Sorensen J.A. (1995). Relative flexural strength of six new ceramic materials. Int. J. Prosthodont. 8, 239–246 [PubMed] [Google Scholar]
- 39.Hwang J.W., and Yang J.H. (2001). Fracture strength of copy-milled and conventional In-Ceram crowns. J. Oral Rehabil. 28, 678–683 [DOI] [PubMed] [Google Scholar]


