Abstract
Background
Pain control is an integral part of minor oral surgery and maxillary/mandibular nerve blocks have proved promising in achieving the same. Although intra oral techniques of maxillary nerve block are common and are widely used, there are certain inherent disadvantages and potential complications. Less commonly described in the literature, the extra oral techniques have a wide spectrum of indications as well as can be more advantageous than the intra oral approach. This prospective clinical trial is an attempt to evaluate the feasibility and the efficacy of the extra oral frontozygomatic approach to the foramen rotundum to block the maxillary nerve.
Materials and Methods
Sample size was 100 patients and the inclusion criteria were patients of ASA I or II category who needed extraction of a minimum of 4 maxillary teeth in the same quadrant in a single sitting while exclusion criteria were patients with a history of allergy to local anesthesia, medically compromised patients in whom dental extraction was contraindicated. Mean age was 71.9 years and 56 patients were males while 44 were females. Only a single quadrant (first or second) was chosen as the operative site in each patient and local anaesthesia was secured using a 21 gauge 89 mm long spinal needle with frontozygomatic angle approach and the parameters used were pain experienced during the injection, onset of subjective symptoms, time required for the peak effect (objective symptoms), pain during extraction and the duration of anesthesia. All the parameters were expressed as mean values with standard deviations.
Results
A successful anesthesia was secured in first attempt in 98 patients while in 2 patients, the procedure had to be repeated owing to the difficulty in reaching the target site. A majority of the patients i.e., 71 % scored 0–2 (no pain) on visual analogue scale (VAS) while only 2 patients experienced a moderate degree of pain. Subjective symptoms were reported in 27.24 s (mean value) and 12.93 s (mean value) in the palate and the infraorbital fossa respectively. Peak effect of anesthesia was noted in 66.7, 37.38 and 31.71 s (all values expressed as mean) in palate, infraorbital fossa and posterior superior alveolar areas respectively.
Conclusion
Although with only dental extraction as the procedure of choice, the present study has favoured the frontozygomatic angle approach for the maxillary nerve block as simple, safe, efficacious and associated with minimum and clinically mild complications.
Keywords: Frontozygomatic angle, Extra oral maxillary nerve block, Pterygopalatine fossa
Introduction
Oral surgical and dental procedures are routinely performed in an out patient setting. Regional anesthesia using nerve block is the most common method to anesthetize the area of surgery [1].
Peripheral trigeminal nerve block anesthesia to achieve pain control may be accomplished either extra or intra orally. Although the intra oral technique is routinely used, patient discomfort and potential complications associated with multiple needle pricks for multiple extractions in a single quadrant particularly in the maxilla has motivated the clinicians to employ the extra oral techniques of nerve block. Although these blocks were first described at the beginning of the 20th century, the techniques are not commonly used because they are believed to be difficult and may be associated with complications [2].
Other indications of extra oral nerve block include, the need to anesthetize the entire distribution of the maxillary nerve for extensive surgery where general anesthesia is not possible, presence of local infection, trismus, other conditions which make blocks of the more terminal branches of the maxillary nerve difficult or impossible, when control of post-operative pain after osteotomies or reduction of facial fractures is desired, and for diagnostic or therapeutic purposes as in trigeminal neuralgias.
There are various techniques outlined for rendering anesthesia of the maxillary nerve through extraoral approach and could be classified as suprazygomatic and infrazygomatic techniques [3]. The most popular approach has been via the sigmoid notch: a variant of the infrazygomatic approaches. Although more commonly used, Poore and Carney reported the possibility of penetrating either the base of skull or the orbit [3].
Suprazygomatic approach from frontozygomatic angle is among the safest of all recommended approaches to the foramen rotundum. The only complication that may be expected is damage to the blood vessels of the infratemporal fossa particularly the maxillary artery and the venous plexus which can be avoided with aspirating prior to depositing the solution [3].
The present prospective clinical trial is aimed at determining the efficacy of frontozygomatic angle approach for extra oral maxillary nerve block in patients undergoing extraction of maxillary teeth in an out patient setting.
Materials and Methods
One hundred patients of ASA I and II category with a mean age of 71.9 years reporting to the department of oral and maxillofacial surgery, PMNM Dental college and hospital, Bagalkot, Karnataka for the extraction of maxillary teeth irrespective of the indication for the extraction were included and the efficacy of extra oral maxillary nerve block using the frontozygomatic angle approach was evaluated. Local ethical committee clearance was obtained and all the patients had given a written consent. The study duration was from-April 2001 to March 2002.
The exclusion criteria were patients less than 40 years and more than 90 years of age, patients with a history of allergy to 2 % Lignocaine with 1:80,000 epinephrine. A detailed clinical case history was recorded. Inter incisal opening was measured and mandibular deviation or an existing visual disturbance if any were noted. After a thorough intra oral examination, either the 1st or the 2nd quadrant that needed a minimum of 4 teeth to be extracted was chosen as the operative site in a single sitting.
Facial skin preparation with Nirlon (Cetrimide 0.6 % and Chlorhexidine Gluconate solution 0.3 %) and Ramidine solution (Povidone Iodine 5 % solution) followed by standard draping procedure was carried out. A 21 gauge 89 mm long spinal needle with a rubber stopper at 50 mm mark from the needle tip was used fitted to a 5 ml disposable syringe. Three ml of 2 % Lignocaine with 1:80,000 epinephrine was used for a single block (Figs. 1–5).
Fig. 2.
Point of entry of the needle
Fig. 3.

Needle at the skin projection of frontozygomatic angle
Fig. 4.

Needle inserted till the rubber stopper contacts facial skin
Fig. 1.
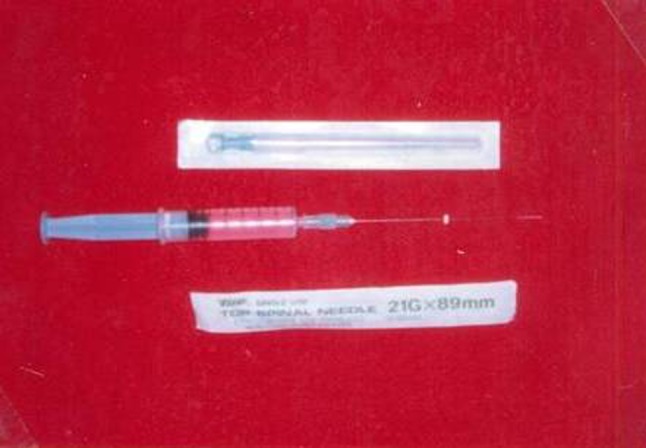
Spinal needle (21G × 89 mm)
Fig. 5.

Final position of the needle
The needle entry point was situated at the skin projection of the frontozygomatic angle—at the angle formed by the superior edge of the zygomatic arch below and the posterior orbital rim forward to the skin and advanced to reach the greater wing of sphenoid bone. This region was anesthetised with 0.5 ml of local anesthetic. The injection needle was inserted until its tip made contact with the bone. After confirming that the needle was in contact with the greater wing of sphenoid bone, it was advanced through the infratemporal fossa angulated at approximately 60° and 10° towards the sagittal and horizontal planes respectively. To avoid pain, 0.2–0.3 ml of local anesthetic was injected each time before the needle was advanced about 5–8 mm at each attempt. When the rubber marker approached the surface of the skin, patients were instructed to warn the surgeon when they felt local anaesthetic dropping in their nose or throat. This meant that the tip of the needle had reached the posterior wall of the pterygopalatine fossa and penetrated the nasal mucosa. The needle was then withdrawn for 3–5 mm to avoid intranasal injection and after careful aspiration in at least 2 different planes about 30°–40° apart, the remaining drug was slowly deposited into the vicinity of the foramen rotundum where the maxillary nerve leaves the base of the skull to enter the pterygopalatine fossa.
Pain experienced during the injection of the local anesthetic was recorded on a Visual Analogue Scale (VAS) and the scale used was: 0 to 2-no pain, 3 to 5-mild pain, 6 to 8-moderate pain and 8 to 10-severe pain. The time required for the onset of anesthesia (subjective symptoms) was recorded in seconds when the patients reported a feeling of numbness in the respective anatomic area i.e., palate and the infraorbital fossa. Time needed for the onset of peak effect of anesthesia referred to as the objective symptoms was also recorded in seconds and was assessed by the operator by probing the mucosa with a blunt instrument initially after 15 min followed by once every 5 min.
Pain experienced during dental extraction was also reported by the patients on a Visual Analogue Scale and the scale used was 0 to 2-no pain, 3 to 5-mild pain, 6 to 8-moderate pain and 8 to 10-severe pain. Duration of anesthesia was assessed in hours and was recorded when the patients reported of return of the sensory function. All the parameters were subjected to statistical evaluation and a mean and standard deviation value was obtained for each.
Complications namely, hematoma, ecchymosis, visual disturbance, limitation of mouth opening or deviation of the lower jaw immediately following the injections were assessed.
Results and Observations
Demographically, the mean age of the sample was 71.9 years and 56 patients were males while 44 patients were females. In 46 of the total sample size, maxillary left quadrant was the operative site and thus a left maxillary nerve block was administered, while in 54 patients right maxillary nerve block was administered. In all, a successful local anesthesia was secured in 98 patients in first attempt while in 2 patients the nerve block procedure had to be repeated.
The study parameters included were pain during the administration of local anesthesia evaluated as per visual analogue scale, onset of anesthesia in accordance with the subjective feeling of the same in seconds, objective evaluation of symptoms termed as peak effect, pain during extraction as per VAS and duration of anesthesia assessed in hours. All the parameters were statistically evaluated and a mean value along with standard deviation was obtained.
As seen in Table 1, 71 patients did not experience pain during the administration of the anesthetic [VAS score 0–2 (no pain)]. Twenty-seven patients scored 4 (mild pain) and 2 patients experienced a moderate pain (score 7). None of the patients complained of severe pain. The mean pain score was calculated as 1.31.
Table 1.
Pain scores during injection of local anesthetic solution (VAS)
| Pain score (visual analogue scale) during injection | No. of patients (%) |
|---|---|
| 0–2 (no pain) | 71 (71 %) |
| 3–5 (mild pain) | 27 (27 %) |
| 6–8 (moderate pain) | 02 (02 %) |
| 8–10 (severe pain) | 00 (00 %) |
| Mean | 1.31 |
| SD | 0.51 |
Onset of anesthesia evaluated in seconds varied according to the anatomic site. In the palate, in 18 patients, the onset of anesthesia was noted in less than 20 s, in 28 patients it was within 21–25 s, while in 26 patients, the time duration was between 26–30 s. In the remaining 28 patients, the subjective symptoms occurred in 31–35 s as depicted in Table 2. Calculated mean value was 27.24 s and the standard deviation was 5.94. In the infraorbital fossa, 9 patients reported subjective symptoms in less than 10 s, 31 patients within 10–12 s, 48 patients within 13–15 s while more than 15 s were needed for the onset of subjective symptoms in 12 patients with an over all mean value of 12.93 s with a standard deviation of 2.58 Table 2.
Table 2.
Onset of anesthesia (subjective symptoms) (seconds)
| Palate (time in seconds) | No. of Patients (%) | Infraorbital fossa (time in seconds) | No. of patients (%) |
|---|---|---|---|
| <20 | 18 (18 %) | <10 | 09 (09 %) |
| 21–25 | 28 (28 %) | 10–12 | 31 (31 %) |
| 26–30 | 26 (26 %) | 13–15 | 48 (48 %) |
| 31–35 | 28 (28 %) | >15 | 12 (12 %) |
| Mean | 27.24 | 12.93 | |
| SD | 5.94 | 2.58 |
The peak effect of anesthesia has been denoted in Table 3 and the time duration varied according to the anatomic site. In the palate, 38 patients needed 50–60 s. In 34 patients objective symptoms were noted within 61–70 s. In 27 patients, the time duration was 71–80 s while in 1 patient, the symptoms were noted after 80 s following the administration of local anesthetic and the mean value was 66.7 s with a standard deviation of 7.92. Overall time duration needed for the objective symptoms in the infra orbital fossa was more as against in palate. Fifty-six patients needed 30–35 s, 18 needed 36–40 s, 41–50 s were required in 26 patients with a mean value of 37.38 s and a standard deviation of 4.87.
Table 3.
Peak effect (objective symptoms) (seconds)
| Palate (time in seconds) | No. of patients (%) | Infraorbital fossa (time in seconds) | No. of patients (%) | Posterior superior alveolar region (time in seconds) | No. of patients (%) |
|---|---|---|---|---|---|
| 50–60 | 38 (38 %) | 30–35 | 56 (56 %) | 20–25 | 02 (02 %) |
| 61–70 | 34 (34 %) | 36–40 | 18 (18 %) | 26–30 | 36 (36 %) |
| 71–80 | 27 (27 %) | 41–50 | 26 (26 %) | 31–35 | 62 (62 %) |
| Above 80 | 01 (01 %) | >50 | 0 (0 %) | >35 | 00 (00 %) |
| Mean | 66.7 | 37.38 | 31.71 | ||
| SD | 7.92 | 4.87 | 2.56 |
At evaluation of objective symptoms in the posterior superior alveolar region, the following were the observations: 20–25 s in 2 patients, 26–30 s in 36 patients, 31–35 s in 62 patients. Mean value was 31.71 s.
After the local anesthesia was secured, the dental extraction was carried out in accordance with the standard procedure by a single operator in all the patients, and the operative pain was evaluated according to VAS. Eighty-nine patients scored 1 (no pain), 9 patients scored 3–5 (mild pain) while 2 patients scored 6 (moderate pain) while none of the patients experienced a severe pain. A mean value was calculated and was 1.13 with a standard deviation of 0.39 (Table 4).
Table 4.
Pain scores during extraction (VAS)
| Pain score (visual analogue scale) during extraction | No. of patients (%) |
|---|---|
| 0–2 (no pain) | 89 (89 %) |
| 3–5 (mild pain) | 09 (09 %) |
| 6–8 (moderate pain) | 02 (02 %) |
| 8–10 (severe pain) | 00 (00 %) |
| Mean | 1.13 |
| SD | 0.39 |
Table 5 shows the duration of the anesthetic effect assessed in hours and the mean value obtained was 3.83 with a standard deviation of 0.47.
Table 5.
Duration of anaesthesia (hours)
| Duration of anesthesia range (hours) | No. of patients (%) |
|---|---|
| 2.1–3 | 13 (13 %) |
| 3.1–4 | 73 (73 %) |
| 4.1–5 | 14 (14 %) |
| Mean | 3.83 |
| SD | 0.47 |
No systemic toxicity or allergic manifestations were reported in any of the patients. There was no incidence of mandibular deviation or alteration in the mouth opening. In two patients, a transient ipsilateral diplopia was noted immediately after the injection and the same subsided after 5–6 h.
Discussion
Numerous methods have been described in the literature for producing profound regional anaesthesia in the maxillary arch [4–6]. Although they probably work, each has significant drawbacks and none have gained the wide acceptance of the mandibular nerve block [4, 7]. The most commonly described intra oral route of administration for the maxillary nerve block is passing a needle down the greater palatine canal to deposit the anaesthetic solution in the vicinity of the maxillary nerve trunk at the base of that canal [4, 8]. This approach has two disadvantages., it is technically rather difficult to administer because the needle must pass down the long axis and to the base of a narrow canal. It is also extremely painful for the patient because the needle passes through a canal that contains a nerve trunk, artery and vein and the anaesthetic solution is deposited into a space that has very little compliance [4]. Hence extra oral technique to block the maxillary nerve, though believed to be technically difficult, has gained popularity.
With a sparse literature available, of the various extra oral techniques to approach the foramen rotundum, the frontozygomatic approach is believed to be safe and efficacious. The present study makes an attempt to evaluate the same.
In this study, the mean pain score during the administration of the local anaesthetic, was 1.31 (visual analogue scale) and thus the injection procedure can be considered as painless although 2 patients out of the total sample, experienced a moderate pain which could be attributed to their lower pain threshold.
Subjective symptoms in the region of palate were experienced in 27.24 s and in the infraorbital fossa, the mean time required for the same was 12.93 s.
The peak anaesthetic effect considered as the mean time needed for the objective symptoms of anaesthesia, was 66.7, 37.38, and 31.71 s in palate, infraorbital fossa and the posterior superior alveolar region respectively. The variations in the time duration could be attributable to the varying distances of the respective anatomic sites from the point where the anesthetic solution was deposited.
A majority of the patients (89 %) reported no pain during the dental extraction thus favouring the efficacy of the frontozygomatic angle approach. Nine patients experienced a mild pain and 2 patients in whom the nerve block had to be repeated owing to failure in the first attempt, scored 3 on VAS (moderate pain). Malcie Mesnil et al. evaluated the efficacy of bilateral maxillary nerve block using a suprazygomatic approach with pain relief and consumption of rescue analgesics as the parameters. Thirty-three children with a mean age of 5 ± 1.8 months were scheduled for cleft palate repair under general anaesthesia and the local anaesthetic was administered after intubation and prior to surgery. Authors observed that none of the patients needed morphine post-operatively and that there was an early resumption to oral feeds. The nerve block technique was found to be effective, simple and safe with no incidence of technical failure [9]. Fifty ultrasound guided suprazygomatic maxillary nerve blocks were performed in 25 children scheduled to undergo cleft palate repair and Chrystelle Sola et al. reported that the median pain scores and the consumption of nalbuphine were low during the study period while no complications related to the maxillary blocks were reported. The technique was favoured owing to a very low technical failure rate, and a good clinical success rate [10].
Stajcic and Todorovic [2] described the suprazygomatic approach to the foramen rotundum and stated that the approach to the pterygopalatine fossa from the frontozygomatic angle is among the safest of all other recommended techniques without any risk of penetrating the base of skull or the orbit.
The duration of anaesthesia was recorded as 3.83 h, which is considerably higher as against intra oral approach.
As against the infrazygomatic approach the suprazygomatic does not pose the risk of damaging the maxillary artery since the vessel lies ventrally and inferiorly to the maxillary nerve [3, 9] and also there is no risk of ocular injury [2, 12]. Even if any blood vessel is injured, the collected blood is limited since the infratemporal fossa is filled with temporalis muscle and it does not need any treatment apart from antibiotic cover [2].
Safety of the block could be increased by using a nerve stimulator which could stimulate the temporalis muscle. The pterygopalatine fossa is situated just behind the muscle: and disappearance of the muscular response to direct stimulation with the block needle indicates that its tip is in the infratemporal fossa [9].
It is often stated that a deep location of the maxillary nerve trunk at the foramen rotundum makes the regional block using extra oral technique more difficult [2, 11, 13]. In our study in 2 patients, a second attempt was needed while successful anaesthesia was secured in 98 patients in 1st attempt. It could be due to the possible skull variation that is the presence of an enlarged infratemporal tubercle (spinous process) or a relatively narrow entrance to the pterygopalatine fossa (pterygomaxillary fissure) (<2 mm) which may contribute to the difficulty in reaching the injection site [2] and the same was observed by Stajcic et al. [12].
In 85 dried human skulls Stajcic et al. noted that the median volume of the pterygopalatine fossa was 0.7 cm3, width was 5 mm, height was 18 mm and depth was 13 mm respectively. Though slight variations were there between the left and right sides, but the differences were statistically insignificant [12]. The authors also investigated the possible anatomic barriers that could interfere with the execution of the nerve block and stated that if the width of the pterygomaxillary fissure is less than 2 mm, the tip of the needle is prevented from entering the pterygopalatine fossa. Similarly an enlarged sphenoidal spine obstructs the entrance to the pterygomaxillary fissure. On the contrary, even if the width is more than 2 mm or if the sphenoidal spine is not obstructing, difficulty could still be faced due to the variable location of the sphenopalatine foramen in the medial wall of the fossa [12].
But the authors in this experimental study inferred that it is not necessary to reach the sphenopalatine foramen before injecting the maxillary nerve stump, stopping the needle along the depth of the pterygopalatine fossa (6–22 mm) seems to be sufficient for the execution of the technique [12].
Since the needle on its route to the injection site in this technique passes closely to or contacts the peripheral branches of the facial nerve, superficial temporal artery branches, maxillary artery, pterygoid venous plexus and the maxillary nerve with its pterygopalatine ganglion and the sphenopalatine blood vessels, the authors to prevent a damage to these vital structures, recommend injecting small quantities of local anaesthetic each time before the needle is advanced about 5–8 mm at each attempt [2, 12].
Ipsilateral diplopia occurred in two patients immediately after the injection but the normal vision restored within 3 h. Possible explanation could be the small size of the pterygopalatine fossa (0.7 cm3) which cannot accommodate 3 ml of local anaesthesia. The excess quantity returns to the infratemporal fossa via the pterygomaxillary fissure. Smaller quantities of the anaesthetic enters the infraorbital canal or the middle cranial fossa through the foramen rotundum which is precisely the cause of transient diplopia, sudden attack of headache or even more serious complication such as inadvertent brain stem anesthesia [12].
This prospective clinical trial proposes that frontozygomatic angle approach for maxillary nerve block is a safe and reliable technique since it provides an excellent anaesthesia in a relatively larger surgical field with a wide spectrum of indications and is associated with minimal complications which can easily be managed. Although, only dental extraction was selected as the procedure of choice in this study, the authors have made an attempt to elaborately describe the technique which could be employed for various other procedures for which further clinical trials may need to be undertaken.
References
- 1.Padhye M, Gupta S, Chandiramani G, Bali R. PSA block for maxillary molar’s anesthesia–an obsolete technique? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e39–e43. doi: 10.1016/j.tripleo.2011.04.046. [DOI] [PubMed] [Google Scholar]
- 2.Stajcic Z, Todorovic Lj. Blocks of the foramen rotundum and the oval foramen: a reappraisal of extraoral maxillary and mandibular nerve injections. Br J Oral Maxillofac Surg. 1997;35:328–333. doi: 10.1016/S0266-4356(97)90405-8. [DOI] [PubMed] [Google Scholar]
- 3.Captier G, Dadure C, Leboucq N, Sagintaah M. Anatomic study using three-dimensional computed tomographic scan measurement for truncal maxillary nerve blocks via the suprazygomatic route in infants. J Craniofac Surg. 2009;20:224–228. doi: 10.1097/SCS.0b013e318191d067. [DOI] [PubMed] [Google Scholar]
- 4.Moiseiwitsch J, Irvine T, Hill C. Clinical significance of the length of the pterygopalatine fissure in dental anesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:325–328. doi: 10.1067/moe.2001.115977. [DOI] [PubMed] [Google Scholar]
- 5.Poore TE, Carney FMT. Maxillary nerve block: a useful technique. J Oral Surg. 1973;31:749–755. [PubMed] [Google Scholar]
- 6.Broering R, Reader A, Beck M, Meyers W. Evaluation of second division nerve blocks in human maxillary anesthesia (abstract) J Endod. 1991;17:194. [Google Scholar]
- 7.Walton RE, Reader A. Local anesthesia. In: Walton RE, Torabinejad M, editors. Principles and practice of endodontics. 2. Philadelphia: WB Saunders Co; 1996. p. 105. [Google Scholar]
- 8.Loetscher C, Melton DC, Walton RE. Injection regimen for anesthesia of the maxillary first molar. J Am Dent Assoc. 1988;117:337–340. doi: 10.1016/s0002-8177(88)72020-6. [DOI] [PubMed] [Google Scholar]
- 9.Mesnil M, Dadure C, Captier G, Raux O, Rochette A, Canaud N, Sauter M, Capdevila X. A new approach for per-operative analgesia of cleft palate repair in infants: the bilateral suprazygomatic maxillary nerve block. Pediatr Anesth. 2010;20:343–349. doi: 10.1111/j.1460-9592.2010.03262.x. [DOI] [PubMed] [Google Scholar]
- 10.Sola C, Raux O, Savanth L, Macq C, Capdevila X, Dadure C Ultrasound guidance characteristics and efficiency of suprazygomatic maxillary nerve blocks in infants: a descriptive prospective study. Pediatr Anesth ISSN 1155–5645 [DOI] [PubMed]
- 11.Neill RS. Head and neck. In: Nimmo WS, Rowbothan DJ, Smith G, editors. Anaesthesia vol 2. 2. Oxford: Blackwell Scientific Publications; 1995. pp. 1524–1536. [Google Scholar]
- 12.Stajcic LS, Gacic B, Popovic N, Stajcic Z. Anatomical study of the pterygopalatine fossa pertinent to the maxillary nerve block at the foramen rotundum. Int J Oral Maxillofac Surg. 2010;39:493–496. doi: 10.1016/j.ijom.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Priman J, Etter LE. Significance of variations of the skull in blocking the maxillary nerve—an anatomical and radiological study. Anesthesiology. 1961;22:42–48. doi: 10.1097/00000542-196101000-00009. [DOI] [PubMed] [Google Scholar]



