Abstract
Central odontogenic fibroma has been defined as a benign odontogenic tumor, representing the intraosseous counterpart of a peripheral odontogenic fibroma. The odontogenic fibroma is a rare tumor. Differential diagnosis of radiolucent lesions in the molar-premolar region of mandible which involve impacted tooth may include central odontogenic fibroma, hyperplastic dental follicle, dentigerous cyst, unicystic ameloblastoma, and keratocystic odontogenic tumor. We describe an example of a small central odontogenic fibroma mimicking hyperplastic dental follicle and dentigerous cyst, resulting in uneruption of a primary tooth.
Keywords: Central odontogenic fibroma, Differential diagnosis, Hyperplastic dental follicle, Dentigerous cyst
Introduction
Central odontogenic fibroma (COF) has been defined as a benign neoplasm in the jawbones, representing the intraosseous counterpart of a peripheral odontogenic fibroma, with a slow growth resulting in painless cortical expansion [1]. Bhaskar [2] classified all enlarged dental follicles as odontogenic fibroma and concluded that it was the most common odontogenic tumor, representing 23% of all odontogenic tumors. Gardner [3] separated later the hyperplastic dental follicle (HDF) from central odontogenic fibroma, but acknowledged the difficulty in differentiating the simple odontogenic fibroma from the HDF.
Clinically, the central odontogenic fibroma could appear as an asymptomatic expansion of the buccal or lingual cortical plate [4]. Brannon et al. [4] revealed a total of 73 cases in the English-language literature. The age range of the 73 patients was 5–80 years (mean age, 37). Only three patients were in the first decade of life. There was a female predilection of 2.8:1. The mandible was the site of occurrence in 38 (52%) cases. In the maxilla the lesion appears frequently to involve the anterior region, whereas in the mandible the lesion tends to be located in the posterior area, involving the premolar and molar areas. With the exception of one case, all the lesions tended to be slow growing with progressive enlargement. The true incidence of odontogenic fibromas is difficult to determine because of the different diagnostic criteria that have been applied to the lesion over the years [4].
We describe an example of a small central odontogenic fibroma mimicking hyperplastic dental follicle and dentigerous cyst, resulting in uneruption of a primary tooth.
Case Report
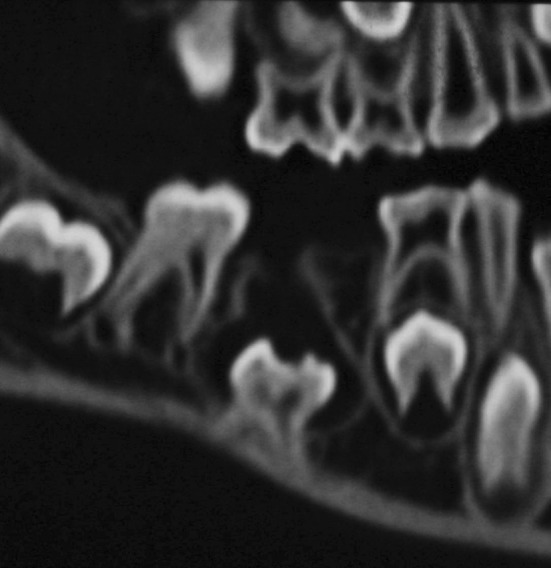
A healthy 7-year old male presented with a clinically absent right mandibular second primary molar with no history of that tooth ever being present. No swelling was noted intraorally. Radiographic examination revealed that the mandibular right second premolar was absent (Fig. 1). A well circumscribed pericoronal radiolucency with a well defined sclerotic rim surrounding the mandibular right primary second molar was also noted (Fig. 2).
Fig. 1.

Initial radiographic situation
Fig. 2.
Pericoronal radiolucency reaching the jaw ridge (CT)
Treatment consisted of enucleation of the lesion with removal of the unerupted primary second molar and the pericoronal tissue (Fig. 3) through a buccal approach. The lesion shelled out easily and completely from the surrounding bone. There was no jaw cortex perforation. The lesion was cystic and measured approximately 1.2 cm mesio-distally and 1.5 cm cranio-caudally. The excised lesion revealed a central odontogenic fibroma epithelium-rich type. Mature connective tissue containing abundant calcified deposits of dentinoid material (Figs. 4, 5) were observed, together with islands of inactive-looking odontogenic epithelium (Fig. 6). The arrows (Fig. 5) indicate the epithelial hyalinization areas (stronger pink coloration), suggestive of areas of induction.
Fig. 3.
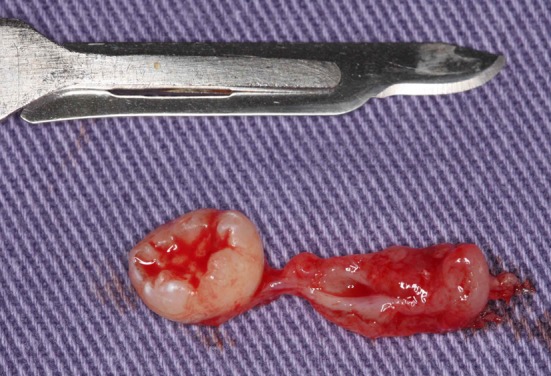
Unerupted primary second molar and the pericoronal tissue removed
Fig. 4.
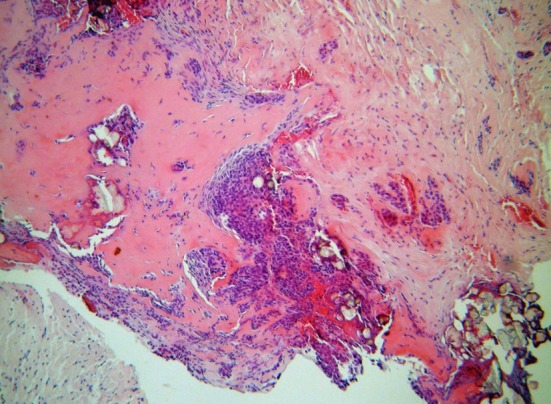
Mature connective tissue containing abundant calcified deposits of dentinoid material (hematoxylin and eosin stain, ×100)
Fig. 5.
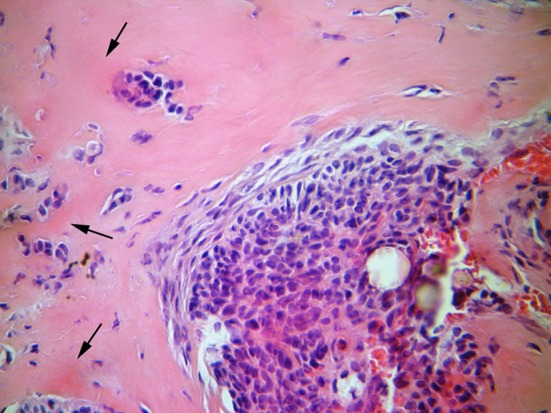
The cellular fibrous stroma and a nest of odontogenic epithelium can be seen. Foci of calcifications are in the lower right (hematoxylin and eosin stain, ×400). The arrows indicate the epithelial hyalinization areas (stronger pink coloration), suggestive of areas of induction
Fig. 6.
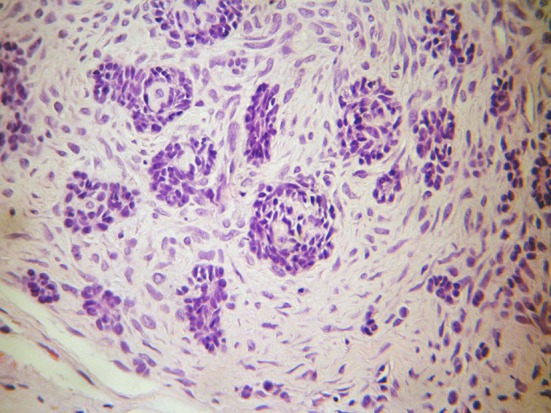
Islands of inactive-looking odontogenic epithelium (hematoxylin and eosin stain, ×400)
The patient is being followed up 9 months after the surgery without signs of recidive.
Discussion
The present case it is the fourth case of COF reported in the literature in patients in the first decade of life. The other three cases were reported by Brannon [4] in a review of 73 well-documented cases reported until the year 2004. No other additional cases in this age group have been reported so far. Therefore, the prevalence of COF in primary teeth appears to be extremely rare.
Differential diagnosis of radiolucent lesions in the molar-premolar region of mandible which involve impacted tooth may include central odontogenic fibroma, hyperplastic dental follicle, dentigerous cyst, unicystic ameloblastoma, and keratocystic odontogenic tumor. The radiographic features of COF are non-pathognomonic. This fact explains the variability in the clinical differential diagnoses submitted in our case.
Most COF appear as unilocular radiolucent lesions with well-defined borders but may manifest as multilocular lesions and in rare instances may exhibit a mixed radiolucent and radiopaque appearance. The smaller lesions are unilocular while the larger ones tend to have scalloped margins or are multilocular [5]. Unlike dental follicles, odontogenic fibromas are destructive lesions with persistent growth [1, 6]. In cases of small lesions without significant destruction of adjacent tissues as demonstrated here COF may also be associated with the crown of an unerupted tooth [5], as normally occurs with HDF [7]. In an extensive review of the literature regarding odontogenic fibromas, Kaffe and Buchner [5] found that 27% were associated with the crown of an unerupted tooth. Thus, a problem existed in assessing whether the small lesion in the present case was an enlarged dental follicle or an odontogenic fibroma. The HDF appears as a well-circumscribed radiolucency around the crown of an unerupted tooth, and its radiologic appearance is similar to that of a small dentigerous cyst [3, 8], and these clinical characteristics also raised some doubts regarding the diagnosis of the present case, as the fact that only 1 out of the 57 cases of central odontogenic fibroma, radiologically examined by Ramer et al. [9], has been reported to have features of dentigerous cyst.
The dentigerous cysts clinical features may also show some similarities with this case. It frequently occurs in the mandibular premolar region [10]. It develops around the crown of an unerupted tooth by expansion of follicle when fluid collects or a space occurs between the reduced enamel epithelium and the enamel of an impacted tooth. Radiographs show a unilocular lesion characterized by a well-defined sclerotic margin [11].
The usual clinical and radiological characteristics of the cystic ameloblastoma have some similarities to the present case. It also usually occurs in the mandibular molar area. Radiographically, the lesion is lucent with well-defined margins. It may appear at the apex of a tooth or around the crown of an impacted tooth. It is usually small, although it can reach several centimeters in size [12]. Cystic ameloblastomas have the capacity to expand or perforate jaw cortex, which was not the case. But the average age found for unilocular impaction-associated ameloblastomas was 20.8 [13] and 22 years [14], and the lowest age found in unicystic ameloblastoma associated with an impacted tooth and radiographically mimicking a dentigerous cyst was 19 years [14]. Because this patient presented at the age of 7 years, unicystic ameloblastoma was not assigned prominence.
The keratocystic odontogenic tumor is a commonly encountered developmental cyst. It is significantly more found in the mandible [15]. It appears as a well-defined lucency, but is often multilocular [12]. The radiographic features can also include the following features [15]: (1) a radiolucent mass surrounded by a radiopaque margin; (2) radiolucent areas associated with impacted or unerupted teeth, giving the radiographic impression of a dentigerous cyst or a HDF; (3) occasional resorption or displacement of teeth or roots.
It is important to microscopically differentiate the odontogenic fibroma from other odontogenic and non-odontogenic alterations. Desmoplastic fibroma is an uncommon bone tumor that has occasionally been reported as occurring in the jaws, with numerous cases involving children. In some instances distinguishing microscopically between a central odontogenic fibroma and a desmoplastic fibroma of the jaws remains an insoluble problem. Slootweg and Müller [16] state that the desmoplastic fibroma is a well-delineated entity that is characterized histologically by abundant collagen fibers separated by spindle-shaped fibroblasts with elongated or ovoid nuclei, which is in terms in contrast with the collagen fibers in the present tumor. The presence of even an occasional rest of odontogenic epithelium strongly supports the diagnosis of odontogenic fibroma but is not absolutely necessary for that diagnosis [17]. Slootweg and Müller [16] propose that every jaw fibroma is odontogenic if it does not clearly show the features of a desmoplastic fibroma. As odontogenic epithelium and dentinoid material was significantly found in the present case, a diagnosis of desmoplastic fibroma was not made. Theoretically, distinguishing between these two lesions is important because desmoplastic fibromas infiltrate surrounding tissues while odontogenic fibromas do not [17].
The odontogenic myxoma is another neoplasia that should be considered in the differential diagnosis with odontogenic fibroma. Histologically, the myxoma is bland in appearance and is composed of loosely arranged, evenly dispersed spindle-shaped, rounded, and stellate cells with a lightly eosinophilic cytoplasm in a mucoidrich (myxoid), intercellular matrix [18]. A dental follicle or odontogenic fibroma should be considered if myxomatous tissue contains islands or cords of odontogenic epithelium [19], but probably represents a residual rest rather than an integral part of the neoplasm [20], which is conclusive in the differential diagnosis between the COF.
Bhaskar [2] had erroneously regarded hyperplasic dental follicles as odontogenic fibromas and contended that these lesions are the most common odontogenic tumors. Most authors, however, try to differentiate hyperplasic dental follicles from odontogenic fibromas, which are considered to be true odontogenic tumors [1, 6].
It is generally accepted that narrow, well-circumscribed lesions around the crown of an impacted tooth, which histologically consist of fibrous or myxoid connective tissue similar to that of a dental follicle, represent hyperplastic dental follicles [17]. According to Hirshberg et al. [21], since the histologic features of COF and HDF are similar, distinction between the two lesions is based primarily on their clinical and radiologic appearances. But in the present case, the presence of dentinoid material and numerous remnants of odontogenic epithelium were more suggestive of odontogenic fibroma.
In order to find a method that may be useful as a diagnostic tool between the two lesions, Hirshberg et al. [21] evaluated the nature of collagen fibers in COF and HDF by determining the polarization colors of collagens in Picrosirius red-stained sections, which revealed a different pattern of collagen fiber colors between the two lesions.
In this case, the size of the follicular lesions and their characteristic microscopic features point to an interpretation of central odontogenic fibroma-like WHO-type lesions (epithelial-rich type). The hamartomatous versus neoplastic nature of these lesions is speculative [22]. One can assume that these lesions are not typical COF neoplasms because clinical bone expansion or perforations were not evident. However, owing to the large size of the lesions and the great displacement of the lower impacted primary second molar, and on histopathologic grounds, the lesion cannot be classified as HDF, either. Thus, we interpreted these lesions to be hamartomatous in nature.
The decision-making process for this patient was guided by a distinction among the etiologies and the treatment guidelines for various tooth-eruption disturbances. Because the teeth were not in ectopic positions, the hypothesis of a physical barrier in the eruption path seemed likely. The evaluation of the radiological exams led to the hypothesis of dentigerous cyst. After the histopathologic findings, COF became the realistic hypothesis for the alveolar cuffing of bone, the displaced teeth, and the delayed eruption by causing their impaction.
The mode of treatment of COF is enucleation. Some recurrent cases have been reported. Heimdal et al. [6] reported a case that recurred 9 years following surgery. Since then, Svirsky et al. [23] have reported a 13% (2 out of 15 cases) rate of recurrence. Jones et al. [24] reported a case, which recurred 16 months after surgery. But on the evidence of cases of recurrence it is suggested that patients who have been treated for odontogenic fibroma be followed up postoperatively to detect any recurrence.
COF is considered to be a neoplasm, and surgical therapy is usually more extensive than that required for removal of unerupted teeth and their associated follicles. Diagnostic misinterpretation can result in unnecessary surgical procedures [8].
Conclusion
The decision-making process for a patient must focus on a differential diagnosis. This case indicates the importance of strong cooperation between specialists for a better differential diagnosis and the best comprehensive treatment plan.
Contributor Information
Bruno Ramos Chrcanovic, Phone: +55-31-91625090, FAX: +55-31-32920997, Email: brunochrcanovic@hotmail.com.
Belini Freire-Maia, Phone: +55-31-99843817, FAX: +55-31-32813817, Email: belinimaia@lifecenter.com.br.
Ricardo Santiago Gomez, Phone: +55-31-34092477, FAX: +55-31-34092472, Email: rsgomez@odonto.ufmg.br.
References
- 1.Wesley RK, Wvsocki GP, Mintz SM. The central odontogenic fibroma: clinical and morphological studies. Oral Surg Oral Med Oral Pathol. 1975;40(2):235–245. doi: 10.1016/0030-4220(75)90155-3. [DOI] [PubMed] [Google Scholar]
- 2.Bhaskar SN. Synopsis of oral pathology. 5. Mosby: St. Louis; 1977. p. 259. [Google Scholar]
- 3.Gardner DG. The central odontogenic fibroma: an attempt at clarification. Oral Surg Oral Med Oral Pathol. 1980;50(5):425–433. doi: 10.1016/S0030-4220(80)80011-9. [DOI] [PubMed] [Google Scholar]
- 4.Brannon RB. Central odontogenic fibroma, myxoma (odontogenic myxoma, fibromyxoma), and central odontogenic granular cell tumor. Oral Maxillofac Surg Clin N Am. 2004;16(3):359–374. doi: 10.1016/j.coms.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Kaffe I, Buchner A. Radiologic features of central odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1994;78(6):811–818. doi: 10.1016/0030-4220(94)90101-5. [DOI] [PubMed] [Google Scholar]
- 6.Heimdal A, Isacsson G, Nilsson L. Recurrent central odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1980;50(2):140–145. doi: 10.1016/0030-4220(80)90201-7. [DOI] [PubMed] [Google Scholar]
- 7.Walker LM, Wood AJ, McDonald A, Carpenter W. Unerupted mandibular second primary molar with an unusual histopathological finding: a case report. J Dent Child. 2004;71(1):77–79. [PubMed] [Google Scholar]
- 8.Kim J, Ellis GL. Dental follicular tissue; misinterpretation as odontogenic tumors. J Oral Maxillofac Surg. 1993;51(7):762–767. doi: 10.1016/S0278-2391(10)80417-3. [DOI] [PubMed] [Google Scholar]
- 9.Ramer M, Buonocore P, Krost B. Central odontogenic fibroma—report of a case and review of the literature. Period Clin Investig. 2002;24(1):27–30. [PubMed] [Google Scholar]
- 10.Tachibana T, Shimizu M, Shioda S. Clinical observation on the cysts of the jaws in childhood, especially on the follicular cysts. Jpn J Oral Maxillofac Surg. 1980;26(4):337. doi: 10.5794/jjoms.26.337. [DOI] [Google Scholar]
- 11.Daley TD, Wysocki GP. The small dentigerous cyst. A diagnostic dilemma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79(1):77–81. doi: 10.1016/S1079-2104(05)80078-2. [DOI] [PubMed] [Google Scholar]
- 12.Regezi JA. Odontogenic cysts, odontogenic tumors, fibroosseous, and giant cell lesions of the jaws. Mod Pathol. 2002;15(3):331–341. doi: 10.1038/modpathol.3880527. [DOI] [PubMed] [Google Scholar]
- 13.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Oral Oncol Eur J Cancer B Oral Oncol. 1995;31B(2):86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 14.Eversole LR, Leider AS, Strub D. Radiographic characteristics of cystogenic ameloblastoma. Oral Surg Oral Med Oral Pathol. 1984;57(5):572–577. doi: 10.1016/0030-4220(84)90320-7. [DOI] [PubMed] [Google Scholar]
- 15.Chow HT. Odontogenic keratocyst: a clinical experience in Singapore. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86(5):573–577. doi: 10.1016/S1079-2104(98)90348-1. [DOI] [PubMed] [Google Scholar]
- 16.Slootweg PJ, Müller H. Central fibroma of the jaw, odontogenic or desmoplastic: a report of five cases with reference to differential diagnosis. Oral Surg Oral Med Oral Pathol. 1983;56(1):61–70. doi: 10.1016/0030-4220(83)90057-9. [DOI] [PubMed] [Google Scholar]
- 17.Gardner DG. Central odontogenic fibroma current concepts. J Oral Pathol Med. 1996;25(10):556–561. doi: 10.1111/j.1600-0714.1996.tb01731.x. [DOI] [PubMed] [Google Scholar]
- 18.Halfpenny W, Verey A, Bardsley V. Myxoma of the mandibular condyle: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(3):348–353. doi: 10.1067/moe.2000.107364. [DOI] [PubMed] [Google Scholar]
- 19.Slater LJ, Woo SB. Pathology of the oral cavity, oropharynx, and odontogenic lesions. In: Fu YS, Wenig BM, Abemayor E, Wenig BL, editors. Head and neck pathology with clinical correlations. New York: Churchill Livingstone; 2001. pp. 508–574. [Google Scholar]
- 20.Barker BF. Odontogenic myxoma. Semin Diagn Pathol. 1999;16(4):297–301. [PubMed] [Google Scholar]
- 21.Hirshberg A, Buchner A, Dayan D. The central odontogenic fibroma and the hyperplastic dental follicle: study with Picrosirius red and polarizing microscopy. J Oral Pathol Med. 1996;25(3):125–127. doi: 10.1111/j.1600-0714.1996.tb00206.x. [DOI] [PubMed] [Google Scholar]
- 22.Raubenheimer EJ, Noffke CE. Central odontogenic fibromae like tumours, hypodontia, and enamel dysplasia: review of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(1):74–77. doi: 10.1067/moe.2002.124862. [DOI] [PubMed] [Google Scholar]
- 23.Svirsky JA, Abbey LM, Kaugars GE. A clinical review of central odontogenic fibroma: with addition of 3 new cases. J Oral Med. 1986;41(1):51–54. [PubMed] [Google Scholar]
- 24.Jones GM, Eveson JW, Shepherd JP. Central odontogenic fibroma. A report of two controversial cases illustrating diagnostic dilemmas. Br J Oral Maxillofac Surg. 1989;27(5):406–411. doi: 10.1016/0266-4356(89)90081-8. [DOI] [PubMed] [Google Scholar]


