Abstract
Lipomas are among the most common benign tumors affecting the human body. However, they are relatively uncommon in the oral cavity. Oral lipomas are likely to affect cheek, tongue, lips, gingiva and rarely the floor of the mouth. We report a case of huge lipoma of the floor of the mouth, associated with difficulty in speech and mastication in a 72-year-old male. The tumor was completely excised and sent for histopathological examination, which confirmed the tumor to be a simple classical lipoma.
Keywords: Lipoma, Oral cavity, Floor of the mouth
Introduction
Lipoma is rarely seen in the oral cavity, but when it exists, it presents as a well defined, slow growing, painless mass with a consistency varying from soft to firm [1–3]. The incidence of oral lipomas is approximately 1.0–4.4% of all benign oral lesions [4, 5]. Oral lipomas occur at various sites including the major salivary glands, buccal mucosa, lip, tongue, palate, vestibule and floor of mouth [6]. Histologically they can be classified as simple lipomas or its variants [7]. They are either encapsulated or non encapsulated or present in an infiltrating manner [8]. Oral lipomas are usually asymptomatic and detected on routine examination. However, with continued growth they may interfere with speech and mastication.
We report a case of 72-year-old male who had inability to occlude his teeth, difficulty in speech and mastication caused by a large lipoma in the floor of the mouth.
Case Report
A 72-year-old male in good general health presented with the chief complaint of painless, slowly growing mass in the floor of the mouth of 6 months duration. He complained that the mass caused interference with speech, mastication, and movements of the tongue. He also complained having difficulty to occlude his teeth properly.
Clinical evaluation revealed a firm, non-tender mass of approximately 4 × 3 cm in size occupying the floor of the mouth completely extending posteriorly up to first molar region bilaterally and towards the base of the tongue (Fig. 1). The posterior margin was not well defined as it was extending into the substance of the tongue. The mucosa overlying the swelling was normal in colour and appearance and there were no signs of inflammation or ulceration. The salivary flow from the submandibular ducts was normal and clear.
Fig. 1.

Showing swelling in the floor of the mouth
The oral cavity was otherwise healthy except for generalized attrition of existing teeth. There was no history of any oral habits. The patient’s medical history was non- contributory and vital signs were stable. The extraoral and general examination was unremarkable without any lymphadenopathy.
Ultrasonography showed an altered echotexture lesion measuring 3.7 × 2.4 cm in the floor of the mouth without internal vascularity (Fig. 2). Computed tomography scan showed a well defined fat density lesion of 3.7 × 2.5 cm in the floor of the mouth indenting the genioglossus muscle suggestive of dermoid cyst or lipoma (Fig. 3). Fine needle aspiration yielded no fluid and was inconclusive. Based on the above findings, the provisional diagnosis of benign lesions such as lipoma or adenoma was made owing to the nature of the lesion such as size, normal overlying mucosa, nonfluctuant and slow growing nature and a lack of nodal involvement.
Fig. 2.
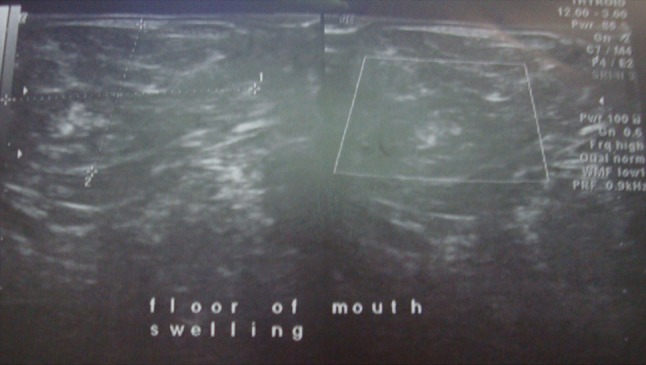
Ultrasonography showing lesion of altered echotexture
Fig. 3.

Computed tomography showing well defined fat density lesion in the floor of mouth
The surgical excision of the mass was done under general anesthesia. A midline, vertical mucosal incision was made directly over the crest of mass. The mucosa was dissected laterally to expose the superior aspect of the mass (Fig. 4). Extreme caution was taken and only blunt dissection was carried out throughout the procedure to prevent damage to the Wharton’s duct, lingual nerve, and sublingual gland. This yielded an unexpectedly soft, yellowish lobulated mass measuring 3.7 × 3.3 × 2.2 cm (Fig. 5). The classical sight of an adipose tissue coupled with a capsule surrounding its periphery reclassified our diagnosis as lipoma. The mass shelled out easily, with no adhesions to the surrounding structures. As the mass was in the submucosal plane, none of the vital structures in the floor of the mouth such as lingual nerve, sublingual gland and Wharton’s ducts were encountered during the dissection. After achieving good hemostasis the mucosal layer was closed together with absorbable sutures. Gross histopathological examination revealed round to oval matured fat cells (with peripherally placed nucleus) arranged in lobules separated by thin cords of fibers. Numerous striated muscles and few blood vessels containing lymphocytes and mast cells were evident. This was consistent with the diagnosis of a simple classical lipoma as shown (Fig. 6). Healing was uneventful. No recurrence was observed at 1 year follow-up.
Fig. 4.
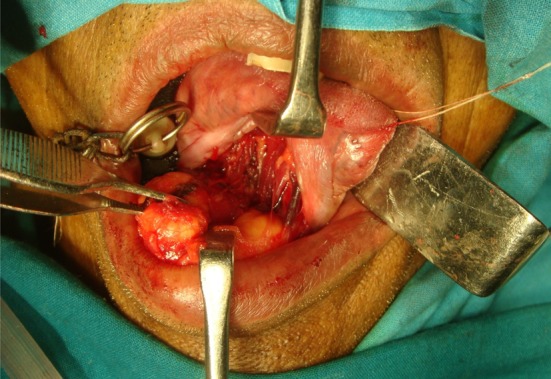
Intra-operative appearance of the yellowish lobulated mass
Fig. 5.

Excised mass
Fig. 6.
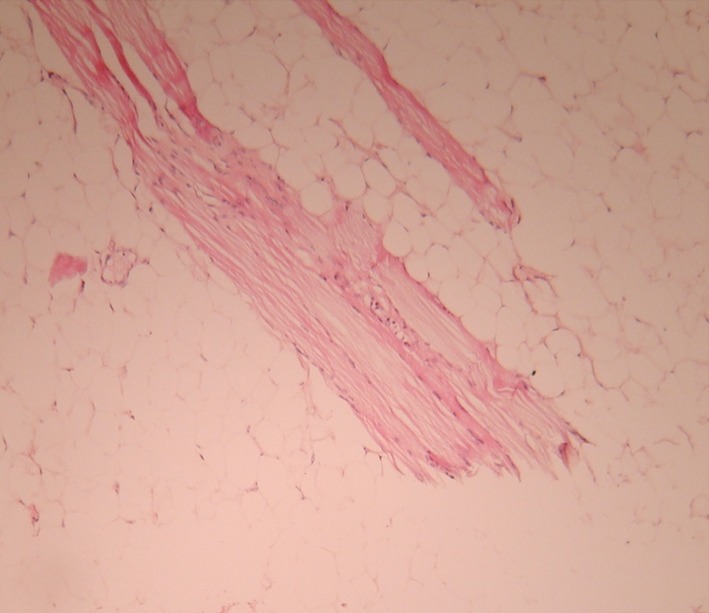
Histopathology appearance showing round to oval mature fat cells
Discussion
When a patient presents with a slow growing, painless swelling in the floor of the mouth, a variety of pathologic lesions arising from diverse sources must be considered in the differential diagnosis by the oral and maxillofacial surgeon. A complete history, followed by a thorough head and neck examination, will often narrow the differential diagnosis, and radiologic imaging can provide the surgeon with likely answers as to the possible cause. Such lesions can be broadly grouped into four categories: infectious, inflammatory, developmental and neoplastic lesions.
An infectious process is unlikely in this case because of lack of constitutional symptoms like fever and malaise, overlying mucosa was not erythematous and the lesion was non-tender. A swelling in the floor of the mouth could be secondary to obstruction of the salivary flow leading to mucocele or ranula. However, these conditions are precluded in this case because of the presence of normal salivary flow, presence of a firm, rather than a cystic or fluid filled swelling and there was negative aspiration upon fine needle aspiration cytology. Developmental conditions such as dermoid or epidermoid cyst and thyroglossal duct cyst are common in the midline of the floor of the mouth. However, these cystic lesions are unlikely in this particular case because of the negative aspiration and because of computerized tomography scan finding stating clearly fat density mass. The present swelling being a malignant lesion is very unlikely, owing to the fact that lesion was non-tender, slow growing, having normal overlying mucosa and lack of nodal involvement. Excluding the above mentioned lesions the most likely origin of this patient’s lesion falls within the benign category. This includes a lipoma or an adenoma. As the lesion was in the midline the most compatible provisional diagnosis could be lipoma.
Lipoma is a slow growing, benign tumour and intra-oral incidence vary as low as 1% to as high as 4.4% [4, 5]. Although the incidence of lipoma is higher in females than males, intra-oral lipomas show predilection for males over 40 years [6]. The cheek is the commonest site of occurrence for intra-oral lipomas followed by the tongue, vestibule, lips, gingiva and floor of the mouth [6]. As most of the intra-oral lipomas are slow growing, usually they are less than 2 cm in diameter [9]. However, lipomas of floor of the mouth may occasionally reach large size as seen in the present case and may interfere with speech, mastication and movement of tongue [9]. Although the etiology of intra-oral lipoma is not fully understood, various predisposing factors have been proposed such as trauma, hereditary, hormonal, chronic irritation and embryonic cell nest origin etc. [10].
Lipoma has a characteristic radiographic appearance. On computed tomography scan it shows a high density from 83 to 143 Hamsfield units with well or poorly defined margins depending on the capsule [11]. Ultrasonography shows a lesion which is round or elliptical in shape with intact or mostly intact capsule [12]. Most lipomas are hypoechoic with ecogenic lines or spots [11, 12].
Histopathological examination of the lesion gives the definite diagnosis. Histopathologically lipomas can be classified as (1) classical lipoma; (2) lipoma variants, such as angiolipoma, chondroid lipoma, myolipoma and spindle cell/pleomorphic lipoma, all with specific clinical and histological features; (3) hemartomatous lesions; (4) diffuse lipomatous proliferations; and (5) hibernoma [13]. In the present case, histopathologically all the features were suggestive of simple classical lipoma.
Classical lipomas are often well encapsulated as seen in the present case and it could be easily excised in toto and recurrence is unlikely [14]. The infiltrating lipomas are not encapsulated and invade easily to deeper soft tissues and recurrence after surgical excision is above 60% [15]. In the present case the tumor was indenting into the genioglossus muscle as evident in the computed tomography scan but not infiltrating into it. Rarely oral lipomas can change into liposarcoma [16]. In contrast to the present case liposarcomas lack a lobular appearance, usually occur in deeper locations and contain lipoblasts [16]. Surgical excision is the main treatment for lipoma. The complete resection should be emphasized, which is the key in avoiding recurrence. The prognosis of this tumor is good as evident in the present case. There has been no recurrence after 1 year of follow-up.
Surgical excision of lipoma in the floor of the mouth can be very challenging as the lesion may be contiguous with vital structures such as salivary glands and their ducts and lingual nerves and vessels. Manipulation or iatrogenic trauma to these structures may result in the formation of ranula, nerve injuries etc.
Nevertheless, common occurrence of ranula, sialocele and adenomas in the floor of the mouth often may lead to misdiagnosis and wrong surgical planning such as excision of submandibular or sublingual glands. Hence it is prudent to investigate further with preoperative imagings such as computed tomography scan, magnetic resonance imaging or ultrasonography to aid in proper diagnosis and surgical planning.
References
- 1.Hatziotis JC. Lipoma of the oral cavity. Oral Surg. 1971;31:511–524. doi: 10.1016/0030-4220(71)90348-3. [DOI] [PubMed] [Google Scholar]
- 2.Pindborg JJ. Atlas of diseases of the oral mucosa. 2. Copenhagen: Munksgaard; 1973. pp. 90–91. [Google Scholar]
- 3.Batsakis JG. Tumors of the head and neck. Clinical and pathological considerations. 2. London: Williams & Wilkins; 1979. pp. 60–61. [Google Scholar]
- 4.Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg. 2003;32:49–53. doi: 10.1054/ijom.2002.0317. [DOI] [PubMed] [Google Scholar]
- 5.Lombardi T, Odell EW. Spindle cell lipoma of the oral cavity: report of a case. J Oral Pathol Med. 1994;23:237–239. doi: 10.1111/j.1600-0714.1994.tb01120.x. [DOI] [PubMed] [Google Scholar]
- 6.Furlong MA, Fanburg-Smith JC, Childers EL. Lipoma of the oral and maxillofacial region: site and subclassifications of 125 cases. Oral Surg Oral Med Oral Pathol Oral Rad Endod. 2004;98:441–450. doi: 10.1016/j.tripleo.2004.02.071. [DOI] [PubMed] [Google Scholar]
- 7.Epivatianos A, Markopoulos AK, Papanayotou P. Benign tumors of adipose tissue of the oral cavity: a clinical pathologic study of 13 cases. J Oral Maxillofac Surg. 2000;58:1113–1117. doi: 10.1053/joms.2000.9568. [DOI] [PubMed] [Google Scholar]
- 8.Chidzonga MM, Mahomva L, Marimo C. Gigantic tongue lipoma: a case report. Med Oral Patol Oral Cir Bucal. 2006;11:E437–E439. [PubMed] [Google Scholar]
- 9.de Visscber JGAM. Lipomas and fibrolipomas of the oral cavity. J Maxillofac Surg. 1982;10:177–181. doi: 10.1016/S0301-0503(82)80036-2. [DOI] [PubMed] [Google Scholar]
- 10.Tan MS, Singh B. Difficulties in diagnosing lesions in the floor of the mouth—report of two rare cases. Ann Acad Med Singapore. 2004;33(Suppl 4):72S–76S. [PubMed] [Google Scholar]
- 11.de Vera Del Castillo Pardo JL, Cebrian Carrretero JL, Gomez-Garcia E. Chronic lingual ulceration caused by lipoma of the oral cavity. Med Oral. 2004;9:163–167. doi: 10.3353/omp.9.163. [DOI] [PubMed] [Google Scholar]
- 12.Zhong LP, Zhao SF, Chen GF, Ping FY. Ultrasonographic appearance of lipoma in the oral and maxillofacial region. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:738–740. doi: 10.1016/j.tripleo.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 13.Fletcher CDM, Unni KK, Mertens F (eds) (2002) Adipocytic tumors. In: Pathology and genetics: tumors of soft tissue and bone. World Health Organization Classification of tumors, IARC Press, Lyon, pp 9–46
- 14.Ayasaka N, Chino T, Jr, Chino T, Antoh M, Kawakami T. Infiltrating lipoma of the mental region: report of a case. Br J Oral Maxillofac Surg. 1993;31:388–390. doi: 10.1016/0266-4356(93)90196-4. [DOI] [PubMed] [Google Scholar]
- 15.Dionne GP, Seemayer TA. Infiltrating lipomas and angiolipomas revisited. Cancer. 1974;33:732–738. doi: 10.1002/1097-0142(197403)33:3<732::AID-CNCR2820330319>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 16.Darling M, Thompson I, Schneider J. Spindle cell lipoma of the alveolar mucosa: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:171–173. doi: 10.1067/moe.2002.120520. [DOI] [PubMed] [Google Scholar]


