Abstract
Aim
The objective of this retrospective cohort study was to compare the amount of marginal bone loss (MBL) in a bone-level and a soft-tissue-level implant system, both of which have similar intra-bony shape and surface composition. A subgroup analysis was done to compare the amount of MBL of each implant type in relation to the different vertical placement within the respective groups of implants.
Materials and Methods
Records of all patients who underwent implantation for replacement of teeth using comparable bone level (BL) and soft tissue level implants (TE) from 1st January 2006 to 31st December 2009 were scrutinized. Initial depth of implant placement (IDIP) was measured for all implants. Marginal bone loss was measured in patients whose records were available at time point corresponding to 12, 24 and 36 months post insertion.
Results
Out of a total of 384 implants, 337 implants were included for study. The mean MBL for the BL implants were 0.3, 0.38, 0.48 and for TE implant were 0.6, 0.54 and 0.93 for time periods 12, 24 and 36 months respectively. Although there was no statistically significant difference between the two groups at time periods at 6–12 months, in later time periods, there was a slightly greater amount of MBL around TE implants as compared to BL implants (p < 0.001). When comparing the IDIP and MBL in the same implant type, there was a statistically significant (p < 0.001) positive correlation between the depth of implant placement and the amount of MBL, with deeper placed implants having more bone loss.
Conclusion
Within the limitations of this retrospective cohort study design, one can conclude that BL implants had statistically significant lesser MBL as compared to TE in time periods above 12 months. Although the difference is statistically significant, the difference may not be clinically significant. The IDIP had an influence on the amount of MBL, with deeper placed implants and screw structure of the implant placed below the bone, having more MBL in the period of study.
Keywords: Marginal bone level, Bone loss, Retrospective clinical study, Bone level implant, Tissue level implant, Implant depth
Introduction
Maintenance of bony support around implants is of prime importance for successful outcome following implantation. From the 1980s, among the various criteria to assess implant success, amount of marginal bone loss over a period of time was an important factor [1]. Moreover the marginal bone reactions are very important in replacement of teeth in esthetic areas like maxillary anterior teeth in patients with a high lip line. Although the exact etiology of crestal bone changes around dental implants is not yet completely understood, many factors have been stated to influence this phenomenon [2, 3]. Among this, some of the important criteria were the type of implant (1 piece vs. 2 piece), the type of abutment (platform switch or matching platform—i.e. with or without a horizontal offset), the location of the implant–abutment junction (IAJ) in relation to the crest of the alveolus and the stability of the IAJ [4–6].
Studies show that supracrestal position of implant placement results in significantly lesser marginal bone reactions as compared to crestally placed implants [7]. With the concept of fixed biologic width, it has been proposed that soft tissue level implants with the IAJ coronal to the crestal bone level would result in minimal marginal bone resorption [8]. However, the concept of horizontal offset (platform switching) has made it possible to place implant shoulders at the crestal bone level with predictable minimal marginal bone resorption [9–11]. Certain studies also show bone deposition on the implant shoulder when implants with horizontal offset abutments were used with the IAJ in deeper subcrestal regions [12–15].
The objective of this retrospective study was to compare the amount of marginal bone loss in a horizontally offset implant system using a bone level implant-abutment interface, with a matching platform implant system using a soft tissue level implant-abutment interface; both of which have similar characteristics in terms of the intra-bony shape and surface composition (Fig. 1). A subgroup analysis was done to relate the amount of vertical marginal bone loss in relation to the IDIP in each of the two types of implants.
Fig. 1.

The implants evaluated in the study. (Left) Tissue level TE implant, (right) Bone level BL implant
Materials and Methods
In this retrospective study, records of all patients who underwent implantation for replacement of teeth using Straumann BL implants (BL) and Straumann TE implants (TE) (Institute Straumann AG, Basel, Switzerland), from 1st January 2006 to 31st December 2009 in the Department of Maxillofacial and Plastic Surgery, University of Mainz were evaluated and scrutinized. Patient data were scrutinized for medical anamnesis, local risk factors as well as the treatment procedures followed. Age of the patient, the region of implantation, length and diameter of implant, type of implant used as well as the number and times of radiographic follow-up were all recorded.
Out of this patient data, the ones chosen for the study fulfilled the following inclusion criteria (which were noted from the patient records): patients with no medical condition that would jeopardize the implant treatment (such as uncontrolled diabetes, etc.), sound periodontal status, and adequate width of attached gingiva at the region of implant placement. All implants were placed into sockets at least after 3 months following their extraction. All surgical procedures were performed by the same surgical unit and all restorations were performed by the same prosthetic team. All personnel involved in the treatment of these cases had adequate training in advanced implantology to routinely perform these procedures. A two-staged technique was used for the installation of both the implants.
Exclusion criteria were implants with inadequate follow-up documentation (<12 months follow-up documentation and representation in <2 time periods) and documented medical problems that were detrimental to implant survival. Patients with simultaneous bone augmentation procedures were excluded from the study. Four TE implants and two BL implants failed (the reasons for which were not clearly stated in the case sheet) and were removed and these were excluded from the study.
The intention of the data collection for the study was to form similar sub groups of patients treated with the two different implant systems in statistically sufficient numbers to enable meaningful comparisons of marginal bone loss.
The Implants
The BL implant is inserted all the way down to the bone level, as the implants rough surface extends to the top of the implant and the connection is shifted inwards with an internal connection. The abutment connection for this system consists of a mechanically locking friction fit with a 15° taper, and four internal grooves. The abutment has a horizontal offset concept. The TE implant is placed with the rough surface of the implant up to the crestal bone. It has a smooth neck part of 1.8 mm projecting above the crestal bone. This implant system also uses an internal connection, and the abutment is fixed to an internal morse taper design (with 8° taper) (Fig. 2). However, the implant and the abutments have matching platforms.
Fig. 2.
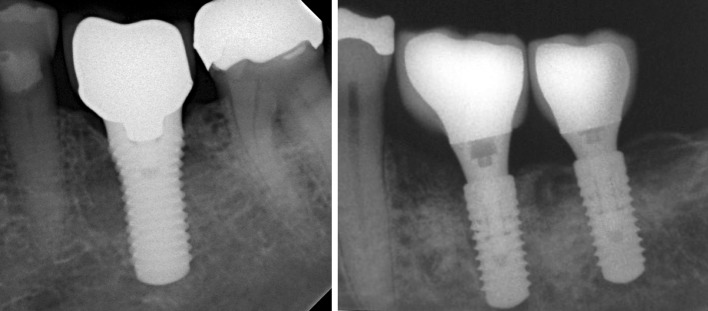
Radiographs of TE (Left) and BL (Right) implants
Surgical Procedure
After a crestal incision, full thickness flaps were elevated minimally so as to aid in proper placement of implants. Osteotomy preparations were performed with low speed- high torque drill units (800 rpm) using copious irrigation with cold saline solution. The implants had been placed as per the instructions of the manufacturers, with the BL implants intended to be screwed at flush edge to the crestal bone, whereas, the TE implants were intended to be inserted up to the level of the screws, which left a smooth neck of 1.8 mm projecting above the bone level. Primary stability was achieved in every case. Antibiotics were not routinely administered but patients were advised to rinse with chlorhexidine. NSAID analgesics were given for pain relief. All implants were loaded approximately 3 months following implant placement although no efforts were made to calculate the exact time of loading.
Marginal Bone Level Measurements
Radiographic measurements of marginal bone loss were done using panoramic x-rays following the methods described previously [16–18]. The measurements with standardized intra-oral films were not possible in this retrospective study design.
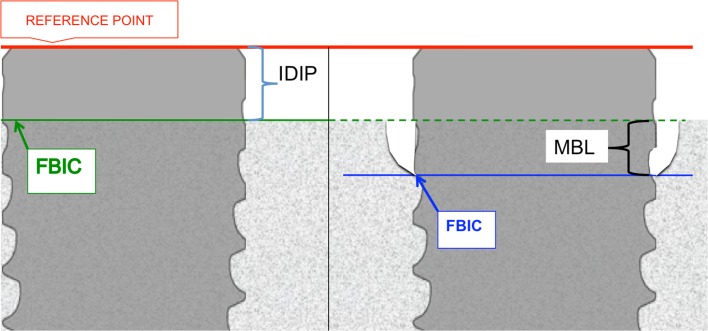
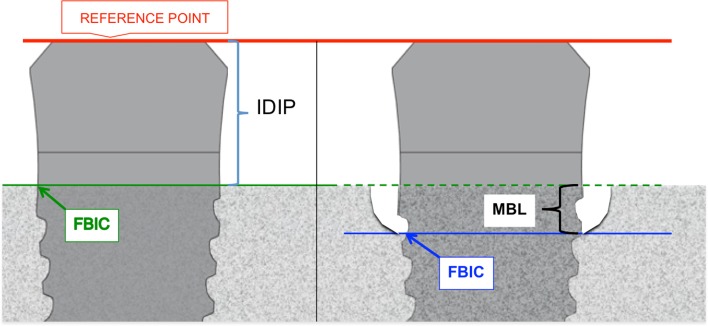
The reference points for the measurements were the implant platform (the horizontal interface between the implant and the abutment) and the first bone-implant contact (FBIC). The initial depth of implant placement (IDIP) was measured in mm using the immediate post implantation radiograph. It was calculated as the distance between the reference line and the FBIC in the immediate post implantation radiograph. Marginal bone loss (MBL) amounts were measured as the difference in the marginal bone level at the particular time of follow-up and IDIP (baseline measurement). It was measured as the difference of the distance between reference line and the FBIC and the IDIP value. This method is diagrammatically represented in Figs. 3 and 4.
Fig. 3.
Diagrammatic representation of the measurement of marginal bone level changes of BL implant. Red line denotes the reference line; Green line represents the FBIC at the time of placement and the Blue line represents the FBIC at the follow-up time period
Fig. 4.
Diagrammatic representation of the measurement of marginal bone level changes of BL implant. Red line denotes the reference line; Green line represents the FBIC at the time of placement and the Blue line represents the FBIC at the follow-up time period
The follow-up radiographs were grouped into the following based on the time period post implant insertion: 12 months (6–12 months); 24 months (13–24 months); 36 months (25–36 months); and 48 months (37–48 months) post insertion.
Panoramic x-rays were analyzed with an image analyzing software (Image J 1.4q, National Institute of Health, USA). Implant depth measurements were taken for each implant individually. The radiographic picture was magnified and the level of crestal bone was assessed and measured at the mesial and distal margins of the implant by two independent examiners. In cases of discrepancy between the two measurements the site was viewed again and the values were discussed until an agreement could be found. The bone level changes were calculated both mesially and distally, based on the baseline and the follow-up measurements. The mean average of the mesial and distal measurements of each implant at each period of time was calculated and noted as average bone loss. An algorithm for implant insertion depth and marginal bone loss at different periods of time was established based on the average values.
Statistical Analysis
To compare the MBL at the different time points within two groups, a one-way analysis of variance (ANOVA) was conducted. p values <0.001 were termed significant. In a sub-group analysis, the IDIP was correlated with the MBL values in both the implant types at the different points of time mentioned above. Here, a two-tailed Pearson correlation coefficient was calculated and p values <0.001 were termed significant. The analyses were conducted using SPSS version 15.0 (SPSS, Chicago, Il., USA).
Results
A total of 384 implants (185 BL and 192 TE) in 145 patients were placed in the time period under consideration, out of which 6 implants (2 BL and 4 TE) had failed and had to be removed. Only 337 implants (179 BL and 158 TE) inserted in 129 patients fulfilled the inclusion criteria and hence were included in the study. The year-wise break-up of the implants and patients are shown in Table 1. The distribution of implants based on the diameter and the length are provided in Table 2. The distribution of the region of implant replacement is provided in Table 3.
Table 1.
Year-wise distribution of implants (and patients in parenthesis)
| Type/year | 2009 | 2008 | 2007 | 2006 | Total |
|---|---|---|---|---|---|
| BL | 59 (18) | 74 (26) | 46 (19) | 0 (0) | 179 (63) |
| TE | 26 (8) | 21 (9) | 40 (17) | 71 (32) | 158 (66) |
| Total | 85 (26) | 95 (35) | 86 (36) | 71 (32) | 337 (129) |
Table 2.
Distribution of implants based on the (a) diameter, (b) length
| (a) Diameter (mm) | |||
|---|---|---|---|
| 3.3 | 4.1 | 4.8 | |
| Number of implants | |||
| BL | 80 | 92 | 7 |
| TE | 34 | 105 | 19 |
| Total | 114 | 197 | 26 |
| (b) Length (mm) | ||||
|---|---|---|---|---|
| 8 | 10 | 12 | 14 | |
| Number of implants | ||||
| BL | 5 | 69 | 100 | 5 |
| TE | 6 | 65 | 84 | 3 |
| Total | 11 | 134 | 184 | 8 |
Table 3.
Distribution of the region of implant placement
| Region | |||
|---|---|---|---|
| Frontal | Premolar | Molar | |
| Maxillary | |||
| Number of implants | |||
| BL | 30 | 41 | 18 |
| TE | 19 | 45 | 33 |
| Mandibular | |||
| Number of implants | |||
| BL | 41 | 27 | 22 |
| TE | 10 | 16 | 35 |
| Total | 100 | 129 | 108 |
Table 4 enumerates the number of implants and patients that were evaluated at each time period of follow-up. The number of radiographs assessed are equal to the number of patients at each point of time as each patient underwent a single OPG at the particular time of follow-up.
Table 4.
Number of implants (and the number of patients) evaluated at each time point of the study
| Initial placement | Time period: 6–12 months | Time period: 13–24 months | Time period: 25–36 months | Time period: 37–48 months | Total | |
|---|---|---|---|---|---|---|
| BL | 179 (63) | 77 (42) | 132 (51) | 56 (30) | 15 (6) | 459 (192) |
| TE | 158 (66) | 79 (44) | 89 (48) | 43 (26) | 41 (19) | 410 (203) |
| Total | 337 (129) | 156 (86) | 221 (99) | 99 (56) | 56 (25) | 869 (395) |
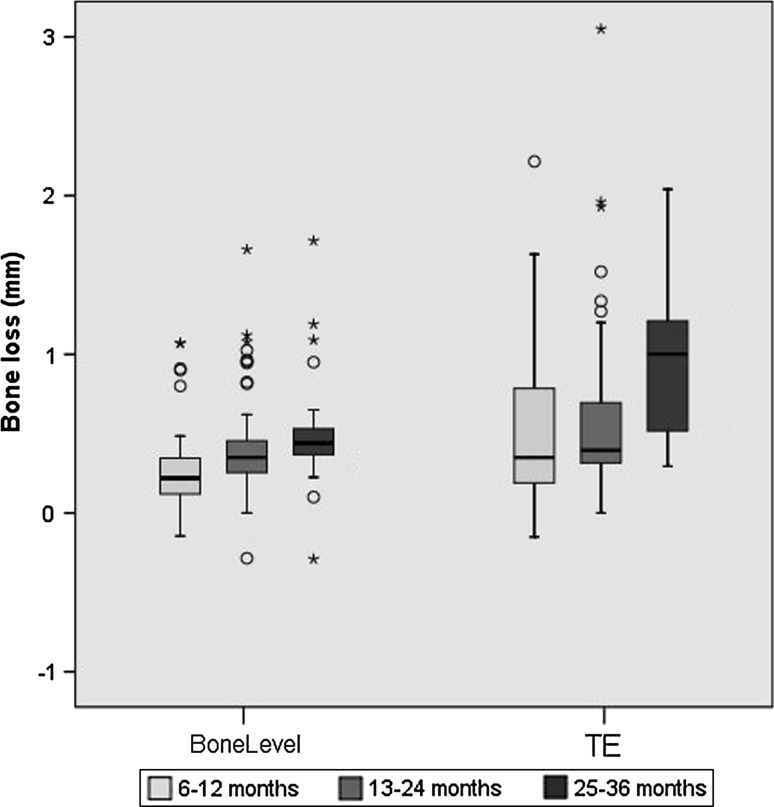
The values of marginal bone loss (MBL) in the different time groups of follow-up: 1 year (6–12 months); 2 years (13–24 months); 3 years (25–36 months) and 4 years (37–48 months) are presented in Table 5 and Fig. 5. Table 5 also provides the number of implants evaluated at each time period (mentioned in parenthesis). Statistical significant differences are marked with an asterisk.
Table 5.
The mean values of average marginal bone loss in the different time groups of follow up subdivided into types of implants
| Follow-up groups | Bone loss mean in mm; (number of implants) | ||||
|---|---|---|---|---|---|
| BL | TE | BL SD | TE SD | p value | |
| 6–12 | 0.3 (77) | 0.61 (79) | 0.431 | 1.13 | 0.28 |
| 13–24 | 0.38 (132) | 0.54 (89) | 0.233 | 0.462 | 0.001* |
| 25–36 | 0.48 (56) | 0.93 (43) | 0.269 | 0.420 | <0.0001* |
| 37–48 | 0.33 (15) | 1.11 (41) | 0.098 | 0.748 | <0.0001* |
Standard deviations (SD) and respective p values are given. The number placed in parenthesis are the number of implants that were evaluated at each time point
Fig. 5.
Box plot diagram showing the amount of marginal bone loss of different implants in different time periods
When comparing the two groups (BL vs. TE), there was no statistically significant difference between the two groups at time periods at 6–12 and 13–24 months. However in the time period of 25–36 months, there was a slightly greater amount of marginal bone loss (MBL) around TE implants as compared to BL implants. Although this difference was statistically significant, the magnitude of the difference was not clinically relevant (<0.5 mm difference in the time group of 25–36 months).
The average initial depth of implant placement (IDIP) for both implants were as per the different concepts of the implants. The BL implants were inserted with the implant shoulder very near the crestal bone, (range: −0.71 to +0.78 mm; mean: +0.007 mm; SD 0.2); where del # as the TE implants were placed with the shoulder of the implant (above a machined collar part) 0.43 mm above crestal bone margin to 2.73 mm above crestal bone margin (mean: 1.65; SD: 0.33 mm).
Correlations between the IDIP and the MBL in both the systems at the different points of time are given in Table 5. In the BL group, there was a statistically significant positive correlation between the IDIP and MBL for time periods up to 36 months, with greater amount of marginal bone resorption at deeper placements. In the TE group, statistically significant positive correlation was found in the time group of up to 24 months (Table 6).
Table 6.
Correlation between average initial implant depth and marginal bone loss (number of implants)
| Follow-up groups | BL p value | TE p value |
|---|---|---|
| 6–12 | <0.0001 (77)* | 0.977 (79) |
| 13–24 | <0.0001 (132)* | <0.0001 (89)* |
| 25–36 | <0.0001 (56)* | 0.436 (43) |
| 37–48 | 0.814 (15) | 0.751 (41) |
Discussion
The principle of crestal bone remodelling (saucerisation) around a dental implant has been widely noted in the literature. The etiology of this bone loss can vary depending on the type of implant (one-piece vs. two-piece) and also on the type of abutment especially in case of two-piece implants. In this study, BL is a type of 2 piece implant with the IAJ at the level of crestal bone and uses a horizontal offset concept whereas, TE is a type of 2 piece implant, with the IAJ above the crestal bone, at the soft tissue level. Both the implant systems have a similar outer surface composition of the intra-bony component, and a similar intra-bony design of a cylindrical apex with a conical coronal taper. Both implant systems have a similar thread pitch. In both the subsets of patients implant surface, intra bony implant design, structure of the implant collar, timing of implant placement, timing of implant loading and mobility of the mucosa were similar. Hence this study could compare the effects of two variables in terms of implant depth from bone level and the difference of abutment design (bone level implant with horizontal offset vs. soft tissue level implant without horizontal offset) on the influence of marginal bone levels.
The results of the retrospective study showed that in both the systems there was minimal bone loss, and both systems had stable, acceptable marginal bone reactions. There was statistically significant lesser amount of marginal bone loss in BL implants as compared to TE implants, although the magnitude of the difference may not be clinically significant.
It has been observed in the literature that the use of a reduced diameter abutment connected to a wider diameter implant platform (‘horizontal offset’ or ‘platform switching’), is associated with a reduced amount of crestal bone loss in comparison to matching implant and abutment interfaces [9–11, 19, 20]. Several studies have noticed a lesser amount of marginal bone resorption associated with platform switched implants, including a recent systematic review and meta-analysis which states that platform switching can be considered a desirable morphologic feature that may prevent the horizontal saucerization and preserve the vertical crestal bone levels [2]. A prospective case series by Buser et al. [21], demonstrated much lesser marginal bone loss in single crowns in esthetic zones when bone level implant system with horizontal offset was used as early implant placement. Other clinical studies too support these findings [22, 23].
As the concept is not fully understood, there are different theories that try and explain reduced crestal bone loss in (platform switched) horizontally offset implants. The different theories are based on various factors like less stress distribution on the crestal bone [24, 25]; increasing the distance of the inflammatory infiltrate to crestal bone [11, 26, 27] and medializing the location of biologic width [19].
Analysis of our results also showed that the depth of implant placement (within the range of IDIP of our study) had a positive correlation to the amount of marginal bone loss, with deeper placed implants having slightly more bone loss than higher placed implants, when the abutment junction in BL-level implants or the rough-machined border in TE Implants is positioned below the bone level. This correlation could only be seen up to time period of 36 months (the period of the study), which clearly shows that careful longer follow-up studies would be needed. It could be opined from these findings that the marginal bony remodeling is dependent on the depth of implant placement as also noted by previous studies [7].
The initial depth of implant placement has very important clinical implications in terms of esthetics [28]. Implant placement at deeper positions for esthetic improvements would allow the use of healing caps with an emergence profile and the substitution of the prosthetic component in case of marginal tissue recession, would contribute to the maintenance of the peri-implant mucosa texture and tonality and would provide the reestablishment of the marginal tissue architecture [29, 30].
However, the marginal bone changes in relation to different vertical positions of implants have been variably reported with certain authors demonstrating greater bone loss in sub-crestal placement and certain others reporting lesser bone loss in sub-crestal positions.
Hermann and colleagues showed that when the IAJ was positioned above the crest, there was significantly less bone resorption than when it was positioned below the crest. It was also shown that the final distance of the crestal bone from the IAJ never exceeded 2 mm [4–6, 31]. Some studies [32] demonstrated that moving the IAJ supra-crestally reduces peri-implant bone loss as greater amount of inflammatory cells were seen in cases of sub-crestal implant placement. However, these studies were done on implants with matching platforms.
A more apical position of the micro-gap at the IAJ is said to be predisposed to a more anaerobic environment which could favor a more pathogenic bacterial composition that could lead to an increased amount of peri-implant inflammation [33, 34], although this exact relationship is still unclear [20].
Contradictorily, several studies have shown lesser amounts of bone resorption around implants that have been inserted much deeper. Weng et al. [12] noted (in histologic, experimental studies in dogs) lesser marginal bone loss if the implants are placed 1.5 mm sub-crestally instead of equi-crestally, with bone growth onto the implant shoulder in cases of subcrestal placement. Moreover, several histological studies have shown mineralized tissue deposits at the interface and on top of the implant surface in sub-crestally placed implants that have been loaded immediately [13–15]. The studies that showed lesser bone loss at deeper initial implant depths used two-piece implants with horizontally offset abutments when the IDIP were deeper than 1.5 mm below crestal bone level.
In our retrospective analysis, among the BL implants, the deepest implant had been placed only 0.710 mm below crestal bone margin. This may be the reason why there was more bone loss with increasing depth of placement.
A major drawback of this study was in its retrospective study design, as a result of which, the implants were not placed in a randomized manner. Another drawback was that actual clinical examinations of the patients were not performed, and inclusion criteria like ‘sound periodonal status’ and ‘adequate width of attached gingiva’ were extracted from patient records. Although the radiographic method of measurement of MBL changes from orthopantamograms that has been followed in this study is an accepted method, the data is not as accurate as measurements from standardized periapical radiographs. All the implants/subjects included in the study were not examined at every follow-up time, which is another limitation. Consequentially, the respective subjects/implants represented in each time periods were necessarily not the same and the follow-up time periods were not taken at a given point of time, but were grouped over a 1-year period. No sub group analysis was done based on the type of prosthetic rehabilitation and hence this variation was not considered on the marginal bone loss of the implants.
In spite of these drawbacks, however, within the limitations of this study design, one can conclude that both the implant systems had comparable minimal bone loss up to 36 months with BL having statistically significant lesser bone loss as compared to the TE (although the difference may not be clinically significant). Both implant concepts show high clinical success with stable marginal bone levels: either with the abutment connection away from the bone in the tissue level, or a horizontally offset abutment connection at bone level. So the choice between these implant designs should be dependent on other clinical demands such as aesthetics, crown length, emergence profile, etc. The initial depth of implant placement had an influence on the amount of marginal bone loss, with deeper placed implants having more marginal bone loss in periods up to 3 years.
Acknowledgments
The study was supported by the ITI Research Scholarship grant by the ITI-Foundation to the corresponding author.
Conflict of interest
The senior authors Prof Wagner und Prof Al-Nawas declare that they were involved in education and scientific lectures and get research grants by the Straumann company but have no conflicts of interest in this study. All other authors have no conflict of interest in the study.
Footnotes
The data from this study is part of the dissertation work submitted to Johannes Gutenberg University, Mainz as part of doctoral thesis of Dr. Vinay V. Kumar.
References
- 1.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 2.Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol. 2010;81:1350–1366. doi: 10.1902/jop.2010.100232. [DOI] [PubMed] [Google Scholar]
- 3.Jones AA, Cochran DL. Consequences of implant design. Dent Clin North Am. 2006;50:339–360. doi: 10.1016/j.cden.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Hermann JS, Buser D, Schenk RK, Schoolfield JD, Cochran DL. Biologic width around one- and two-piece titanium implants. Clin Oral Implants Res. 2001;12:559–571. doi: 10.1034/j.1600-0501.2001.120603.x. [DOI] [PubMed] [Google Scholar]
- 5.Hermann JS, Schoolfield JD, Nummikoski PV, Buser D, Schenk RK, Cochran DL. Crestal bone changes around titanium implants: a methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants. 2001;16:475–485. [PubMed] [Google Scholar]
- 6.Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001;72:1372–1383. doi: 10.1902/jop.2001.72.10.1372. [DOI] [PubMed] [Google Scholar]
- 7.Al-Nawas B, Kämmerer PW, Morbach T, Ophoven F, Wagner W. Retrospective clinical evaluation of an internal tube-in-tube dental implant after 4 years, with special emphasis on peri-implant bone resorption. Int J Oral Maxillofac Implants. 2001;26:1309–1316. [PubMed] [Google Scholar]
- 8.Hermann JS, Buser D, Schenk RK, Higginbottom FL, Cochran DL. Biologic width around titanium implants. A physiologically formed and stable dimension over time. Clin Oral Implants Res. 2000;11:1–11. doi: 10.1034/j.1600-0501.2000.011001001.x. [DOI] [PubMed] [Google Scholar]
- 9.Jung RE, Jones AA, Higginbottom FL, Wilson TG, Schoolfeild J, Buser D, Hammerle CH, Cochran DL. The influence of non matching implant and abutment diameters on radiographic crestal bone levels in dogs. J Periodontol. 2008;79:260–270. doi: 10.1902/jop.2008.070132. [DOI] [PubMed] [Google Scholar]
- 10.Enkling N, Jöhren P, Klimberg V, Bayer S, Mericske-Stern R, Jepsen S. Effect of platform switching on peri-implant bone levels: a randomized clinical trial. Clin Oral Implants Res. 2011;22:1185–1192. doi: 10.1111/j.1600-0501.2010.02090.x. [DOI] [PubMed] [Google Scholar]
- 11.Canullo L, Quaranta A, Teles RP. The microbiota associated with implants restored with platform switching: a preliminary report. J Periodontol. 2010;81:403–411. doi: 10.1902/jop.2009.090498. [DOI] [PubMed] [Google Scholar]
- 12.Weng D, Nagata MJH, Bell M, Bosco AF, de Melo LGN, Richter EJ. Influence of microgap location and configuration on the periimplant bone morphology in submerged implants. An experimental study in dogs. Clin Oral Implants Res. 2008;19:1141–1147. doi: 10.1111/j.1600-0501.2008.01564.x. [DOI] [PubMed] [Google Scholar]
- 13.Degidi M, Perrotti V, Shibli JA, Novaes AB, Piatelli A, Iezzi G. Equicrestal and subcrestal dental implants: a histologic and histomorphometric evaluation of nine retrieved human implants. J Periodontol. 2011;82:708–715. doi: 10.1902/jop.2010.100450. [DOI] [PubMed] [Google Scholar]
- 14.Novaes AB, Jr, Barros RR, Mugila VA, Borges GJ. Influence of interimplant distances and placement depth on papilla formation and crestal resorption: a clinical and radiographic study in dogs. J Oral Implantol. 2009;35:18–27. doi: 10.1563/1548-1336-35.1.18. [DOI] [PubMed] [Google Scholar]
- 15.Barros RR, Novaes AB, Jr, Mugila VA, Iezzi G, Piattelli A. Influence of interimplant distances and placement depth on peri-implant bone remodeling of adjacent and immediately loaded Morse cone connection implants: a histomorphometric study in dogs. Clin Oral Implants Res. 2010;21:371–378. doi: 10.1111/j.1600-0501.2009.01860.x. [DOI] [PubMed] [Google Scholar]
- 16.Zechner W, Watzak G, Gahleitner A, Busenlechner D, Tepper G, Watzek G. Rotational panoramic versus intraoral rectangular radiographs for evaluation of peri-implant bone loss in the anterior atrophic mandible. Int J Oral Maxillofac Implants. 2003;18:873–878. [PubMed] [Google Scholar]
- 17.Kullman L, Al-Asfour A, Zetterqvist L, Andersson L. Comparison of radiographic bone heights assessments in panoramic and intraoral radiographs of implant patients. Int J Oral Maxillofac Implants. 2007;22:96–100. [PubMed] [Google Scholar]
- 18.Al-Nawas B, Brägger U, Meijer HJ, Naert I, Persson R, Perucchi A, Quirynen A, Raghoebar GM, Reichert TE, Romeo E, Santing HJ, Schimmel M, Storelli S, Bruggenkate CT, Vandekerckhove B, Wagner W, Wismeijer D, Müller F. A double-blind randomized controlled trial (RCT) of titanium-13zirconium versus titanium Grade IV small-diameter bone level implants in edentulous mandibles—results from a 1-year observation period. Clin Implant Dent Rel Res. 2012;14:896–904. doi: 10.1111/j.1708-8208.2010.00324.x. [DOI] [PubMed] [Google Scholar]
- 19.Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling post restorative crestal bone levels. Int J Periodontics Restor Dent. 2006;2006:9–17. [PubMed] [Google Scholar]
- 20.Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Implants Res. 2010;21:115–121. doi: 10.1111/j.1600-0501.2009.01867.x. [DOI] [PubMed] [Google Scholar]
- 21.Buser D, Wittneben J, Bornstein MM, Grütter L, Chappuis V, Belser UC. Stability of contour augmentation and esthetic outcomes of implant-supported single crowns in the esthetic zone: 3-year results of a prospective study with early implant placement postextraction. J Periodontol. 2011;82:342–349. doi: 10.1902/jop.2010.100408. [DOI] [PubMed] [Google Scholar]
- 22.Wennström JL, Ekestubbe A, Gröndahl K, Karlsson S, Lindhe J. Implant-supported single-tooth restorations: a 5-year prospective study. J Clin Periodontol. 2005;32:567–574. doi: 10.1111/j.1600-051X.2005.00715.x. [DOI] [PubMed] [Google Scholar]
- 23.Chou CT, Morris HF, Ochi S, Walker L, DesRosiers D. AICRG, Part II: crestal bone loss associated with the Ankylos implant: loading to 36 months. J Oral Implantol. 2004;30:134–143. doi: 10.1563/1548-1336(2004)30<134:APICBL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Maeda Y, Miura J, Taki I, Sogo M. Biomechanical analysis on platform switching: is there any biomechanical rationale? Clin Oral Implants Res. 2007;18:581–584. doi: 10.1111/j.1600-0501.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 25.Canay S, Akca K. Biomechanical aspects of bone-level diameter shifting at implant–abutment interface. Implant Dent. 2009;18:239–248. doi: 10.1097/ID.0b013e318198ffd1. [DOI] [PubMed] [Google Scholar]
- 26.Cocchetto R, Traini T, Caddeo F, Celletti R. Evaluation of hard tissue response around wider platform-switched implants. Int J Periodontics Restor Dent. 2010;30:163–171. [PubMed] [Google Scholar]
- 27.Cappiello M, Luongo R, Di Iorio D, Bugea C, Cocchetto R, Celletti R. Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restor Dent. 2008;28:347–355. [PubMed] [Google Scholar]
- 28.Buser D, von Arx T. Surgical procedures in partially edentulous patients with ITI implants. Clin Oral Implants Res. 2000;11(Suppl 1):83–100. doi: 10.1034/j.1600-0501.2000.011S1083.x. [DOI] [PubMed] [Google Scholar]
- 29.Pontes AEF, Ribeiro FS, Iezzi G, Piattelli A, Cirelli JA, Marcantonio E. Biologic width changes around loaded implants inserted in different levels in relation to crestal bone: histometric evaluation in canine mandible. Clin Oral Implants Res. 2008;19:483–490. doi: 10.1111/j.1600-0501.2007.01506.x. [DOI] [PubMed] [Google Scholar]
- 30.Pontes AEF, Ribeiro FS, da Silva VC, Margonar R, Piattelli A, Cirelli JA, Marcantonio E. Clinical and radiographic changes around dental implants inserted in different levels in relation to the crestal bone, under different restoration protocols, in the dog model. J Periodontol. 2008;79:486–494. doi: 10.1902/jop.2008.070145. [DOI] [PubMed] [Google Scholar]
- 31.Todescan FF, Pustiglioni FE, Imbronito AV, Albrektsson T, Gioso M. Influence of the microgap in the peri-implant hard and soft tissues: a histomorphometric study in dogs. Int J Oral Maxillofac Implants. 2002;17:467–472. [PubMed] [Google Scholar]
- 32.Broggini N, McManus LM, Hermann JS, Medina R, Schenk RK, Buser D, Cochran DL. Peri-implant inflammation defined by the implant–abutment interface. J Dent Res. 2006;85:473–478. doi: 10.1177/154405910608500515. [DOI] [PubMed] [Google Scholar]
- 33.Callan DP, Cobb CM, Williams KB. DNA probe identification of bacteria colonizing internal surfaces of the implant–abutment interface: a preliminary study. J Periodontol. 2005;76:115–120. doi: 10.1902/jop.2005.76.1.115. [DOI] [PubMed] [Google Scholar]
- 34.Quirynen M, van Steenberghe D. Bacterial colonization of the internal part of the two-stage implants. An in vivo study. Clin Oral Implants Res. 1993;4:158–161. doi: 10.1034/j.1600-0501.1993.040307.x. [DOI] [PubMed] [Google Scholar]