Abstract
Falls in older adults are a major health and societal problem. It is thus imperative to develop highly effective training paradigms to reduce the likelihood of falls. Perturbation training is one such emerging paradigm known to induce shorter term fall reduction in healthy young as well as older adults. Its longer term benefits are not fully understood, however. The purpose of this study was to determine whether and to what degree older adults could retain their fall-resisting skills acquired from a single perturbation training session. Seventy-three community-dwelling older adults (≥65 years) received identical single-session perturbation training consisting of 24 slips. This was delivered through unannounced unlocking (and mixed with relocking) of low-friction movable sections of the walkway. A single retest was subsequently scheduled based on a three-stage sequential, pre-post-retest design. Outcome measurements, taken upon the first (novel) and the 24th (final) slips of the initial session and the retest slip, included fall-or-no-fall and stability (quantified by the shortest distance from relative motion state of the center-of-mass and the base-of-support to the limits of stability) at instants prior to (proactive) and after (reactive) the onset of the slip. The training boosted subjects’ resilience against laboratory-induced falls demonstrated by a significant reduction from 42.5 % falls on the first slip to 0 % on the 24th slip. Rate of falls which occurred during the laboratory retest remained low in 6-month (0 %), 9-month (8.7 %), and 12-month retest (11.5 %), with no significant difference between the three time intervals. Such reduction of laboratory-induced falls and its retention were attributable to the significant training-induced improvement in the proactive and reactive control of stability. This unique pre-post-retest design enabled us to provide scientific basis for the feasibility of a single session of perturbation training to “inoculate” older adults and to reduce their annual risk of falls in everyday living.
Keywords: Stability control, Motor memory, Resilience, Inoculation, Perturbation training
Introduction
Increasing susceptibility to falls with age (Tinetti et al. 1988) poses a health threat to older adults. Even the most healthy and active older adults are not immune to falls (Rubenstein 2006), which can cause bone fracture and have devastating consequences (Englander et al. 1996). Perturbation-related falls (i.e., from trips or slips) are responsible for about 60 % of outdoor falls among community-living adults aged 70 or older (Luukinen et al. 2000). It is therefore imperative to develop intervention paradigms that can reduce such falls among these older adults.
Humans learn at an early age how to resist falls after actually experiencing a fall (Joh and Adolph 2006). At later ages, perturbation training (an external factor that disrupts the regular falling-and-catching relations in locomotion between one’s center-of-mass (COM) and base-of-support (BOS)) can be employed to achieve similar objectives by inducing repeated slips that mimic life-threatening situations (Bhatt and Pai 2009a; Pai and Bhatt 2007). Such training can involve a destabilization process that disrupts the usual, predictable relations between one’s COM and the BOS through a sudden forward slip. The trial-and-error practice stimulates the central nervous system (CNS) to make adaptive improvements in motor behavior that can resist laboratory-induced falls (Pai and Bhatt 2007). Previous studies have demonstrated the efficacy of such training, whereby adaptation to perturbation can occur rapidly within a single training session, by shifting one’s reliance on feedback-controlled reactive responses to a significantly improved feed-forward (proactive) as well as reactive control strategy to reduce the likelihood of laboratory-induced falls (Bhatt et al. 2006b; Pai et al. 2010; Yang et al. 2009). The reduction of laboratory-induced falls has been attributable to improved control of COM state (i.e., its position and velocity) stability.
Nevertheless, for this preventive strategy to work in practice, the effects of a single perturbation training session must be retained over significant lengths of time. Although the efficacy of a single perturbation training session is mostly unknown, there is sufficient evidence of long-term (weeks or months) motor retention of adaptation induced from various types of single-session repeated perturbation exposure, at least among young adults (Bhatt and Pai 2009a; Pai and Bhatt 2007; Tjernstrom et al. 2002; Wrisley et al. 2007). Clearly, it is not a trivial question because the longer the retention a single training session can produce, the greater the value such a preventive strategy will have. Previous studies have shown that low-frequency sessions provided at frequent intervals can provide retention similar to a single high-intensity training session (Bhatt and Pai 2009b). The requirement of frequent “booster” sessions to maintain their resilience, however, will increase logistical difficulty of scheduling, create adherence issues among participants, and also drive up the overall cost of the intervention.
The purpose of this study was therefore to determine whether and to what degree older adults can retain their fall-resisting skills acquired from a single perturbation training session. To eliminate any bias (the training effect resulting from multiple retest) and to provide a high temporal resolution of training retention (as fine as 1.5 months), this study was based on a conditional three-stage, sequential, pre-post-retest design. Although it is very time consuming, this design does offer maximal flexibility to enable us to set the optimal time for the retest at the next stage. The primary hypothesis was therefore that the beneficial effects derived from a single session of perturbation training on the control of COM stability and the reduction of laboratory-induced falls upon an unannounced slip would still persist in the next 6 to 12 months.
Methods
Study design
In this design, subjects underwent the initial training session at the beginning of each stage in precisely the same manner as their cohorts of other stages and returned to participate in a retest only once just as did the other cohorts at the end of that stage (Fig. 1). The training method employed in this study has been able to dramatically reduce the incidence of laboratory-induced falls from the first, novel slip (pre-training) to the final slip (post-training, also please see below) in a single session, often by 40 % or more among older adults (Pai et al. 2010). Whether or not the participants in a given stage successfully retained their training would then determine the timing for the retest in the next stage. Successful retention is defined by the significantly lower laboratory-induced fall incidence in the retest than that upon the unrehearsed novel slip trial during the initial training session.
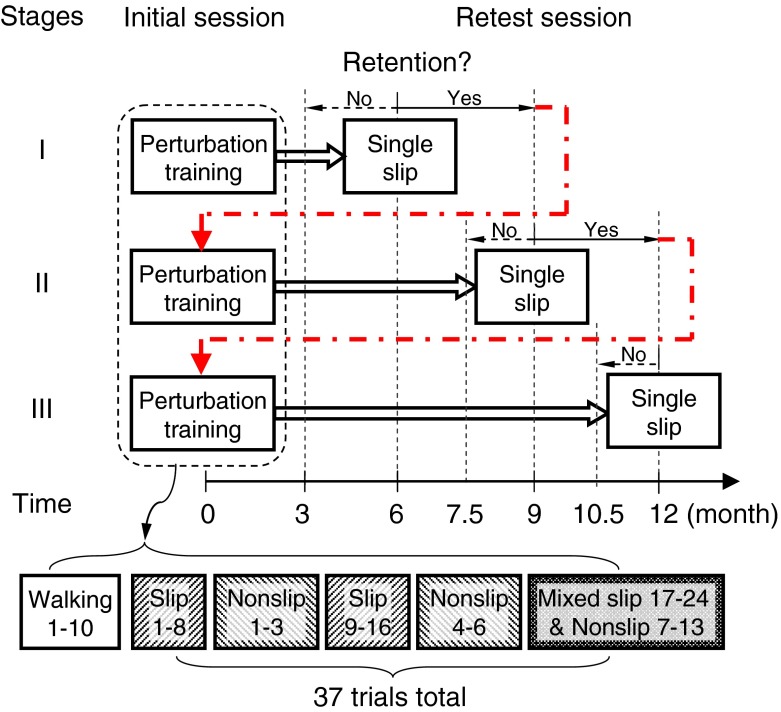
Fig. 1.
Schematic of the conditional, three-stage, sequential, pre-post-retest design and protocol. The retest for stage I was set 6 months after the initial training session. If participants in stage I displayed successful retention (“Retention? Yes”), the retest of the stage II cohort would be set at 9 months; if the retention in stage I was unsuccessful (“Retention? No”), the stage II retest would be 3 months after the initial session. Subsequently, if retention in stage II was successful (“Yes”), the stage III cohort would retest 12 months after their initial session; if the stage II retest was successful but stage III retest was unsuccessful, the length of retention would be recorded as at least 10.5 months. If retention in stage I was successful but stage II was unsuccessful, the stage III retest would be 7.5 months after the initial session. If retention did not occur in stage I or stage II, the stage III retest would occur 1.5 months after its initial training (not shown). If stage I was unsuccessful but the stage II retest was successful, stage III would retest 4.5 months after initial training (also not shown). The overtraining in this block-and-random design consists of 24 slips (bottom), all of which are unannounced. No rehearsal is given prior to the first novel trial so subjects do not know where, when, or how a slip will occur
Because this study was the first of its kind, we had little knowledge pertaining to when was the best time to set the retest for the subjects in the first stage. Based on the findings of previous studies that young adults are able to retain laboratory-induced fall-resisting skills for 4 months (Bhatt et al. 2006a), we then set the retest for first stage exploration to be at 6 months after the initial training among older adults. A 6-month retention is meaningful because it can span the entire winter session when weather-related slips can become prevalent among pedestrians.
If the participants in stage I exhibited significant retention during their 6-month retest (stage I “Retention? Yes” in Fig. 1), the second cohort of subjects (stage II) would then retest 9 months after their initial training. Alternatively, if 6-month retention was not observed in stage I, stage II participants would retest 3 months after their initial session (stage I “Retention? No” in Fig. 1). The outcomes observed for stage I and stage II would then dictate whether the retest for the cohort in stage III would be at 7.5 months (stage II “No” in Fig. 1) or 12 months after their initial session (stage II “Yes” in Fig. 1). If retention was not observed in stage I or stage II—a scenario not shown in Fig. 1—the retest for stage III would occur 1.5 months after the initial session (not shown in Fig. 1). However, if stage I failed to exhibit retention but stage II was successful at 3 months, the retest for stage III would take place 4.5 months after the initial session (not shown in Fig. 1).
Participants
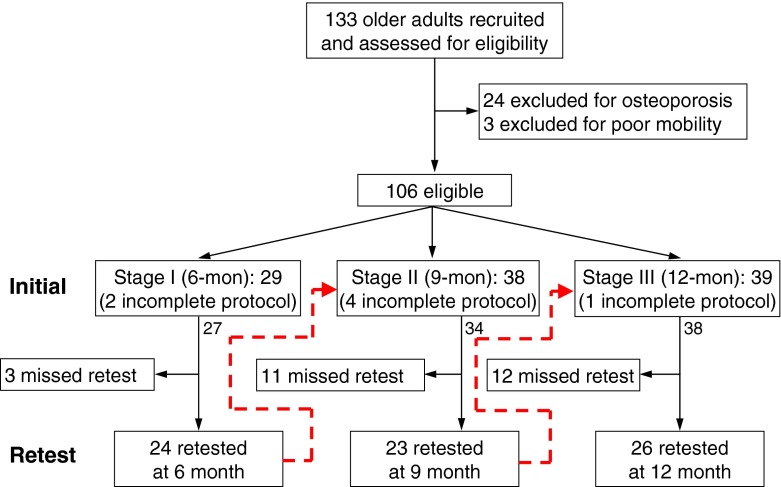
One hundred thirty-three community-dwelling older adults (≥65 years, Fig. 2) were initially recruited from exercise and community centers, independent senior living facilities, the Aging Research Registry of the Buehler Center on Aging at Northwestern University, and affiliates of the City of Chicago Department on Aging. This pool of participants completed a questionnaire on their history of neurological, musculoskeletal, cardiopulmonary, and other systemic disorders, as well as any falls they had experienced over the preceding 12 months. These people were screened for the use of selected drugs that may have altered their control of stability (e.g., tranquilizers). As a safety precaution, they were also screened for an elevated risk of fracture during training (based on calcaneal ultrasound body mineral density scan T score <−1.5 (Thompson et al. 1998)), difficulty following instructions (Folstein Mini Mental Status Exam score <25 (Folstein et al. 1975)), or poor mobility (>13.5 s on the Timed-Up-and-Go test (Podsiadlo and Richardson 1991)), which could have rendered them unable to complete the protocol. After this exclusion screening, a total of 106 eligible subjects consented to and participated in one of the three cohorts: stage I, II, or III (Fig. 2). Among those, 24 of 29 in stage I returned for their retest; 23 of 38 participants in stage II and 26 of the 39 subjects in stage III returned (Table 1 and Fig. 2). There were no differences in demographics or response to training between those subjects who returned for retest and those who did not (Table 1).
Fig. 2.
A flow diagram demonstrating subject recruitment and progress through the various phases for all three stages of the study. Subjects with T scores on calcaneal ultrasounds less than −1.5, Folstein Mini Mental Status Exam scores under 25, or Time-Up-and-Go test scores greater than 13.5 s were excluded. The red broken arrows indicate the sequential design of the study. For details of the study design, please refer to Fig. 1
Table 1.
Means (standard deviations) and comparisons of subject demographics and training parameters for the three independent retest cohorts
| Demographics and training | Stages | p value | Pooled | p value | |||
|---|---|---|---|---|---|---|---|
| I (n = 24) | II (n = 23) | III (n = 26) | Returned (n = 73) | Not returned (n = 26) | |||
| Demographics | |||||||
| Age (years) | 74.6 (5.8) | 71.8 (5.5) | 72.0 (4.7) | 0.14 | 72.7 (5.4) | 70.8 (4.7) | 0.10 |
| Gender (female) | 13 (54.2 %) | 15 (65.2 %) | 19 (73.1 %) | 0.37 | 47 (64.4 %) | 16 (61.5 %) | 0.80 |
| Body height (m) | 1.70 (0.09) | 1.68 (0.09) | 1.66 (0.09) | 0.44 | 1.68 (0.09) | 1.66 (0.11) | 0.32 |
| Body mass (kg) | 74.9 (12.3) | 75.9 (13.8) | 75.1 (12.9) | 0.96 | 75.3 (12.9) | 75.8 (13.6) | 0.86 |
| Perturbation training | |||||||
| Falls upon novel slip | 10 (41.7 %) | 9 (39.1 %) | 12 (46.2 %) | 0.94 | 31 (42.5 %) | 16 (61.5 %) | 0.10 |
| Proactive stability control | −0.15 (0.04) | −0.17 (0.06) | −0.16 (0.05) | 0.14 | −0.16 (0.05) | −0.15 (0.06) | 0.56 |
| Reactive stability control | −0.43 (0.20) | −0.39 (0.20) | −0.43 (0.19) | 0.14 | −0.41 (0.19) | −0.36 (0.19) | 0.23 |
| Falls upon final slip | 0 (0 %) | 0 (0 %) | 0 (0 %) | 1.00 | 0 (0 %) | 0 (0 %) | 1.00 |
| Proactive stability control | −0.08 (0.07) | −0.12 (0.05) | −0.11 (0.06) | 0.23 | −0.10 (0.06) | −0.11 (0.06) | 0.66 |
| Reactive stability control | 0.65 (0.44) | 0.72 (0.44) | 0.79 (0.24) | 0.34 | 0.72 (0.38) | 0.69 (0.36) | 0.47 |
Also listed are the comparisons of subject demographics and training parameters between those returned for the retest session and those who did not
Instrumented walkway
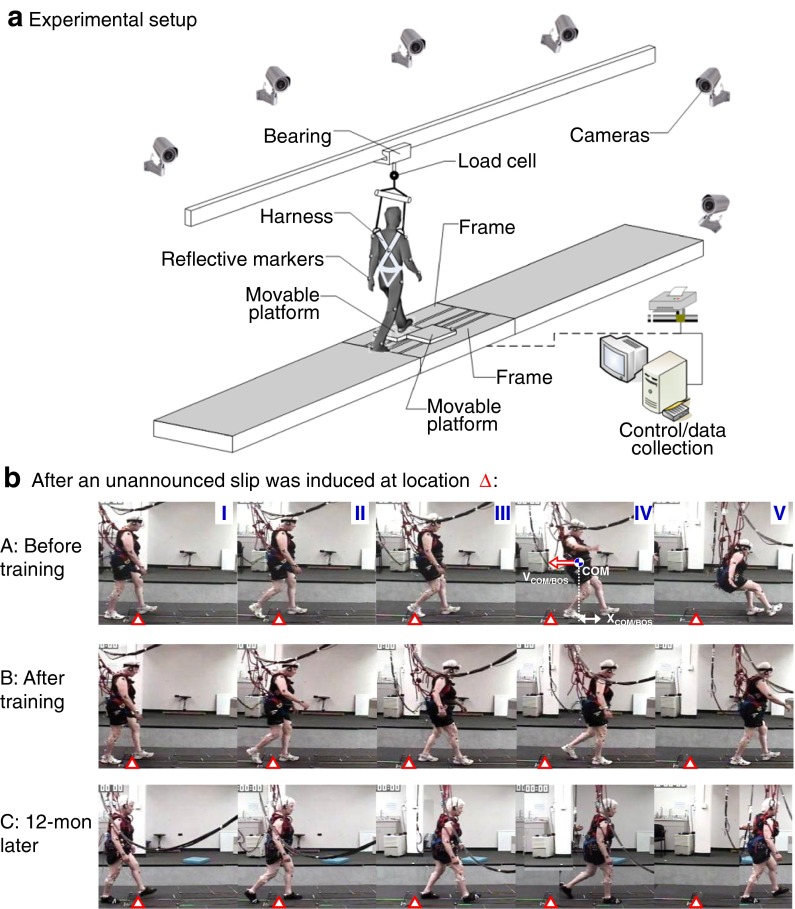
Slips were induced through the release of a pair of side-by-side, low-friction, movable platforms embedded near the midsection of a 7-m walkway (Fig. 3a). These platforms were locked in place when subjects stepped onto them. During a slip trial, the platforms were allowed to slide freely for up to 90 cm forward or 58 cm backward after force plates (AMTI, Newton, MA, not shown in Fig. 3a) installed beneath them detected the subject’s footstep. Upon receiving a signal from the force plates, a computer program triggered the release of the electronic mechanical locking mechanism that held the plates in place. All slips were unannounced in order to mimic real-life situations. Although the device allows the slip to occur in both directions, all slips during the training were initiated naturally in the forward direction simulating the consequence in real life, such as when a person suddenly steps onto a patch of ice in the parking lot. Such slips led to backward balance loss rather than forward balance loss. A full-body harness, connected through a load cell and shock-absorbing ropes to an overhead trolley on a track over the walkway, enabled subjects to walk freely while providing protection against any harmful body impact with the floor surface (Fig. 3a).
Fig. 3.
a Schematics of the experimental setup used to induce an unannounced slip in the person traversing the walkway. A slip is induced by releasing two low-friction movable platforms embedded in the middle of this 7-m walkway. Each of the two movable platforms is mounted to the walkway base-frame with four low-friction linear bearings. The base-frame is bolted to two force plates (not shown) which are used to measure ground reaction force; each platform is unlocked electronically after the force plates detect the landing of the corresponding foot. All subjects wore a safety harness adjusted to prevent any part of the body (other than the feet) to come in contact with the ground. b Still-frame video images (taken after the release of moveable platform) of a subject who fell upon the first novel slip (panel A) but was subsequently able to walk over the slippery surface in the final slip of the initial session (panel B) and again employed the “walkover” strategy traversing the same slippery surface 12 months later (panel C). The first three frames in each panel were taken near slipping foot touchdown (I), trailing foot liftoff (II), and trailing foot touchdown (III). In panel A, the subject began to fall in the fourth frame (IV), as defined when the load cell force exceeded 30 % of the subject’s body weight. Location of center-of-mass (COM) is marked, as well as the relative velocity between the COM and the base-of-support (BOS), V COM/BOS, and their relative position, X COM/BOS. The subject’s stability was computed based on her instantaneous motion state (X COM/BOS and V COM/BOS) (Pai and Patton 1997; Yang et al. 2008a). The last (V) frame was near the end of the fall when she was completely suspended by the harness. The frames IV and V in panels B and C were taken near slipping foot liftoff and touchdown. The open triangle in each frame approximates the initial position of the slipping foot at slip onset. Based on the distance of the slip, the person in b(B) and b(C) apparently had adopted the walkover strategy
Protocol for the training and the retest
The concept of overlearning in blocked-and-random designs was applied to enhance the retention of motor memory (Schmidt and Lee 1999). The sequence of the blocked-and-random training was the same for all subjects (Bhatt et al. 2006b). It began with a block of eight slips, followed by a block of three nonslip trials, another block of eight slips, a second block of three nonslip trials, and a final block of 15 mixed trials (Fig. 1). During these trials, subjects were instructed to walk with their preferred speed and manner and were informed only that they “may or may not be slipped” at any time and that, if a slip occurred, they should “try to recover” and “continue to walk.” None of them were told when, where, and how they might slip; to make the first unannounced slip completely novel, no rehearsal was provided. Further, the platforms were firmly locked in the first ten trials (Fig. 1) in order to make it probabilistically difficult to predict when the novel slip would eventually occur. Retest sessions used an identical setup and protocol as the initial session. Subjects in retest sessions were exposed to their first slip after eight to 13 trials.
Data collection and analysis
During subjects’ initial sessions, data collected during their first (novel) slip trial was used to provide the pre-training measurements. The final (24th) slip represented the post-training trial and data collected from it were used to assess training effects. All of the measurements used to assess training retention were taken from the first slip trial of the retest. Full body kinematics from 28 retro-reflective markers placed on the subject’s body and movable platforms was collected using an 8-camera motion capture system (MAC, Santa Rosa, CA). Each subject’s COM kinematics were computed using gender-dependent segmental inertial parameters (de Leva 1996) based on the filtered marker positions. Relative COM position and velocity were referenced to the rear edge of the BOS, with the position normalized by foot length (lBOS) and velocity by  , where g is gravitational acceleration and bh is body height. Data from walkway force plate signals and the overhead load cell were synchronously recorded and used to identify the instant of foot touchdown and the identification of laboratory-induced falls, respectively.
, where g is gravitational acceleration and bh is body height. Data from walkway force plate signals and the overhead load cell were synchronously recorded and used to identify the instant of foot touchdown and the identification of laboratory-induced falls, respectively.
Outcome measurements
The present study tracked three outcome variables for each slip trial: first, whether or not the subject fell in a trial, and, second and third, the subject’s proactive and reactive control, as calculated in terms of stability at two distinct intervals after slip onset (Yang et al. 2009). A subject was identified as having fallen in a given trial when the peak force experienced by the overhead load cell during that trial exceeded 30 % of the subject’s body weight (Yang and Pai 2011) (Fig. 3b(A)). To assess proactive and reactive control, stability was calculated as the shortest distance from the relative motion state between the COM and the BOS (in terms of their relative horizontal position and velocity) to the stability limits predicted by the mathematical model (Pai and Patton 1997; Yang et al. 2008a, b). Such theoretically derived stability limits have been extensively verified with experimental data (Bhatt et al. 2006b; Hof et al. 2005; Patton et al. 1999; Yang et al. 2008a). In the present study, larger values indicate greater stability: subjects with greater stability values were less likely to take a protective step that would land posterior to the slipping foot in order to recover from a slip (Pai et al. 2003). Data for the assessment of proactive control was recorded at the instant of slipping foot touchdown, 30–50 ms prior to the onset of the slip (Yang et al. 2009). Reactive control was calculated based on data recorded at the touchdown of the trailing limb in the recovery (or protective) step—generally 300–500 ms after slip onset (Yang et al. 2009).
Statistical analysis
To assess demographic and age differences between the subjects in different trial stages, these variables were compared across all three stages using a one-way analysis of variance (ANOVA) with stage as the factor. The generalized estimating equation (GEE) statistical model with post-hoc Wilcoxon signed-rank test and Mann–Whitney test were applied to examine the training and retention effect on laboratory-induced fall reduction in each stage (the within-group or trial factor), to examine the similarity of training effects across all three cohorts for uniformity, and to determine the maximum length of retention (the between-group or stage factor). In parallel, repeated measures ANOVAs and post hoc Turkey’s HSD tests were used to assess adaptive improvements and the retention of stability control (the trial factor) and to determine whether any bias existed across the cohorts (the stage factor). Significant main effects and interactions were resolved with paired and independent t tests using the Bonferroni corrections for multiple comparisons. All analyses were performed using SPSS 19 (IBM Corp., Armonk, NY) with a two-tailed test at significance level of 0.05.
Results
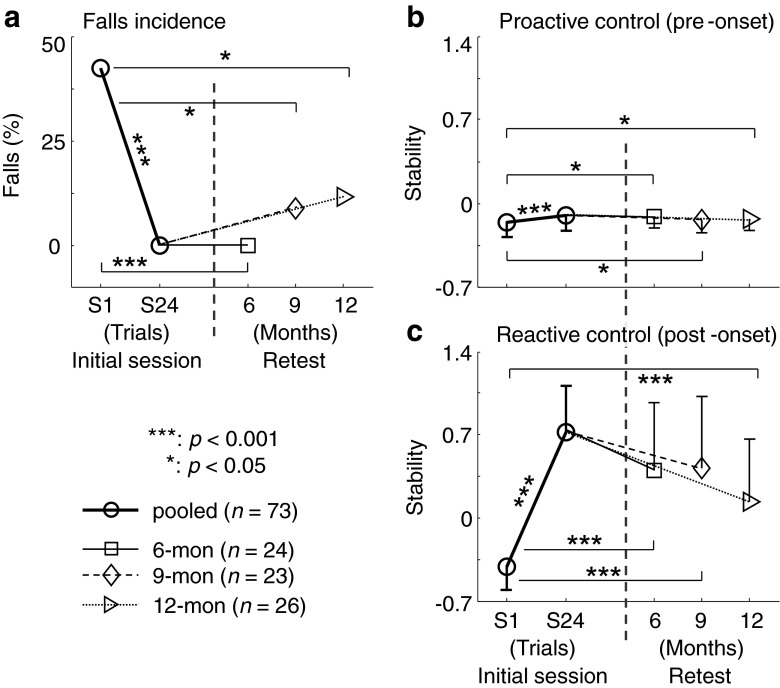
The subjects in each cohort (stage) had comparable demographic characteristics; the incidence of laboratory-induced falls exhibited by subjects upon their novel and final slips was also similar for all cohorts (p > 0.05 for all, Table 1). Subjects’ proactive and reactive control of stability was comparable during the initial training session as well (Table 1 and Fig. 4b, c). Demographic characteristics and training effect were also similar for those who returned and those who did not return for the retest (Table 1). Because the subjects in the first cohort displayed successful retention (at 6 months), the second cohort then began their initial training and was retested after 9 months. The second cohort’s success in retention eventually led to the final cohort that began its initial training and returned for retest 12 months later.
Fig. 4.
a Training-induced reduction in falls incidence (%) and the adaptive change and retention in b proactive and c reactive control of stability. Measurements were taken from the first novel slip (S1) and final slip (S24) of the initial training session, as well as the retest slip, which took place 6 months (square), 9 months (diamond), or 12 months (triangle) after the initial session. For S1 and S24, the values were pooled from all three cohorts (circle, please see Table 1)
During all initial sessions, perturbation training significantly reduced the incidence of laboratory-induced falls: while 42.5 % of participants (31/73) fell upon exposure to the novel slip, none fell during their final slip exposure (p < 0.001, Fig. 4a). These improvements attributed to the subjects’ increasing proactive (Cohen’s d = 1.0, p < 0.001, Fig. 4b) and reactive control of stability (Cohen’s d = 2.9, p < 0.001, Fig. 4c). In each cohort’s corresponding retest, laboratory-induced fall incidence was 0 % (0/24 falls), 8.7 % (2/23 falls), or 11.5 % (3/26 falls) at 6, 9, or 12 months, respectively (Fig. 4a). Subjects in all cohorts fell less during the retest because they maintained significantly better control of stability than they had upon their novel slip trial (Fig. 4b, c).
Discussion
Community-dwelling older adults displayed outstanding motor retention for as much as 12 months in this study. These results demonstrated that their CNS can implicitly adapt (without needing any instructions) and successfully develop proactive (feed-forward) and reactive (feedback) control strategies. Their resilience against laboratory-induced falls was clearly retained which enabled them to effectively reduce peak slip speed thereby reducing the intensity of slips (Bhatt et al. 2006b; Yang and Pai 2010) by adopting the skate-over or the walkover strategies (as shown in Fig. 3b(B, C), the person adopted the walkover strategy upon the final slip during the training and upon the only slip during the retest).
The overlearning concept has been followed in the design of the blocked-and-random training protocol (with 24 slips) to improve long-term retention after the results from an early study showed that an initial training consisting of five repeated slips only yielded limited retention among young adults (Bhatt et al. 2006a). The acquisition of these skills could be accompanied by a transformation in memory from the short-term labile state to a longer lasting stable state (Kandel et al. 2000). The retention produced by perturbation training may also be reinforced by the perceived penalties that could result from such errors. Falls reproduced under well-protected conditions in our laboratory are involuntary and inadvertent, like those that occur outside of the laboratory. However, outside of the laboratory, such falls often lead to severe (even life-threatening) injuries. Such consequences of an inappropriate response to slip (a fall), whether induced in laboratory or in everyday living, may force (or motivate) the CNS at least to try to quickly adapt for an extended period (Adkin et al. 2000). After all, fear-conditioning studies in mice have demonstrated that a single session is sufficient for long-term retention of the acquired stimulus–response behavior (Sacchetti et al. 2004).
Perturbation training is emerging as a viable means to reduce laboratory-induced falls (Pai and Bhatt 2007; Parijat and Lockhart 2012; Shimada et al. 2004; Yang et al. 2013). This approach is novel because it focuses on adaptation to externally induced perturbation instead of self-motivated improvements in physical conditioning, balance control, or volitional performance like other contemporary fall reduction methods (Rubenstein and Josephson 2006; Shumway-Cook et al. 2007; Tinetti et al. 1994; Wolf et al. 2003). Perturbation training may have some advantages. It can induce gross errors that are involuntary in nature and therefore cannot be corrected by merely volitional performance (Scheidt et al. 2001; Tseng et al. 2007). Experiencing such errors is essential for the CNS to recalibrate an existing internal representation of the environment (Blakemore et al. 1998; Shadmehr and Mussa-Ivaldi 1994)—in this case pertaining to the stability limits—which provides the required basis for adaptive adjustments in both proactive and reactive control of stability.
Such perturbation-based training may in fact be preferable also because training that focuses only on volitional performance (and in essence, self-motivation) clearly lacks the opportunity for someone to improve his or her reactive control of stability—which is vital for recovery from unexpected or unpreventable postural disturbances. Further, the recalibration process appears to take place in just a few perturbation trials (Bhatt et al. 2006a; Karniel and Mussa-Ivaldi 2002): “skate-over” or “walkover” strategies quickly emerge when older adults traverse the same slippery surface (Bhatt et al. 2006a). In contrast, learning an entirely new motor program (such as Tai Chi) in order to reduce the likelihood of falls takes much longer (weeks or months) to accomplish (Wolf et al. 2003).
The current findings have societal implications. Susceptibility to falls generally increases with age, so falls pose a particularly significant health threat to older adults. Common injuries that result from falls—like hip fractures—often require surgical intervention and extensive post-surgical management. Beyond human suffering, this comes at significant economic cost to patients and the health-care system. Because fall-related injury affects not only individuals who are already frail or impaired but also healthy and independent older adults, these societal effects are even more pronounced, impacting a larger population of people. When paradigms such as perturbation training can quickly lead to significant adaptation and long-term retention, it becomes a prime candidate for application to the general public. While contemporary posture-and-balance-training programs commonly require multiple sessions over many weeks (or months) (Rubenstein and Josephson 2006; Shumway-Cook et al. 2007; Tinetti et al. 1994; Wolf et al. 2003), this relatively low-cost and quick prophylactic strategy can still yield long-lasting effects. Our most recent evidence indicates that one session of such perturbation training can reduce these older adults’ annual risk of falls by 50 % in their everyday living (Pai et al. 2014, Perturbation training can reduce community-dwelling older adults’ annual fall-risk: a randomized controlled trial, in review). These facts make a compelling case for including perturbation training in the repertoire of fall reduction techniques (Fitzharris et al. 2010; Pai et al. 2014, Perturbation training can reduce community-dwelling older adults’ annual fall-risk: a randomized controlled trial, in review; Rubenstein and Josephson 2006; Shumway-Cook et al. 2007; Tinetti et al. 1994; Wolf et al. 2003).
In summary, by letting older adults slip-and-fall in a safe and well-controlled laboratory environment, perturbation training puts such slips to good use. Given its efficacy and potential cost-effectiveness, perturbation training represents a paradigm shift in the range of prophylactic approaches that aim to reduce older adults’ likelihood of falls in their everyday living (Pai et al. 2014, Perturbation training can reduce community-dwelling older adults' annual fall-risk: a randomized controlled trial, in review). The findings of the present study provide the first evidence that by subjecting older adults to real-life-like postural disturbances in a safe environment—even for only a short period of time—older adults are likely to retain laboratory-induced fall resistance skills for at least a year.
Acknowledgments
This work was supported by grants from the U.S. National Institute of Health (NIH 2RO1-AG16727 and RO1-AG029616). The authors would like to thank Dr. Karen Adolph for her thoughtful comments and Dr. Debbie Espy for assisting in data collection and processing.
References
- Adkin AL, Frank JS, Carpenter MG, Peysar GW. Postural control is scaled to level of postural threat. Gait Posture. 2000;12:87–93. doi: 10.1016/S0966-6362(00)00057-6. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Pai Y-C. Generalization of gait adaptation for fall prevention: from moveable platform to slippery floor. J Neurophysiol. 2009;101(2):948–957. doi: 10.1152/jn.91004.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatt T, Pai Y-C. Prevention of slip-related backward balance loss: the effect of session intensity and frequency on long-term retention. Arch Phys Med Rehabil. 2009;90(1):34–42. doi: 10.1016/j.apmr.2008.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatt T, Wang E, Pai Y-C. Retention of adaptive control over varying intervals: prevention of slip- induced backward balance loss during gait. J Neurophysiol. 2006;95(5):2913–2922. doi: 10.1152/jn.01211.2005. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Wening JD, Pai Y-C. Adaptive control of gait stability in reducing slip-related backward loss of balance. Exp Brain Res. 2006;170(1):61–73. doi: 10.1007/s00221-005-0189-5. [DOI] [PubMed] [Google Scholar]
- Blakemore SJ, Goodbody SJ, Wolpert DM. Predicting the consequences of our own actions: the role of sensorimotor context estimation. J Neurosci. 1998;18(18):7511–7518. doi: 10.1523/JNEUROSCI.18-18-07511.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leva P. Adjustments to Zatsiorsky-Seluyanov's segment inertia parameters. J Biomech. 1996;29:1223–1230. doi: 10.1016/0021-9290(95)00178-6. [DOI] [PubMed] [Google Scholar]
- Englander F, Hodson TJ, Terregrossa RA. Economic dimensions of slip and fall injuries. J Forensic Sci. 1996;41(5):733–746. [PubMed] [Google Scholar]
- Fitzharris MP, Day L, Lord SR, Gordon I, Fildes B. The Whitehorse NoFalls trial: effects on fall rates and injurious fall rates. Age Ageing. 2010;39(6):728–733. doi: 10.1093/ageing/afq109. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. A practical method for grading the cognitive state of patients for the clinician. J Psychiatry Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Hof AL, Gazendam MG, Sinke WE. The condition for dynamic stability. J Biomech. 2005;38(1):1–8. doi: 10.1016/j.jbiomech.2004.03.025. [DOI] [PubMed] [Google Scholar]
- Joh AS, Adolph KE. Learning from falling. Child Dev. 2006;77:89–102. doi: 10.1111/j.1467-8624.2006.00858.x. [DOI] [PubMed] [Google Scholar]
- Kandel ER, Schzwartz JH, Jessell TM. Principles of neural science. 4. McGraw Hill: Health Professions Division; 2000. [Google Scholar]
- Karniel A, Mussa-Ivaldi FA. Does the motor control system use multiple models and context switching to cope with a variable environment? Exp Brain Res. 2002;143(4):520–524. doi: 10.1007/s00221-002-1054-4. [DOI] [PubMed] [Google Scholar]
- Luukinen H, Herala M, Koski K, Honkanen R, Laippala P, Kivela SL. Fracture risk associated with a fall according to type of fall among the elderly. Osteoporos Int. 2000;11(7):631–634. doi: 10.1007/s001980070086. [DOI] [PubMed] [Google Scholar]
- Pai Y-C, Bhatt T. Repeated slip training: an emerging paradigm for prevention of slip-related falls in older adults. Phys Ther. 2007;87(11):1478–1491. doi: 10.2522/ptj.20060326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai Y-C, Patton JL. Center of mass velocity-position predictions for balance control. J Biomech. 1997;30(4):347–354. doi: 10.1016/S0021-9290(96)00165-0. [DOI] [PubMed] [Google Scholar]
- Pai Y-C, Wening JD, Runtz EF, Iqbal K, Pavol MJ. Role of feedforward control of movement stability in reducing slip-related balance loss and falls among older adults. J Neurophysiol. 2003;90:755–762. doi: 10.1152/jn.01118.2002. [DOI] [PubMed] [Google Scholar]
- Pai Y-C, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Arch Phys Med Rehabil. 2010;91(3):452–459. doi: 10.1016/j.apmr.2009.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parijat P, Lockhart TE. Effects of moveable platform training in preventing slip-induced falls in older adults. Ann Biomed Eng. 2012;40(5):1111–1121. doi: 10.1007/s10439-011-0477-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton JL, Pai Y-C, Lee WA. Evaluation of a model that determines the stability limits of dynamic balance. Gait Posture. 1999;9(1):38–49. doi: 10.1016/S0966-6362(98)00037-X. [DOI] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed "up & go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin N Am. 2006;90(5):807–824. doi: 10.1016/j.mcna.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Sacchetti B, Scelfo B, Tempia F, Strata P. Long-term synaptic changes induced in the cerebellar cortex by fear conditioning. Neuron. 2004;42:973–982. doi: 10.1016/j.neuron.2004.05.012. [DOI] [PubMed] [Google Scholar]
- Scheidt RA, Dingwell JB, Mussa-Ivaldi FA. Learning to move amid uncertainty. J Neurophysiol. 2001;86(2):971–985. doi: 10.1152/jn.2001.86.2.971. [DOI] [PubMed] [Google Scholar]
- Schmidt RA, Lee TD. Conditions of practice. In: Schmidt RA, Lee TD, editors. Motor control and learning: a behavioral emphasis. Champaign: Human Kinetics Publishers, Inc.; 1999. pp. 285–318. [Google Scholar]
- Shadmehr R, Mussa-Ivaldi FA. Adaptive representation of dynamics during learning of a motor task. J Neurosci. 1994;14:3208–3224. doi: 10.1523/JNEUROSCI.14-05-03208.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill. Am J Phys Med Rehabil. 2004;83:493–499. doi: 10.1097/01.PHM.0000130025.54168.91. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Silver IF, LeMier M, York SC, Cummings P, Koepsell TD. Effectiveness of a community-based multifactorial intervention on falls and fall risk factors in community-living older adults: a randomized, controlled trial. J Gerontol A: Biol Med Sci. 2007;62(12):1420–1427. doi: 10.1093/gerona/62.12.1420. [DOI] [PubMed] [Google Scholar]
- Thompson PW, Taylor J, Oliver R, Fisher A. Quantitative ultrasound (QUS) of the heel predicts wrist ad osteoporosis-related fractures in women aged 45-75 years. J Clin Densitom. 1998;1:219–225. doi: 10.1385/JCD:1:3:219. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, Koch ML, Trainor K, Horwitz RI. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821–827. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- Tjernstrom F, Fransson P-A, Hafstrom A, Magnusson M. Adaptation of postural control to perturbations—a process that initiates long-term motor memory. Gait Posture. 2002;15(1):75–82. doi: 10.1016/S0966-6362(01)00175-8. [DOI] [PubMed] [Google Scholar]
- Tseng YW, Diedrichsen J, Krakauer JW, Shadmehr R, Bastian AJ. Sensory prediction errors drive cerebellum-dependent adaptation of reaching. J Neurophysiol. 2007;98(1):54–62. doi: 10.1152/jn.00266.2007. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Sattin RW, Kutner M, O'Grady M, Greenspan AI, Gregor RJ. Intense Tai Chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51:1693–1701. doi: 10.1046/j.1532-5415.2003.51552.x. [DOI] [PubMed] [Google Scholar]
- Wrisley DM, Stephens MJ, Mosley S, Wojnowski A, Duffy J, Burkard R. Learning effects of repetitive administrations of the sensory organization test in healthy young adults. Arch Phys Med Rehabil. 2007;88(8):1049–1054. doi: 10.1016/j.apmr.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Yang F, Pai Y-C. Role of individual lower limb joints in reactive stability control following a novel slip in gait. J Biomech. 2010;43:397–404. doi: 10.1016/j.jbiomech.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Pai Y-C. Automatic recognition of falls in gait-slip training: harness load cell based criteria. J Biomech. 2011;44:2243–2249. doi: 10.1016/j.jbiomech.2011.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Anderson FC, Pai Y-C. Predicted threshold against backward balance loss following a slip in gait. J Biomech. 2008;41:1823–1831. doi: 10.1016/j.jbiomech.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Passariello F, Pai Y-C. Determination of instantaneous stability against backward balance loss: two computational approaches. J Biomech. 2008;41(8):1818–1822. doi: 10.1016/j.jbiomech.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Bhatt T, Pai Y-C. Role of stability and limb support in recovery against a fall following a novel slip induced in different daily activities. J Biomech. 2009;42:1903–1908. doi: 10.1016/j.jbiomech.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Bhatt T, Pai Y-C. Generalization of treadmill-slip training to prevent a fall following a sudden (novel) slip in over-ground walking. J Biomech. 2013;46(1):63–69. doi: 10.1016/j.jbiomech.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]