Abstract
Background
The data analysis was conducted to describe the rate of unsuccessful copper T380A intrauterine device (IUD) insertions among women using the IUD for emergency contraception (EC) at community family planning clinics in Utah.
Methods
These data were obtained from a prospective observational trial of women choosing the copper T380A IUD for EC. Insertions were performed by nurse practitioners at two family planning clinics in order to generalize findings to the type of service setting most likely to employ this intervention. Adjuvant measures to facilitate difficult IUD insertions (cervical anesthesia, dilation, pain medication, and use of ultrasound guidance) were not utilized. The effect of parity on IUD insertion success was determined using exact logistic regression models adjusted for individual practitioner failure rates.
Results
Six providers performed 197 IUD insertion attempts. These providers had a mean of 14.1 years of experience (range 1–27, S.D. ±12.5). Among nulliparous women, 27 of 138 (19.6%) IUD insertions were unsuccessful. In parous women, 8 of 59 IUD insertions were unsuccessful (13.6%). The adjusted odds ratio (aOR) showed that IUD insertion failure was more likely in nulliparous women compared to parous women (aOR=2.31, 95% CI 0.90–6.52, p=.09).
Conclusion
The high rate of unsuccessful IUD insertions reported here, particularly for nulliparous women, suggests that the true insertion failure rate of providers who are not employing additional tools for difficult insertions may be much higher than reported in clinical trials. Further investigation is necessary to determine if this is a common problem and, if so, to assess if the use of adjuvant measures will reduce the number of unsuccessful IUD insertions.
Keywords: IUD, Insertion, Nulliparous, Advanced practice clinician
1. Introduction
After years of being one of the least used contraceptives in the United States, the intrauterine device (IUD) is now steadily regaining interest among women seeking a highly effective reversible method of contraception. IUD use is currently at its highest level in 20 years [1]. With changes in the guidelines of major organizations [2–5], more young and nulliparous women are being offered and choosing this method.
In recent years, several published studies have examined IUD use in nulliparous women. These studies have examined continuation rates, complications and reasons for removal in nulliparous women [5–10], but there are few data regarding unsuccessful insertions. Recognizing that IUD insertion may be more difficult in nulliparous women compared to parous women, the use of additional modalities to ease insertions has been examined, with attention mainly focused on use of misoprostol prior to insertion. All studies included or were limited to nulliparous women. However, the majority of these studies failed to show any difference in ease of insertion with use of misoprostol when compared to placebo [11–14].
Additionally, the studies cited above are large clinical trials, with insertions performed by highly experienced practitioners. Insertion failure rates reported in these studies are low, ranging from 0–3.4% [6,7,10–14]. There are minimal published data to date on insertion failures in community-based clinical practice. However, the majority of providers caring for women at Title X family planning clinics in the United States are advanced practice clinicians (APCs), who may not be trained in the use of adjunctive measures to aid in their insertions. We performed this study as secondary data analysis from a study of the IUD for emergency contraception (EC) to describe the incidence of IUD insertion failure in community practice.
2. Methods
These data were obtained from a prospective observational trial of women choosing the copper T380A IUD for EC [15]. The study was approved by the University of Utah institutional review board. Women between 18–30 years old presenting for EC at two Planned Parenthood clinics in Utah between November 2009 and July 2010 were offered participation in the study. Women were considered eligible for participation if they had unprotected intercourse within 120 hours, negative pregnancy test, expressed desire to prevent pregnancy for 1 year, and were willing to comply with the study requirements. They were also required to have a functioning phone number at time of entry into the study. Exclusion criteria included current pregnancy, breastfeeding, intrauterine infection within the past 3 months, history of sterilization, an IUD or contraceptive implant already in place, vaginal bleeding of unknown etiology, known gonorrhea or Chlamydia infection in the last 30 days (unless successfully treated at least 7 days prior to study entry), allergy to levonorgestrel (LNG) (for oral EC patients) or allergy to copper or Wilson’s disease (for Copper IUD patients) or known abnormalities of the uterus that distort the uterine cavity. The main study was powered to detect a difference in pregnancy rates between women choosing oral LNG or the copper T380 IUD for EC at 12 months.
After enrollment, patients chose their desired method of EC, 1.5 mg oral LNG or the copper T380A IUD. Patients selecting the IUD needed to identify themselves as desiring long-term contraception. The original study was designed to evaluate the long-term rates of unplanned pregnancy in IUD or oral LNG EC users, with the primary outcome being occurrence of an unplanned pregnancy within 12 months of presenting for EC. Participants were contacted by telephone for follow-up at 1, 3, 6, 9 and 12 months after enrollment.
Insertions were performed by nurse practitioners at the two family planning clinics, in order to generalize findings to the type of service setting most likely to employ this intervention. Patients presented as walk-ins and, thus, were not scheduled into IUD insertion time slots. IUDs were inserted in the following standard fashion: after bimanual exam and placement of speculum the cervix was prepped with betadine and a tenaculum was placed on the anterior lip of the cervix. The uterus was then sounded using a 4-mm stainless steel sound and IUD insertion was attempted. Adjuvant measures to facilitate difficult IUD insertions (cervical anesthesia, dilation, pain medication, and use of ultrasound guidance) were not utilized. If the provider was not able to place the IUD on the first attempt, patients were given oral LNG for EC instead. No other providers assisted in the insertions.
For this analysis, we compared the insertion rates in nulliparous women versus parous women. Unsuccessful insertion was defined as failure to place the IUD at that visit. Data from providers performing less than five insertions during the study period were excluded. The effect of parity on IUD insertion failure was determined using exact logistic regression models, adjusted for individual practitioner failure rates to estimate odds ratios and 95% confidence intervals (95% CIs). Demographic variables were compared using chi-square analysis. p Values less than .05 were considered significant. All data were analyzed using Stata 12.0 statistical software (Stata, College Station, TX, USA) and SAS version 9.2 (SAS Institute, Cary, NC, USA).
3. Results
A total of 549 women were enrolled in the study and of these, 218 chose the IUD for EC, of whom three did not meet criteria for IUD insertion. One patient self-reported a history of bicornuate uterus, one sounded to 9.5 cm (clinic guidelines limit use to uteri sounding to 9 cm), and another patient’s uterus was perceived to be “too small” on bimanual exam, before any attempt at insertion was made. Six providers met the criteria of performing at least five insertions during the study period, leaving 197 IUD insertion attempts for inclusion in this analysis. Among these providers there were three Family Nurse Practitioners (FNP) and 3 Women’s Health Nurse Practitioners (WHNP). Their clinical experience, based on years since completing training, ranged from 1 to 27 years (mean 14.1, S.D. ±12.5).
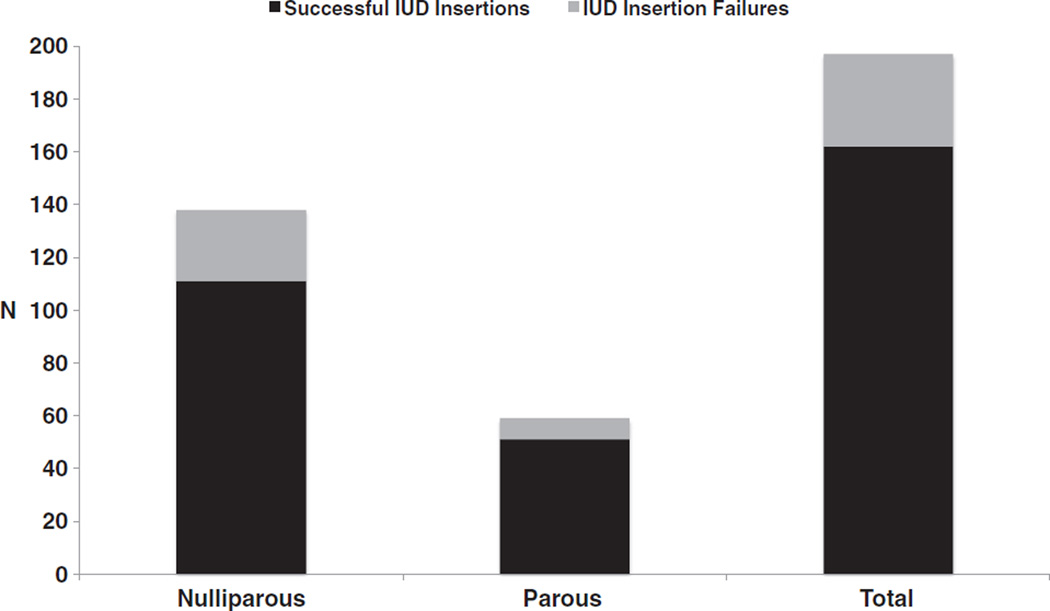
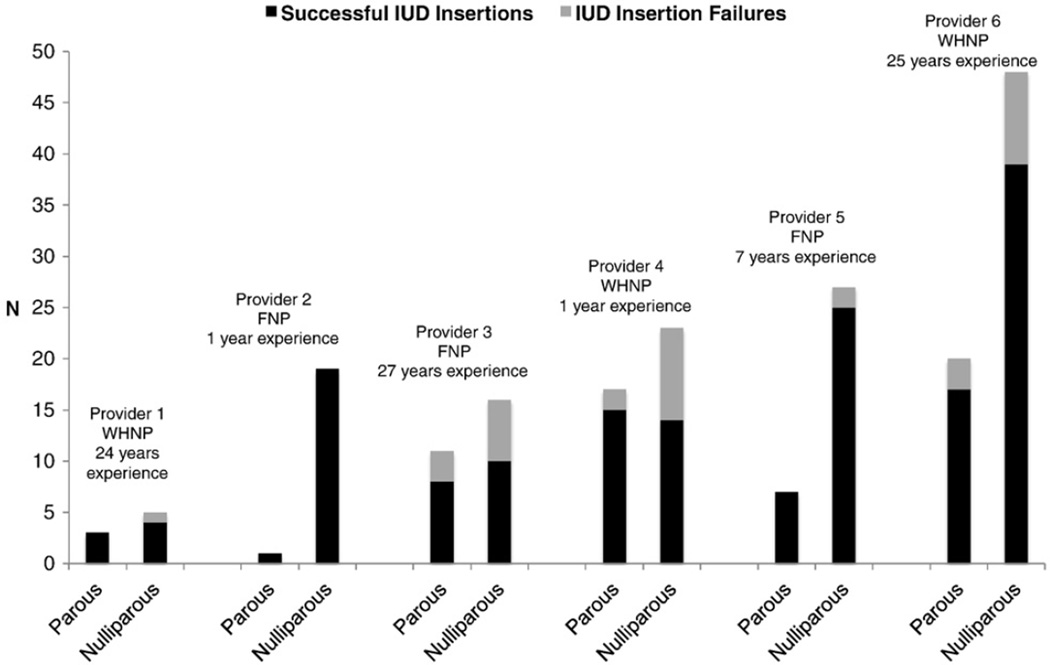
Table 1 displays the demographic characteristics of the patient study population. There were no statistically significant differences between the two groups. The insertion outcomes, both overall and by parity, are shown in Fig. 1. Overall, 35 of the 197 attempted insertions were unsuccessful (17.8%). Among nulliparous women, IUD insertion failures occurred in 27 of 138 women (19.6%). Of these insertion failures, 26 women were nulligravid. In parous women, IUD insertion failures occurred in 8 of 59 women (13.6%). This difference was not statistically significant (p=.25). However, since one practitioner had a 0% failure rate, an adjusted odds ratio for IUD insertion failure based on parity was calculated using an exact logistic regression, controlling for individual practitioners’ failure rates when determining the effect of parity. There was a trend toward increased risk of IUD insertion failures in nulliparous compared to parous women. The adjusted odds ratio for an unsuccessful IUD insertion by parity was 2.31 (95% CI 0.90–6.52, p=.09) with insertion failures more likely in the nulliparous group. Insertion outcomes for each provider are displayed in Fig. 2, and stratified by parity.
Table 1.
Baseline demographics
| All IUD attempts |
Successful insertions |
Unsuccessful insertions |
||
|---|---|---|---|---|
| n=197 | n=162 (82.2%) | n=35 (17.8%) | ||
| Mean (S.D.) | Mean (S.D.) | Mean (S.D.) | ||
| Age, years | 23 (3.39) | 23 (3.73) | 23 (3.31) | |
| n (%a) | n (%a) | n (%a) | p value | |
| Race | ||||
| White, non-Hispanic | 127 (64.4) | 108 (66.7) | 19 (54.2) | .17 |
| Hispanic | 36 (18.2) | 29 (17.9) | 7 (20) | .77 |
| Other | 34 (17.2) | 25 (15.4) | 9 (25.7) | .14 |
| Parity | ||||
| Nulliparous | 138 (70) | 109 (67.2) | 27 (77.1) | .25 |
| Parous | 59 (30) | 53 (32.7) | 8 (22.9) | |
| Birth control method prior | ||||
| None | 50 (25.4) | 41 (25.3) | 9 (25.7) | .96 |
| Hormonal | 29 (14.7) | 27 (16.7) | 2 (5.7) | .10 |
| Non-hormonal | 64 (32.5) | 52 (32.1) | 12 (34.3) | .80 |
| Multiple | 54 (27.4) | 42 (25.9) | 12 (34.3) | .31 |
Percentages may not add up to 100% due to rounding.
Fig. 1.
IUD insertion attempts by parity.
Fig. 2.
IUD insertions by provider and parity.
Reasons for unsuccessful insertion were recorded in 32/35 cases. “Unable to sound” was the most common reason listed in 29/32 cases (90.6%). “Uterus too small” was cited in 2/35 (6.3%), where uterus sound depth was listed as <5 cm. In the remaining insertion attempt the provider was unable to visualize the cervix.
Expulsions occurred in 13/162 women during the first 6 months of the study (8%), 10 of whom were nulliparous. There were no cases of uterine perforation, nor were there any episodes of pelvic inflammatory disease or infections necessitating treatment among study patients as assessed during telephone follow-up contact with the participants and review of clinic records.
4. Discussion
In the family planning clinic setting, among women choosing copper IUDs for EC, these data revealed a higher number of unsuccessful insertions than expected.Most notably, 17.6% of women electing to receive the IUD for EC failed to have an IUD inserted that day. The data from this study demonstrate a much higher rate of unsuccessful insertions than previously reported in the literature [7,11–14,16–24]. There are several aspects of this study differing from other published studies that may account for this disparity.
The high proportion of nulliparous women in this study (70%) is one potential contributor. The impact of nulliparity on insertion success is an important one because of the changing profile of IUD users in the United States [25]. These patients present a potentially greater challenge compared to women who made up the majority of IUD insertions in the past. Higher IUD insertion failure rates or increased use of adjuvant measures among nulliparous women have been reported in other studies [6,10,13,23]. Nulliparous women in this study experienced a higher insertion failure rate than parous women, at 19.6%. In this relatively small sample size, the difference in insertion success based on parity approached significance. It is possible that a larger sample of patients would show a significant difference. However, even among parous women, the failure rate of 13.6% was also higher than anticipated, suggesting that parity alone does not explain our findings.
The fact that this study was an investigation of women requesting EC may also have influenced the findings. In this situation, patients did not enter the clinic intending to have an IUD inserted and anxiety may have played a larger role in failures than in other settings. Patient’s anxiety was not assessed in this study and thus the role it may have played on insertion success is not clear. However, there is evidence to suggest that women with anxiety over the procedure would have higher level of perceived pain [26], potentially contributing to a more difficult insertion. On the clinical side, the fact that these were unscheduled procedure visits may also have contributed to the failure rate through a real or perceived disruption in clinic flow, resulting in less time being taken with more challenging insertions.
The role of the provider in insertion success has not been widely studied. It is notable here that all providers performing insertions were APCs, though the specific type of training or years of experience did not appear to correlate with IUD insertion success rate. The most commonly cited reason for failed insertion was failure to sound the uterus. Increased resistance at the internal os may lead providers to abort the procedure, either due to patient discomfort or fear of perforation. Of perhaps greater significance, these providers did not use any adjunctive measures such as cervical dilation, paracervical block or ultrasound to aid insertions. While most studies do not specifically describe use of these measures, those that do report a rate of use in up to 20% of insertions [6,10,13]. It can be extrapolated that non-use of these measures would result in a higher insertion failure rate.
This study is limited by the fact that it was not designed to evaluate insertion success rates and thus was not powered to determine a difference in IUD insertion success by parity. Also, as a secondary data analysis there are potentially data not collected that may have allowed better understanding of the reasons for this higher failure rate. Examples could include provider experience with IUD insertions, as well as patient factors, such as history of cervical surgery or pelvic infection. However, while this study is a secondary data analysis and the effect of parity did not reach statistical significance, the findings do reflect what is happening in a community based clinical care setting and have clinical significance.
These results do suggest a higher rate of unsuccessful insertions in nulliparous compared to parous women. However, given the overall insertion failure rate is much higher than expected in both populations, it is clear that further studies in this area are needed to assess the frequency of IUD insertion failures in community settings, the reasons for insertion failures, to prospectively assess patient and provider risk factors for insertion failure and to examine interventions that will increase the proportion of successful insertions.
Acknowledgments
The authors gratefully acknowledge the support of Planned Parenthood Association of Utah patients, staff and administration with this project, as well as editorial support from Kirtly Parker-Jones and Patricia Murphy.
Footnotes
Funding: The project described was supported by a grant from the Society of Family Planning and Award Number R21HD063028 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health. The project received further support from the Planned Parenthood Association of Utah clinic staff and administration.
References
- 1.Mosher WD, Jones J. Use of contraception in the United States, 1982–2008. Vital Health Stat. 2010;23(29):1–44. [PubMed] [Google Scholar]
- 2.ACOG Committee Opinion No. 392, December 2007. Intrauterine device and adolescents. Obstet Gynecol. 2007;110:1493–1495. doi: 10.1097/01.AOG.0000291575.93944.1a. [DOI] [PubMed] [Google Scholar]
- 3.ACOG Committee Opinion no. 450: increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2009;114:1434–1438. doi: 10.1097/AOG.0b013e3181c6f965. [DOI] [PubMed] [Google Scholar]
- 4.ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118:184–196. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 5.Lyus R, Lohr P, Prager S. Use of the Mirena LNG-IUS and Paragard CuT380A intrauterine devices in nulliparous women. Contraception. 2010;81:367–371. doi: 10.1016/j.contraception.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Bahamondes MV, Hidalgo MM, Bahamondes L, Monteiro I. Ease of insertion and clinical performance of the levonorgestrel-releasing intrauterine system in nulligravidas. Contraception. 2011;84:e11–e16. doi: 10.1016/j.contraception.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Brockmeyer A, Kishen M, Webb A. Experience of IUD/IUS insertions and clinical performance in nulliparous women—a pilot study. Eur J Contracept Reprod Health Care. 2008;13:248–254. doi: 10.1080/02699200802253706. [DOI] [PubMed] [Google Scholar]
- 8.Duenas JL, Albert A, Carrasco F. Intrauterine contraception in nulligravid vs parous women. Contraception. 1996;5:23–24. doi: 10.1016/0010-7824(95)00025-9. [DOI] [PubMed] [Google Scholar]
- 9.Veldhuis HM, Vos AG, Lagro-Janssen AL. Complications of the intrauterine device in nulliparous and parous women. Eur J Gen Pract. 2004;10:82–87. doi: 10.3109/13814780409044540. [DOI] [PubMed] [Google Scholar]
- 10.Suhonen S, Haukkamaa M, Jakobsson T, Rauramo I. Clinical performance of a levonorgestrel-releasing intrauterine system and oral contraceptives in young nulliparous women: a comparative study. Contraception. 2004;69:407–412. doi: 10.1016/j.contraception.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Dijkhuizen K, Dekkers OM, Holleboom CA, et al. Vaginal misoprostol prior to insertion of an intrauterine device: an RCT. Hum Reprod. 2011;26:323–329. doi: 10.1093/humrep/deq348. [DOI] [PubMed] [Google Scholar]
- 12.Edelman AB, Schaefer E, Olson A, et al. Effects of prophylactic misoprostol administration prior to intrauterine device insertion in nulliparous women. Contraception. 2011;84:234–239. doi: 10.1016/j.contraception.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 13.Heikinheimo O, Inki P, Kunz M, et al. Double-blind, randomized, placebo-controlled study on the effect of misoprostol on ease of consecutive insertion of the levonorgestrel-releasing intrauterine system. Contraception. 2010;81:481–486. doi: 10.1016/j.contraception.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 14.Saav I, Aronsson A, Marions L, Stephansson O, Gemzell-Danielsson K. Cervical priming with sublingual misoprostol prior to insertion of an intrauterine device in nulliparous women: a randomized controlled trial. Hum Reprod. 2007;22:2647–2652. doi: 10.1093/humrep/dem244. [DOI] [PubMed] [Google Scholar]
- 15.Turok D, Jacobson J, Simonsen S, Gurtcheff S, Trauscht-Van Horn J, Murphy P. The copper T380A IUD vs. oral levonorgestrel for emergency contraception: a prospective observational study [abstract] Contraception. 2011;84:321. [Google Scholar]
- 16.Andrews GD, French K, Wilkinson CL. Appropriately trained nurses are competent at inserting intrauterine devices: an audit of clinical practice. Eur J Contracept Reprod Health Care. 1999;4:41–44. doi: 10.3109/13625189909043479. [DOI] [PubMed] [Google Scholar]
- 17.Chi IC, Champion CB, Wilkens LR. Cervical dilatation in interval insertion of an IUD. Who requires it and does it lead to a high expulsion rate? Contraception. 1987;36:403–415. doi: 10.1016/0010-7824(87)90089-8. [DOI] [PubMed] [Google Scholar]
- 18.Chi IC, Farr G, Dominik R, Robinson N. Do retroverted uteri adversely affect insertions and performance of IUDs? Contraception. 1990;41:495–506. doi: 10.1016/0010-7824(90)90059-5. [DOI] [PubMed] [Google Scholar]
- 19.Chi IC, Rogers S. Failure to insert an intrauterine device. Contracept Deliv Syst. 1983;4:207–211. [PubMed] [Google Scholar]
- 20.Farmer M, Webb A. Intrauterine device insertion-related complications: can they be predicted? J Fam Plann Reprod Health Care. 2003;29:227–231. doi: 10.1783/147118903101197854. [DOI] [PubMed] [Google Scholar]
- 21.Farr G, Rivera R, Amatya R. Non-physician insertion of IUDs: clinical outcomes among TCu380A insertions in three developing-country clinics. Adv Contracept. 1998;14:45–57. doi: 10.1023/a:1006575610716. [DOI] [PubMed] [Google Scholar]
- 22.Hubacher D, Reyes V, Lillo S, Zepeda A, Chen PL, Croxatto H. Pain from copper intrauterine device insertion: randomized trial of prophylactic ibuprofen. Am J Obstet Gynecol. 2006;195:1272–1277. doi: 10.1016/j.ajog.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 23.Lassner KJ, Chen CH, Kropsch LA, Oberle MW, Lopes IM, Morris L. Comparative study of safety and efficacy of IUD insertions by physicians and nursing personnel in Brazil. Bull Pan Am Health Organ. 1995;29:206–215. [PubMed] [Google Scholar]
- 24.Li YT, Kuo TC, Kuan LC, Chu YC. Cervical softening with vaginal misoprostol before intrauterine device insertion. Int J Gynaecol Obstet. 2005;89:67–68. doi: 10.1016/j.ijgo.2005.01.036. [DOI] [PubMed] [Google Scholar]
- 25.Hubacher D, Finer LB, Espey E. Renewed interest in intrauterine contraception in the United States: evidence and explanation. Contraception. 2011;83:291–294. doi: 10.1016/j.contraception.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Murty J. Use and effectiveness of oral analgesia when fitting an intrauterine device. J Fam Plann Reprod Health Care. 2003;29:150–151. doi: 10.1783/147118903101197539. [DOI] [PubMed] [Google Scholar]