Abstract
The fatty acid binding protein FABP5 shuttles ligands from the cytosol to the nuclear receptor PPARβ/δ (encoded for by Pparδ), thereby enhancing the transcriptional activity of the receptor. This FABP5/PPARδ pathway is critical for induction of proliferation of breast carcinoma cells by activated EGFR. In this study, we show that FABP5 is highly upregulated in human breast cancers and we provide genetic evidence of the pathophysiological significance of FABP5 in mammary tumorigenesis. Ectopic expression of FABP5 was found to be oncogenic in 3T3 fibroblasts where it augmented the ability of PPARδ to enhance cell proliferation, migration and invasion. To determine whether FABP5 was essential for EGFR-induced mammary tumor growth, we interbred FABP5-null mice with MMTV-ErbB2/HER2 oncomice which spontaneously develop mammary tumors. FABP5 ablation relieved activation of EGFR downstream effector signals, decreased expression of PPARδ target genes that drive cell proliferation, and suppressed mammary tumor development. Our findings establish that FABP5 is critical for mammary tumor development, rationalizing the development of FABP5 inhibitors as novel anticarcinogenic drugs.
Keywords: fatty acid binding protein, PPARβ/δ, ErbB2, breast cancer, retinoic acid
INTRODUCTION
The intracellular lipid-binding protein (iLBP) termed fatty acid-binding protein 5 (FABP5, also called keratinocyte FABP5, eFABP, cFABP, or mal1) is upregulated in multiple human cancers including prostate (1-4), head & neck (5), bladder (6), and esophageal (7) cancers as well as in astrocytic glioma (8), glioblastoma (9), and squamous cell carcinoma (10, 11). Similarly, FABP5 is highly upregulated in the FVB/N-Tg(MMTVneu)202Mul/J (MMTV-neu) transgenic mouse model of breast cancer in which Neu/Erb-B2/Her2, encoding for an epidermal growth factor receptor tyrosine kinase, is specifically over-expressed in the mammary epithelium, resulting in spontaneous development of mammary tumors in 100% of female mice (12). The mechanisms that underlie the upregulation of FABP5 in various cancers are incompletely understood. However, we previously showed that, in mammary carcinoma cells, FABP5 expression is controlled by EGFRs through activation of NFκB which directly targets the FABP5 promoter (13). Considering that the EGFR gene HER2/ERBB2/neu is amplified in a significant fraction of human breast cancers, these observation provide at least a partial explanation for upregulation of FABP5 in breast tumors as well as in mammary tumors that arise in the MMTV-neu mouse model. High expression level of FABP5 is correlated with poor patient survival in some cancers (9, 14), and it was shown that the protein displays pro-proliferative and anti-apoptotic activities (13, 15-18). Available information thus suggests that FABP5 may play an important role in promoting tumor development in some cancers.
The iLBPs are members of a family of 15 small (~15 KDa) soluble proteins that include fatty acid binding proteins (FABPs), which associate with long-chain fatty acids and various other lipophilic compounds, and proteins that specifically bind retinoids, including cellular retinol-binding proteins (CRBP I-IV) and cellular retinoic acid (RA) binding proteins (CRABP-I, II) (19). It has been long believed that iLBPs serve a general role in solubilizing and protecting their hydrophobic and often labile ligands in the aqueous milieu of the cytosol. However, it is becoming increasingly clear that these proteins also have specific functions through which they regulate the biological activities of their ligands (reviewed in (20)). The precise nature of the functions of most iLBPs remains to be elucidated but it has been established that several of them cooperate with ligand-activated transcription factors of the nuclear hormone receptor family. It was thus shown that CRABP-II, FABP1, FABP4, and FABP5 transport specific ligands from the cytosol to the nucleus where they directly deliver them to the nuclear receptors RAR, PPARα, PPARγ, and PPARβ/δ (PPARδ) respectively (21-26). These binding proteins thus facilitate the ligation and enhance the transcriptional activity of their cognate receptors. Interestingly, like FABP5, its cognate receptor PPARδ displays distinct prooncogenic activities (27-33). It has been suggested that the receptor exerts such activities in part by decreasing the expression of the tumor suppressor PTEN (32) and by direct induction of the survival factors ILK and PDPK1 (28, 32), the angiogenic factor VEGFa (27, 34), and the pro-oncogenic adipokine ANGPTL4 (33, 35). Hence, the oncogenic activities of FABP5 may stem from its ability to enhance the transcriptional activity of its cognate receptor. Indeed, it was reported that down-regulation of either FABP5 or PPAR/δ inhibits the growth of the highly malignant prostate cancer PC3M cells (18), and abolishes the ability of the EGFR ligand heregulin β1 to enhance proliferation of MCF-7 mammary carcinoma cells (13).
PPARδ displays a broad ligand selectivity and can be activated by a variety of hydrophobic compounds including unsaturated long chain fatty acids (36). It has also been reported that RA, the transcriptionally active metabolite of vitamin A classically known to activate the nuclear receptors RARs, serves as a high affinity natural agonist for PPARδ (16, 17, 37). Like its cognate receptor, FABP5 can associate with multiple types of lipophilic compounds. Interestingly however, in support of the notion that FABP5 and PPARδ cooperate in regulating the transcriptional activity of shared ligands, the binding protein is mobilized to the nucleus only in specific response to ligands that activate this receptor. For example, despite similar binding affinities towards the protein, RA and the synthetic PPARδ-selective agonist GW0742 trigger nuclear translocation of FABP5 but stearic acid, a saturated fatty acid that does not activate PPARδ and synthetic ligands that selectively activate other PPAR isotypes do not (16).
Mammary tumors that arise in MMTV-Erbb2 mice display profound RA-resistance. Hence, while RA exerts anticarcinogenic activities and is currently used in treatment of various human cancers (38), the hormone promotes tumor development in MMTV-Erbb2 mice (17). It has been suggested that this paradoxical response stems from the marked upregulation of FABP5 upon tumorigenesis in these mice, i.e. that the increased expression of the binding protein results in diversion of RA to PPARδ and thus in induction of pro-carcinogenic PPARδ target genes (17).
Here, the involvement of FABP5 in regulating oncogenic properties and mammary tumor development was investigated using cultured cells as well as in the mouse model of breast cancer FVB-Tg(MMTV-Erbb2)NK1Mul/J (MMTV-Erbb2) in which an activated form of Erbb2 is specifically expressed in mammary tissue (39). Similarly to MMTV-Neu mice in which the WT Neu gene is amplified, 100% of MMTVErbb2 female mice develop mammary tumors. MMTV-Erbb2 mice were crossed with FABP-null animals to generate mouse models expressing varying levels of FABP5 and development of tumors in these mice was monitored. The observations indicate that FABP5 enhances the ability of PPARδ to promote oncogenic properties in cultured cells. Moreover, the data show that ablation of FABP5 inhibits the transcriptional activity of PPARδ and dramatically suppresses Erbb2 signaling and tumorigenesis in vivo.
MATERIALS AND METHODS
Ligands
All-trans-RA was purchased from Calbiochem (Millipore Corp), GW0742 was obtained from Toronto research Chemicals, and TTNPB was from Sigma-Aldrich. The PPARδ antagonist PT-S58 was synthesized using the protocol described in (40).
Cells
Human normal mammary epithelial cells (HMEC) were cultured in HMEC ready medium (Invitrogen Life Sciences, Carlsbad, CA). NaF cells, originated from MMTV-neu tumors, were cultured in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (Invitrogen Life Sciences, Carlsbad, CA). 3T3 fibroblasts were passaged fewer than 6-7 times and never grown to confluence. Cell lines stably over-expressing FABP5 or with reduced FABP5 expression were generated by transfecting a vector encoding FABP5 or harboring FABP5shRNA, respectively, using PolyFect transfection reagent (Qiagen). Cells overexpressing FABP5 or FABP5shRNA were selected using G418 (10 mg/ml) and puromycin (10 mg/ml), respectively. Individual colonies were pooled and assessed.
MTT proliferation assay
1000 cells were plated in quadruplicates in a 96-well plate and treated with ligand for 4 days. Cells were incubated with MTT reagent (5 mg/ml in PBS) (Sigma-Aldrich) until the formation of formazan crystals. Crystals were dissolved in 4 mM HCl in isopropanol, and absorbance at 590 nm was measured using a microplate reader.
Binding Assays
Were carried out by fluorescence titrations. FABP5 was bacterially expressed and purified and the equilibrium dissociation constants (Kd) that characterize its interactions with different FAs were measured by fluorescence competition assays. The method entails two steps. In the first step, Kd for the association of the protein with the fluorescent fatty acid probe ANS was measured. Protein (1 μM) was titrated with ANS from a concentrated solution in ethanol. Ligand binding was monitored by following the increase in the fluorescence of the ligand upon binding to the protein, and Kd for the association of ANS with FABP5 was computed from titration curves. Kds for binding of non-fluorescent ligands were then measured by monitoring their ability to compete with ANS for binding to the protein. FABP5 was pre-complexed with ANS at 1:1 molar ratio and titrated with the different FAs whose binding was reflected by a decrease in probe fluorescence. Kds were extracted from the EC50 of the competition curve and the measured Kd for ANS. Analyses were carried out using Origin 8 software (MicroCal Software Inc., Northampton, Mass.).
Quantitative Real-Time PCR (qPCR)
Total RNA was extracted using TRIZOL (Molecular Research Center). cDNA was generated using GeneAmp RNA PCR (Applied Biosystems). qPCR was carried out using TaqMan chemistry and Assays-on-Demand probes (Applied Biosystems). 18s rRNA (4352930) was used for normalization. Relative expression was calculated as 2−ΔΔCT for cell culture experiments and as 2−ΔCT for tumors.
Migration assays
Assays were performed using 8 μm pore size Corning Transwell migration plates following the manufacture's protocol. 104 cells/cm2 of NIH3T3 fibroblasts were plated. Cells in the upper chamber were allowed to migrate for 12 h, the upper portion of the insert was wiped with a cotton swab and inserts were fixed in 4% formalin for 30 min then washed twice with PBS. Cells were then stained with 0.5% crystal violet for 10-15 min, washed twice with PBS, visualized and counted.
Wound healing assays
NIH3T3 fibroblasts cells were grown to 100% confluence and scratched using a 10 μl pipette tip. Cells were washed extensively with PBS to remove floating cells and images were taken at initial 24 h after scratching.
Invasion assays
Assays were performed using BD bioscience invasion assay following manufacture's protocol. Briefly, 5x104 cells/ml were placed in a 24 well plate containing matrigel and grown for 24 h in normal growth media. Medium was aspirated and excess cells removed using a cotton swab. Membranes were then stained using the Diff-Quik staining kit (IMBC Inc), excised, mounted on a microscope slide and cells were counted.
Immunohistochemistry
Antigen retrieval was done by boiling the slides in 10 mM citric buffer (pH 6.0, 15 min). Apoptosis and cell proliferation were examined by immunohistochemical analyses using rabbit polyclonal antibody recognizing cleaved caspase-3 (Cell Signaling, no. 9661; dilution 1:200), and Ki67 (Novocastra Laboratories, no. NCL-Ki67p; dilution 1:500), respectively. Primary antibodies were incubated with deparaffinized sections (overnight at 4oC). Sections were incubated (30 min) with biotinylated secondary antibody and detected with EnVision System-HRP (DAB) (Dako) kit.
Immunoblots
Total protein was extracted from cells or tumor samples using RIPA buffer (25 mM Tris-HCl, pH 7.2, 150 mM NaCl, 1% NP40, 1% sodium deoxycholate, and 0.1% SDS). Proteins were resolved by SDS-PAGE and transferred onto a nitrocellulose membrane. Membranes were incubated with primary antibodies, washed, and incubated with HRP-conjugated antibodies. Proteins were detected by exposure to ECL and visualized on XR-B x-ray film. Band intensities were quantified using ImageJ 1.40g software (Wayen Rasband, NIH,USA). The following antibodies were used: FABP5 antibodies were obtained from R&D Systems (catalog no. AF3077), antibodies against AKT (catalog no. 9272), phospho-AKT (Thr308, catalog no. 4056), ERK1 (catalog no. 4372), phospho-ERK 1/2 (Thr202/Tyr204, catalog no. 9106) and PTEN (catalog no. 9559) were from Cell Signaling Technology. β-tubulin antibodies were from Santa Cruz Biotechnology (catalog no.sc-9104), Connexin26 was purchased from Zymed (catalog no.13-8100), ad antibodies against PDPK1 were from BD Biosciences (catalog no.61107).
Zebrafish maintenance and in vivo zebrafish metastatic assay
Zebrafish (strain AB/TL) were bred and maintained under standard conditions at 28 °C. Morphological features were used to determine the stage of the embryos in hours (hpf) or days (dpf) post fertilization. Embryos used for injection were raised in 1X E3 medium in the presence of 200 μM 1-phenyl-2-thiourea (PTU; Sigma) to inhibit pigmentation.
NaF cells stably expressing control shRNA or FABP5shRNA were trypsinized, washed and stained with the fluorescent cell membrane dye CM-DiO (Vibrant, Invitrogen). Labeled cells were resuspended in PBS (150 cells/4 nl) containing 0.5% phenol red in PBS (Sigma). Cells were then injected into the yolk sac of 2 dpf dechorionated zebrafish embryos, using a manual micro-injector (Pressure-pulsed micro injector Model PV830; World Precision Instruments, Sarasota, FL) according to the method described in Marques et al., 2009. Fish with fluorescent cells outside the implantation area at 2 hr post injection were excluded from further analysis. All other fish were maintained at 28 °C for 4 days in 1X E3 medium containing PTU and analyzed. Microscopy was performed using Zeiss AxioCam MR camera attached to a Zeiss Axioplan 2 fluorescence microscope (GFP filter set: excitation 488, emission 530; Samrock, Rochester, NY) (Imaging Core Facility of the Genetics Department at CWRU) at a magnification of 5-40X. Experiments were repeated four times with 10-15 fish per condition.
Mice studies
Mice were housed according to ARC protocol and IACUC regulations. Mice were maintained on a 12 hours light and dark cycle on a normal chow diet. The mice had access to water and diet ad libitum. FVB/N-Tg(MMTV-Erbb2)1Led (Jackson Laboratories, stock no. 005038) mice, homozygous for the Erbb2 transgene were crossed with C57BL/6-FABP5−/− mice, generously provided by Gökhan S. Hotamisligil (41). F1 mice were bred with FABP5+/− females to yield MMTV-Erbb2+/−/FABP5+/+ (M5+/+), MMTV-Erbb2+/−/FABP5+/− (M5+/−), and MMTV-Erbb2+/−/FABP5−/− (M5−/−) littermates. All experiments were performed using virgin females. Tumor development was monitored by measuring the length and width with calipers and tumor volume calculated as length × width2/2. Statistical analyses of tumor growth curves were performed on the natural log of tumor volumes in the two groups and compared to the WT with unpaired t-test using Origin 8.5.1 software.
RESULTS
Expression of FABP5 is upregulated in breast cancers
Similarly to the marked upregulation of FABP5 that accompanies mammary tumor development in the MMTV-neu mouse model of breast cancer (17), examination of expression array profiles of human breast tumors deposited in the OncomineTM DataBase (https://www.oncomine.org/) indicated that the expression level of FABP5 was found to be elevated in human breast tumors in two independent studies (Fig. 1a). In accordance, analysis of FABP5 mRNA levels in cDNA arrays of human breast cancer samples (OriGene) showed that FABP5 is markedly upregulated in early stage of breast cancer and remains high through disease progression (Fig 1b).
Figure 1. FABP5 is upregulated in human breast tumors.
a) Levels of FABP5 mRNA in samples of normal human breast and invasive breast carcinoma reported in: The Cancer Genome Atlas - Invasive Breast Carcinoma Gene Expression Data (https://tcga-data.nci.nih.gov/tcga/) and (52). Data were obtained from OncomineTM (Compedia Bioscience, Ann Arbor, Michigan). b) Analysis of TissueScanTM tissue qPCR array consisting of cDNA derived from samples of normal breast and denoted stages of breast tumors (OriGene). FABP5 expression was normalized to 18s and calibrated to the mean mRNA level in normal tissue (grey bars).
FABP5 promotes cell proliferation, migration, and invasion by enhancing the transcriptional activity of PPARδ
Two types of cells were used to examine whether FABP5 is involved in regulating mammary carcinoma cell growth: NaF cells, a cell line generated from mammary tumors that arise in MMTV-neu mice which expresses a high level of FABP5, and normal human mammary epithelium cells which display a low expression level of the protein (HMEC, Fig 2a). An NaF cell line in which FABP5 expression is stably reduced was generated (Fig. 2b). Reducing the expression of FABP5 markedly suppressed the proliferation of these cells (Fig 2c). Conversely, ectopic over-expression of FABP5 in HMEC (Fig. 2d) facilitated their growth (Fig. 2e). The effect of FABP5 on cell growth was further assessed using 3T3 fibroblasts, cells that have long been used as a model for investigating processes underlying oncogenic transformation (42). Two 3T3 clones that overexpress different levels of FABP5 were generated (Fig. 2f) and their rates of proliferation measured using MTT assays. Similarly to the response of HMEC, over-expression of FABP5 facilitated the proliferation of 3T3 cells and did so in a dose-responsive fashion (Fig. 2g).
Figure 2. FABP5 promotes cell proliferation and invasion.
a) Expression levels of FABP5 in normal human breast epithelial cells (HMEC) and in NaF mammary carcinoma cells, derived from a tumor that arose in the MMTV-neu mouse model of breast cancer. b) Immunoblot demonstrating reduced level of FABP5 in NaF cells stably expressing FABP5shRNA. c) Proliferation of NaF cells stably expressing empty vector (e.v.) or FABP5shRNA. d) Levels of FABP5 mRNA in HMEC cells transfected with e.v. or a vector encoding FABP5. Inset: Immunoblot demonstrating higher levels of FABP5 in HMEC cells overexpressing FABP5. e) Rate of growth of HMEC cells expressing e.v. or vector encoding FABP5. f) Levels of FABP5 mRNA in NIH3T3 fibroblasts expressing e.v., and in two NIH3T3 cell lines stably over-expressing FABP5 (F5-1, F5-2). Inset: immunoblots demonstrating expression levels of FABP5 in the NIH3T3 lines. g) Proliferation of NIH3T3 cells stably expressing varying levels of FABP5, measured by MTT assays. h) Representative images of zebrafish embryos injected into the yolk sac (YS) with NaF cells stably expressing control shRNA (Ctrlsh, upper panels) or shRNA directed towards FABP5 (FABP5shRNA, lower panels). Cells were stained with the fluorescent cell membrane dye CM-DiO and injected into the yolk sac of 2 dpf dechorionated zebrafish embryos (Marques et al., 2009). Fish were imaged 4 days later (see Experimental Procedures). Left panels: merge of light and fluorescent images of a whole zebrafish. Middle panels: merge of light and fluorescent images of zebrafish tails. Right panels: fluorescent images of zebrafish tails. The images show massive invasion into the tail by control cells (arrow in upper panels). Cells with reduced expression of FABP5 remained in the yolk sac and did not metastasize. Experiments were repeated four times with 10-15 fish per condition. Magnification 5x. i) Left: “Wound healing” assays using 3T3 cells stably expressing varying levels of FABP5. Images were obtained immediately following and 24 h. after scratching. Right: wound widths, quantified using image J software. Data are mean±S.D. (n=3).
The effect of reducing the expression of FABP5 in NaF cells on their metastatic potential was evaluated in vivo using a recently developed zebrafish embryo model of cell invasion (43, 44). Embryos were raised in medium containing 1-phenyl-2-thiourea (PTU) to inhibit pigmentation. NaF cells or counterparts with reduced expression of FABP5 (Fig. 2b) were stained with the fluorescent cell membrane dye CM-DiO (Vibrant, Invitrogen) and injected into the yolk sac of 2 dpf dechorionated zebrafish embryos (see Experimental Procedures for details). Fish with fluorescent cells outside the implantation area at 2 h post injection were excluded from further analysis. Fish were maintained for 4 days prior to fluorescence microscopy imaging (Fig. 2h). Control NaF cells efficiently exited the yolk sac and many of them were found along the embryo body (Fig 2h, upper panels). In contrast, cells that express a low level of FABP5 remained in the yolk sac and very few were observed in the embryo tail (Fig 2h, lower panels). Hence, expression of FABP5 markedly enhanced the metastatic potential of the cells. Further attesting to an involvement of FABP5 in promoting oncogenic properties, “wound healing” assays showed that ectopic overexpression of FABP5 in 3T3 fibroblasts facilitated the wound closure behavior of the cells and did so in a dose-dependent manner (Fig 2i).
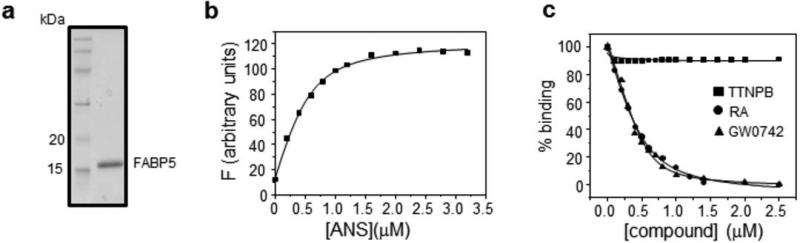
The only known specific activity of FABP5 is the delivery of ligands to the nuclear receptor PPARδ, an activity through which the binding protein facilitates the ligation and thus enhances the activation of the receptor (13, 18, 26). The observations that FABP5 affects cellular behavior in the absence of added ligands likely reflect the presence of endogenous agonists for the receptor. Notably, the ligand selectivity of PPARδ is quite broad and the receptor can be activated by multiple endogenous compounds including RA and various unsaturated long chain fatty acids. As cells were cultured in 5% (3T3) or 10% (NaF, HMEC) FBS which contains ~0.05 or ~0.1 μM retinol, the precursor for RA, as well as long chain fatty acids, the presence of these compounds accounts for the activity of the FABP5/ PPARδ pathway in the absence of added ligands. In order to examine the effect of defined exogenously-added compounds, the association of FABP5 with several ligands was assessed. The protein was expressed in E. coli and purified (Fig. 3a) and the equilibrium dissociation constants (Kd) that characterize its association with ligands were measured by fluorescence competition assays utilizing the fluorescent probe anilinonaphtalene-8-sulphonic acid (ANS). The method entails two steps (45). In the first step, Kd for association of the protein with ANS was measured by fluorescence titrations. Titration with ANS resulted in a saturable increase in fluorescence (Fig. 3b), and analysis of titration curves (46) yielded a Kd 70±6.4 nM. Kds for non-fluorescent ligands were then measured by monitoring their ability to compete with the probe for binding. FABP5 was pre-complexed with ANS and titrated with a non-fluorescent ligand whose binding was reflected by a decrease in fluorescence upon displacement of the probe from the protein. Association of FABP5 with the synthetic PPARδ-selective ligand GW0742, the natural PPARδ ligand RA (16, 37), and the pan-RAR ligand TTNPB (4-[(E)-2-(5,6,7,8-Tetrahydro-5,5,8,8-tetramethyl-2-naphthalenyl)-1-propenyl]benzoic acid) was thus examined (Fig. 3c). Kds for GW0742 and RA, extracted from the EC50 of competition curves and the measured Kd for the probe, were found to be 38.4±8.2 and 42.3±6.4 nM, respectively. While displaying a high affinity towards these PPARδ ligands, FABP5 did not associate with TTNPB (Fig. 3c), demonstrating the specific common ligand selectivity of the binding protein and its cognate receptor.
Figure 3. FABP5 binds GW0742 and RA but not TTNPB.
a) Recombinant mFABP5 expressed in E. coli and purified was resolved by SDS-PAGE and visualized by Coomassie-blue staining. b) Fluorescence titration of FABP5. Protein (1 μM) was titrated with ANS and probe fluorescence was monitored. Data were fit to obtain Kd. c) Association of FABP5 with RA, GW0742 and TTNPB was assessed by fluorescence competition titrations. FABP5 was pre-complexed with ANS and titrated with non-fluorescent ligands.
3T3 fibroblasts with varying expression levels of FABP5 (Fig. 2f) were used to further examine whether PPARδ is involved in the oncogenic activities of FABP5. In accordance with the reports that this receptor promotes cell growth and survival (27-30), treatment with the selective PPARδ agonist GW0742 facilitated proliferation of 3T3 cells (Fig. 4a). The ligand also enhanced the ability of the cells to migrate through a membrane in transwell migration assays (Fig. 4b), and to translocate through a Matrigel matrix in invasion assays (Fig. 4c). Indicating that 3T3 cells contain endogenous ligands for PPARδ, increasing the expression of FABP5 per se enhanced cell proliferation, migration, and invasion and did so in a dose-dependent manner. Increasing the expression of FABP5 markedly potentiated the ability of ectopically added GW0742 to induce proliferation, migration, and invasion (Fig. 4a-4c). In keeping with the reports that RA serves as a ligand for PPARδ and that, like other PPARδ ligands, it is delivered to the receptor by FABP5 (16, 37), RA mirrored the effects of the synthetic PPARδ ligand in enhancing proliferation, migration and invasion of 3T3 cells, and overexpression of FABP5 enhanced the effects in a dose-dependent fashion (Fig. 4d-4f). Unlike RA and GW0742, the synthetic pan-RAR ligand TTNPB had little effect on these parameters of cell behavior (Fig. 4d-4f), substantiating that the pro-oncogenic activity of RA in these cells is mediated by FABP5 and its cognate receptor PPARδ and not by the classical RA receptor RAR.
Figure 4. FABP5 promotes oncogenic properties in NIH3T3 fibroblasts by enhancing the transcriptional activity of PPARβ/δ.
a) Proliferation of NIH3T3 cells stably expressing varying levels of FABP5 and treated with the PPARβ/δ-selective agonist GW0742 (1 μM, 4 days), assessed by MTT assays. b) Migration assays using NIH3T3 cells stably expressing varying levels of FABP5 and treated with GW0742 (1 μM, 24 h). c) Invasion assays using NIH3T3 cells stably expressing varying levels of FABP5 and treated with GW0742 (1 μM, 24 h). d)-f) proliferation (d) migration (e) and invasion (f) of 3T3 cell lines treated with retinoic acid (RA) or the pan-RAR agonist TTNPB (1 μM) as in panels b)-d). *p denotes values vs. non-treated 3T3 cells expressing an empty vector (e.v.). g) Levels of Pdpk1 and Plin2 mRNA in 3T3 cells stably expressing varying levels of FABP5 in the absence or presence of the PPARδ antagonist PTS58 (2 μM, 6h). ‡p=0.03; ‡‡p= 0.00004; #p=0.006; ##p=0.000009. h) Proliferation of 3T3 cells stably expressing varying levels of FABP5 and treated with denoted ligands (1 μM, 4 days) in the presence or absence of PTS58 (2 μM), assessed by MTT assays. Data are mean±SD from 3 independent experiments. Statistical analyses were carried out using two-tailed Student's t-test.
The synthetic PPARδ-selective antagonist PT-S58 (47) was then used to further examine the involvement of PPARδ in the pro-oncogenic activities of FABP5. In keeping with its function in enhancing the transcriptional activity of the receptor, over-expression of FABP5 increased the levels of two well-established PPARδ-target genes, Pdpk1 and Plin2 (Fig. 4g). Treatment with PT-S58 decreased the expression of both genes and abrogated the effect of FABP5 on their expression (Fig. 4g). Strikingly, PT-S58 completely abolished the ability of FABP5 to facilitate cell proliferation both in the absence and in the presence of added PPARδ ligands (Fig. 4h). Taken together, the data establish that pro-oncogenic activities of FABP5 are critically mediated by PPARδ and emanate from its ability to enhance the transcriptional activity of the receptor.
Ablation of FABP5 suppresses ErbB2-induced mammary tumor development in vivo
The MMTV-Erbb2 transgenic mouse model of breast cancer (39) was used to examine the effect of FABP5 expression on mammary tumor development in vivo. To generate MMTV-Erbb2 mice models with varying expression levels of FABP5, MMTVErbb2 mice were crossed with FABP5-null mice (41) to obtain MMTV- Erbb2+/−/FABP5+/+ (M5+/+), MMTV-Erbb2+/−/FABP5+/− (M5+/−), and MMTV-Erbb2+/−/FABP5−/−(M5−/−) mice. Monitoring tumor development in these mice showed that animals with reduced expression of FABP5 developed tumors at a dramatically slower rate than control MMTV-Erbb2+/− mice and, notably, that the rate of tumor development correlated with the expression level of the binding protein (Fig. 5a). Survival of the mice, defined as the age at which the first tumor to arise reached a volume of 1200 mm3, was markedly longer in M5−/− vs. control mice and M5+/− mice displayed an intermediate survival rate (Fig. 5b). The differential tumor growth in these groups is exemplified by assessing tumor volumes at 59 weeks of age (Fig. 5c). At this age, all M5+/+ had large tumors while only one M5−/− mouse had a discernible tumor which was quite small. M5+/+ mice also displayed a higher number of tumors per animal (Fig. 5d) as compared with mice with reduced expression of FABP5, with M5+/− mice bearing an intermediate number of tumors per mouse. Strikingly, while tumors developed in 100% of mice in the control group, 3 out of 15 M5+/−, and 6 out of 14 M5−/− mice remained tumor-free throughout the experiment (Fig. 5d).
Figure 5. Ablation of FABP5 suppresses mammary tumor growth in vivo.
a) Time course of tumor development in M5+/+ (n=15), M5+/− (n=14), and M5−/− (n=14) mice. Development of the first tumor to appear in each mouse was monitored by measuring its length and width, and tumor volume calculated as length × width2/2. Data are mean±S.E.M. Inset: immunoblots of FABP5 in tumors that developed in three individual M5−/−, M5+/− and M5+/+ mice. b) Kaplan-Meier analysis of survival of M5+/+, M5+/−, and M5−/− mice. Mice were sacrificed when their largest tumors reached a volume of 1200 mm3. Surviving M5+/−, and M5−/− mice had no measurable tumors at termination of the experiments. c) Scatter plots of volume of tumors measured as in (c) at age 59 weeks. Horizontal grey lines indicate the mean in each group. d) Scatter plots of the number of tumors/mouse found at termination of the experiment as indicated in (d). Horizontal lines indicate the mean in each group. e) Immunostaining of the proliferation marker Ki67 and the apoptosis marker cleaved caspase 3 in tumors that arose in M5+/+, M5+/−, and M5−/− mice. (Scale bars: 50 μm).
Consistent with the behavior of cultured cells, immunostaining for the proliferation marker Ki67 showed that reduced expression of FABP5 was associated with a dose-responsive decrease in proliferation in tumors (Fig. 5e). On the other hand, the fraction of apoptotic cells, evaluated by immunostaining for cleaved caspase 3, was higher in mammary tumors of mice with reduced expression of FABP5 compared to the MMTV-Erbb2 controls (Fig. 5e).
Ablation of FABP5 diminishes ErbB2-induced signaling and attenuates the transcriptional activity of PPARδ in vivo
It was previously reported that reducing the expression of FABP5 abolishes the ability of the EGFR ligand hertegulin β1 to enhance the proliferation of MCF-7 mammary carcinoma cells (13). EGFRs, e.g. Erbb2, can promote cell growth through activation of a signaling network that includes pathways that are mediated by ERK and PI3 kinase and its downstream effector the survival factor AKT (48, 49). Examination of the activation status of these pathways revealed that the reduced expression of FABP5 in M5+/− and M5−/− tumors resulted in decreased phosphorylation levels of both ERK (Fig. 6a) and AKT (Fig. 6b), suggesting that the oncogenic activity of the FABP5/ PPARδ pathway in these tumors emanates at least in part through promotion of EGFR signaling. The reduced expression of FABP5 in M5+/− and M5−/− tumors also resulted in a dose-responsive upregulation of connexin 26 (CNX26 Fig. 6c), a protein that was reported to function as a tumor suppressor in mammary carcinomas (50).
Figure 6. Ablation of FABP5 diminishes ErbB2-induced proliferative signaling and attenuates the transcriptional activity of PPAR □In vivo.
a)-c) Upper panels: immumoblots demonstrating phosphorylation status of ERK (a), phosphorylation status of AKT (b), and expression level of CNX26 (c) in tumors of three individual M5+/+, M5+/−, and M5−/− mice. Lower panels: quantitation of immunoblots. Data are mean±S.D. p values for differences between denoted groups and respective M mice were calculated by a two-tail Student's t-test. d) Levels of mRNA for the direct PPAR~target gene VEGFa in tumors of three individual M5+/+, M5+/−, and M5−/− mice. Mean±S.D. p values vs. M5+/+ tumors are shown. e) Left: immunoblots of PDPK1, encoded by the direct PPAR~target gene pdpk1, and PTEN, whose expression is suppressed by PPARβ/δ, in tumors of three individual M5+/+, M5+/−, and M5−/− mice. Right: quantitation of immunoblots. Mean±S.D. *p vs. respective M mice, and **p vs. M5+/− mice are shown.
In accordance with the cooperation of FABP5 with PPARδ, the expression levels of two direct PPARδ target genes involved in mediating oncogenic activities of the receptor, the growth factor VEGFa (27, 34) and the survival factor PDPK1 (28, 29), were lower in tumors that arose in MMTV-Erbb2 mice with reduced expression of FABP5 as compared to tumors of control mice (Fig. 6d, 6e). Notably, the expression of these genes correlated in dose responsive manner with the expression of FABP5, showing an intermediate level in FABP5+/− tumors. Further indicating that lack of FABP5 impairs the activity of PPARδ, PTEN, a tumor suppressor whose expression is repressed by this receptor (28), was upregulated in FABP5−/− tumors (Fig. 6e).
DISCUSSION
The data presented above indicate that expression of FABP5 is upregulated early in breast tumor development and remains high throughout disease progression. The observations thus add another cancer to the list of human cancers in which tumorigenesis is accompanied by a high level of expression of this binding protein (1-11). The observations further show that reducing the expression of FABP5 in NaF mammary carcinoma cells dramatically reduces their rate of proliferation and metastatic potential. Furthermore, ectopic over-expression of FABP5 in normal mammary epithelium cells or in 3T3 fibroblasts enhanced their proliferation, and, in 3T3 cells, facilitated “wound closure” in scratch assays. Considering that the only known specific activity of FABP5 is the delivery of ligands to PPARδ (13, 18, 26), and that it was reported that PPARδ promotes cell migration, proliferation and survival (27-32), the oncogenic activities of the binding protein are likely to stem from its ability to enhance the transcriptional activity of the receptor. In accordance, ectopic expression of FABP5 enhanced the ability of endogenous ligands and two exogenously-added agonists, the synthetic PPARβ/δ-selective ligand GW0742 and the natural PPARδ ligand RA, to promote proliferation, migration and invasion of 3T3 fibroblasts and the activity was completely abolished in the presence of a PPARδ antagonist. To examine whether the FABP5/ PPARδ pathway is involved in mammary tumor development in vivo, we generated MMTV-Erbb2 mouse models of breast cancer expressing varying levels of FABP5. Monitoring mammary tumor growth revealed that ablation of FABP5 markedly suppressed tumor development in these mice. While tumors rapidly developed in all M5+/+ mice, tumor growth was dramatically delayed in mice with reduced expression of FABP5 and 20% of M5+/− mice, and 43% of M5−/− mice remained tumor-free throughout the 504 days of the experiment. In agreement with the report that FABP5 is a critical mediator of the pro-proliferative activities of EGFR signaling (13), the phosphorylation/activation status of two downstream effectors of HER2/Erbb2, the mitogenic kinase ERK and the survival factor AKT, was markedly reduced in M5−/− tumors. In contrast, the level of the tumor suppressor CNX26, whose expression decreases upon EGFR activation, was higher in tumors with reduced FABP5 levels. Finally, in accordance with the function of the binding protein in enhancing the transcriptional activity of PPARδ, expression of the PPARδ target genes PDPK1 and VEGFa was lower and that of the PPARδ-repressed tumor suppressor gene PTEN was higher in tumors with reduced FABP5 expression.
Taken together with previous reports, the findings described here show that FABP5 efficiently promotes tumor development and that it does so by activating PPARδ. It is noteworthy that PPARδ agonists are currently being tested in clinical trials for treatment of metabolic diseases (51). The observations that the FABP5/PPARδ pathway displays potent pro-oncogenic activities indicate that such agonists should be carefully assessed prior to clinical utilization. The present observations suggest that the pathway is a promising druggable target for counteracting oncogenic activities in the many human cancers in which the expression of FABP5 is upregulated. Hence, inhibitors of FABP5 may comprise a novel class of potent anticarcinogenic agents.
Acknowledgements
We are grateful to Gökhan S. Hotamisligil (Harvard School of Public Health) for sharing his FABP5−/− mice and to Philip Leder (Harvard Medical School) for the NaF mammary carcinoma cells.
Grant Support: This work was supported by NIH grant R01 DK060684 to NN. MKD was supported by NIH training grant R25-CA148052.
This work was supported by NIH grant RO1-DK060684 to NN. MKD was supported by NIH training grant R25-CA148052.
Footnotes
The authors declare that they do not have any conflict of interest with the work described in this manuscript
REFERENCES
- 1.Pang J, Liu WP, Liu XP, Li LY, Fang YQ, Sun QP, et al. Profiling protein markers associated with lymph node metastasis in prostate cancer by DIGE-based proteomics analysis. Journal of proteome research. 2010;9:216–26. doi: 10.1021/pr900953s. [DOI] [PubMed] [Google Scholar]
- 2.Alshalalfa M, Bismar TA, Alhajj R. Detecting cancer outlier genes with potential rearrangement using gene expression data and biological networks. Advances in bioinformatics. 2012;2012:373506. doi: 10.1155/2012/373506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adamson J, Morgan EA, Beesley C, Mei Y, Foster CS, Fujii H, et al. High-level expression of cutaneous fatty acid-binding protein in prostatic carcinomas and its effect on tumorigenicity. Oncogene. 2003;22:2739–49. doi: 10.1038/sj.onc.1206341. [DOI] [PubMed] [Google Scholar]
- 4.Morgan EA, Forootan SS, Adamson J, Foster CS, Fujii H, Igarashi M, et al. Expression of cutaneous fatty acid-binding protein (C-FABP) in prostate cancer: potential prognostic marker and target for tumourigenicity-suppression. International journal of oncology. 2008;32:767–75. [PubMed] [Google Scholar]
- 5.Han J, Kioi M, Chu WS, Kasperbauer JL, Strome SE, Puri RK. Identification of potential therapeutic targets in human head & neck squamous cell carcinoma. Head & neck oncology. 2009;1:27. doi: 10.1186/1758-3284-1-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen R, Feng C, Xu Y. Cyclin-dependent kinase-associated protein Cks2 is associated with bladder cancer progression. The Journal of international medical research. 2011;39:533–40. doi: 10.1177/147323001103900222. [DOI] [PubMed] [Google Scholar]
- 7.Ogawa R, Ishiguro H, Kuwabara Y, Kimura M, Mitsui A, Mori Y, et al. Identification of candidate genes involved in the radiosensitivity of esophageal cancer cells by microarray analysis. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus / ISDE. 2008;21:288–97. doi: 10.1111/j.1442-2050.2007.00759.x. [DOI] [PubMed] [Google Scholar]
- 8.Campos B, Centner FS, Bermejo JL, Ali R, Dorsch K, Wan F, et al. Aberrant expression of retinoic acid signaling molecules influences patient survival in astrocytic gliomas. The American journal of pathology. 2011;178:1953–64. doi: 10.1016/j.ajpath.2011.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barbus S, Tews B, Karra D, Hahn M, Radlwimmer B, Delhomme N, et al. Differential retinoic acid signaling in tumors of long- and short-term glioblastoma survivors. Journal of the National Cancer Institute. 2011;103:598–606. doi: 10.1093/jnci/djr036. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe R, Fujii H, Yamamoto A, Hashimoto T, Kameda K, Ito M, et al. Immunohistochemical distribution of cutaneous fatty acid-binding protein in human skin. Journal of dermatological science. 1997;16:17–22. doi: 10.1016/s0923-1811(97)00615-4. [DOI] [PubMed] [Google Scholar]
- 11.Masouye I, Saurat JH, Siegenthaler G. Epidermal fatty-acid-binding protein in psoriasis, basal and squamous cell carcinomas: an immunohistological study. Dermatology. 1996;192:208–13. doi: 10.1159/000246367. [DOI] [PubMed] [Google Scholar]
- 12.Guy CT, Webster MA, Schaller M, Parsons TJ, Cardiff RD, Muller WJ. Expression of the neu protooncogene in the mammary epithelium of transgenic mice induces metastatic disease. Proceedings of the National Academy of Sciences of the United States of America. 1992;89:10578–82. doi: 10.1073/pnas.89.22.10578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kannan-Thulasiraman P, Seachrist DD, Mahabeleshwar GH, Jain MK, Noy N. Fatty acid-binding protein 5 and PPARbeta/delta are critical mediators of epidermal growth factor receptor-induced carcinoma cell growth. The Journal of biological chemistry. 2010;285:19106–15. doi: 10.1074/jbc.M109.099770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu RZ, Graham K, Glubrecht DD, Germain DR, Mackey JR, Godbout R. Association of FABP5 expression with poor survival in triple-negative breast cancer: implication for retinoic acid therapy. The American journal of pathology. 2011;178:997–1008. doi: 10.1016/j.ajpath.2010.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta S, Pramanik D, Mukherjee R, Campbell NR, Elumalai S, Dewilde RF, et al. Molecular Determinants of Retinoic Acid Sensitivity in Pancreatic Cancer. Clin Cancer Res. 2011 doi: 10.1158/1078-0432.CCR-11-2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schug TT, Berry DC, Shaw NS, Travis SN, Noy N. Opposing effects of retinoic acid on cell growth result from alternate activation of two different nuclear receptors. Cell. 2007;129:723–33. doi: 10.1016/j.cell.2007.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schug TT, Berry DC, Toshkov IA, Cheng L, Nikitin AY, Noy N. Overcoming retinoic acid-resistance of mammary carcinomas by diverting retinoic acid from PPARbeta/delta to RAR. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:7546–51. doi: 10.1073/pnas.0709981105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morgan E, Kannan-Thulasiraman P, Noy N. Involvement of Fatty Acid Binding Protein 5 and PPARbeta/delta in Prostate Cancer Cell Growth. PPAR Res. 2010:2010. doi: 10.1155/2010/234629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smathers RL, Petersen DR. The human fatty acid-binding protein family: evolutionary divergences and functions. Human genomics. 2011;5:170–91. doi: 10.1186/1479-7364-5-3-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Storch J, Corsico B. The emerging functions and mechanisms of mammalian fatty acid-binding proteins. Annual review of nutrition. 2008;28:73–95. doi: 10.1146/annurev.nutr.27.061406.093710. [DOI] [PubMed] [Google Scholar]
- 21.Hostetler HA, Balanarasimha M, Huang H, Kelzer MS, Kaliappan A, Kier AB, et al. Glucose regulates fatty acid binding protein interaction with lipids and peroxisome proliferator-activated receptor alpha. Journal of lipid research. 2010;51:3103–16. doi: 10.1194/jlr.M005041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayers SD, Nedrow KL, Gillilan RE, Noy N. Continuous nucleocytoplasmic shuttling underlies transcriptional activation of PPARgamma by FABP4. Biochemistry. 2007;46:6744–52. doi: 10.1021/bi700047a. [DOI] [PubMed] [Google Scholar]
- 23.Budhu A, Gillilan R, Noy N. Localization of the RAR interaction domain of cellular retinoic acid binding protein-II. J Mol Biol. 2001;305:939–49. doi: 10.1006/jmbi.2000.4340. [DOI] [PubMed] [Google Scholar]
- 24.Budhu AS, Noy N. Direct channeling of retinoic acid between cellular retinoic acid-binding protein II and retinoic acid receptor sensitizes mammary carcinoma cells to retinoic acid-induced growth arrest. Molecular and cellular biology. 2002;22:2632–41. doi: 10.1128/MCB.22.8.2632-2641.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dong D, Ruuska SE, Levinthal DJ, Noy N. Distinct roles for cellular retinoic acid-binding proteins I and II in regulating signaling by retinoic acid. The Journal of biological chemistry. 1999;274:23695–8. doi: 10.1074/jbc.274.34.23695. [DOI] [PubMed] [Google Scholar]
- 26.Tan NS, Shaw NS, Vinckenbosch N, Liu P, Yasmin R, Desvergne B, et al. Selective cooperation between fatty acid binding proteins and peroxisome proliferator-activated receptors in regulating transcription. Molecular and cellular biology. 2002;22:5114–27. doi: 10.1128/MCB.22.14.5114-5127.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang D, Wang H, Guo Y, Ning W, Katkuri S, Wahli W, et al. Crosstalk between peroxisome proliferator-activated receptor delta and VEGF stimulates cancer progression. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:19069–74. doi: 10.1073/pnas.0607948103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Di-Poi N, Tan NS, Michalik L, Wahli W, Desvergne B. Antiapoptotic role of PPARbeta in keratinocytes via transcriptional control of the Akt1 signaling pathway. Molecular cell. 2002;10:721–33. doi: 10.1016/s1097-2765(02)00646-9. [DOI] [PubMed] [Google Scholar]
- 29.Di-Poi N, Michalik L, Tan NS, Desvergne B, Wahli W. The anti-apoptotic role of PPARbeta contributes to efficient skin wound healing. J Steroid Biochem Mol Biol. 2003;85:257–65. doi: 10.1016/s0960-0760(03)00215-2. [DOI] [PubMed] [Google Scholar]
- 30.Wagner KD, Benchetrit M, Bianchini L, Michiels JF, Wagner N. Peroxisome proliferator-activated receptor beta/delta (PPARbeta/delta) is highly expressed in liposarcoma and promotes migration and proliferation. The Journal of pathology. 2011;224:575–88. doi: 10.1002/path.2910. [DOI] [PubMed] [Google Scholar]
- 31.Tan NS, Icre G, Montagner A, Bordier-ten-Heggeler B, Wahli W, Michalik L. The nuclear hormone receptor peroxisome proliferator-activated receptor beta/delta potentiates cell chemotactism, polarization, and migration. Molecular and cellular biology. 2007;27:7161–75. doi: 10.1128/MCB.00436-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan NS, Michalik L, Noy N, Yasmin R, Pacot C, Heim M, et al. Critical roles of PPAR beta/delta in keratinocyte response to inflammation. Genes & development. 2001;15:3263–77. doi: 10.1101/gad.207501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adhikary T, Brandt DT, Kaddatz K, Stockert J, Naruhn S, Meissner W, et al. Inverse PPARbeta/delta agonists suppress oncogenic signaling to the ANGPTL4 gene and inhibit cancer cell invasion. Oncogene. 2012 doi: 10.1038/onc.2012.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fauconnet S, Lascombe I, Chabannes E, Adessi GL, Desvergne B, Wahli W, et al. Differential regulation of vascular endothelial growth factor expression by peroxisome proliferator-activated receptors in bladder cancer cells. The Journal of biological chemistry. 2002;277:23534–43. doi: 10.1074/jbc.M200172200. [DOI] [PubMed] [Google Scholar]
- 35.Tan MJ, Teo Z, Sng MK, Zhu P, Tan NS. Emerging roles of angiopoietin-like 4 in human cancer. Molecular cancer research : MCR. 2012;10:677–88. doi: 10.1158/1541-7786.MCR-11-0519. [DOI] [PubMed] [Google Scholar]
- 36.Desvergne B, Wahli W. Peroxisome proliferator-activated receptors: nuclear control of metabolism. Endocr Rev. 1999;20:649–88. doi: 10.1210/edrv.20.5.0380. [DOI] [PubMed] [Google Scholar]
- 37.Shaw N, Elholm M, Noy N. Retinoic acid is a high affinity selective ligand for the peroxisome proliferator-activated receptor beta/delta. The Journal of biological chemistry. 2003;278:41589–92. doi: 10.1074/jbc.C300368200. [DOI] [PubMed] [Google Scholar]
- 38.Soprano DR, Qin P, Soprano KJ. Retinoic Acid Receptors and Cancers. Annual review of nutrition. 2004;24:201–21. doi: 10.1146/annurev.nutr.24.012003.132407. [DOI] [PubMed] [Google Scholar]
- 39.Muller WJ, Sinn E, Pattengale PK, Wallace R, Leder P. Single-step induction of mammary adenocarcinoma in transgenic mice bearing the activated c-neu oncogene. Cell. 1988;54:105–15. doi: 10.1016/0092-8674(88)90184-5. [DOI] [PubMed] [Google Scholar]
- 40.Toth PM, Naruhn S, Pape VF, Dorr SM, Klebe G, Muller R, et al. Development of improved PPARbeta/delta inhibitors. ChemMedChem. 2012;7:159–70. doi: 10.1002/cmdc.201100408. [DOI] [PubMed] [Google Scholar]
- 41.Maeda K, Uysal KT, Makowski L, Gorgun CZ, Atsumi G, Parker RA, et al. Role of the fatty acid binding protein mal1 in obesity and insulin resistance. Diabetes. 2003;52:300–7. doi: 10.2337/diabetes.52.2.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muchardt C, Yaniv M. The mammalian SWI/SNF complex and the control of cell growth. Seminars in cell & developmental biology. 1999;10:189–95. doi: 10.1006/scdb.1999.0300. [DOI] [PubMed] [Google Scholar]
- 43.Marques IJ, Weiss FU, Vlecken DH, Nitsche C, Bakkers J, Lagendijk AK, et al. Metastatic behaviour of primary human tumours in a zebrafish xenotransplantation model. BMC cancer. 2009;9:128. doi: 10.1186/1471-2407-9-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jelassi B, Chantome A, Alcaraz-Perez F, Baroja-Mazo A, Cayuela ML, Pelegrin P, et al. P2X(7) receptor activation enhances SK3 channels- and cystein cathepsin-dependent cancer cells invasiveness. Oncogene. 2011;30:2108–22. doi: 10.1038/onc.2010.593. [DOI] [PubMed] [Google Scholar]
- 45.Lin Q, Ruuska SE, Shaw NS, Dong D, Noy N. Ligand selectivity of the peroxisome proliferator-activated receptor alpha. Biochemistry. 1999;38:185–90. doi: 10.1021/bi9816094. [DOI] [PubMed] [Google Scholar]
- 46.Norris AW, Li E. Fluorometric titration of the CRABPs. Methods Mol Biol. 1998;89:123–39. doi: 10.1385/0-89603-438-0:123. [DOI] [PubMed] [Google Scholar]
- 47.Naruhn S, Toth PM, Adhikary T, Kaddatz K, Pape V, Dorr S, et al. High-affinity peroxisome proliferator-activated receptor beta/delta-specific ligands with pure antagonistic or inverse agonistic properties. Molecular pharmacology. 2011;80:828–38. doi: 10.1124/mol.111.074039. [DOI] [PubMed] [Google Scholar]
- 48.Prenzel N, Fischer OM, Streit S, Hart S, Ullrich A. The epidermal growth factor receptor family as a central element for cellular signal transduction and diversification. Endocrine-related cancer. 2001;8:11–31. doi: 10.1677/erc.0.0080011. [DOI] [PubMed] [Google Scholar]
- 49.Eccles SA. The epidermal growth factor receptor/Erb-B/HER family in normal and malignant breast biology. The International journal of developmental biology. 2011;55:685–96. doi: 10.1387/ijdb.113396se. [DOI] [PubMed] [Google Scholar]
- 50.McLachlan E, Shao Q, Wang HL, Langlois S, Laird DW. Connexins act as tumor suppressors in three-dimensional mammary cell organoids by regulating differentiation and angiogenesis. Cancer research. 2006;66:9886–94. doi: 10.1158/0008-5472.CAN-05-4302. [DOI] [PubMed] [Google Scholar]
- 51.Billin AN. PPAR-beta/delta agonists for Type 2 diabetes and dyslipidemia: an adopted orphan still looking for a home. Expert opinion on investigational drugs. 2008;17:1465–71. doi: 10.1517/13543784.17.10.1465. [DOI] [PubMed] [Google Scholar]
- 52.Richardson AL, Wang ZC, De Nicolo A, Lu X, Brown M, Miron A, et al. X chromosomal abnormalities in basal-like human breast cancer. Cancer cell. 2006;9:121–32. doi: 10.1016/j.ccr.2006.01.013. [DOI] [PubMed] [Google Scholar]