Abstract
Background
Plantar heel pain is a common disorder of the foot for which patients seek medical treatment. The purpose of this study is to explore the relationship between duration of symptoms in plantar fasciitis patients and demographic factors, the intensity and location of pain, extent of previous treatment and self reported pain and function.
Methods
The charts of patients presenting with plantar heel pain between June 2008 and October 2010 were reviewed retrospectively and 182 patients with a primary diagnosis of plantar fasciitis were identified. Patients with symptoms less than 6 months were identified as acute and patients with symptoms greater than or equal to six months were defined as having chronic symptoms. Comparisons based on duration of symptoms were performed for age, gender, BMI, comorbidities, pain location and intensity, and a functional score measured by the Foot and Ankle Ability Measure (FAAM).
Results
The two groups were similar in age, BMI, gender, and comorbidities. Pain severity, as measured by a VAS, was not statistically significant between the two groups (6.6 and 6.2). The acute and chronic groups of patients reported similar levels of function on both the activity of daily living (62 and 65) and sports (47 and 45) subscales of the FAAM. Patients in the chronic group were more likely to have seen more providers and tried more treatment options for this condition.
Conclusion
As plantar fasciitis symptoms extend beyond 6 months, patients do not experience increasing pain intensity or functional limitation. No specific risk factors have been identified to indicate a risk of developing chronic symptoms.
Keywords: plantar fasciitis, heel pain, functional limitation
INTRODUCTION
Plantar heel pain or plantar fasciitis is one of the most common disorders of the foot that causes patients to seek medical care. This condition results in approximately 1 million visits to healthcare providers each year and over $284 million in medical costs.15,19 Up to two million Americans are affected with plantar heel pain, and the lifetime risk of an individual to develop plantar fasciitis has been estimated at 10%.4,12 Although patients exhibit similar patterns of symptomatology, the clinical presentation can vary in location and intensity of pain as well as duration of symptoms.
Nonoperative therapies are associated with variable rates of success and no one treatment has been shown to be the “gold standard”.5,8,10,22 Low cost options are favored as the primary treatments given the lack of evidence to support the use of more expensive therapies. In a recent analysis of the economic burden associated with plantar fasciitis, Tong and Furia attribute the majority of the yearly cost of treatment for plantar fasciitis to office visits and medications prescribed.19
Previous studies suggest that plantar heel pain is common in runners and military personnel.7,17 In addition, work related factors seem to play a role in the development of this condition.21 Identified risk factors for plantar fasciitis include obesity, decreased ankle dorsiflexion, the amount of time spent standing and walking, and standing on hard surfaces.13,21
Frequently, patients do not seek care until the symptoms are considered chronic. Multiple treatment options exist for this debilitating condition, but no single treatment has emerged as the standard of care. As a result, many patients develop chronic pain and seek treatment from multiple providers particularly when attempted treatments do not bring about the desired pain relief. The benefit of these multiple provider visits is unclear given the known self limiting nature of plantar fasciitis.
The pain of plantar fasciitis may significantly limit activities for those affected. Although the disability related to plantar fasciitis, in activities of daily living and sports-related activities, has not been clearly defined, previous studies suggest that the disability related to plantar fasciitis is most affected by body mass index (BMI).14 There have been no clinical studies identifying demographic or clinical factors associated with the location of pain, duration of symptoms, self-reported function, and extent of treatment for individuals with plantar fasciitis.
The purpose of this study was to explore the relationship between duration of symptoms in plantar fasciitis patients and demographic factors, the intensity and location of pain, extent of previous treatment and self reported pain and function. We hypothesized that patients with chronic symptoms would report more severe pain levels and decreased function primarily in sports-related activities. In addition, we sought to verify that patients with chronic symptoms see a greater number of providers and receive more treatments for this condition.
MATERIALS AND METHODS
This study was approved by the Human Research Protection Organization at Washington University School of Medicine. A total of 218 patients seen by one of three fellowship trained adult orthopaedic foot and ankle surgeons between July 2008 and October 2010 were identified through billing databases by ICD-9 code for plantar fasciitis (728.71). All patients with a primary diagnosis of plantar fasciitis based on clinical examination by one of three surgeons were included. Patients were excluded from the study if chart review determined that they did not have a diagnosis of plantar fasciitis, if the plantar heel pain was not the primary condition leading to the clinic visit, if they had a diagnosis of plantar fascia rupture or neurogenic causes of heel pain. Two patients were excluded because no information was available regarding the duration of symptoms. No patients identified were under the age of 18 years old. Thirty-six patients were excluded leaving 182 patients with a primary diagnosis of plantar fasciitis. New patient visits for plantar fasciitis represented 5.0 % of all new patient visits to these providers during the time period studied. All patients were treated initially with nonoperative measures.
The following clinical variables were extracted from each patient chart: BMI, medical comorbidities (diabetes, rheumatologic conditions, cardiac history) and, tobacco use. The number of previous providers seen and number of treatment types attempted was recorded for each patient in addition to the number of office visits to our office. At their initial visit, patients were asked to complete a Visual Analog Scale (VAS) pain score to describe their current level of pain. Functional performance level was determined by the Foot and Ankle Ability Measure (FAAM), a validated self reported measure of physical function for the foot and ankle.9 Patient responses to the FAAM were scored for both the two subscales: the 21 item activity of daily living subscale and the 8 item sports subscale. On each subscale a maximum score of 100 is possible representing no limitation in function. The FAAM was scored using previously published methods.9 VAS pain scores were available for 148 (81%) patients. FAAM scores were available for 151 (83%) patients on the activities of daily living (ADL) subscale and 116 (64%) patients on the sports subscale.
Patients were asked to mark the location of pain on a foot diagram at the initial clinic visit. The diagram of the foot was divided into six areas (Figure 1); each patient’s foot diagram was reviewed and scored based on location and total number of areas marked for each foot. One hundred sixty-nine patients (223 feet) completed the foot diagram. Complete data, which included FAAM scores (ADL and sports subscales), VAS pain scores and foot diagram data, was available for 120 patients. Patients with data available for any of these parameters were included in the evaluation.
Fig. 1.
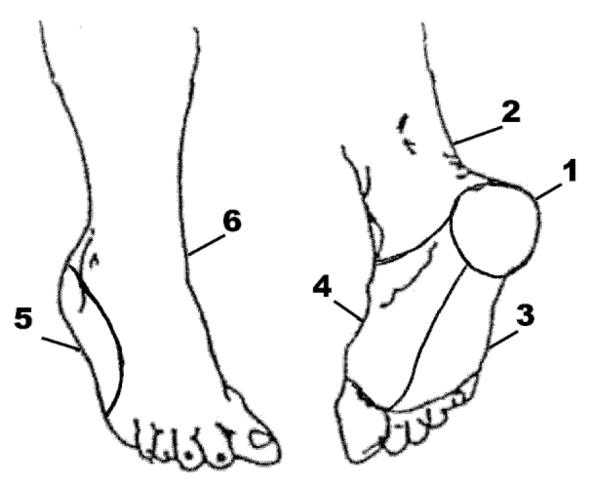
Foot diagram divided into six areas so patient can mark the location of the pain.
One hundred twenty-four (68.1%) female and 58 (31.9%) male patients were included. Thirty-nine (21.4%) patients reported bilateral symptoms. Sixty-six (36.3%) patients with unilateral symptoms had right sided pain and seventy-seven (42.3%) patients reported symptoms on the left side. The average age of patients was 48.9 (±12). The average BMI was 29.1 (±6.2), with an average of 28.9 (±6.7) for female patients and 29.8 (±5.2) for male patients. The average duration of symptoms was 14.1 (±23.1) months. Patients with symptoms less than 6 months were placed in a category defined as “acute”, and patients with symptoms greater than or equal to 6 months were considered to have “chronic” symptoms. Six months was used as the criteria for chronic symptoms based on published indications of operative intervention for plantar fasciitis.2,3,6,18 Four patients identified a previous, separate episode of similar symptoms and were included in the chronic group. A total of 90 patients were identified has having acute symptoms, and 92 patients reported chronic symptoms. Demographic data for patients with acute and chronic symptoms is shown in Table 1.
Table 1.
Patient Demographics
|
Total (n=182) |
Acute (< 6 months) (n=92) |
Chronic (≥ 6 months) (n=90) |
|
|---|---|---|---|
|
|
|||
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age | 48.9 (12.0) | 49.1 (11.9) | 48.7 (12.1) |
| BMI (8 missing) | 29.1 (6.2) | 28.9 (6.2) | 29.3 (6.2) |
| Duration of Symptoms (months) | 14.1 (23.1) | 3.1 (1.8) | 25.7 (28.8) |
|
| |||
| N (%) | N (%) | N (%) | |
|
|
|||
| Gender | |||
| Female | 124 (68.1%) | 57 (61.3%) | 67 (75.3%) |
| Male | 58 (31.9%) | 36 (38.7%) | 22 (24.7%) |
| Unilateral Symptoms | |||
| Right | 66 (36.3%) | 43(46.2%) | 23(25.8%) |
| Left | 77 (42.3%) | 38 (40.9%) | 39 (43.8%) |
| Bilateral symptoms | 39 (21.4%) | 12 (12.9%) | 27 (30.3%) |
| Comorbidities | |||
| Diabetes Mellitus | 13(7.1%) | 6 (6.5%) | 7 (7.9%) |
| Heart disease | 12 (6.6%) | 5 (5.4%) | 7 (7.9%) |
| Inflammatory Arthropathy | 5 (2.7%) | 1 (1.1%) | 4 (4.5%) |
| Tobacco use current (4 missing) | 10 (5.5 %) | 7 (7.8%) | 3 (3.4%) |
| Tobacco use ever (4 missing) | 51 (28.0%) | 32 (34.4%) | 19 (21.3%) |
Statistical Analysis
Spearman’s correlation was used to evaluate the relationship between duration of symptoms and the primary variables of interest: pain intensity score (VAS) and FAAM subscale scores. Patients were categorized as acute or chronic based on duration of symptoms. Comparisons of demographic data, previous number of providers and treatments, and VAS and FAAM scores were made between the acute and chronic groups using chi-square, Mann Whitney U non-parametric test and t-tests. Comparative analyses for all completed foot diagrams were conducted on the total number of painful regions as well as differences between the two groups for each region identified using chi-square tests. A power analysis was performed to determine the power of the sample size to detect meaningful differences between the ADL scores of the acute and chronic groups. The minimal clinically important difference for the ADL score has been previously defined as 8 points.9 All analyses used SPSS statistical software version 17.0.
RESULTS
The location of pain on the foot diagram was similar between the acute and chronic groups. The average number of areas marked on the foot diagram was similar between the acute (2, SD±1.3) and chronic (3, SD±1.4) groups (p=0.34). The most frequently reported location of pain for both groups was region one. (Figure 1) There was no significant difference in the proportion of patients indicating pain in region 1 between the acute (89%) and chronic group (91%). Forty five (53%) patients in the chronic group indicated pain in region 3 compared to 33 (40%) patients in the acute group (p=0.09). There were no other differences noted in the pattern of pain between the acute and chronic group. The mean VAS pain scores did not differ significantly between the acute and chronic groups, 6.2 (±2.2) versus 6.61 (±2.2) respectively (p=0.21) and Spearman’s correlation showed no association between pain level and duration of symptoms (r=0.1).
Patients with chronic symptoms were more likely to see multiple providers for treatment of their heel pain and to try multiple treatments (Table 2). The most common treatments attempted by both groups were physical therapy and orthotics. Patients with chronic pain were more likely to have tried cortisone injections, orthotics, physical therapy, massage and boot or cast treatment than patients in the acute group. Higher rates of treatments such as acupuncture, Coblation with bipolar radiofrequency, shock wave therapy, prolotherapy and surgical intervention were also reported by the chronic group. Only 4 patients had previous surgical intervention by an outside provider. Within our practice, patients were seen for an average of 1.6 (±1) office visits although specific follow up was recommended for most patients. There was no difference in the number of office visits to our group by the chronic group (1.7 ± 1.0) compared to the acute group (1.5 ± 0.8). The minimum number of visits to our clinic for both groups was one and the maximum was five Sixty four percent of all patients were seen for one visit only and 22 % were seen twice. In the acute group, 64% were seen for one visit and 28% were seen twice. In the chronic group 63% were seen once, 16% were seen twice, and 14% were seen three times.
Table 2.
Treatment Types
| Total | Acute | Chronic | p-value* | |
|---|---|---|---|---|
|
| ||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Previous Number of providers |
0.37 (0.6) | 1.2 (1.0) | 0.001 | |
| Previous number of treatments |
1.5 (1.4) | 3.7 (2.3) | 0.001 | |
|
| ||||
| N(%) | N(%) | N(%) | p-value** | |
|
| ||||
| Cortisone injection | 60 (33.0%) | 12 (12.9%) | 48 (53.9%) | 0.001 |
| Physical Therapy | 71 (39.0%) | 21 (22.6%) | 50 (56.2%) | 0.001 |
| Massage | 40 (22.0%) | 10 (10.8%) | 30 (33.7%) | 0.001 |
| Orthotics | 90 (49.5%) | 31 (33.3%) | 59 (66.3%) | 0.001 |
| NSAIDS | 101 (55.5%) | 50 (53.8%) | 51 (57.3%) | 0.63 |
| Narcotics | 16 (8.8%) | 5 (5.4%) | 11(12.4%) | 0.10 |
| Steroid (pills) | 3 (1.6%) | 0 (0) | 3 (3.4%) | 0.07 |
| Boot/Cast | 33 (18.1%) | 6 (6.5%) | 27 (30.3%) | 0.001 |
| Night splint | 13 (7.1%) | 5 (5.4%) | 8 (9.0%) | 0.34 |
| Brace | 9 (4.9%) | 3 (3.2%) | 6 (6.7%) | 0.29 |
| Surgery | 4 (2.2%) | 1 (1.1%) | 3 (3.4%) | 0.30 |
| ECSWT | 4 (2.2%) | 0 (0) | 4 (4.5%) | 0.04 |
| Prolotherapy | 1 (0.5%) | 0 (0) | 1 (1.1%) | 0.31 |
| Laser | 3 (1.6%) | 0 (0) | 3 (3.4%) | 0.07 |
| TOPAZ | 2 (1.1%) | 0 (0) | 2 (2.2%) | 0.15 |
| Other | 24 (13.2%) | 4 (4.3%) | 20 (22.5%) | 0.001 |
T-test,
Chi-square test
Patients in the acute and chronic groups did not differ in their overall assessment of function as reported on the FAAM. The average score on the ADL subscale was 62.4 (±20.4) for the acute group and 65.4 (±22.6) for the chronic group (p=0.39). Spearman’s correlation of total ADL and Sports function scores did not vary with the duration of symptoms (r= 0.08 and r= 0.01 respectively). The power analysis indicated a power of 80% to detect an 8 point difference (minimal clinically important difference) in the ADL scores between the two groups. Patients in the acute group scored an average of 46.5 (±28.5) on the sports subscale compared to 44.7 (±26.8) for the chronic group (p=0.73). In the individual domains of walking down stairs, on curbs or walking less than five minutes, the chronic group reported a higher level of function that was statistically significant (p<0.05).
Comorbidities such as diabetes, heart disease and rheumatoid arthritis did not affect functional status as reported on the FAAM in the ADL or sports scales in this group of patients seeking treatment for plantar fasciitis. Patients with BMI in the obese category (BMI ≥ 30) did not report differences in functional status as measured on the FAAM ADL and sports scales.
DISCUSSION
In this group of 182 patients with plantar fasciitis, patients with symptoms greater than or equal to 6 months (chronic) did not display statistically significant differences in age, gender or BMI when compared to patients with symptoms less than 6 months (acute). Comorbidities were similar between the acute and chronic groups. While patients with chronic symptoms reported higher numbers of providers seen and treatments attempted, they did not report more extensive location of pain or higher pain intensity. The functional limitations in both groups were similar with no difference detected between the acute and chronic groups on the ADL and sports subscales of the FAAM. We hypothesized that patients with chronic symptoms would report decreased function due to longstanding symptoms. This was not seen in this patient group. In fact, chronic symptoms were not associated with higher scores on a VAS or changes in function as evaluated by the FAAM. In the few subscales where differences were detected, the patient with chronic symptoms reported higher function possibly suggesting an adaptation in function to a long-standing pain condition.
There have been multiple studies investigating the risk factors for development of plantar fasciitis, but very little is known about the risk for developing chronic symptoms that are unresponsive to the most common nonsurgical interventions. Plantar fasciitis is thought to be a self limiting process with over 80% of patients experiencing resolution of symptoms within 1 year.5,8,10,22 Davis et al reported 89.5% of patients in their series had resolution of symptoms within 11 months.5 Wolgin et al noted similar patterns of symptom relief, but also noted that patients with a longer duration of symptoms before seeking medical attention were more likely to report lower satisfaction after nonoperative treatments.22 In addition, Ferkel et al reported lower satisfaction after endoscopic plantar fascia release in patients with symptoms present for over 2 years prior to surgery.2 While many patients experience symptom duration that extends to a year or more, the characteristics of this group of patients have not previously been defined. Based on this patient group, there are no demographic differences, pain or functional performance differences between patients with acute or chronic symptoms.
It is possible that there is a difference in the pathophysiology of heel pain in patients who develop chronic symptoms. Baxter, et al proposed that compression of the first branch of the lateral plantar nerve may be an explanation for the recalcitrant symptoms seen in some patients.1 Multiple authors have proposed release of the nerve combined with plantar fascia release as a surgical option for patients who have continued pain despite nonoperative therapy.1,16,20 Identification of patients with nerve compression has simply been based on failure to respond to nonoperative treatments. The results of this study indicate that patterns of pain or intensity of pain reported by the patient is not indicative of a more chronic condition and will not aid in the identification of a nerve compression syndrome. Further comparison of a group of patients who improve with nonoperative therapy and patients who fail nonoperative therapy but improve with surgical nerve release is needed to identify specific factors that might allow for earlier diagnosis of a nerve compression syndrome.
Currently, there are no clinical factors that distinguish the potential to develop chronic symptoms. While this study primarily focuses on patient reported symptoms and patterns of pain, Patel et al evaluated a large group of patients with plantar fasciitis for isolated contracture of the gastrocnemius.11 When they stratified patients into acute and chronic groups, there was no difference noted in the type of contracture between the two groups. In general, there are no specific identifiable predictors of the development of chronic symptoms of plantar fasciitis. Pain seems to be the predominant factor that motivates patients to seek treatment. In this series, patients did not report differences in function or pain levels when comparing the acute and chronic groups. The tendency to develop pain along the lateral border of the foot was more frequent in the chronic group of patients. This lateral overload is likely the result of gait changes over time to offload the more painful medial aspect of the heel.
Patients with chronic symptoms were more likely to seek treatment from multiple providers than those with acute symptoms. Patients with heel pain are typically frustrated as therapies fail to resolve their pain, and they frequently seek the opinion of another provider hoping for new or different alternatives. When additional providers continue to offer the same alternatives, patients move on to another provider looking for other options. Further study is needed to address the economic burden to the healthcare system of this pattern of use of medical resources.
The primary limitation of this study is that it is from retrospective data. Patient charts were the only source of information and the accuracy of the data provided by the patients is unknown. Due to failure to complete the forms provided, pain scores and FAAM scores were not available for all patients. Compliance with completion of the forms was not checked at the time of the initial visit so the incomplete response or lack of response was discovered as the charts were reviewed retrospectively. Patients were not contacted for missing data. In addition, the retrospective nature of this study may limit the ability to identify all patients with chronic symptoms. Patients were asked for duration of the current episode of heel pain, but they were not questioned about past episodes. Patients with a current episode of less than 6 months of symptoms but multiple episodes over several years would be considered in the chronic group. The diagnosis of plantar fasciitis in this group of patients was based on the clinical impression of a fellowship trained orthopaedic foot and ankle surgeon, not on a predetermined set of clinical criteria.
In this study an equal number of patients were seen with acute versus chronic cases of plantar fasciitis (92 verus 90). As a large tertiary care center, we receive referrals from a large geographic area with frequent referrals of more complex problems or patients with failed treatment elsewhere. As a result, we see a large number of patients with chronic symptoms.
CONCLUSION
Plantar fasciitis is one of the more common conditions for which patients with foot pain seek medical treatment. Although the condition is often self limiting, many patients seek treatment from multiple providers and attempt multiple treatment modalities. As symptoms extend beyond 6 months, patients do not develop increased pain intensity or a progression of symptoms. Patients with symptoms for a longer duration do not report an increase in functional limitations. This study did not identify any specific risk factors for developing the chronic condition. This study also did not investigate the impact of chronic pain on the patient’s perception of well-being. The VAS and FAAM scales evaluate pain and function only.
Footnotes
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
REFERENCES
- 1.Baxter DE, Pfeffer GB. Treatment of chronic heel pain by surgical release of the first branch of the lateral plantar nerve. Clin Orthop Relat Res. 1992;(279):229–236. [PubMed] [Google Scholar]
- 2.Bazaz R, Ferkel RD. Results of endoscopic plantar fascia release. Foot Ankle Int. 2007;28(5):549–556. doi: 10.3113/FAI.2007.0549. [DOI] [PubMed] [Google Scholar]
- 3.Conflitti JM, Tarquinio TA. Operative outcome of partial plantar fasciectomy and neurolysis to the nerve of the abductor digiti minimi muscle for recalcitrant plantar fasciitis. Foot Ankle Int. 2004;25(7):482–487. doi: 10.1177/107110070402500707. [DOI] [PubMed] [Google Scholar]
- 4.Crawford F, Atkins D, Edwards J. Interventions for treating plantar heel pain. Cochrane Database of Systematic Reviews. 2000;(3) doi: 10.1002/14651858.CD000416. CD000416. [DOI] [PubMed] [Google Scholar]
- 5.Davis PF, Severud E, Baxter DE. Painful heel syndrome: results of nonoperative treatment. Foot Ankle Int. 1994;15(10):531–535. doi: 10.1177/107110079401501002. [DOI] [PubMed] [Google Scholar]
- 6.Hogan KA, Webb D, Shereff M. Endoscopic plantar fascia release. Foot Ankle Int. 2004;25(12):875–881. doi: 10.1177/107110070402501206. [DOI] [PubMed] [Google Scholar]
- 7.Knobloch K, Yoon U, Vogt PM. Acute and overuse injuries correlated to hours of training in master running athletes. Foot Ankle Int. 2008;29(7):671–676. doi: 10.3113/FAI.2008.0671. [DOI] [PubMed] [Google Scholar]
- 8.Lapidus PW, Guidotti FP. Painful Heel: Report of 323 Patients with 364 Painful Heels. Clin Orthop Relat Res. 1965;39:178–186. [PubMed] [Google Scholar]
- 9.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 10.Martin RL, Irrgang JJ, Conti SF. Outcome study of subjects with insertional plantar fasciitis. Foot Ankle Int. 1998;19(12):803–811. doi: 10.1177/107110079801901203. [DOI] [PubMed] [Google Scholar]
- 11.Patel A, DiGiovanni B. Association between plantar fasciitis and isolated contracture of the gastrocnemius. Foot Ankle Int. 2011;32(1):5–8. doi: 10.3113/FAI.2011.0005. [DOI] [PubMed] [Google Scholar]
- 12.Pfeffer G, Bacchetti P, Deland J, et al. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 1999;20(4):214–221. doi: 10.1177/107110079902000402. [DOI] [PubMed] [Google Scholar]
- 13.Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for Plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003;85-A(5):872–877. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Riddle DL, Pulisic M, Sparrow K. Impact of demographic and impairment-related variables on disability associated with plantar fasciitis. Foot Ankle Int. 2004;25(5):311–317. doi: 10.1177/107110070402500506. [DOI] [PubMed] [Google Scholar]
- 15.Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25(5):303–310. doi: 10.1177/107110070402500505. [DOI] [PubMed] [Google Scholar]
- 16.Sammarco GJ, Helfrey RB. Surgical treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 1996;17(9):520–526. doi: 10.1177/107110079601700902. [DOI] [PubMed] [Google Scholar]
- 17.Scher DL, Belmont PJ, Jr., Bear R, et al. The incidence of plantar fasciitis in the United States military. J Bone Joint Surg Am. 2009;91(12):2867–2872. doi: 10.2106/JBJS.I.00257. [DOI] [PubMed] [Google Scholar]
- 18.Sinnaeve F, Vandeputte G. Clinical outcome of surgical intervention for recalcitrant inferomedial heel pain. Acta orthopaedica Belgica. 2008;74(4):483–488. [PubMed] [Google Scholar]
- 19.Tong KB, Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthop (Belle Mead NJ) 2010;39(5):227–231. [PubMed] [Google Scholar]
- 20.Watson TS, Anderson RB, Davis WH, Kiebzak GM. Distal tarsal tunnel release with partial plantar fasciotomy for chronic heel pain: an outcome analysis. Foot Ankle Int. 2002;23(6):530–537. doi: 10.1177/107110070202300610. [DOI] [PubMed] [Google Scholar]
- 21.Werner RA, Gell N, Hartigan A, Wiggerman N, Keyserling WM. Risk factors for plantar fasciitis among assembly plant workers. PM R. 2010;2(2):110–116. doi: 10.1016/j.pmrj.2009.11.012. quiz 111 p following 167. [DOI] [PubMed] [Google Scholar]
- 22.Wolgin M, Cook C, Graham C, Mauldin D. Conservative treatment of plantar heel pain: long-term follow-up. Foot Ankle Int. 1994;15(3):97–102. doi: 10.1177/107110079401500303. [DOI] [PubMed] [Google Scholar]


