Abstract
Purpose
Canine rabies is a serious health problem in Morocco and about 22 human deaths are reported yearly. Following the World Health Organization (WHO) recommendations, Moroccan authorities evaluated oral rabies vaccine baits specially designed for dogs.
Materials and Methods
The study was performed in Tiflet area. The vaccine strain was SAG2, a modified live oral rabies vaccine strain. Each bait contained an aluminium/PVC capsule filled with a liquid. Two kinds of baits were used: placebo baits containing methylene blue as a topical marker and vaccine baits containing vaccine suspension. The study was performed according to recommended WHO strategies, i.e., door to door model (DDDM), hand-out and wildlife immunization model (WIM). The DDDM was performed in the rural area of Tiflet on 60 owned dogs. The hand-out strategy was tested on 15 stray dogs. The WIM was performed on 4 transects lines near Tiflet slaughterhouse and near the weekly traditional market location.
Results
Using the DDDM, 100% of owned dogs were attracted by the baits and 77% ate the bait. Using the hand-out model, 100% of dogs showed interest in baits and 46.7% took the baits. Using the WIM in stray dogs, up to 73% of baits disappeared and 68% of the capsules containing the SAG2 vaccine were found pierced, depending on the sites of distribution.
Conclusion
This pilot study showed that baits have a good palatability and that oral vaccination of both owned and stray dogs is feasible with baits specifically developed for dogs and with adapted strategy of distribution.
Keywords: Rabies, Dogs, Oral administration, Vaccination, Morocco
Introduction
Although rabies is a reportable disease, the true incidence of the disease is greatly underestimated due to a lack of systematic surveillance and reporting by most developing countries [1]. In news published in September of 2011, the Global Alliance for Rabies Control estimates that 70,000 people die of rabies every year (http://rabiesalliance.org/media/news/annual-number-of-deaths-from-rabies-hits-70000-worldwide), mostly in developing countries from Asia (58%) and Africa (42%) [2]. Rabies is a vaccine-preventable disease. Since dogs are the main reservoir and source of infection for humans, a better control of rabies could be achieved through vaccination of dogs [3]. In Latin America, the mass vaccination of the dog population has led to a significant drop in the number of human and canine rabies cases [4].
Despite several mass campaigns of parenteral vaccination of dogs, canine rabies remains a serious health problem in Morocco and about 22 human deaths are reported every year [5]. Parenteral vaccination is the method of choice for owned dogs (i.e., dogs with a person that claims responsibility, according to the World Organisation for Animal Health (OIE) definition [6]), since approximately 70% of dogs in Morocco are considered accessible [7]. However, a proportion of dogs are stray (i.e., free-roaming with or without owner, or feral, according to the OIE definition [6]), and owned dogs may also be aggressive and difficult to handle, therefore oral vaccination could be helpful [8]. Rabies has been successfully controlled in several European countries through oral vaccination of wildlife with vaccine baits and considerable success has been achieved in the control of Arctic fox rabies [9] and raccoon rabies in Canada and in the United States [10]. International guidelines for rabies control in dogs and implementation of field trials using oral vaccines are available [11,12].
Moroccan authorities opted for evaluating oral rabies vaccine strain SAG2 in field conditions. The present study is a first trial undertaken in the region of Rabat (Morocco) to evaluate the acceptance of baits specifically designed for dogs.
Materials and Methods
Study zone
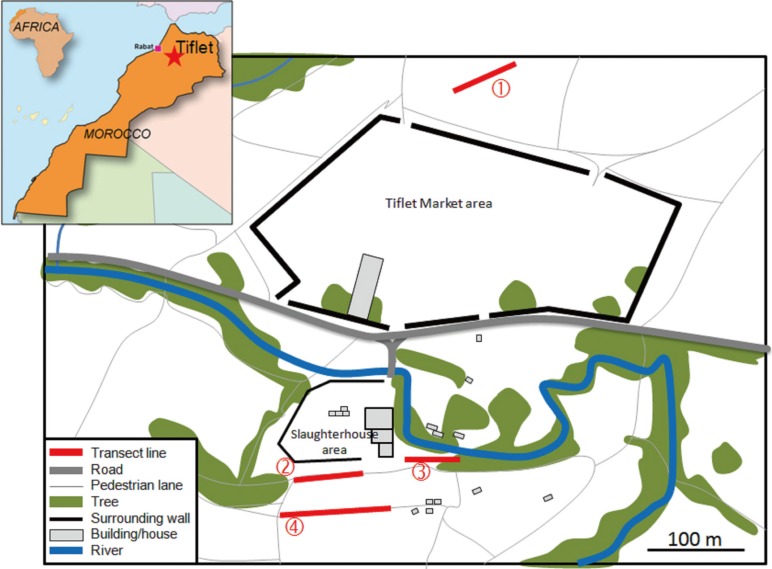
The field study was carried out in the rural area of Tiflet city located 40 km from east of Rabat (capital of Morocco) (Fig. 1). The slaughterhouse activity and the weekly regional traditional market (souk) of Tiflet are attractive for both the population and dogs from neighbouring rural municipalities. The dog population of the area was estimated in 2010 and the results are reported in Table 1 [13].
Fig. 1.
Location of the transect lines for the distribution of baits. SAG2 baits were distributed in the evening along transect lines used by free-roaming dogs to go to the slaughterhouse: 1, beside the market area; 2 and 3, near the surrounding wall of the slaughterhouse; 4, along an access path to the district.
Table 1.
Dog population characteristics in Tiflet area in 2010
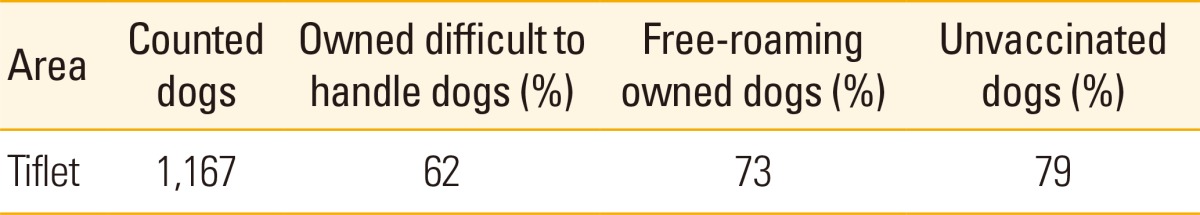
Percentages were calculated according to the responses given by the dog owners in the questionnaires.
Vaccine strain
The tested vaccine strain was SAG2, a modified live attenuated rabies virus. SAG2 is one of the two rabies vaccine strains recommended by World Health Organisation (WHO) to be used in dogs by the oral route [11,12].
SAG2 strain was constructed by two successive mutations from the rabies strain SAD Bern using neutralizing monoclonal antibodies. The mutations are on the position 333 of the antigenic site III of the rabies virus glycoprotein. In this position (333) SAG2 has GAA which codes for glutamic acid and SAD Bern strain has AGA which codes for arginine, resulting in a double avirulent mutant [14].
The genetic stability of SAG2 was largely demonstrated in vitro and in vivo (in mice) [14].
Baits
The baits were provided by Virbac Laboratories (Carros, France). The baits were cylindrical with 44 mm diameter, 16 mm height and 23 g weight for both baits types (vaccine baits and placebo baits). The colour of the baits was "cement/dirt" and the baits were "chicken liver" flavoured. The cylindrical shape, the colour and the chicken liver flavour were modifications to adapt the fox bait [15] (49 mm×44 mm×15 mm and 28 g, chocolate colour and fish flavour) to the Moroccan dog. The baits contained an aluminium/PVC sachet filled with a liquid. Vaccine baits and placebo baits were provided by the manufacturer. The baits were stored at -20℃ until use.
Vaccine baits
Each bait contained a liquid suspension (107.8 DICT50) of SAG2 vaccine strain. Its safety and efficacy have been demonstrated in fox, raccoon dog and dog [12,15,16,17] and the innocuity in numerous wild non-target species [16,18,19,20,21,22].
Placebo baits
Placebo baits contained a capsule with methylene blue as a topical marker. The bait uptake and perforation of the capsule could be evaluated visually. This aimed the monitoring of the bait uptake as recommended by the WHO [11,12].
The placebo bait casing had the same dimensions and composition as the vaccine baits.
Dogs
A total of 60 owned dogs, mainly adult males, living in villages located around Tiflet and 15 stray dogs living close to the slaughterhouse of Tiflet were included in the study.
Study strategy
Different strategies of distribution were tested for dogs according to directions of WHO [11].
First trial
This trial was conducted in the rural area of Tiflet according to the "door to door" oral vaccination model or door to door model (DDDM) [11] for owned dogs to assess the attractiveness and palatability of the bait casing. Each of 60 dogs was offered one placebo bait (Fig. 2A).
Fig. 2.
Uptake of the bait shown by the blue colour of the tongue. (A) Bait. (B) Dog consuming a bait. (C) Capsule pierced. (D) Tongue coloured by methylene blue.
Second trial
This trial was conducted with stray dogs in two steps. First, baits were offered to 15 dogs present on the site to evaluate their attractiveness according to the WHO "hand-out" model [11]. Secondly, a total of 30 SAG2 baits were distributed in the evening along 4 transect lines used by stray dogs to go to the slaughterhouse (Fig. 1) [13]. The distribution was carried out according to the "wildlife immunization model" or wildlife immunization model (WIM) [11]. The targeted sites were known to be visited by free ranging dogs [13]. The vaccine baits were left overnight. The next morning, remaining baits were removed.
Results
First trial
All dogs smelled the bait and most of them (77%) ate it in less than 3 minutes (Fig. 2B). The capsule was pierced by 62% of the dogs, i.e., 80% of dogs which consumed the bait (Fig. 2C). Although the mouth could not be examined in all dogs, the tongue was coloured in blue in at least 25 dogs, i.e., 67% of dogs which ate the bait (Fig. 2D). Some dogs, probably disturbed by the presence of strangers, did not eat the bait, but when they were left alone, half of them ate the bait within few minutes.
Second trial
For baits presented according to the hand-out model, although the environment was filled with meat odours, all 15 dogs smelled the baits. Four dogs ate the bait immediately and 3 dogs took the baits to bury them (46.7%).
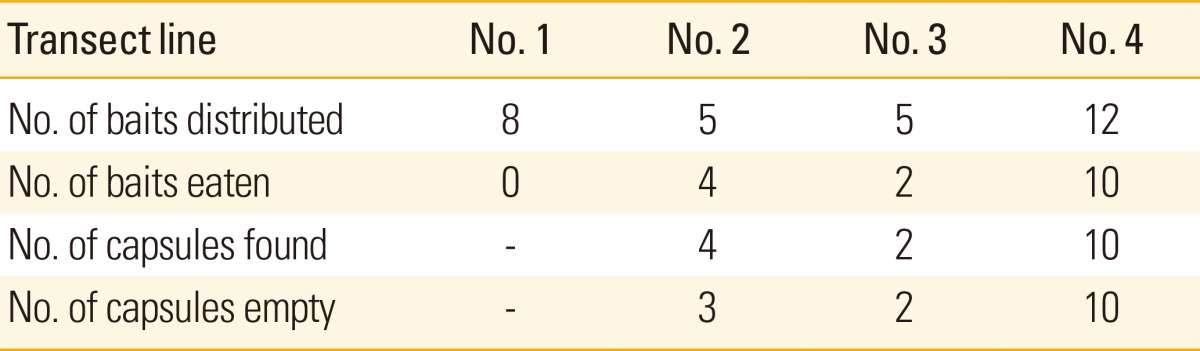
For baits distributed according to the WIM, none of them deposited along line 1 were taken. In contrast, a high proportion of baits distributed in lines 2, 3 and 4 (16 out of 22, i.e., 73%) had disappeared overnight and 68% of the capsules were found perforated (Table 2).
Table 2.
Attractiveness and palatability of SAG2 dog baits in free-roaming dogs
Discussion
Only two vaccines strains (SAG2 and V-RG) are currently recommended by WHO for oral vaccination of dogs [12]. SAG2 has been widely used in Europe and led to wildlife rabies elimination in several European countries [23]. It should be noted that no vaccine-induced rabies cases were reported in Europe after the distribution in the environment of more than 20 millions of SAG2 baits. This vaccine is registered for the control of canine rabies in India [16] and has been mainly evaluated in Tunisia [22], in Mexico [24], in South Africa [25] and in Indonesia [26], demonstrating its efficacy for dog vaccination in the field [27].
Numerous and extensive pathogenicity studies undertaken on more than 30 target and non-target warm-blooded species, including 5 from the canine family (of which dog), wild carnivores, rodents and non-human primates, demonstrated that SAG2 is an avirulent rabies vaccine strain [28]. The studies were performed according to the guidelines of WHO for safety testing of modified live-rabies vaccines [29] in species including rodents (mouse, rat, vole, squirrel, gerbil, jerboa, and meriones), carnivores (coyote, ferret, civet, mongoose, badger, and genet), non-human primates (Chacma baboons), other mammals (hedgehog, wild boar, domestic goat, and cow), and diurnal and nocturnal birds (crow, rook, buzzard, kite, and owl) [18,19,20,22,30]. Different studies showed that the persistence of the SAG2 virus in the oral cavity is very limited or even nil in non target species [14,19,20,21,22].
The immunogenicity and efficacy of SAG2 were evaluated in laboratory (mouse model) and in field conditions. Different trials demonstrated the protective effect of SAG2 vaccine bait in controlled laboratory conditions in different wildlife species and in dogs. These studies suggest that SAG2 induce humoral [15,16,17,31,32,33,34] and cell mediated immunity [31].
SAG2 vaccine baits appeared well-adapted to both owned and stray dogs living in Morocco. The shape of the bait is round (diameter=44 mm), facilitating the uptake by dogs of different sizes. The quantity of bait matrix was reduced to facilitate the puncture of the capsule to favour the contact of the liquid vaccine with oral mucosa and tonsils. It should be noted that capsules which were not pierced did not stick enough to the bait. It was observed that when the capsule was pierced before detaching from the bait, dogs tended to take again the capsule and lick the sweet content of the capsule. The baits have "cement/dirt" colour so that it merged with the colour of the soil and it does not attract children's attention. The chicken liver flavour has an attractive smell and a high palatability for Moroccan dogs. Several studies have shown that there were regional preferences for the bait flavours, such as poultry in Guatemala [35], dog biscuits in Mexico [24], chicken heads in Egypt [36] or fish in US Indian reservations (Navajo Nation and the Hopi Nation lands) [37].
Three different methods of distribution (central point, DDDM, and WIM) were previously tested in semi-rural areas in Tunisia with placebo baits containing sulfadimethoxine as a systemic marker [27]. When baits were given to dog owners at mobile vaccination centres with precise instructions for use, 79% of baits were fully consumed by the dogs [27]. The uptake reached 59% in owned dogs after door-to-door baiting and 42% in owned and ownerless dogs after transect line baiting [38]. In another study conducted in South Africa, the DDDM was tested. In total, 77% of the vaccine baits were at least partly consumed [39].
These methods of distribution were tested in this study. The DDDM, which reached primarily owned dogs and the hand-out model, which reached accessible stray dogs [11], were intended to evaluate bait palatability. The WIM adopted to distribute baits to stray dogs around the slaughterhouse of Tiflet gave encouraging results. More than 70% of the baits distributed along lines 2, 3, and 4 disappeared overnight despite the presence of abundant food and familiar smells in the environment. We assume that baits had been consumed by stray dogs, since 68% of capsules were found pierced with different characteristic canine teeth marks from dogs and because there were no feral animals in this area close to human habitations. No bait distributed along line 1 was consumed, probably because dogs could not hide in this fallow land. When this line 1 was identified on the previous year [13], the area was covered with bushes where stray dogs used to stay. This result illustrates that baits should not be distributed at random. Baits could be placed at selected sites where large numbers of stray dogs congregate such as slaughterhouses, garbage dump or public markets (souks) and along ways frequently used by dogs. Although the WIM is not specific and less safe than the DDDM and hand-out method, it allows the access to free-roaming and feral dogs, which constitute a high risk group in terms of rabies transmission [11]. The WIM requires the use of safe vaccines, fulfilling all criteria listed by WHO [11,12].
This pilot study showed that oral vaccination of both owned and stray dogs is feasible with baits specifically developed for dogs and adapted modes of distribution. These data will be confirmed with a larger field trial taking into account results of this study. The necessary 60-70% vaccination coverage could be achieved using vaccine baits to target stray dogs in addition to injectable vaccines used during mass parenteral vaccination programmes. Methods of distribution should be adapted to local conditions. For instance, in Asia, the "hand-out" model can be used because free-roaming dogs accept easily baits even when given by unknown people, whereas in Maghreb dogs wary of strangers because usually people prevent contacts with them by throwing stones in their direction, people worrying of dog bites and diseases (personal observations). Although the cost of oral vaccination is higher than that of the parenteral vaccination, the combination of both vaccination strategies may increase the vaccination coverage in the vector population and lead to rabies elimination. The cost of vaccination could be reduced by the use of aerial distribution in certain well defined and restricted areas.
Research on effective field methods for control and elimination of rabies, although less attractive than sophisticated molecular analyses, should remain the priority [40].
Footnotes
We thank Marie-José Duchêne and Dr. Anne-Laure Guiot for helping in the preparation of the manuscript. We are grateful to Dr Karima Zouine, Head of Prophylactic Activities Department of ONSSA and to Dr. Ahmed Derouich, Head of Veterinary Inspection Department of Tiflet, to ONSSA staff for support to this study, and to Dr. Philippe Mahl and Dr. Luc Martel from Virbac for designing the dog baits and discussing the protocol design. This research was funded by the institutional agricultural cooperation between Morocco and France.
No potential conflict of interest relevant to this article was reported.
References
- 1.Nel LH. Discrepancies in data reporting for rabies, Africa. Emerg Infect Dis. 2013;19:529–533. doi: 10.3201/eid1904.120185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knobel DL, Cleaveland S, Coleman PG, et al. Re-evaluating the burden of rabies in Africa and Asia. Bull World Health Organ. 2005;83:360–368. [PMC free article] [PubMed] [Google Scholar]
- 3.World Organization for Animal Health. Stray dog population control. Terrestrial animal health code. Paris: World Organization for Animal Health; 2012. [Google Scholar]
- 4.Schneider MC, Belotto A, Ade MP, et al. Current status of human rabies transmitted by dogs in Latin America. Cad Saude Publica. 2007;23:2049–2063. doi: 10.1590/s0102-311x2007000900013. [DOI] [PubMed] [Google Scholar]
- 5.El Harrak M. Epidemiological factors and control of rabies in North Africa; Compendium of the OIE Global Conference on Rabies Control; 2011 Sep 7-9; Incheon, Korea. Paris: World Organization for Animal Health; 2012. pp. 45–49. [Google Scholar]
- 6.World Organization for Animal Health. Terrestrial Animal Health Code. General provisions. Paris: World Organization for Animal Health; 2013. [Google Scholar]
- 7.Fassi-Fihri O. Historique et situation épidémiologique de la rage au Maroc. Renforcement de la surveillance et des systèmes d'alerte pour la fièvre catarrhale ovine, la fièvre du Nil occidental et la rage au Maroc, en Algérie et en Tunisie. Projet FAO GCP/RAB/002/FRA. Rome: Food and Agriculture Organization of the United Nations; 2008. [Google Scholar]
- 8.Yang DK, Kim HH, Lee KW, Song JY. The present and future of rabies vaccine in animals. Clin Exp Vaccine Res. 2013;2:19–25. doi: 10.7774/cevr.2013.2.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosatte RC, Power MJ, Donovan D, et al. Elimination of arctic variant rabies in red foxes, metropolitan Toronto. Emerg Infect Dis. 2007;13:25–27. doi: 10.3201/eid1301.060622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosatte R, MacDonald E, Sobey K, et al. The elimination of raccoon rabies from Wolfe Island, Ontario: animal density and movements. J Wildl Dis. 2007;43:242–250. doi: 10.7589/0090-3558-43.2.242. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Oral vaccination of dogs against rabies. Guidance for research on oral rabies vaccines and field application of oral vaccination of dogs against rabies. Geneva: World Health Organization; 2007. [Google Scholar]
- 12.World Health Organization. WHO expert consultation on rabies. Second report WHO technical report series. No. 982. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 13.Zouine K, Ezzahra Lahkak F, Demerson JM, et al. La rage au Maroc: situation, perspectives de lutte, faisabilité de la vaccination orale des chiens contre la rage; Troisièmes Rencontres du Bureau des Experts de la Rage du Continent Africain (AfroREB); 2011 May 23-26; Casablanca, Maroc. [Google Scholar]
- 14.Lafay F, Benejean J, Tuffereau C, Flamand A, Coulon P. Vaccination against rabies: construction and characterization of SAG2, a double avirulent derivative of SADBern. Vaccine. 1994;12:317–320. doi: 10.1016/0264-410x(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 15.Cliquet F, Guiot AL, Munier M, Bailly J, Rupprecht CE, Barrat J. Safety and efficacy of the oral rabies vaccine SAG2 in raccoon dogs. Vaccine. 2006;24:4386–4392. doi: 10.1016/j.vaccine.2006.02.057. [DOI] [PubMed] [Google Scholar]
- 16.Cliquet F, Gurbuxani JP, Pradhan HK, et al. The safety and efficacy of the oral rabies vaccine SAG2 in Indian stray dogs. Vaccine. 2007;25:3409–3418. doi: 10.1016/j.vaccine.2006.12.054. [DOI] [PubMed] [Google Scholar]
- 17.Schumacher CL, Coulon P, Lafay F, et al. SAG-2 oral rabies vaccine. Onderstepoort J Vet Res. 1993;60:459–462. [PubMed] [Google Scholar]
- 18.Bingham J, Schumacher CL, Aubert MF, Hill FW, Aubert A. Innocuity studies of SAG-2 oral rabies vaccine in various Zimbabwean wild non-target species. Vaccine. 1997;15:937–943. doi: 10.1016/s0264-410x(97)00009-1. [DOI] [PubMed] [Google Scholar]
- 19.Follmann EH, Ritter DG, Baer GM. Evaluation of the safety of two attenuated oral rabies vaccines, SAG1 and SAG2, in six Arctic mammals. Vaccine. 1996;14:270–273. doi: 10.1016/0264-410x(95)00208-i. [DOI] [PubMed] [Google Scholar]
- 20.Masson E, Cliquet F, Aubert M, et al. Safety study of the SAG2 rabies virus mutant in several non-target species with a view to its future use for the immunization of foxes in Europe. Vaccine. 1996;14:1506–1510. doi: 10.1016/s0264-410x(96)00114-4. [DOI] [PubMed] [Google Scholar]
- 21.Follmann EH, Ritter DG, Hartbauer DW. Safety of lyophilized SAG2 oral rabies vaccine in collared lemmings. J Wildl Dis. 2002;38:216–218. doi: 10.7589/0090-3558-38.1.216. [DOI] [PubMed] [Google Scholar]
- 22.Hammami S, Schumacher CL, Cliquet F, et al. Safety evaluation of the SAG2 rabies virus mutant in Tunisian dogs and several non-target species. Vet Res. 1999;30:353–362. [PubMed] [Google Scholar]
- 23.Cliquet F, Aubert M. Elimination of terrestrial rabies in Western European countries. Dev Biol (Basel) 2004;119:185–204. [PubMed] [Google Scholar]
- 24.Frontini MG, Fishbein DB, Garza Ramos J, et al. A field evaluation in Mexico of four baits for oral rabies vaccination of dogs. Am J Trop Med Hyg. 1992;47:310–316. doi: 10.4269/ajtmh.1992.47.310. [DOI] [PubMed] [Google Scholar]
- 25.Schumacher CL, Hammami S, Chaparro F, et al. Safety of the oral rabies vaccine SAG2 and efficacy of its delivery system DBL2 in indigenous dogs; Proceedings of the Southern and Eastern African Rabies Group (SEARG) Meeting; 1997 Mar 4-6; Nairobi, Kenya. pp. 163–174. [Google Scholar]
- 26.Faizah, Mantik-Astawa IN, Putra AA, Suwarno The humoral immunity response of dog vaccinated with oral SAG2 and parenteral Rabisin and Rabivet Supra92. Indones J Biomed Sci. 2012;6:26–29. [Google Scholar]
- 27.Ben Youssef S, Matter HC, Schumacher CL, et al. Field evaluation of a dog owner, participation-based, bait delivery system for the oral immunization of dogs against rabies in Tunisia. Am J Trop Med Hyg. 1998;58:835–845. doi: 10.4269/ajtmh.1998.58.835. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. WHO expert consultation on rabies, 1st report. WHO Technical Report Series 931. Geneva: World Health Organization; 2005. [PubMed] [Google Scholar]
- 29.World Health Organization. WHO expert committee on rabies, 8th report. WHO Technical Report Series 824. Geneva: World Health Organization; 1992. [PubMed] [Google Scholar]
- 30.van Heerden J, Bingham J, van Vuuren M, Burroughs RE, Stylianides E. Clinical and serological response of wild dogs (Lycaon pictus) to vaccination against canine distemper, canine parvovirus infection and rabies. J S Afr Vet Assoc. 2002;73:8–12. doi: 10.4102/jsava.v73i1.541. [DOI] [PubMed] [Google Scholar]
- 31.Lambot M, Blasco E, Barrat J, et al. Humoral and cell-mediated immune responses of foxes (Vulpes vulpes) after experimental primary and secondary oral vaccination using SAG2 and V-RG vaccines. Vaccine. 2001;19:1827–1835. doi: 10.1016/s0264-410x(00)00321-2. [DOI] [PubMed] [Google Scholar]
- 32.Bingham J, Schumacher CL, Hill FW, Aubert A. Efficacy of SAG-2 oral rabies vaccine in two species of jackal (Canis adustus and Canis mesomelas) Vaccine. 1999;17:551–558. doi: 10.1016/s0264-410x(98)00233-3. [DOI] [PubMed] [Google Scholar]
- 33.Follmann EH, Ritter DG, Donald WH. Oral vaccination of captive arctic foxes with lyophilized SAG2 rabies vaccine. J Wildl Dis. 2004;40:328–334. doi: 10.7589/0090-3558-40.2.328. [DOI] [PubMed] [Google Scholar]
- 34.Hanlon CA, Niezgoda M, Morrill P, Rupprecht CE. Oral efficacy of an attenuated rabies virus vaccine in skunks and raccoons. J Wildl Dis. 2002;38:420–427. doi: 10.7589/0090-3558-38.2.420. [DOI] [PubMed] [Google Scholar]
- 35.Corn JL, Mendez JR, Catalan EE. Evaluation of baits for delivery of oral rabies vaccine to dogs in Guatemala. Am J Trop Med Hyg. 2003;69:155–158. [PubMed] [Google Scholar]
- 36.Linhart SB, Baer GM, Balderas Torres JM, et al. Acceptance of candidate baits by domestic dogs for delivery of oral rabies vaccines. Onderstepoort J Vet Res. 1997;64:115–124. [PubMed] [Google Scholar]
- 37.Bergman D, Bender S, Wenning K, et al. Bait acceptability for delivery of oral rabies vaccine to free-ranging dogs on the Navajo and Hopi Nations. Dev Biol (Basel) 2008;131:145–150. [PubMed] [Google Scholar]
- 38.Matter HC, Schumacher CL, Kharmachi H, et al. Field evaluation of two bait delivery systems for the oral immunization of dogs against rabies in Tunisia. Vaccine. 1998;16:657–665. doi: 10.1016/s0264-410x(97)00259-4. [DOI] [PubMed] [Google Scholar]
- 39.Bishop GC. Increasing dog vaccination coverage in South Africa: is oral vaccination the answer? In: Dodet B, Meslin FX, editors. Rabies control in Asia. London: John Libbey & Sons, Ltd.; 2001. pp. 105–109. [Google Scholar]
- 40.Zinsstag J. Towards a science of rabies elimination. Infect Dis Poverty. 2013;2:22. doi: 10.1186/2049-9957-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]