Abstract
Aim
The aim of this study was to assess changes in trends of meningococcal disease and strain diversity of Neisseria meningitidis in Europe, South America, and Africa over the last 100 years.
Methods
Healthcare databases and sources of grey literature were searched in 2012 and records were screened against the protocol eligibility criteria using a three-stage sifting process. Studies included in the review were subject to data extraction. Results were summarised using a narrative approach.
Results
Serogroup A was the dominant cause of invasive meningococcal disease in Europe before and during World Wars I and II. Whilst serogroup B has been dominant from the 1970s in Europe and the 1980s in South America, outbreaks have emerged associated with serogroups W135 and Y in the twenty-first century. There has been a shift in the age groups affected by invasive meningococcal disease with an increase in incidence among the elderly associated with serogroup Y and a decline in serogroup C among adolescent populations. Recent outbreaks of serogroup W135 have occurred in some countries in South America. The epidemiological trend of invasive meningococcal disease has remained largely static across Africa and dominated by serogroup A although recently serogroups X and W135 have accounted for a large proportion of morbidity and mortality.
Conclusion
The epidemiology of N. meningitidis has been dynamic in Europe and South America especially over the last 30 years. Routine vaccination with serogroup C vaccines has led to reduced carriage and incidence of invasive meningococcal disease and herd immunity.
Keywords: Neisseria meningitidis, Serogroups, Meningococcal, Meningitis, Epidemiology
Introduction
Invasive meningococcal disease as meningitis and other sites is one of the foremost causes of morbidity and mortality globally. The case fatality rate is approximately 5–10%, and 12–20% of survivors suffer significant clinical sequelae including deafness, seizures, paralysis, amputation, and mental impairment.1–4 Bacterial meningitis is most commonly caused by invasive Neisseria meningitidis.
Meningococcal disease is a relatively new disease that was first observed in 1805 in Europe, 1806 in North America, and 1905 in Africa.5–7 During that time, it was recognised when clusters of cases occurred that presented with a rash and meningitis (cerebrospinal fever) that persisted for a week and was common in the military with a mortality of approximately 70%.5,8,9 Meningococcal disease usually presents with meningitis and less commonly with septicaemia.5 In 1950, N. meningitidis was classified into serogroups by an international committee.5,7 Thirteen serogroups have been characterised although serogroups A, B, C, W135, and Y are the most clinically significant in causing disease.4,5,10,11 Generally, the incidence of meningococcal disease varies by age, gender, socioeconomic conditions, the serogroup, and bacterial strain.2,5,11 Over the years, the epidemiology of invasive meningococcal disease has changed significantly in various regions of the world.
This study reports changes in trends of laboratory confirmed invasive meningococcal disease and strain diversity of N. meningitidis in Europe, South America, and Africa across all age groups over the last 100 years. We sought to complement previous reviews by summarising epidemiological data reporting rates of N. meningitidis carriage in Europe and South America and linking our findings to the implementation of vaccination strategies.
Methodology
This study is an epidemiological review of literature which describes changes in meningococcal biology over the past 100 years. A protocol including the literature search strategy and eligibility criteria was developed and is available on request from the corresponding author. A search was conducted in 2012 to identify literature from the continents of Europe (with special emphasis on Czech Republic, France, Germany, Greece, Norway, Russia, and United Kingdom), South America, and Central America (Belize, El Salvador, Guatemala, Honduras, Mexico, and Nicaragua). A brief review was conducted for Africa owing to the largely static epidemiological trend. On-going studies that had been presented in conferences were also identified and reviewed. Reference tracking and citation tracking were also carried out.
Healthcare databases searched were MEDLINE, PUBMED, Cochrane Database of Systematic Review, and the Database of Promoting Health Effectiveness Reviews. Sources of grey literature included OpenSIGLE, World Health Organization Global Index Medicus, and the European Centre of Disease Control and Prevention. After removing duplicate records, a three-stage sifting process was followed to screen the title, abstract, and full text of the identified articles against the protocol eligibility criteria. A piloted data extraction form was used to obtain descriptive information from each article by a single researcher. The extracted data was tabulated to aid narrative review, while the analysis and synthesis was done using Microsoft® Office Excel® 2007 version 12 (Microsoft Corporation, Richmond, VA, USA) to obtain summary statistics. No carriage studies conducted in South America were available in English.
Results
The search strategy yielded 3529 records and a total of 60 met the protocol eligibility criteria for inclusion (see Fig. 1). We identified 29 analytical epidemiological studies, 14 cross-sectional studies, 14 review articles, two case–control studies and one systematic review and meta-analysis. Tables 1 and 2 show data extracted from the included studies pertaining to the epidemiology of invasive meningococcal disease and carriage of N. meningitidis.
Figure 1.
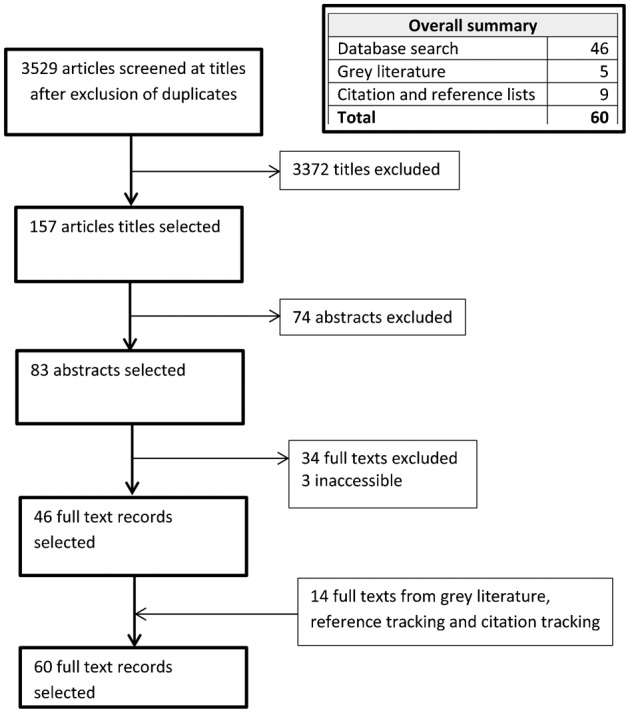
Summary of study selection process.
Table 1. Epidemiological studies describing incidence and serogroups of invasive meningococcal disease.
| Paper | Study area | Study period | Study design | Participant population | Number of participants | Incidence | Dominant serogroups (increases) | |
| Studies before serogrouping was introduced | ||||||||
| Houston et al.22 | England | 1907–1940 | Epidemiological analysis | Cases | ||||
| Arkwright21 | England, France | 1915 | Epidemiological analysis | Cases | Group B and P | |||
| Pringle23 | England | 1915–1917 | Epidemiological analysis | Cases | ||||
| Fairbrother20 | England | 1940–1947 | Epidemiological analysis | Cases | Group II | |||
| Studies after serogrouping was introduced | ||||||||
| Puricelli et al.47 | Brazil | 1971–2000 | Epidemiological analysis | Cases | 7893 | 6.4 | B | C |
| de Cassia et al.48 | Brazil | 1987–2003 | Epidemiological analysis | Cases | 5512 | 7.9 | B | C |
| Barroso et al.49 | Brazil | 1990–1996 | Epidemiological analysis | Cases | 2338 | – | B | C |
| Baethgen et al.50 | Brazil | 1995–2003 | Epidemiological analysis | Cases | 2215 | 3.5–1.8 | B | C |
| Cordeiro et al.51 | Brazil | 1996–2000 | Epidemiological analysis | Cases | 408 | 1.7 | B | C |
| Iser et al.52 | Brazil | Jun–Sept 2008 | Case–control | Patients neighbouring households | 8 cases 32 controls | 12 | C | – |
| Olivares et al.32 | France | 1987–1988 | Epidemiological analysis | Cases | 1132 | 0.7 | B | C |
| Perrocheau et al.44 | France | 2003 | Epidemiological analysis | cases | 803 | 1.8 | B | C |
| Grahlow et al.26 | Germany | 1971–1984 | Epidemiological analysis | Cases | 650 | – | B | C |
| Tzanakaki et al.36 | Greece | 1989–1991 | Epidemiological analysis | Cases | 31 | – | B | C |
| Kafetzis et al.41 | Greece | 1993–2004 | Epidemiological analysis | Cases | 1144 | – | B | C (A, W135) |
| Tsolia et al.35 | Greece | 1999–2000 | Epidemiological analysis | Cases | 157 | 10.2 | B | C (A) |
| Berild et al.28 | Norway | 1967–1979 | Epidemiological analysis | Cases | – | 24–43 | A, B | – |
| Bovre et al.30 | Norway | 1975–1979 | Epidemiological analysis | Cases | 1574 | 7.8 | B | – |
| Lystad et al.31 | Norway | 1975–1991 | Epidemiological analysis | Cases | – | 15–4.1 | B | C |
| Iversen et al.29 | Norway | 1992–1995 | Epidemiological analysis | Cases | 586 | 3.4 | B | C |
| Wylie et al.38 | England | 1982–1995 | Epidemiological analysis | Cases | 252 | 5.6 | ||
| Stanton et al.27 | England | 1977–2007 | Epidemiological analysis | Cases | 1157 | – | B | C |
| Gray et al.39 | England and Wales | 1993–2004 | Epidemiological analysis | Cases | 21 711 | 2.3–5.4 | B | C |
| Shigematsu et al.40 | England, Wales, and Northern Ireland | 1999–2001 | Epidemiological analysis | Cases | 11 522 | 9.2–8.0 | B | C (W135) |
| Demina et al.33 | USSR | 1980–1984 | Epidemiological analysis | Cases | 2653 | – | A | B |
| Connolly et al.34 | Europe | 1993–1996 | Epidemiological analysis | Cases from 35 countries | 16 734 | 1.1 | B | C |
| Trotter et al.72 | Europe | 1999–2004 | Epidemiological analysis | Cases from 27 countries | – | 0.2–5.4 | B | C |
Table 2. Epidemiological studies investigating carriage of N. meningitidis.
| Paper | Study area | Study period | Study design | Participant population | Number of participants | Carriage rate | Highest rate age group (%) | Dominant serogroup | Outbreak strain |
| Glover75 | England | Autumn 1917 | Survey | Military recruits | 3–38% | – | – | – | |
| Dudley et al.8 | England | 1933–1934 | Survey | Military recruits | 50 | – | Type II | – | |
| Jolley et al.56 | Czech Republic | Mar–Jun 1993 | Survey | 15–24 years | 1400 | 11.1 | – | – | – |
| Claus et al.65 | Germany | Nov 1999–Mar 2000 | Survey | 3–26 school children military camp | 8000 | 10.4 | 15–21 (18.1%) | B | – |
| 18–26 (32.6%) | |||||||||
| Glitza et al.57 | Germany | Feb–Sept 2000 | Survey | 15–18 years | 981 | 18.8 | – | B | – |
| Blackwell et al.59 | Greece | July 1990 | Survey | Military recruits | 993 | 25 | < 19 | – | – |
| Kremastinou et al.64 | Greece | Feb–Mar 1995 | Survey | 6–15-year old school children | 625 | 13.1 | – | A | – |
| Pavlopoulou et al.37 | Greece | Nov 2000–Feb 2001 | Survey | 2–19-year old school children | 554 | 4 | > 12 (9.2%) | C | – |
| Caugant et al.60 | Norway | Feb–Mar 1991 | Survey | All ages selected randomly | 943 | 9.6 | 20–24 (32.7%) | B | 8.8 |
| Bevanger et al.67 | Norway | 1 Oct–31 Dec 1995 | Survey | 0–19-year olds after 4 cluster cases in community | 523 | 9.4 | 18–19 (36.4%) | B | 0.8 |
| Cartwright et al.68 | UK | Nov 1986 | Survey | All ages | 6234 | 10.9 | 15–19 (24.5%) | B, C | 1.4 |
| Neal et al.58 | UK | Sept–Dec 1997 | Serial survey | 18–19-year-old first year university students | 2453 | 6.9–34.2 | B | 1–6.3 | |
| MacLennan et al.69 | UK | Autumn 1999 | Survey | 15–19 college students | 14 057 | 16.7 | 18–19 (22.6%) | – | – |
| Maiden et al.74 | UK | Oct–Dec 2000 | Survey | 15–17 students | 16 583 | 17.9 |
Epidemiology
Africa
Since the early twentieth century, meningococcal disease attributed to serogroup A has been dominant in sub-Saharan Africa, specifically in the Meningitis belt.2,12 Epidemics typically occur during the dry season with an annual incidence of 1000–1200 per 100 000 inhabitants per epidemic and 10–20 cases per 100 000 population during the non-epidemic seasons.2,4,12–14 Epidemics were first reported during 1905 in Ghana and Nigeria, and then later in 1934, 1942, and 1949.5–7 The epidemics due to serogroup A occurred in the 1950s in Nigeria and Sudan causing approximately 50 000 cases as well as 16 000 cases in Burkina Faso, although outbreaks caused by serogroup C were reported in the 1970s.7 In 1996, a major serogroup A outbreak affecting Burkina Faso, Chad, and Niger resulted in 250 000 cases and 25 000 deaths were reported.6,15,16 Serogroup Y has more recently been reported in Kenya, Burkina Faso, Togo, Ghana, and Niger during 1990–2000.6,15,17
Serogroup W135 was responsible for a major outbreak in Burkina Faso in 2002 following a Hajj pilgrimage affecting 13 000 people1,2,16,18 and in Niger between 2010 and 2011.19 In Gauteng Province of South Africa, serogroup W135 caused a rise in cases and replaced A as dominant with a five-fold increase to four cases per 100 000 population during 2003–2007.2,7,19 Serogroup X caused outbreaks in Niger reported in 2006 with 27.5 cases per 100 000 population and other outbreaks were reported in Ghana and Kenya in 2005 while 86% of 92 cases were reported in the Kara region of Togo.5,12,19 Serogroup A caused the majority of cases between 2007 and 2009 including an outbreak in 2007 in Burkina Faso which caused 26 878 cases.19
Europe
At the start of the twentieth century, large epidemics were reported across Europe predominantly caused by serogroup A.7,19–23 During 1904–1907 and 1915–1919 outbreaks linked to serogroup A that caused over 10 000 cases associated with military training camps were reported in Europe.5,7 During the period 1940–1942 over 54 000 cases were reported from England, Italy, and Germany.5,7 From the mid-to-late 1960s serogroup A outbreaks were reported in Norway and Russia13,24 while from 1966 to 1971, serogroup B accounted for more than half of the cases in the United Kingdom24 and was the dominant cause of cases in the Czech Republic, Germany, and Norway.24–27 Serogroup A was dominant in Norway from 1967 to 197328 which shifted to serogroup B in the mid-1970s and caused an outbreak in 1974.7,24,25,29–31 During 1971–1984 and 1987–1988 approximately half of the cases were due to serogroup B in Germany and France, respectively.26,32 A study conducted in Russia over 1980–1984 revealed that 58.2% of invasive meningococcal disease cases were caused by serogroup A.33 In the 1990s, serogroup C accounted for half of the cases in Czech Republic and was predominant until the end of the decade.3,34 However, peaks were observed in France, Germany, Greece, Norway, and the United Kingdom where the incidence of invasive meningococcal disease was largely attributed to serogroup B.1,3,29,34–38 Between 1993 and 1996 in Russia or the Soviet Union, approximately half of the cases were attributed to serogroup A.3,34 Cases due to serogroup W135 increased to account for approximately 3.6% of cases in France in 1999 as well as exhibiting a 25% increase in United Kingdom between 1999 and 2001.1,3,39,40 In Greece, a rise in cases due to serogroup A was observed from 4% in 1999 which peaked at 19.6–16.8% from 2001 to 2003 before declining to 4.7% in 2004.35,41 Increases from 3 to 8% in serogroup Y from 2006–2007 to 2010–2011 were noted in the United Kingdom, and a 17–31% rise was observed during 2008–2010 in Norway.19,24,39,42,43 Serogroup B is currently dominant across Europe, which has increased following the widespread use of the MenC vaccine.19,27,39,44
South America
Cases were identified as early as 1906 in Brazil and outbreaks were first reported in 1914 and 1920 in Brazil and Mexico, respectively with majority of cases due to serogroup A.7 Outbreaks were reported during the World War II period in Brazil, Chile, and Mexico.7,45 In 1974, 82% of cases were caused by serogroup C in Argentina while during the 1978–1979 outbreak in Chile, a serogroup shift from C to A occurred.7 In Brazil during the epidemic in 1972, 90% of cases were due to serogroup C while in 1974, 90% of cases were due to serogroup A.4,6,14,19,46 From 1987, Brazil had approximately more than three-quarters of invasive meningococcal disease attributed to serogroup B,4,47,48 while in Chile and Cuba, outbreaks caused by serogroup B occurred in 1985 and 1980 respectively.6,19,25,45 From 1990 to 1992, serogroup B caused more than 80% of invasive meningococcal disease in Brazil. A shift to serogroup C occurred during 1993–1996 which led to a rise of approximately 10 cases per 100 000 population in some parts of the country (particularly in Rio de Janeiro). However, there was another shift back to serogroup B towards the end of the decade which caused approximately 80% of cases.14,19,48–51 Serogroup C was dominant in Argentina from 1995 until the end of the decade.7,14,15,45 In the 2000s, serogroup B was the leading cause of disease although serogroup C increased from 2002 in Brazil and caused 63% of cases in Sao Paulo in 2005.4,19,48,50,52 From 2000 to 2006, two-thirds of isolates were from serogroup C in Ecuador.14 From 2006 to 2007, serogroup B accounted for two-thirds of cases in Argentina and Chile.14,19 Increases were noted due to serogroup Y with half of the cases in 2006 recorded in Colombia and Venezuela although these declined to 18 and 22% respectively in 2010.14,19 In Argentina, 28% of isolates were attributed to serogroup W135 in 2008 rising to half of all cases in 2010.19 Serogroup B dominated in Chile in 2010 and caused 67% of cases.19 Less than 10 confirmed cases were reported for each year for Bolivia, Paraguay, and Peru however serogroup B was predominant in Peru and Paraguay.14
Carriage
Studies on meningococcal carriage were conducted as far back as the early twentieth century although the distinction between N. meningitidis and N. lactamica was not made before 1969.53,54 This study therefore concentrated on studies performed after this date. A majority of the carriage studies were conducted among high-risk populations specifically among adolescents and young adults,55–58 the military,36,59 the general population,60,61 and also among close contacts.62
Europe
A study conducted in Czech Republic in 1980 among 0–24-year olds found a carriage rate of 10.2% with serogroup B dominant at 43.9%.62,63 Two studies surveyed all age groups in the population in 1986 from the United Kingdom and 1991 from Norway had carriage rates of 10.9% and 9.6% respectively with a predominance in serogroup B.60,61 A study conducted among school children aged 6–15 years in 1995 found a carriage rate of 13% with a predominance of serogroup A at 28%.35,64 A study conducted in 2000 among Greek school children aged 2–19 years found a carriage rate of 4%, (which increased to 9.3% for the children older than 12 years) but among the isolates obtained, 32% belonged to serogroup C and 23% belonged to serogroup B.37 In Germany, a study conducted in 2000 among teenagers 15–18 years following an increased incidence reported a carriage rate of 18.8% with a predominance of serogroup B at 12.3%.57,62 A different study also conducted in Germany between 1999 and 2000 found a carriage rate of 10.4% with a dominance of serogroup B at 32%.65 Among military recruits, two studies conducted in Germany in 2000 and Greece in 1990 had carriage rates of 32.6% and 25% respectively.65,57 Among preschool-aged children, school-aged children, and adults aged up to 26 years, four studies reported the highest carriage rates among ages ranging from 15 to 24 years.60,61,63,65 A systematic review conducted in 2010 reported that the highest rate of carriage was among 19-year olds at 24%54 and approximately 35% of young adults in Europe carried N. meningitidis at one point in time over the last decade.66 The rate of carriage ranged from 9.2 to 32.7% with serogroup B as dominant and outbreak strains ranging from 0.8 to 8.8%.56,60,65,67–69
Discussion
Since the 1970s serogroups A, B, and C have accounted for 90% of meningococcal disease globally; before that date serogroup A dominated in African and European countries.2,70,71 Outbreaks due to serogroup A have been reported in Russia and Greece in the 1960s and 1980s, although epidemics have not been observed over these times across Europe.24,33 Over the last decade, there has equally been a noticeable increase in the incidence of disease caused by serogroups W135 and Y particularly among adults and the elderly.12,14,35 Serogroup A was the dominant cause of infections in Europe before and during both World Wars but largely disappeared after World War II.1,5,6,15
The 1990s saw a rise in the incidence of serogroup C and this serogroup was the dominant cause of infections in Czech Republic, with peaks in Greece and the United Kingdom.3,34 This was until the introduction of the MenC vaccine which lead to serogroup B dominating and a decline in incidence in the 2000s.6,19,41,42,72 The MenC vaccine was first introduced in 1999 in the United Kingdom and a 93% protective effect was found among teenagers in a study conducted the same year.73 After one year of vaccination, the incidence of disease was observed to have reduced by 81% and herd immunity was induced4,54,66,74 while carriage reduced by 66% from 1999 to 2000.1,4,74 This finding suggests that whilst vaccination may provide protection against serogroup-specific colonisation and disease, further studies should investigate the impact of routine vaccination programmes on shifting dominant serogroups and outbreak strains within defined populations.
Studies showed that serogroup B dominated in numerous countries36,57,58,60,62,65,67,68 although in Greece serogroup A was reported as dominant in 199564 and serogroup C in 2000.37 The longitudinal studies found rates ranging 6.9–34% and 17.5–20.6%.58 The acquisition rate was high in one study possibly due to more socialisation with peers.69
A majority of the carriage studies were conducted among high-risk populations. Carriage was highest among military populations.59,65,75 Among civilian populations, carriage ranged from 4 to 18.8% although two-thirds of participants were less than 12 years old in the study where the lowest average carriage rate of 4% was reported.37,57
It was reported that the presence of respiratory infections facilitates carriage but no evidence of association between respiratory infections and carriage was found in two studies.37,60 However, the number of persons with respiratory infections was too small for an independent analysis in one of the studies.59 Age, male sex, socialising with peers, overcrowding, and active or passive smoking were associated with carriage in some studies.37,54,60,68 Studies that reported no association with smoking had small sample sizes compared to those which found an association which may suggest the former studies lacked sufficient statistical power to detect an association. The largest teenager study showed carriage in males and was explained by social factors.55
Epidemiological data shows that serogroup B meningococcal infections continue to pose a significant burden on human health. From 2008, Novartis Vaccines conducted clinical trials with a MenB vaccine which covers all meningococcal serogroups and relies on other surface targets. Clinical studies have so far demonstrated that this provides an immunological memory and a good safety and tolerability profile. Phase III clinical trial data indicates it could be used for all ages and dispensed with routine vaccines.17
The Meningitis Vaccine Project has led to the development of a conjugate serogroup A vaccine (MenAfriVac) specifically for the Meningitis belt in Africa.76 This was introduced in 2010 with mass vaccinations for persons aged 1–29 years in Burkina Faso and parts of Niger and Mali.6,13,15,19,76 No cases due to serogroup A were detected in Burkina Faso the year after the campaign. The vaccine has been found to be immunogenic and safe, with a 94% difference in crude incidence of meningitis in the areas with mass vaccination verses areas without mass vaccination in Chad in 2012.77,78
This review has a number of limitations which warrant discussion. Although active surveillance of invasive meningococcal disease has been performed in many countries (perhaps increasingly over the last two decades), data was not published or accessible from numerous countries. Relatively few data were available especially before the 1970s. The establishment of national reference laboratories for surveillance and microbiological characterisation of clinical isolates varied across countries. Whilst the search strategy was deemed to be sufficiently robust using four electronic databases as well as grey literature from other credible sources, some relevant literature is likely to have been missed since included articles were restricted to those published in English. Underreporting of cases could have occurred as well as ascertainment, recruitment, and misclassification bias in the studies.
Conclusion
Whilst serogroup B dominates in numerous countries, outbreaks of invasive meningococcal disease caused by serogroups W135 and Y have been observed in numerous countries in recent years. The spread of virulent strains may have been facilitated by international travel and mass gatherings of susceptible individuals as demonstrated by the Hajj pilgrimage outbreaks. There has been a shift in the age groups affected by invasive meningococcal disease with an increase among the elderly due to serogroup Y and a decrease in adolescents due to serogroup C. Very low incidences of disease were reported in some countries compared to others which may be explained through underreporting of cases. Routine serogroup C vaccination programmes have played an important role in reducing carriage rates and the incidence of disease as well as inducing herd immunity.
References
- 1.Pollard AJ. Global epidemiology of meningococcal disease and vaccine efficacy. Pediatr Infect Dis J. 2004;23:S274–9. [PubMed] [Google Scholar]
- 2.Al-Tawfiq JA, Clark TA, Memish ZA. Meningococcal disease: the organism, clinical presentation, and worldwide epidemiology. J Travel Med. 2010;17:3–8. doi: 10.1111/j.1708-8305.2010.00448.x. [DOI] [PubMed] [Google Scholar]
- 3.Cartwright K, Noah N, Peltola HMeningococcal Disease Advisory Board. Meningococcal disease in Europe: epidemiology, mortality, and prevention with conjugate vaccines. Report of a European advisory board meeting Vienna, Austria, 6–8 October, 2000. Vaccine. 2001194347–56. [DOI] [PubMed] [Google Scholar]
- 4.Safadi MA, Barros AP. Meningococcal conjugate vaccines: efficacy and new combinations. J Pediatr (Rio J). 2006;82:S35–44. doi: 10.2223/JPED.1495. [DOI] [PubMed] [Google Scholar]
- 5.Frosch M, Maiden MCJ. Handbook of meningococcal disease: infection biology, vaccination, clinical management. Weinheim, Germany: Wiley-VCH; 2006. [Google Scholar]
- 6.Safadi MAP, McIntosh EDG. Epidemiology and prevention of meningococcal disease: a critical appraisal of vaccine policies. Expert Rev Vaccines. 2011;10:1717–30. doi: 10.1586/erv.11.159. [DOI] [PubMed] [Google Scholar]
- 7.Leimkugel J, Racloz V, Jacintho da Silva L, Pluschke G. Global review of meningococcal disease. A shifting etiology. J Bacteriol Res. 2009;1:6–18. [Google Scholar]
- 8.Dudley SF, Brennan JR. High and persistent carrier rates of Neisseria meningitidis, unaccompanied by cases of Meningitis. J Hyg. 1934;34:525–41. doi: 10.1017/s0022172400043291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Medical progress: Meningococcal disease. N Engl J Med. 2001;344:1378–88. doi: 10.1056/NEJM200105033441807. [DOI] [PubMed] [Google Scholar]
- 10.Ibarz-Pavón AB, MacLennan J, Andrews NJ, Gray SJ, Urwin R, Clarke SC. Changes in serogroup and genotype prevalence among carried meningococci in the United Kingdom during vaccine implementation. J. Infect. Dis. 2011;204:1046–53. doi: 10.1093/infdis/jir466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kristiansen AP, Diomandé F, Wei CS, Ouédraogo R, Sangaré L, Sanou I. Baseline meningococcal carriage in Burkina Faso before the introduction of a meningococcal serogroup A conjugate vaccine. Clin Vaccine Immunol. 2011;18:435–43. doi: 10.1128/CVI.00479-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrison LH, Trotter CL, Ramsay ME. Global epidemiology of meningococcal disease. Vaccine. 2009;2:B51–63. doi: 10.1016/j.vaccine.2009.04.063. [DOI] [PubMed] [Google Scholar]
- 13.Morley SL, Pollard AJ. Vaccine prevention of meningococcal disease, coming soon? Vaccine. 2001;20:666–87. doi: 10.1016/s0264-410x(01)00410-8. [DOI] [PubMed] [Google Scholar]
- 14.Safadi MAP, Cintra OAL. Epidemiology of meningococcal disease in Latin America: current situation and opportunities for prevention. Neurol Res. 2010;32:263–71. doi: 10.1179/016164110X12644252260754. [DOI] [PubMed] [Google Scholar]
- 15.Khatami A, Pollard AJ. The epidemiology of meningococcal disease and the impact of vaccines. Expert Rev Vaccines. 2010;9:285–98. doi: 10.1586/erv.10.3. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Meningococcal meningitis. Geneva: World Health Organization; 2003. [Google Scholar]
- 17.Panatto D, Amicizia D, Lai PL, Gasparini R. Neisseria meningitidis B vaccines. Expert Rev Vaccines. 2011;10:1337–51. doi: 10.1586/erv.11.103. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Emergence of W135 meningococcal disease. Geneva: World Health Organization; 2001. [Google Scholar]
- 19.Halperin SA, Bettinger JA, Greenwood B, Harrison LH, Jelfs J, Ladhani SN, et al. The changing and dynamic epidemiology of meningococcal disease. Vaccine. 2012;30:B26–B36. doi: 10.1016/j.vaccine.2011.12.032. [DOI] [PubMed] [Google Scholar]
- 20.Fairbrother RW. Meningococcal meningitis with particular reference to epidemiology and pathogenesis. J Clin Pathol. 1947;1:10–8. doi: 10.1136/jcp.1.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arkwright JA. Grouping of the strains of meningococcus: isolated during the epidemic of cerebrospinal meningitis in 1915. Br Med J. 1915;2:885–8. doi: 10.1136/bmj.2.2868.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Houston T, Rankin JC. Cerebro-spinal fever and meningococci infection. Ulster Med J. 1940;9:61–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Pringle AM. The epidemiology of meningococcal meningitis, or cerebro-spinal fever. BMJ. 1918;1:398. doi: 10.1136/bmj.1.2988.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kriz P, Wieffer H, Holl K, Rosenlund M, Budhia S, Vyse A. Changing epidemiology of meningococcal disease in Europe from the mid-20th to the early 21st Century. Expert Rev Vaccines. 2011;10:1477–86. doi: 10.1586/erv.11.117. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz B, Moore PS, Broome CV. Global epidemiology of meningococcal disease. Clin Microbiol Rev. 1989;2:S118–S24. doi: 10.1128/cmr.2.suppl.s118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grahlow WD, Ocklitz HW, Mochmann H. Meningococcal infections in the German Democratic Republic 1971–1984. Infection. 1986;14:286–8. doi: 10.1007/BF01643964. [DOI] [PubMed] [Google Scholar]
- 27.Stanton MC, Taylor-Robinson D, Harris D, et al. Meningococcal disease in children in Merseyside, England: a 31 year descriptive study. PLoS One. 2011;6:e25957. doi: 10.1371/journal.pone.0025957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berild D, Gedde-Dahl TW, Abrahamsen T. Meningococcal disease in the Norwegian Armed Forces 1967–1979. Some epidemiological aspects. NIPH Ann. 1980;3:23–30. [PubMed] [Google Scholar]
- 29.Iversen BG, Aavitsland P. Meningococcal disease in Norway 1992–1995. Epidemiology and fatality. Scand J Infect Dis. 1996;28:253–9. doi: 10.3109/00365549609027167. [DOI] [PubMed] [Google Scholar]
- 30.Bovre K, Gedde-Dahl TW. Epidemiological patterns of meningococcal disease in Norway 1975–1979. NIPH Ann. 1980;3:9–22. [PubMed] [Google Scholar]
- 31.Lystad A, Aasen S. The epidemiology of meningococcal disease in Norway 1975–91. NIPH Ann. 1991;14:57–65. discussion-6. [PubMed] [Google Scholar]
- 32.Olivares R, Hubert B. Clusters of meningococcal disease in France (1987–1988). Eur J Epidemiol. 1992;8:737–42. doi: 10.1007/BF00145393. [DOI] [PubMed] [Google Scholar]
- 33.Demina AA, Pokrovskij VI, Iljina TI, Larina LI, Devjakina NP. Surveillance of meningococcal infections and other forms of purulent meningitis: a 4-year study in the USSR. Bull World Health Organ. 1986;64:263–9. [PMC free article] [PubMed] [Google Scholar]
- 34.Connolly M, Noah N. Is group C meningococcal disease increasing in Europe? A report of surveillance of meningococcal infection in Europe 1993–6. European Meningitis Surveillance Group. Epidemiol Infect. 1999;122:41–9. doi: 10.1017/s0950268898001848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsolia MN, Theodoridou M, Tzanakaki G, Kalabalikis P, Urani E, Mostrou G, et al. The evolving epidemiology of invasive meningococcal disease: a two-year prospective, population-based study in children in the area of Athens. FEMS Immunol Med Microbiol. 2003;36:87–94. doi: 10.1016/S0928-8244(03)00083-X. [DOI] [PubMed] [Google Scholar]
- 36.Tzanakaki G, Blackwell CC, Kremastinou J, Weir DM, Mentis A, Fallon RJ. Serogroups, serotypes and subtypes of Neisseria meningitidis isolated from patients and carriers in Greece. J Med Microbiol. 1993;38:19–22. doi: 10.1099/00222615-38-1-19. [DOI] [PubMed] [Google Scholar]
- 37.Pavlopoulou ID, Daikos GL, Alexandrou H, Petridou E, Pangalis A, Theodoridou M, et al. Carriage of Neisseria meningitidis by Greek children: risk factors and strain characteristics. Clin Microbiol Infect. 2004;10:137–42. doi: 10.1111/j.1469-0691.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- 38.Wylie PAL, Stevens D, Drake W, Stuart J, Cartwright K. Epidemiology and clinical management of meningococcal disease in West Gloucestershire: retrospective, population based study. BMJ. 1997;315:774–9. doi: 10.1136/bmj.315.7111.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Unit Meningococcal Reference, Gray SJ, Trotter CL, Ramsay ME, Guiver M, Fox AJ, et al. Epidemiology of meningococcal disease in England and Wales 1993/94 to 2003/04: contribution and experiences of the Meningococcal Reference Unit. J Med Microbiol. 2006;55:887–96. doi: 10.1099/jmm.0.46288-0. [DOI] [PubMed] [Google Scholar]
- 40.Shigematsu M, Davison KL, Charlett A, Crowcroft NS. National enhanced surveillance of meningococcal disease in England, Wales and Northern Ireland, January 1999–June 2001. Epidemiol Infect. 2002;129:459–70. doi: 10.1017/s0950268802007549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kafetzis DA, Stamboulidis KN, Tzanakaki G, Kourea Kremastinou J, Skevaki CL, Konstantopoulos A, et al. Meningococcal group C disease in Greece during 1993–2006: the impact of an unofficial single-dose vaccination scheme adopted by most paediatricians. Clin Microbiol Infect. 2007;13:550–2. doi: 10.1111/j.1469-0691.2007.01704.x. [DOI] [PubMed] [Google Scholar]
- 42.ECDC. Annual epidemiological report 2011. Stockholm: European Centre for Disease Prevention and Control; 2011. [PubMed] [Google Scholar]
- 43.Ladhani SN, Flood JS, Ramsay ME, Campbell H, Gray SJ, Kaczmarski EB, et al. Invasive meningococcal disease in England and Wales: Implications for the introduction of new vaccines. Vaccine. 2012;30:3710–6. doi: 10.1016/j.vaccine.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 44.Perrocheau A, Taha MK, Levy-Bruhl D. Epidemiology of invasive meningococcal disease in France in 2003. . Euro Surveill. 2005;10:238–41. [PubMed] [Google Scholar]
- 45.Safadi MA, Gonzalez-Ayala S, Jakel A, Wieffer H, Moreno C, Vyse A. The epidemiology of meningococcal disease in Latin America 1945–2010: an unpredictable and changing landscape. Epidemiol Infect. 2012:1–12. doi: 10.1017/S0950268812001689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De Gaspari E, Zollinger W. Expression of class 5 antigens by meningococcal strains obtained from patients in Brazil and evaluation of two new monoclonal antibodies. Braz J Infect Dis. 2001;5:143–53. doi: 10.1590/s1413-86702001000300007. [DOI] [PubMed] [Google Scholar]
- 47.Puricelli RCB, Kupek E, Westrupp MHB. Three decades of meningococcal disease in the state of Santa Catarina, Brazil. Braz J Infect Dis. 2004;8:241–8. doi: 10.1590/s1413-86702004000300008. [DOI] [PubMed] [Google Scholar]
- 48.de Cassia Campos Bertoncini R, Andre Herberts R, Goulart Dario M, Roberto Merlin C, Miletti LC. Epidemiological study of Neisseria meningitidis strains isolated from cases of meningococcal disease in Santa Catarina State, Brazil, 1987–2003. Public Health. 2007;121:880–3. doi: 10.1016/j.puhe.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 49.Barroso DE, Carvalho DM, Casagrande ST, Rebelo MC, Soares V, Zahner V, et al. Microbiological epidemiological history of meningococcal disease in Rio de Janeiro, Brazil. Braz J Infect Dis. 2010;14:242–51. [PubMed] [Google Scholar]
- 50.Baethgen LF, Weidlich L, Moraes C, Klein C, Nunes LS, Cafrune PI, et al. Epidemiology of meningococcal disease in southern Brazil from 1995 to 2003, and molecular characterization of Neisseria meningitidis using multilocus sequence typing. Trop Med Int Health. 2008;13:31–40. doi: 10.1111/j.1365-3156.2007.01970.x. [DOI] [PubMed] [Google Scholar]
- 51.Cordeiro SM, Neves AB, Ribeiro CT, Petersen ML, Gouveia EL, Ribeiro GS, et al. Hospital-based surveillance of meningococcal meningitis in Salvador, Brazil. Trans R Soc Trop Med Hyg. 2007;101:1147–53. doi: 10.1016/j.trstmh.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Iser BP, Lima HC, de Moraes C, de Almeida RP, Watanabe LT, Alves SL, et al. Outbreak of Neisseria meningitidis C in workers at a large food-processing plant in Brazil: challenges of controlling disease spread to the larger community. Epidemiol Infect. 2012;140:906–15. doi: 10.1017/S0950268811001610. [DOI] [PubMed] [Google Scholar]
- 53.Hollis DG, Wiggins GL, Weaver RE. Neisseria lactamicus sp. n., a lactose-fermenting species resembling Neisseria meningitidis. Appl Microbiol. 1969;17:71–7. doi: 10.1128/am.17.1.71-77.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Christensen H, May M, Bowen L, Hickman M, Trotter CL. Meningococcal carriage by age: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:853–61. doi: 10.1016/S1473-3099(10)70251-6. [DOI] [PubMed] [Google Scholar]
- 55.MacLennan J, Kafatos G, Neal K, Andrews N, Cameron JC, Roberts R, et al. Social behavior and meningococcal carriage in British teenagers. Emerg Infect Dis. 2006;12:950–7. doi: 10.3201/eid1206.051297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jolley KA, Kalmusova J, Feil EJ, Gupta S, Musilek M, Kriz P, et al. Carried meningococci in the Czech Republic: a diverse recombining population. J Clin Microbiol. 2000;38:4492–8. doi: 10.1128/jcm.38.12.4492-4498.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Glitza IC, Ehrhard I, Mueller-Pebody B, Reintjes R, Breuer T, Ammon A, et al. Longitudinal study of meningococcal carrier rates in teenagers. Int J Hyg Environ Health. 2008;211:263–72. doi: 10.1016/j.ijheh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 58.Neal KR, Nguyen-Van-Tam JS, Jeffrey N, Slack RC, Madeley RJ, Ait-Tahar K, et al. Changing carriage rate of Neisseria meningitidis among university students during the first week of term: cross sectional study. BMJ. 2000;320:846–9. doi: 10.1136/bmj.320.7238.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blackwell CC, Tzanakaki G, Kremastinou J, Weir DM, Vakalis N, Elton RA, et al. Factors affecting carriage of Neisseria meningitidis among Greek military recruits. Epidemiol Infect. 1992;108:441–8. doi: 10.1017/s0950268800049943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Caugant DA, Hoiby EA, Magnus P, Scheel O, Hoel T, Bjune G, et al. Asymptomatic carriage of Neisseria meningitidis in a randomly sampled population. J Clin Microbiol. 1994;32:323–30. doi: 10.1128/jcm.32.2.323-330.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cartwright KAV, Stuart JM, Jones DM, Noah ND. The stonehouse survey: nasopharyngeal carriage of meningococci and Neisseria lactamica. Epidemiol Infect. 1987;99:591–601. doi: 10.1017/s0950268800066449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Soriano-Gabarro M, Wolter J, Hogea C, Vyse A. Carriage of Neisseria meningitidis in Europe: a review of studies undertaken in the region. Expert Rev Anti Infect Ther. 2011;9:761–74. doi: 10.1586/eri.11.89. [DOI] [PubMed] [Google Scholar]
- 63.Kriz P, Kriz B, Svandova E, Musilek M. Antimeningococcal herd immunity in the Czech Republic–influence of an emerging clone, Neisseria meningitidis ET-15/37. Epidemiol Infect. 1999;123:193–200. doi: 10.1017/s095026889900285x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kremastinou J, Tzanakaki G, Velonakis E, Voyiatzi A, Nickolaou A, Elton RA, et al. Carriage of Neisseria meningitidis and Neisseria lactamica among ethnic Greek school children from Russian immigrant families in Athens. FEMS Immunol Med Microbiol. 1999;23:13–20. doi: 10.1111/j.1574-695X.1999.tb01711.x. [DOI] [PubMed] [Google Scholar]
- 65.Claus H, Maiden MC, Wilson DJ, McCarthy ND, Jolley KA, Urwin R, et al. Genetic analysis of meningococci carried by children and young adults. J Infect Dis. 2005;191:1263–71. doi: 10.1086/428590. [DOI] [PubMed] [Google Scholar]
- 66.Caugant DA, Tzanakaki G, Kriz P. Lessons from meningococcal carriage studies. FEMS Microbiol Rev. 2007;31:52–63. doi: 10.1111/j.1574-6976.2006.00052.x. [DOI] [PubMed] [Google Scholar]
- 67.Bevanger L, Bergh K, Gisnas G, Caugant DA, Froholm LO. Identification of nasopharyngeal carriage of an outbreak strain of Neisseria meningitidis by pulsed-field gel electrophoresis versus phenotypic methods. J Med Microbiol. 1998;47:993–8. doi: 10.1099/00222615-47-11-993. [DOI] [PubMed] [Google Scholar]
- 68.Cartwright KAV, Stuart JM, Jones DM, Noah ND. The Stonehouse survey: nasopharyngeal carriage of meningococci and Neisseria lactamica. Epidemiology Infect. 1987;99:591–601. doi: 10.1017/s0950268800066449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.MacLennan J, Kafatos G, Neal K, Andrews N, Cameron JC, Roberts R, et al. Social behavior and meningococcal carriage in British teenagers. Emerg Infect Dis. 2006;12:950–7. doi: 10.3201/eid1206.051297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Barroso DE, Rebelo MC. Recognition of the epidemiological significance of Neisseria meningitidis capsular serogroup W135 in the Rio de Janeiro region, Brazil. Mem Inst Oswaldo Cruz. 2007;102:773–5. doi: 10.1590/s0074-02762007005000104. [DOI] [PubMed] [Google Scholar]
- 71.World Health Organization. Control of epidemic meningococcal disease. WHO practical guidelines. Geneva: World Health Organization; 1998. 2nd edn. [Google Scholar]
- 72.Trotter CL, Chandra M, Cano R, Larrauri A, Ramsay ME, Brehony C, et al. A surveillance network for meningococcal disease in Europe. FEMS Microbiol Rev. 2007;31:27–36. doi: 10.1111/j.1574-6976.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- 73.Bose A, Coen P, Tully J, Viner R, Booy R. Effectiveness of meningococcal C conjugate vaccine in teenagers in England. Lancet. 2003;361:675–6. doi: 10.1016/S0140-6736(03)12563-9. [DOI] [PubMed] [Google Scholar]
- 74.Maiden MC, Stuart JM UK Meningococcal Carriage Group. Carriage of serogroup C meningococci 1 year after meningococcal C conjugate polysaccharide vaccination. Lancet. 2002;359:1829–30. doi: 10.1016/S0140-6736(02)08679-8. [DOI] [PubMed] [Google Scholar]
- 75.Glover JA. Observations on the meningococcus carrier-rate in relation to density of population in sleeping quarters. J Hyg. 1918;17:367–79. doi: 10.1017/s0022172400007221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chang Q, Tzeng Y-L, Stephens DS. Meningococcal disease: changes in epidemiology and prevention. Clin Epidemiol. 2012:237–45. doi: 10.2147/CLEP.S28410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Daugla D, Gami J, Gamougam K, Naibei N, Mbainadji L, Narbé M, et al. Effect of a serogroup A meningococcal conjugate vaccine (PsA–TT) on serogroup A meningococcal meningitis and carriage in Chad: a community trial. Lancet. 2013 doi: 10.1016/S0140-6736(13)61612-8. pii: S0140-6736(13)61612-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sow SO, Okoko BJ, Diallo A, Viviani S, Borrow R, Carlone G, et al. Immunogenicity and safety of a meningococcal a conjugate vaccine in Africans. N Engl J Med. 2011;364:2293–3304. doi: 10.1056/NEJMoa1003812. [DOI] [PubMed] [Google Scholar]


