Abstract
Most arthroscopic rotator cuff repairs utilize suture passing devices placed through arthroscopic cannulas. These devices are limited by the size of the passing device where the suture is passed through the tendon. An alternative technique has been used in the senior author’s practice for the past ten years, where sutures are placed through the rotator cuff tendon using percutaneous passing devices. This technique, dubbed the global percutaneous shuttling technique of rotator cuff repair, affords the placement of sutures from nearly any angle and location in the shoulder, and has the potential advantage of larger suture bites through the tendon edge. These advantages may increase the area of tendon available to compress to the rotator cuff footprint and improve tendon healing and outcomes. The aim of this study is to describe the global percutaneous shuttling (GPS) technique and report our results using this method. The GPS technique can be used for any full thickness rotator cuff tear and is particularly useful for massive cuff tears with poor tissue quality. We recently followed up 22 patients with an average follow up of 32 months to validate its usefulness. American Shoulder and Elbow Surgeons scores improved significantly from 37 preoperatively to 90 postoperatively (P<0.0001). This data supports the use of the GPS technique for arthroscopic rotator cuff repair. Further biomechanical studies are currently being performed to assess the improvements in tendon footprint area with this technique.
Key words: rotator cuff repair, percutaneous, arthroscopy
Introduction
Rotator cuff tears are a common clinical problem. Traditional techniques of repair include open surgical repair and mini-open repair. Newer, more minimally invasive techniques allow for smaller incisions and potential for decreased pain.1,2 Arthroscopic techniques have rapidly evolved and include many minimally invasive techniques. A successful repair requires the surgeon to master a number of tasks including tear pattern recognition, arthroscopic cuff mobilization, suture management, and arthroscopic knot tying.3 There are a number of different techniques for passing the suture through the rotator cuff tendon including direct and indirect (shuttling) techniques.4 Shuttling relay causes minimal trauma to the rotator cuff tissue, which may be delaminated or of poor quality. Percutaneous entry portals for instruments and suture passage allow flexibility in obtaining the correct angle and position of the sutures as well as variation in size of the suture bites.
For the past ten years, the senior author has performed a percutaneous technique, dubbed Global Percutaneous Shuttling (GPS) using a curved, shuttling device (Banana suture lasso, Arthrex, Naples, FL, USA). The short and smaller size of the instrument allows for access to the cuff tendon edge from any angle without the need to create a separate portal. The entry percutaneous portal measures less than 2 mm and leaves virtually no scar at the time of wound healing. Moreover, the short length of the instrument as well as the angle of the instrument allows for easy manipulation and maneuvering around large patients.5-7 The GPS technique can be used for any full thickness rotator cuff tear, and is particularly useful in massive cuff tears with poor tissue quality.7 This can be a useful technique where other instruments may be difficult to allow proper placement of the repair.
Materials and Methods
Surgical technique
The patient can be positioned in either the modified beach chair position (author’s preference) or in the lateral decubitus position ensuring that the shoulder is adequately exposed. This can be facilitated by the use of special arthroscopy tables where the patient’s shoulder and upper torso can be maximally exposed up to the level of the medial angle of the scapula while allowing for a secure positioning of the patient’s head and lower body. The arm can be placed in a special positioner (Spider; Tenet Medical, Calgary, AB, USA) to allow for traction on the arm thereby opening the subacromial space.
An anthropometric study of shoulder width dimensions was performed on seventy consecutive arthroscopic repairs after prepping and draping the patients positioned in a beach chair arthroscopic table (Tenet Medical). The distance from the Neviaser portal entry point to the medial neck crease line was on average 10.68 mm; from the anterolateral corner of the acromion to the medial neck crease line along the clavicle was 15.23 mm and from the posterolateral portal to the medial neck crease along the scapular spine was 14.73 mm. This provides the surgeon with a rough guideline of the appropriate amount of prepping required to perform this percutaneous technique.
The anatomical landmarks are drawn to provide a guideline for placement of the various percutaneous access points. Standard posterior and anterior portals are created by feeling the soft spot between the humeral head and the glenoid. The location of the posterior portal will often depend on the size of the patient’s shoulder. The placement of the lateral portal varies depending on the tear location (either anterolateral for anterosuperior tear or directly lateral for a large U shape tear). A standard glenohumeral diagnostic arthroscopy is first performed to rule out any associated pathology (labral tears, arthritis, subscapularis tears). Mobilization of the cuff tissue can be performed at this time to free up the tendon from the glenoid with the use of the electrocautery device or an elevator. This is critical in large to massive cuff tears with retraction and scarring of the cuff tissue edge.
The camera is then moved to the subacromial space where a thorough bursectomy is performed to allow for visualization. Careful hemostasis and clearing of the medial bursa is critical for passage of the percutaneous device. The tear configuration is then identified and the tendon mobility is assessed by pulling on the tendon edge with a tissue grasper. Additional tendon releases should be performed at this time if the tendon edge cannot be adequately reapproximated to the anatomic footprint to allow for a tension-free repair. This can be achieved with a cautery device, elevator or by performing interval slides. Suture anchors (single or doubly loaded) are then inserted (Figure 1) via a percutaneous superior lateral access point just lateral to the lateral edge of the acromion. Sutures are left through the percutaneous access point to avoid suture entanglement. The suture that will be shuttled is retrieved via the lateral portal.
Figure 1.

Placement of the suture anchor with regard to the rotator cuff tear.
The percutaneous shuttling device can then be passed via percutaneous anteromedial,8 superior medial or posterior medial access points shown in Figure 2. The safety of these access points has been previously described.5-7,9-11 The posterior medial access point can be used for large tear with posteromedial retraction. Superiormedial and anteromedial access points are ideal for inserting a penetrating device through the supraspinatus. It is important to stay superficial to the infraspinatus and teres minor until the torn edge of the cuff is encountered so as to avoid injury to the suprascapular nerve.12 Caution is used to stay in the safe zone for avoiding suprascapular nerve injury along its path 2.5 cm from the supraglenoid tubercle and 1.8 cm from the posterior rim of the glenoid.13,14
Figure 2.
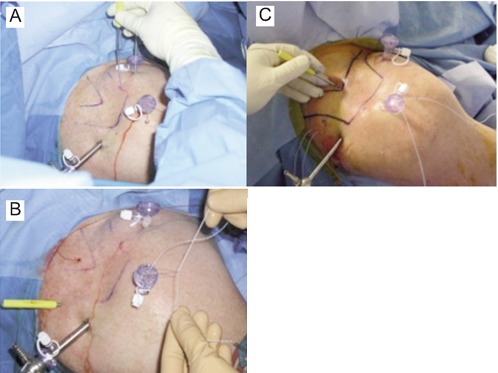
Anterior medial (A), superior medial (B), and posterior medial (C) percutaneous access and shuttling technique.
The percutaneous passing device penetrates a healthy portion of the torn rotator cuff with the aid of a grasper from the lateral portal (Figure 3) and the passing wire or suture is pulled through the lateral cannula (Figure 4) along with the more medial suture limb. The wire along with the suture limb is pulled back through the percutaneous access point. The sutures are passed through the lateral cannula and an arthroscopic knot is tied to secure the fixation (Figure 5).
Figure 3.
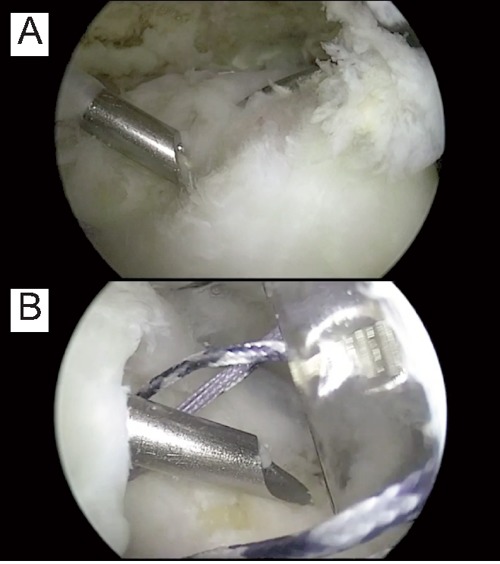
The Banana Suture Lasso is being passed through the medial rotator cuff tissue (A) and it comes out on the inferior aspect and lateral to the rotator cuff (B).
Figure 4.
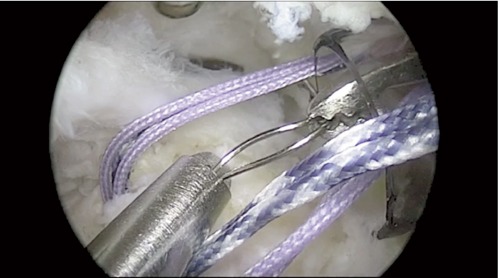
The wire being grasped out of the Banana Lasso in order for the suture to be placed through it.
Figure 5.
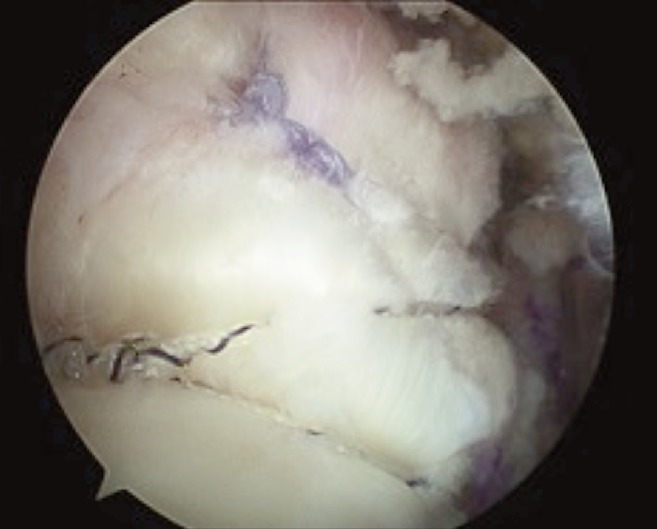
Final repair of the rotator cuff.
Outcomes
There were 55 patients who had undergone arthroscopic rotator cuff repair using the GPS technique by one surgeon and were at least 1 year post-surgery, whom were invited for evaluation. Validated outcome measurements including the visual analog scale (VAS) at rest and with activity,15 the American Shoulder and Elbow Society score and the short form-36 (SF36) scores were obtained preoperatively and at long-term follow-up.16 Clinical parameters including active and passive forward elevation, external rotation, and internal rotation were collected preoperatively and postoperatively. Twenty-two patients with minimum one-year follow up were available for evaluation. Paired t-tests evaluated outcome variable differences for preoperative and postoperative groups using Stata v.12 (Stata Corp., College Station, TX, USA). In all cases, statistical significance was set to P<0.05 a priori.
Mean patient age was 59 (range 39-77). Average follow up after surgery was 32 months (12-88). Mean preoperative VAS score was 4 at rest and 7 with activity decreased significantly to a postoperative rest and activity scores of 1 and 1, respectively (P<0.001, P<0.001). Preoperative active and passive forward elevation had a mean value of 160 degrees (range 90-180), which significantly improved to 170 degrees (range 165-180) postoperatively (P=0.0013). Preoperative active and passive external rotation averaged 69 degrees (range 30-85) and significantly improved to 77 degrees (range 30-90) postoperatively (P=0.0203). Average preoperative internal rotation was T12 (range T6-side) and significantly improved to T7 (range T1-T12) postoperatively (P<0.0001). Preoperative SF36 scores averaged 39 for the physical component score (PCS, range 24.1-70.0) and significantly improved to 49 (range 26.6-59.2) postoperatively (P=0.0013). The preoperative mental component scores (MCS) improved from 51 (range 31.7-66.5) to 55 postoperatively (range 33.9-62.9), however, this was not significant (P=0.1018). ASES scores improved significantly from 37 preoperatively (range 6.7-61.7) to 95 (range 20-100) postoperatively (P<0.0001).
Discussion
Successful arthroscopic rotator cuff repairs rely on the restoration of the anatomic rotator cuff footprint and the recreation of balanced force couples.1 Multiple arthroscopic techniques have been described. The GPS technique affords direct percutaneous access to the rotator cuff tear from any angle or location.1,9 This allows for flexibility in the placement of the medial row sutures through the tendon edge and is a potential advantage over larger, longer tissue penetrating devices that pass through a cannula. Furthermore, the increased size of the tissue bite that can be obtained over other suture passing devices may improve the footprint area and potential for tendon healing. We present our outcomes with 22 patients with this technique for arthroscopic rotator cuff repair, and results were comparable to other techniques in the literature.17,18 We believe that this is a useful technique, which allows a surgeon to have more flexibility with the placement of their repair.
The size of the tissue bite available with common suture passing devices is limited by the jaw length of the devise. Curtis et al.19 demonstrated that the size of the footprint area for the supraspinatus and infraspinatus where the tendon may be repaired has an average medial-to-lateral length of the footprint of 29 mm and 23 mm, respectively. However, other studies have found smaller footprint measurements.20,21 Two common suture passers on the market the Flexible Suture Passer (Mitek, Raynham, MA, USA) with a 4.5mm tip and 18-mm jaw length and the Scorpion Suture Passer (Arthrex, Naples, FL, USA), which is available with a 16-mm or an extended 20-mm jaw length.22 This limits the amount of tissue remaining laterally to the tissue bite to lay down to the footprint. We postulate that the increased bite size obtained by percutaneous shuttling (GPS) will improve this bite size and consequently overall footprint area. While these biomechanical studies are being performed in our laboratory, the present study reports the clinical outcomes of this technique. A recent study by Rousseau et al.23 demonstrated an 88% satisfaction rate with a similar technique using the Banana Lasso. Our outcomes along with this recent study demonstrate this technique as a viable repair option for rotator cuff repairs.
Some of the percutaneous entry portals used in this technique may carry the risk of neurovascular injury, like the placement of arthroscopic cannula. Fortunately, neurovascular injury during arthroscopic shoulder surgery is a rare and unexpected complication of portal placement. Nerve injuries have been reported in 1-2% of patients undergoing arthroscopic rotator cuff repair.24 However, due to the smaller diameter of the percutaneous cannula that is used in this technique, we expect that this potential risk of neurologic injury may be reduced. Furthermore, as long as the percutaneous passing device is inserted under direct visualization, the risk of direct injury to the suprascapular nerve and artery is low.9 There were no injuries to neurovascular structures in this study, and the senior author has not experienced any known neurovascular injuries in ten years of using this technique.
This technique has been performed for ten years, and these results are representative of this larger population. While tendon healing using ultrasound or magnetic resonance imaging scans was not assessed as part of this study, we believe that the rates of healing are comparable to those seen in other series based on the improvements in clinical outcome scores. Additional studies are being performed to assess and validate results with respect to tendon healing.
Conclusions
The global percutaneous shuttling technique for rotator cuff repair is a minimally invasive technique that may offer some advantages over other established arthroscopic techniques. The ability to access the rotator cuff from all angles through small percutaneous punctures may reduce the number of cannulas needed and may allow for improved tissue access. Furthermore, the larger portion of rotator cuff tissue captured by this method may improve the quantity of tissue that may be repaired to the footprint, improving tendon healing. This technique has been the preferred method of repair in the authors practice for ten years. In the present series of patients who had arthroscopic GPS rotator cuff repair, significant improvements were seen in outcome scores comparable to that of other techniques. While further studies are performed to assess footprint size and rates of healing with this technique, these outcomes support the use of the GPS technique for arthroscopic rotator cuff repair.
Acknowledgements
The authors would like to thank Duong Nguyen MD FRCSC, Lan Chen MD, Matthew Kippe MD for their contributions.
References
- 1.Burkhart SS, Lo IK. Arthroscopic rotator cuff repair. J Am Acad Orthop Surg. 2006;14:333-46 [DOI] [PubMed] [Google Scholar]
- 2.Yamaguchi K, Levine WN, Marra G, et al. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 2003;52:81-92 [PubMed] [Google Scholar]
- 3.Thal R, Jennings WB, Heusch WL. Arthroscopic rotator cuff repair using the suture loop shuttle technique. Arthroscopy. 2007;23:561-4 [DOI] [PubMed] [Google Scholar]
- 4.Clark AM, Millet PJ. Minimally invasive shoulder and elbow surgery. 1st ed New York City:Informa Healthcare USA, Inc.; 2007 [Google Scholar]
- 5.Woolf SK, Guttmann D, Karch MM, et al. The superior-medial shoulder arthroscopy portal is safe. Arthroscopy. 2007;23:247-50 [DOI] [PubMed] [Google Scholar]
- 6.Nord KD, Mauck BM. The new subclavian portal and modified Neviaser portal for arthroscopic rotator cuff repair. Arthroscopy. 2003;19:1030-4 [DOI] [PubMed] [Google Scholar]
- 7.Wolff AB, Magit DP, Miller SR, et al. Arthroscopic fixation of bursal-sided rotator cuff tears. Arthroscopy. 2006;22:1247. [DOI] [PubMed] [Google Scholar]
- 8.Morrow DA, Braunwald E, Bonaca MP, et al. Vorapaxar in the secondary prevention of atherothrombotic events. N Engl J Med. 2012;366:1404-13 [DOI] [PubMed] [Google Scholar]
- 9.Davidson PA, Rivenburgh DW. The 7-o’clock posteroinferior portal for shoulder arthroscopy. Am J Sports Med. 2002;30:693-6 [DOI] [PubMed] [Google Scholar]
- 10.Difelice GS, Williams RJ, 3rd, Cohen MS, Warren RF. The accessory posterior portal for shoulder arthroscopy: description of technique and cadaveric study. Arthroscopy. 2001;17:888-91 [DOI] [PubMed] [Google Scholar]
- 11.Lo IK, Lind CC, Burkhart SS. Glenohumeral arthroscopy portals established using an outside-in technique: neurovascular anatomy at risk. Arthroscopy. 2004;20:596-602 [DOI] [PubMed] [Google Scholar]
- 12.Glenn RE, Jr., McCarty LP, Cole BJ. The accessory posteromedial portal revisited: utility for arthroscopic rotator cuff repair. Arthroscopy. 2006;22:1133-5 [DOI] [PubMed] [Google Scholar]
- 13.Bigliani LU, Dalsey RM, McCann PD, April EW. An anatomical study of the suprascapular nerve. Arthroscopy. 1990;6:301-5 [DOI] [PubMed] [Google Scholar]
- 14.Shishido H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: an anatomic study. J Shoulder Elbow Surg. 2001;10:372-6 [DOI] [PubMed] [Google Scholar]
- 15.Vasseur PB, Pool RR, Klein K. Effects of tendon transfer on the canine scapulohumeral joint. Am J Vet Res. 1983;44:811-5 [PubMed] [Google Scholar]
- 16.Marsault E, Hoveyda HR, Gagnon R, et al. Efficient parallel synthesis of macrocyclic peptidomimetics. Bioorg Med Chem Lett. 2008;18:4731-5 [DOI] [PubMed] [Google Scholar]
- 17.Youm T, Murray DH, Kubiak EN, et al. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg. 2005;14:455-9 [DOI] [PubMed] [Google Scholar]
- 18.Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307-16 [DOI] [PubMed] [Google Scholar]
- 19.Curtis AS, Burbank KM, Tierney JJ, et al. The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy. 2006;22:609. [DOI] [PubMed] [Google Scholar]
- 20.Dugas JR, Campbell DA, Warren RF, et al. Anatomy and dimensions of rotator cuff insertions. J Shoulder Elbow Surg. 2002;11:498-503 [DOI] [PubMed] [Google Scholar]
- 21.Mochizuki T, Sugaya H, Uomizu M, et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. 2008;90:962-9 [DOI] [PubMed] [Google Scholar]
- 22.Yanke A, Provencher MT, Cole BJ. Arthroscopic double-row and transosseous-equivalent rotator cuff repair. Am J Orthop (Belle Mead NJ). 2007;36:294-7 [PubMed] [Google Scholar]
- 23.Rousseau T, Roussignol X, Bertiaux S, et al. Arthroscopic repair of large and massive rotator cuff tears using the side-to-side suture technique. Mid-term clinical and anatomic evaluation. Orthop Traumatol Surg Res. 2012;98:S1-8 [DOI] [PubMed] [Google Scholar]
- 24.Boardman ND, 3rd, Cofield RH. Neurologic complications of shoulder surgery. Clin Orthop Relat Res 1999:44-53 [PubMed] [Google Scholar]


