Abstract
Pain is a common symptom in orthopedic patients, but is managed sub-optimally, partly due to scarce opioid use in severe cases. The aim of the Orthopedic Instant Pain Survey (POIS) was to evaluate changes in pain management in Italian orthopedic practice 2 years after a legislative change (Law 38/2010) simplifying opioid access for pain control. A web-based survey on the knowledge of this law and trends observed in clinical practice for severe pain treatment was administered to 143 Italian orthopedic specialists. In total, 101 (70%) respondents showed a high level of knowledge. Nevertheless, 54.5% stated that they do not use opioids for severe osteo-articular pain management. Main barriers to opioid use are fear of adverse events (61.4%), especially nausea/vomiting and constipation, and patient resistance (29.7%). A modest knowledge of pain classification was also demonstrated. Opioid use remains very limited in Italian orthopedic practice. Physicians’ fear of side effects showed poor knowledge of strategies for effective management of opioid-related adverse events, such as combined oral prolonged-release oxycodone/naloxone. Continuing educational programs could improve delivery of evidence-based pain management.
Key words: chronic pain, opioid therapy, orthopedic surgery
Introduction
Chronic pain is a leading cause of disability in adults with a prevalence of 12-30% a median duration of 7 years, nearly half of patients reported to have constant pain, with 66% reporting moderate pain and 34% severe pain.1 Despite availability of effective treatments, nearly 40% of patients report inadequate pain control,1 leading to physiological, psychological and social consequences,2 productivity loss and increased healthcare costs.3
According to the World Health Organization (WHO), correct use of pain management guidelines, especially regarding opioid use, may reduce the incidence of chronic pain, with morphine use regarded an essential indicator of pain control effectiveness.4 Studies by the International Narcotics Control Board (INCB), showed that global opioid consumption was often lower than the levels required.5 Due to growing awareness of the therapeutic value of morphine, substantial increases in therapeutic opioid use have been achieved, albeit only in a few countries. Use in Australia, Canada, New Zealand, USA and several European countries (Austria, Denmark, Portugal) in 2009 accounted for 90% of the global consumption of morphine, fentanyl and oxycodone.6 In other regions, opioid use remained stable or even decreased, showing that most patients with chronic pain may not be getting sufficient pain control, with up to 80% of the world’s population lacking access to basic pain relief.7
In Italy, data show a marked increase in opioid use in recent years, although remaining very low.8 Italian Law 38/2010 represented a break point in chronic pain management, by overcoming the substantial ambiguity in the prescription of strong opioids to relieve pain held by the Italian legislature, and introducing an obligation to report the level of pain and the drugs and dosages used in medical records.9
Pain is common in orthopedic patients – particularly relevant in the elderly population – leading to major surgery such as hip replacement in many patients.10 Preoperative analgesic treatment has been associated with greater mobilization and rehabilitation, improved motor function and social interaction, whereas high pain levels during physical therapy were significantly associated with prolonged hospital stay, more missed rehabilitation sessions, delay in walking and increased postoperative complications.11 Appropriate prescribing for chronic pain by Italian orthopedic specialists is important not only for clinical outcomes but also for economic implications; hence, the POIS (Orthopedic Instant Pain Survey) project was promoted by the Italian Society of Orthopedics and Traumatology (SIOT) and endorsed by the National Commission of the Ministry of Health for the implementation of pain management, with aim of assessing pain management clinical practice among Italian orthopedic specialists, particularly opioid use, more than 2 years since the introduction of Law 38. To our knowledge, this is the first such analysis performed in Italy in the orthopedic setting.
Materials and Methods
An instant Survey (IS) with a multiple choice questionnaire was used for this study. The survey was completed online using a dedicated platform, with password-protected access. For the purpose of the project, the following topics were addressed: i) knowledge of Law 38/2010 on the treatment of pain; ii) knowledge regarding the categorization of pain severity encoded by the Numeric Rating Scale (NSR);12 iii) real trends of severe pain treatment in Orthopedic Units; iv) rationale for the choice of drug treatment; v) interest from orthopedic specialists in improving their knowledge about pain management.
The eligible recipients were Heads of Orthopedics and Traumatology units or, in their absence, the department coordinators. Based on a Ministry of Health database, all public and private hospitals with a department of Orthopedics and Traumatology were considered eligible to participate in the survey. Centre selection took into account the following factors: number of beds available (min 15) and geographical location (north, center, south and islands). Regarding the geographical location, the country has been divided into three macro-areas: north, central, south and islands. A comparable number of centers were assigned to each area. In order to optimize the operational management in each macro-area, a local manager was identified to help promote the project and involve the centers. Considering a response rate of 50%, an alpha error of 5% and beta error of 20%, a sample size of 143 centers was chosen.
Results
Of the 143 selected centers, 101 (70%) participated in the survey. The geographical distribution of the sample shows a predominance of the North of the country (49.5%) and a modest participation of the Centre (19.8%). Almost all respondents were male (93%) and mainly over 40 years (84.2%). The degree of knowledge of Law 38/2010 was elevated and quite detailed, demonstrating the high level of interest and attention raised by the topic of pain management. Almost all of the respondents knew of the obligation to report pain detection in medical records (89.1%), rescue drugs used (76%) and, especially, the simplification in opioid prescription required by law (97%).
Despite these encouraging data from the theoretical point of view, 54.5% reported not to use opioids for severe osteo-articular pain management, prescribing more frequently non-steroidal anti-inflammatory drugs (NSAIDs) (25.7%), cyclooxygenase-2 (COX-2) inhibitors (10%) or paracetamol (18.8%) (Figure 1). While the main reason for not prescribing NSAIDs in patients with severe pain was the occurrence of gastrointestinal adverse events (51.5%), the main barriers to opioid use in severe pain were mainly represented by the fear of adverse events (61.4%) and the resistance posed by the patient (29.7%) (Figure 2), highlighting the fact that education and culture regarding opioids are still important issues. When physicians prescribe opioids, the adverse events they fear most are nausea/vomiting (48.5%) and opioid-induced constipation (OIC) (27.7%) (Figure 3), thus showing a poor knowledge of the available therapeutic strategies for effective management of opioid-related adverse events.
Figure 1.
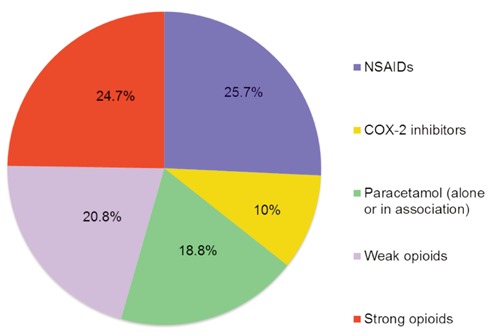
Most frequently prescribed drugs for severe osteo-articular pain management.
Figure 2.
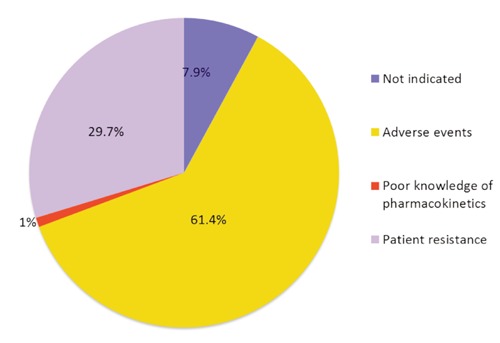
Main reasons discouraging consulting physicians to prescribe opioids for the treatment of severe osteo-articular pain.
Figure 3.
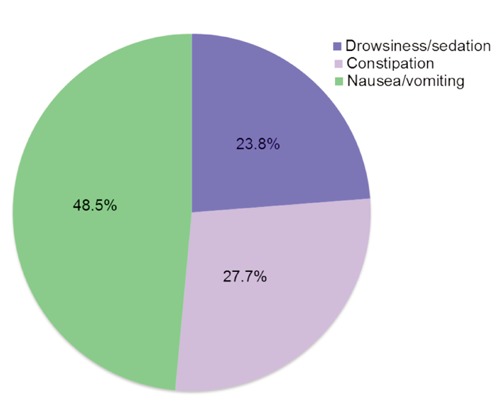
Adverse events most feared by consulting physicians when using opioids to treat pain.
Regarding pain assessment, it is important to note that a significant percentage of participating physicians (58%) had only a modest knowledge of pain categorization according to the NRS scale (Figure 4), showing a gap in pain assessment. However, the majority of respondents (76.2%) declared an interest in increasing their knowledge in the field of pain management through specific training.
Figure 4.
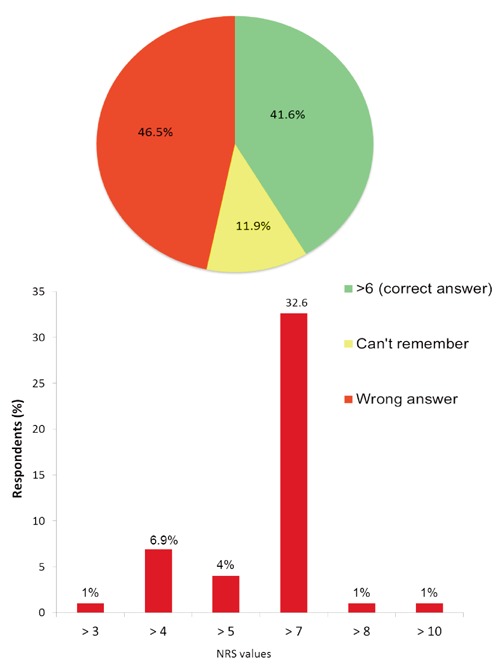
Knowledge of the Numerical Rating Scale (NRS) for pain categorization. Participants were asked to remember the cutoff value for severe pain: A) shows the answers and B) shows frequencies for each cut-off value reported by 46.5% of respondents who missed the correct answer.
Discussion
Italy was the first country in the world to approve a law (38/2010) guaranteeing a citizen’s right to pain management therapy. The aim of this survey was to evaluate changes in pain management in orthopedic clinical practice 2 years since the law was issued. Law 38/2010 has brought innovative changes to prescription of pain medications and pain monitoring, and has actually stimulated opioid prescription in Italy. According to the latest data published by the Italian Medicines Agency (AIFA), the use of natural opium alkaloids (morphine, hydromorphone, oxycodone and codeine) and other opioids (tramadol and tapentadol) in 2012 was significantly higher than in 2011, with an increase in defined daily dose (DDD) per 1000 inhabitants (15.1% and 7.9%, respectively).13 However, Italy remains far below the European Union average opioid use.8
According to the latest INCB data, the average consumption of narcotic drugs in 2008-2010 in Italy was among the lowest (5576 DDD per 1,000,000 inhabitants), slightly higher than that seen in Portugal (5152) and Greece (4783); Spain and Ireland are almost at the average consumption (12,429 and 10,966 DDD, respectively), while Germany, Switzerland and Denmark are above the average of all European countries, with a consumption of narcotic drugs of 21,494, 20,304 and 18,191 DDD per 1,000,000 inhabitants, respectively.8
Thus, there is still considerable room for improvement in pain management in the Italian orthopedic setting. The barriers limiting adequate pain treatment are not connected to regulatory or government restrictions; on the contrary, they are more closely linked with mind-set, education and level of knowledge of pain management. The present study show that the very first barrier to appropriate treatment is at the diagnostic stage. A proper evaluation of pain is crucial, to guide decision making regarding the need for analgesia and for selection of the optimal choice for each individual patient among the various pain relievers available. This is why pain evaluation should be as comprehensive as possible and should take into account etio-pathogenesis, origin, intensity, and duration; in addition to including a valid measure of pain intensity, the impact of pain on the patient’s quality of life should also be evaluated. Even if the experience of pain is quite subjective, the NRS is one of the specific tools currently used to assess and re-assess pain, both before and after treatment initiation, in order to monitor its objective effectiveness. In a recent qualitative study of patients with chronic non-cancer pain, the absence of objective measures of pain was one of the main barriers cited by physicians involved in the interviews.14
The lack of adequate knowledge on assessing pain intensity among Italian orthopedists may be one of the factors contributing to the general trend of low prescriptive appropriateness observed in our survey, documenting that NSAIDs are still the most frequent choice for the treatment of severe osteo-articular pain. While paracetamol has a limited role in severe chronic pain, NSAID use in non-cancer pain management (such as rheumatic and orthopedic conditions) is currently under reassessment due to the accumulating evidence of toxicity both with non-selective NSAIDs and selective COX-2 inhibitors, especially in subgroups of patients at higher risk of developing adverse events, such as the elderly. The risk of upper gastrointestinal complications is increased nearly 4-fold with non-selective NSAIDs, while the risk of peptic ulcer is increased 5-fold.15 Age =65 years is a main risk factor for NSAID-related bleeding and other serious complications, including cardiovascular and renal adverse events.16 The onset of renal failure as a result of NSAID therapy is a particular concern, considering the reduction in glomerular filtration rate and renal blood flow in patients of advanced age, and a creatinine clearance lower than 60 mL/min would contraindicate NSAID use in the postoperative period.17 The number of NSAID-related hospitalizations and deaths per year in the USA is about 100,000 and 7-10,000, respectively; the cost of managing NSAID-related gastrointestinal complications is 4 million US dollars per year.18 Furthermore, there is increasing evidence that all NSAIDs, not only COX-2 inhibitors, are associated with an increased risk of cardiovascular events and should, therefore, be used with caution.19 In patients with prior myocardial infarction, even short-term treatment with most NSAIDs has been shown to be associated with an increased risk of death and recurrence, and neither short- nor long-term NSAID treatment is advised in this population.19 If osteo-articular pain is not relieved by paracetamol or other non-opioid analgesics, weak and strong opioids should be considered as treatment options.20 The WHO three-step pain ladder (paracetamol, NSAIDs, mild and strong opioids) originally proposed for cancer pain treatment,4 extends the use of opioids to non-cancer pain management. With appropriate use, opioids can contribute to optimize non-cancer pain management in the context of an individualized multimodal treatment plan in selected patients:21 including opioids as a treatment option to gain pain control in musculoskeletal conditions and in neuropathic syndromes can be an optimal approach in selected older patients.21 Of major relevance, non-cancer pain syndromes with rheumatic and/or orthopedic conditions account for nearly 80% of chronic non-cancer pain in Europe.1
Recently, opioids have been investigated not only for their central analgesic capacity, but also for their effect on chronic peripheral inflammation. Inflammation is associated with an up-regulation of µ-opioid receptors in the peripheral terminal of the sensitive neuron, and polymorphonuclear cells release endogenous opioid peptides to lower the terminal nerves excitability.22 These observations have increased the interest in improving analgesia through the use of opioid analgesics in the orthopedic setting, where pain and inflammation often coexist. However, resistance to the systematic use of opioids remains, especially in patients with non-cancer pain,14 as also demonstrated in our survey reflecting Italian clinical practice in orthopedic care. The major reasons for not prescribing opioids were concerns related to the development of addiction/misuse and adverse effects, although such concerns have no scientific justification. Mechanisms of tolerance and dependence are different and unrelated: the signs and symptoms of physical dependence are not an indicator for the presence of an addiction problem.23 The risk of addiction to opioids in a framework of chronic severe pain is exceedingly rare in patients with no history of addictive disorders,24 since mechanisms of positive reinforcement promoting gratification – leading in the long run to the development of compulsive behavior – are not active in patients with chronic pain.25
Successful management of pain with opioids requires that their benefits outweigh the impact of treatment-related side effects, in particular nausea/vomiting and constipation. Several strategies have been developed in the past to promote effective management of opioid-induced adverse events, including dose reduction, opioid rotation and a change in the route of administration, with limited effectiveness.26 Our survey clearly shows that there is still a lack of knowledge among clinicians of the newer available therapeutic options that reduce the burden of adverse events. In particular, targeting peripheral receptors whilst sparing central analgesic function through combining an opioid receptor antagonist (i.e., naloxone) with an agonist such oxycodone has emerged as a promising approach. Naloxone, following oral administration, acts almost exclusively on opioid receptors in the gastrointestinal tract and strongly counteracts OIC; due to the extensive first-pass hepatic metabolism, its systemic bioavailability is, however, very low (<3%), an so it does not affect the central analgesic activity of oxycodone. The new formulation of combined oral prolonged-release (PR) oxycodone/naloxone has demonstrated, both in randomized controlled trials and in post-marketing studies, full analgesic efficacy together with reduced OIC incidence, and a consequent decrease in the use of rescue medications and laxatives.27 PR oxycodone/naloxone has potential advantages particularly for the elderly, and it is estimated to be a cost-effective analgesic option.28
Patients often can raise barriers to effective pain medication, as confirmed in our survey where patients’ concerns were the second main reason for not prescribing opioids. Cultural, social and emotional barriers have been investigated as possible factors preventing optimal pain outcomes.29 In particular, opioid use is related to the greatest cognitive concerns raised by patients, with reference to fears of addiction and adverse events. Thus, it is crucial that both parties are involved in educational programs to ensure correct information and perception of opioid drugs. Patients’ as well as nurses’ fear of opioids reduces adherence to treatment, despite proper prescription of these drugs.30 With a 70% response rate, our survey confirmed that more than three-quarters of orthopedic respondents are interested in updating pain management. Such data indicate the presence of a very fertile soil for the development of continuing education programs, the sole tools to improve knowledge of the pathophysiology of chronic pain and to reduce the high rate of treatment failure. In the orthopedic setting, our survey indicates a lack of knowledge of the new treatment options available today such as the co-administration of an opioid agonist with a µ-opioid receptor antagonist with negligible systemic availability, such as oral naloxone, to provide effective simplify and cost-effective analgesia.27,28
Conclusions
The reasons given for not using opioid as pain treatment (fear of gastrointestinal side effects, including constipation) indicate a lack of knowledge of the various treatment options available today. The high rate of survey response and the high level of interest reported by orthopedists in the topic of pain management make it possible to envisage a landscape where real clinical practice is tailored on individual patient need. However, continuing and comprehensive educational activities appear to be crucial to guarantee evidence-based pain management together with a sound opioid culture.
Acknowledgements
Names of all members of the collaborative group are shown in the Appendix.
Funding Statement
Funding: none.
References
- 1.Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287-333 [DOI] [PubMed] [Google Scholar]
- 2.Brennan F, Carr DB, Cousins M. Pain management: a fundamental human right. Anesth Analg. 2007;105:205-21 [DOI] [PubMed] [Google Scholar]
- 3.Sarzi-Puttini P, Vellucci R, Zuccaro SM, et al. The appropriate treatment of chronic pain. Clin Drug Investig. 2012;32:21-33 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organisation (WHO). WHO’s pain ladder 2011. Available from: http://www.who.int/cancer/palliative/painladder/en/
- 5.International Narcotics Control Board (INCB). Availability of internationally controlled drugs: ensuring adequate access for medical and scientific purposes. 2011. Available from: http://www.incb.org/documents/Publications/AnnualReports/AR2010/SupplementAR10_availability_English.pdf
- 6.Manchikanti L, Helm S, 2nd, Fellows B, et al. Opioid epidemic in the United States. Pain Physician. 2012;15:ES9-38 [PubMed] [Google Scholar]
- 7.Scholten W, Nygren-Krug H, Zucker HA. The World Health Organization paves the way for action to free people from the shackles of pain. Anesth Analg. 2007;105:1-4 [DOI] [PubMed] [Google Scholar]
- 8.International Narcotics Control Board (INCB). Narcotic Drugs, Technical Report. 2012. Available from: http://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/2012/NDR_2012_Part4_Tables_EFS.pdf
- 9.Italian Parliament. Provisions to ensure access to palliative care and pain therapy [Italian]. 2010. Available from: http://www.parlamento.it/parlam/leggi/10038l.htm
- 10.Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012;380:1768-77 [DOI] [PubMed] [Google Scholar]
- 11.Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am. 2011;93:1075-84 [DOI] [PubMed] [Google Scholar]
- 12.Farrar JT, Young JP, Jr., LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001; 94:149-58 [DOI] [PubMed] [Google Scholar]
- 13.Italian Medicines Agency (AIFA). Osservatorio nazionale sull’impiego dei medicinali. L’uso dei farmaci in Italia: rapporto nazionale gennaio-settembre. 2012. Available from: http://www.agenziafarmaco.gov.it/sites/default/files/rapporto_osmed2012.pdf
- 14.Barry DT, Irwin KS, Jones ES, et al. Opioids, chronic pain, and addiction in primary care. J Pain. 2010;11:1442-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanas A. A review of the gastrointestinal safety data-a gastroenterologist’s perspective. Rheumatology (Oxford). 2010;49:ii3-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Podichetty VK, Mazanec DJ, Biscup RS. Chronic non-malignant musculoskeletal pain in older adults: clinical issues and opioid intervention. Postgrad Med J. 2003;79:627-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aveline C, Leroux A, Vautier P, et al. [Risk factors for renal dysfunction after total hip arthroplasty]. Ann Fr Anesth Reanim. 2009;28:728-34 [Article in French] [DOI] [PubMed] [Google Scholar]
- 18.Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152:101-13 [DOI] [PubMed] [Google Scholar]
- 19.Schjerning Olsen AM, Fosbol EL, Lindhardsen J, et al. Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation. 2011;123:2226-35 [DOI] [PubMed] [Google Scholar]
- 20.Institute for Clinical Systems Improvement (ICSI). Health care guideline: assessment and management of chronic pain (fourth edition). 2009. Available from: www.icsi.org
- 21.Cherubino P, Sarzi-Puttini P, Zuccaro SM, Labianca R. The management of chronic pain in important patient subgroups. Clin Drug Investig. 2012;32:35-44 [DOI] [PubMed] [Google Scholar]
- 22.Sehgal N, Smith HS, Manchikanti L. Peripherally acting opioids and clinical implications for pain control. Pain Physician. 2011;14:249-58 [PubMed] [Google Scholar]
- 23.Raith K, Hochhaus G. Drugs used in the treatment of opioid tolerance and physical dependence: a review. Int J Clin Pharmacol Ther. 2004;42:191-203 [DOI] [PubMed] [Google Scholar]
- 24.Kirsh KL, Fishman SM. Multimodal approaches to optimize outcomes of chronic opioid therapy in the management of chronic pain. Pain Med. 2011;12:S1-11 [DOI] [PubMed] [Google Scholar]
- 25.Ballantyne JC, LaForge KS. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;129:235-55 [DOI] [PubMed] [Google Scholar]
- 26.Cherny N, Ripamonti C, Pereira J, et al. Strategies to manage the adverse effects of oral morphine: an evidence-based report. J Clin Oncol. 2001;19:2542-54 [DOI] [PubMed] [Google Scholar]
- 27.Gatti A, Casali M, Lazzari M, et al. Prolonged-release oxycodone/naloxone in nonmalignant pain: single-center study in patients with constipation. Adv Ther. 2013;30:41-59 [DOI] [PubMed] [Google Scholar]
- 28.Mercadante S, Giarratano A. Combined oral prolonged-release oxycodone and naloxone in chronic pain management. Expert Opin Investig Drugs. 2013;22:161-6 [DOI] [PubMed] [Google Scholar]
- 29.Jacobsen R, Moldrup C, Christrup L, et al. Psychological and behavioural predictors of pain management outcomes in patients with cancer. Scand J Caring Sci. 2010;24:781-90 [DOI] [PubMed] [Google Scholar]
- 30.Bell L, Duffy A. Pain assessment and management in surgical nursing: a literature review. Br J Nurs. 2009;18:153-6 [DOI] [PubMed] [Google Scholar]


