Abstract
Both bone forearm fractures are common orthopedic injuries. Optimal treatment is dictated not only by fracture characteristics but also patient age. In the pediatric population, acceptable alignment can tolerate greater fracture displacement due to the bone’s ability to remodel with remaining growth. Generally, these fractures can be successfully managed with closed reduction and casting, however operative fixation may also be required. The optimal method of fixation has not been clearly established. Currently, the most common operative interventions are open reduction with plate fixation versus closed or open reduction with intramedullary fixation. Plating has advantages of being more familiar to many surgeons, being theoretically superior in the ability to restore radial bow, and providing the possibility of hardware retention. Recently, intramedullary nailing has been gaining popularity due to decreased soft tissue dissection; however, a second operation is needed for hardware removal generally 6 months after the index procedure. Current literature has not established the superiority of one surgical method over the other. The goal of this manuscript is to review the current literature on the treatment of pediatric forearm fractures and provide clinical recommendations for optimal treatment, focusing specifically on children ages 3-10 years old.
Key words: pediatric, forearm fractures, both-bone fractures, younger children
Introduction
Pediatric diaphyseal fractures of the radius and ulna, commonly referred to as both bone forearm fractures, are the third most common fracture in the pediatric population and account for 13-40% of all pediatric fractures.1,2 Fracture severity falls along a continuum from plastic deformity to significant displacement. Historically, the majority of these fractures have been treated with non-operative management relying on closed reduction and casting. Recently, however, there has been a trend towards increased surgical management of these fractures in an effort to improve clinical outcomes.3
The management of these fractures depends on the age, type of fracture and fracture displacement. Given a child’s physeal growth potential, varying degrees of angulation can be accepted depending on the age of the child and their ability to remodel. Long arm cast immobilization remains a viable treatment option for many of these fractures that fall within acceptable alignment parameters, and children are generally at low risk for developing significant elbow stiffness following cast immobilization. For fracture patterns, which are unable to be closed reduced to an acceptable position, surgical management is recommended. Surgical treatment options include both rigid plate fixation and elastic intramedullary nails. Elastic intramedullary nails were originally developed in the early 1980s by surgeons in Nancy, France.4,5 Recently there has been an increased interest in determining which method provides superior results, but the optimal treatment remains controversial.6 The goal of this paper is to review the current literature on treatment of pediatric both bone forearm fractures in younger children (ages 3-10), and offer useful treatment algorithms for these injuries. However, many of the studies in the literature on this topic are retrospective in design and are limited in the number of patients they contain.
Epidemiology
Pediatric fractures present significant challenges to the orthopedic community. Epidemiologic studies have shown that 18% of children will experience a fracture by the age of 9, with children between the ages of 5 and 14 having the highest fracture incidence.7 Further analyzed by sex, Lyons et al. extrapolated that 63.7% of boys and 39.1% of girls are expected to have sustained a fractured bone by the time they are 15 years of age when they looked at the rate of fracture in 68,231 children.8 Due to the high incidence of fractures in children, it is important to treat them adequately but also to recognize the potential psychosocial impact a fracture can have on a child, possibly limiting physical activity and affecting their grades in school.7
Forearm fractures comprise 40% or more of pediatric fractures.2 The majority of forearm fractures are located in the distal part of the forearm.8,9 The age distribution of these fractures is bimodal; the peak incidence occurs between ages 10-14, coinciding with the adolescent growth spurt, with a second smaller peak incidence between 5-9 years of age.9,10 The most common mechanism is a fall (83%) while direct trauma is a distant second (10%). The most common location of injury is predictably a playground area.7,10 As expected, significant seasonal variation has been noted, with 34.2% of these injuries happening during the spring season and a decreased incidence occurring in the winter.10
Surprisingly, there is a dichotomous relationship between injury rate and incidence regarding pediatric forearm fractures, as the incidence of these injuries continues to increase,11 while the overall injury rate in the pediatric population is declining.12 Ryan et al. hypothesized that this increase in forearm fractures could be due to lower bone mineralization resulting from physical inactivity, poor nutrition, and vitamin D deficiency.10 With no direct studies to prove it, it has been proposed that the rise in obesity numbers has influenced the increase in pediatric forearm fractures, speculating that obese children have an increased fracture risk, secondary to poor balance and increased force in the fall.
Conservative management
The gold standard for pediatric forearm fractures remains closed reduction and casting.2 Given the excellent remodeling potential with younger patients, certain studies have argued that even with 100% displacement of the radius and ulna closed reduction and casting is an excellent treatment choice for children 9 years old and younger.13,14 However, the exact amount of angulation, displacement, and rotation that is acceptable remains controversial in the literature. It is generally accepted that the closer the fracture is to the distal physis, the greater the potential for remodeling. Consequently more deformity can be accepted in the distal one third of the diaphysis versus the middle and proximal thirds. However, a review of the literature is inconclusive in defining precise guidelines for acceptable deformity (Table 1).15-18
Table 1.
Table of recommended acceptable alignment parameters for both-bone pediatric forearm fracture.
| Source | Age, years | Angulation, degrees | Malrotation, degrees | Bayonette apposition /displacement |
|---|---|---|---|---|
| Price (2010)15 | <8 | <15 MS, DS; <10 PS | <30 | 100% displacement |
| Noonan (1998)16 | <9 | <15 | <45 | <1 cm short |
| Tarmuzi (2009)17 | <10 | <20 | No limits | |
| Qairul (2001)20 | <12 | <20 |
MS, mid-shaft; DS, distal-shaft; PS, proximal-shaft.
Franklin et al. defined successful treatment of pediatric forearm fractures should result in painless and complication-free outcomes with functional pronosupintation.14 It has been shown that 15 to 20 degrees of angulation in middle third forearm fractures can lead to major loss of forearm rotation.19 However, the significance of this range of motion loss as it pertains to clinical outcome remains debatable.
Closed reduction is indicated in patients ages 0 to 8 with fracture angulation of greater than 10 degrees and malrotation greater than 30 degrees.15 In patients with angulation less than 10 degrees and malroation less than 30 degrees, splinting without reduction is acceptable. Functional outcomes are satisfactory for closed management if manipulation can maintain reduction within this range.2,17,20 Tarmuzi et al. concluded that up to 1cm of shortening can be accepted for closed management.17 Failure of closed management is rare, with roughly 90% of injuries being amenable to closed management.2,3,13,14,21 Noonan et al. came to the conclusion that once fractures have healed, residual loss of motion of greater than 60 degrees is considered an indication for corrective osteotomy.16
The method of closed reduction and casting varies between institutions, but is guided by common principles: obtaining relaxation/anesthesia, recreating the initial deformity allowing the fracture to unlock, obtaining length, and reducing angular/rotational deformity followed by careful cast application. In the pediatric population this is commonly done under conscious sedation in the emergency room. Proper molding of the cast is essential to successful management of forearm fractures. General principles include 3 point molding, adequate but not excessive padding, and enough casting material to maintain molding without excessive weight and heat generation. Cast index, defined as the ratio of sagittal to coronal width of the cast, has been shown to be important in predicting successful closed management (Figure 1). Kamat et al. demonstrated that a cast index should be below 0.7 to 0.8, as ratios above this range has been correlated with significant increase in risk of lost reduction.22 Children under the age of 4 should be placed in an above-elbow cast for any forearm fractures as short arm casts may slip.23,24 Post reduction, patients should be followed weekly for the first two to three weeks to ensure reduction is maintained. Holmes et al. found that if loss of reduction occurs, wedging the cast may restore alignment, but re-reduction or operative intervention may be required.24
Figure 1.
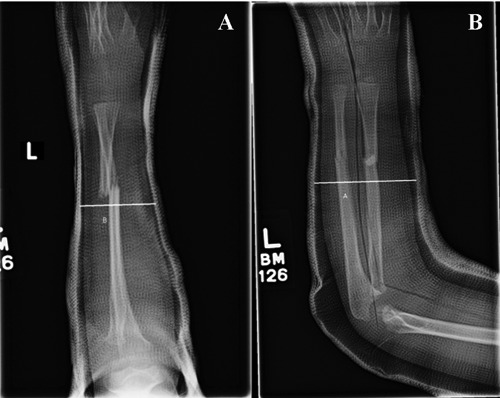
The cast index is sagittal width (B) divided by the coronal width (A). The lines in the figure demonstrate that the measurement is from the inside of the fiberglass.
Greenstick fractures make up a significant subset of pediatric forearm fractures. These injuries involve incomplete disruption of cortical bone continuity at the apex of the fracture with plastic deformity of the opposite cortex. It is widely accepted that these fractures should be managed by closed means. Within closed treatment, there are two approaches to reduction. First is simple correction of the deformity, maintaining the continuity of the surface that has undergone plastic deformity. Second is completion of the fracture through manipulation, with subsequent manipulation and casting; in theory the rupture of the intact periosteum could generate more callous for fracture healing and reduce refracture, while minimizing deformity. A small number of studies have evaluated the treatment of these injuries.25-28
Alpar et al. looked at a series of 80 forearm fractures in which 82.5% of these injuries were greenstick fractures.25 They concluded that greenstick fractures required only simple correction of deformity without fracture completion, followed by six weeks of immobilization.25 They reported no subsequent deformities in this group. A subsequent study by Schmuck et al. evaluated midshaft greenstick fractures in 103 patients.27 They concluded that completion of fractures did not reduce refracture rate, but did result in diminished deformity. A 20% refracture rate was noted in patients who had unicortical delayed union, and the authors emphasized the importance of 6 week follow up radiographs before return to activity.27 Randsborg et al. concluded that while torus fractures do not displace, greenstick fractures of the distal radius are at risk for continued displacement after two weeks and warrant closer follow up.26 Greenstick fractures of the radius often have significant rotational deformities, and generally require rotation of the radial aspect of the forearm in the direction of the deformity for adequate reduction. A method for evaluating the rotational reduction of proximal radial greenstick fractures has been described, and centers on evaluating the proximal and distal segments separately by evaluating their relative rotation based on crossover of the two bones.28 Overall, green-stick fractures require the close attention of a clinician experienced in closed management to obtain optimal outcomes.
Traditionally all open forearm fractures were considered to be operative, however this dogma has been challenged by recent literature. Lobst et al. demonstrated that Type I open fractures that were managed with non-operative management and antibiotics had little difference in infection rate when compared to an operative treatment group (2.5% versus 1.9%).29
The complications associated with cast immobilization include disuse osteopenia, muscle atrophy, skin breakdown, and elbow stiffness.7,9 Loss of reduction is the most common complication in pediatric forearm fractures, with rates between 10 and 60%.7 Refracture is another rare complication that can happen up to 6 months after the initial injury.16 Synostosis may occur after closed management of high-energy fractures and may require resection depending on functional limitations.16 In rare circumstances conservative management results in malreduction that affects activities of daily living.16
In a recent study, Tarmuzi et al. looked at 48 patients between the ages of 4 and 12 years of age with forearm fractures (majority mid-shaft) treated with closed reduction and casting.17 The mean union rate was 4.6 weeks and all but one patient were satisfied with their final result. The authors concluded that when considering children younger than 10 years of age, up to 20 degrees of angulation can be acceptable and managed conservatively.
In one of the largest studies examining pediatric forearm fractures, Jones et al. looked at 730 patients from birth to age 17.2 Fractures were considered for closed reduction if children were 0 to 8 years of age with angulation over 10 degrees. Of these, 22 patients required remanipulation. All of these cases resulted in successful healing of the fractures and did not require any internal fixation. Additionally, final range of motion was within 15 degrees of the contralateral forearm.
Nonoperative management continues to be a very common, safe, and successful treatment option in pediatric forearm fractures. For those fractures that fail or are not amenable to conservative management however, surgical stabilization may need to be considered.
Operative fixation
When acceptable reduction is unable to be attained with closed reduction and casting, operative intervention is recommended. Presently two operative treatment modalities are commonly employed: open compression plating and flexible intramedullary nailing. Each modality has advantages and disadvantages.
Operative fixation with plates
Holmes et al. stated that compression plating maximizes the ability to obtain anatomic reduction and restore normal radial bow.24 Additionally, given the construct fixation strength, plate fixation permits early range of motion. Although exact indications are debatable, it is suggested that plate fixation is indicated in the setting of significant comminution or with late loss of reduction after conservative management, as callous can prevent passage of intramedullary fixation.24 In contrast to adult fixation, smaller plate size and fewer screws can be used in children.24,30 Generally screw diameters are 2.7 mm or 3.5 mm, and 1/3 tubular plates and may be considered adequate.30 Fixation through 4 cortices should be obtained proximal and distal to the fracture site, and the plate should not be wider than the bone.30,31
The question of plate removal versus retention has been debated in the literature. Studies examining retention of implants have reported refracture, bony overgrowth and immunologic reactions to the implants.32 The most common indication for plate removal is pain at the site of hardware, more commonly at the site of ulnar fixation. Significantly, Peterson et al. called for plate removal in those involved in contact sports due to concern for refracture at the area of stress riser generated by the retained plate.32 If plate removal is elected, the literature has shown this practice to be safe, however the evidence is low. Kim et al. reviewed 43 fractures in patients with a mean age of 10.6 years at time of removal. Three refractures occurred in 2 patients, and all were the result of a new trauma. They concluded the implant removal could be done with acceptably low complications rates.33
Implant retention has also been reviewed. A study examining the effects of plate retention in 82 patients between the age of 4 and 13 with 8 year follow up period illustrated peri-implant fracture to be the most common complication (Figure 2).34 Peri-implant fracture was more frequent with dynamic compression plates compared to one-third tubular plates. There was a 7.3% risk of an implant-related fracture in the follow up period, which all occurred within the first 3 years. Overall there was an 85% survivorship of implants, which led the authors to conclude that the decision to retain plate implants versus plate removal is at the discretion of the parents and the surgeon. Vopat et al. published similar data in which the refracture rate was 7.1% in patients with retained plates.35 From their retrospective review, they concluded that retaining plates in pediatric forearm fractures did not increase the refracture rate compared to removal from historical rates in the literature.
Figure 2.
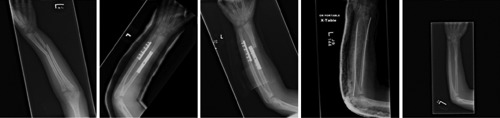
Nine year old boy presented with open fracture after fall from a slide. ORIF was performed at the time of initial debridement. A year and a half later patient fell from a bicycle and fractured around his implants. Revision fixation with nails was performed. Recanullation of the bones was necessary to pass nails through the previous area of plating. Removal of nails was performed at 6 months.
Additional complications of plate fixation include damage to surrounding structures, nonunion/malunion, and synostosis.24 The rate of synostosis has been noted to have an increased incidence if only one incision is used.24 The potential for nerve damage is also present, more commonly secondary to ulnar fixation.36
Operative fixation with flexible nails
With the exception of severe fracture comminution, most both bone forearm fractures that can be treated by plate fixation may also be treated with flexible nails through closed or open reduction techniques. Recently fracture fixation with flexible nails has gained popularity, with proponents arguing that nailing results in decreased surgical dissection and retention of biologic factors at the fracture site.7,37 Both titanium and stainless steel flexible nails are available. In the clinical setting, titanium (Ti 6A114V) is being used more often than stainless steel in most circumstances because of the elastic properties which allow for improved insertion and rotation while still providing adequate fracture stabilization.38
The diameter of available intramedullary implants range from 1.5 to 4 mm. Size selection is dependent on the diameter of the medullary canal.38 A generally accepted method is to use a nail that is 40% of the medullary diameter. Length is determined by placing it over the affected forearm and measuring against bone length under fluoroscopic guidance. Nails should be pre-bent, with maximum curvature at the site of fracture to ensure restoration of the interosseous space.38 An example of this technique is seen in Figure 3.
Figure 3.

Six year old male who suffered initial fracture after a fall. Initial closed management was successful. Six months after initial injury he fell from a motor scooter and refractured. Intramedullary fixation was elected. Removal at 6 months post operatively is the routine at our institution.
Kang et al. evaluated 90 children treated with intramedullary nailing and reported good results and patient outcomes.39 The average patient age was 8.4 years with a follow up of 6.6 months. Eighty-six percent (77/90) of the patients had both-bone fractures and 9% (8/90) had open fractures. Ten were treated with flexible nailing after failed closed management; the remaining fractures were irreducible or considered unstable. Forty-four percent of the fractures required limited open reduction to allow passage of the nail and to obtain satisfactory alignment. Cast immobilization varied with 82.2% (74/90) immobilized with above-elbow cast and 14.4% (13/90) treated with no cast. All but one ulnar fracture healed by 3 months. Eighty-four percent (76/90) of their patients had outcomes that were excellent (equal motion between sides) or good outcomes (less than 20 degree loss of motion versus uninjured arm). Based on their findings the authors recommended the use of intramedullary nailing for treatment of forearm fractures not amenable to closed reduction or after failed closed reduction.
Similar to plate fixation, authors have sought to determine if dual nail fixation is truly necessary. Some advocate for dual fixation, as ulnar fixation alone may lead to an unacceptable rate of loss of reduction of the unfixed radius. In contrast there has been a recent study viewing the outcomes of 38 patients between 4-14 years of age (mean age 9 years) that received single bone IM fixation of the ulna for both-bone forearm fractures.40 There was 2 complications one of the patients developed superficial pin tract infection and one other patient developed a refracture through both the radus and ulna 242 days after the initial injury. All patients progressed to union at an average of 60 days. Only 5% had what was felt to be significant limitation of pronosupination, lacking 20 degrees or more of full supination. The authors concluded that single bone fixation has a favorable risk benefit ratio.
Duration and method of post-operative immobilization amongst studies is variable, ranging from no immobilization to six weeks of long arm casting.19,21,38 Nails are routinely removed at 6 months post-operatively, requiring a second operative procedure.
Complications have been reported to be associated with intramedullary flexible nailing of forearm fractures. In Kang et al.’s study, the overall complication rate was 14% (13/90), and included one compartment syndrome.39 Martus et al. described similar complication rates for intramedullary nailing reporting a complication rate of 12.9% in children less than 10 years old.41
Complications secondary to intramedullary fixation include infection at the site of implantation, skin irritation, refracture after removal, implant failure, nerve/tendon injury, decreased range of motion, and compartment syndrome.3,13,38 The cause of these complications is difficult to determine, is it due to the surgeon’s inexperience with the technique or the surgery itself, since most of the studies that include children less than 10 years old is limited by the number of patients. Some consider the second procedure to remove the implants to be a disadvantage of IM nailing.19
In a recent series of 285 factures, compartment syndrome incidence was evaluated in pediatric forearm fractures treated with intramedullary nails.42 Of the 205 patients who were treated with closed reduction and casting, none developed compartment syndrome. Eighty injuries were managed with intramedullary fixation, including 50 open fractures, and 7.5% (6/80) of these operatively treated patients developed compartment syndrome (3/30 closed fractures, and 3/50 open fractures). All cases of compartment syndrome developed within 24 hours of initial fixation and were treated with fasciotomy and delayed wound closure, and no patient developed permanent neurologic injury after treatment. Other studies have reported a 0-1% incidence of compartment syndrome, with notably shorter tourniquet times.18,39 It appears that longer tourniquet time can be correlated with risk for compartment syndrome.
Despite the complication risk inherently associated with operative insertion of flexible nails, intramedullary nailing can be an effective strategy for treatment of forearm fractures with acceptable complication rates. Careful attention to the length tourniquet time is warranted.
Comparison of outcomes between compression plating and intramedullary nails
A review of the literature illustrates fairly similar outcomes and complication rates between plate fixation and flexible nailing.24 There are, however, differences reported that are unique to each treatment. A retrospective study of 50 patients with a mean age of 9.6 years compared complications of intramedullary nailing versus plate fixation.21 In the intramedullary nailing group, there were 9 complications, and the complication rate was 42%. Complications included: four cases of symptomatic hardware, three delayed unions (one requiring ORIF), one transient sensory neuropraxia, and one ulnar bursitis. In the plate fixation group there were 5 complications comprising a 33% complication rate: two carpal tunnel syndromes requiring release, one dorsal compartment syndrome, one loosening of hardware, and one transient motor neuropraxia. They found that the complication rate was significantly different between the closed and operative groups.20 These complication rates are higher than reported in other studies.
Another recent study comparing the operative treatment of both-bone mid-shaft forearm fractures described minimal differences between plating and intramedullary fixation among 34 children.43 Plating did result in a trend toward more anatomic restoration of radial bow, however the difference was not significant. In terms of complications, in the nail group, one radioulnar synostosis occurred, there was one infection that progressed to osteomyelitis that was successfully treated with antibiotics, and there was loss of rotational range of motion in 6 patients. In the plate group there was one transient ulnar nerve palsy, one case of painful hardware requiring removal, and 5 patients with decreased rotational motion. The authors concluded that functional outcomes are likely to be equivalent independent of method of fixation.
Conclusions
Conservative management is still the first line of treatment for pediatric forearm fractures especially in children less than 10 years old. Presently if operative intervention is required, both plate fixation and flexible nailing are acceptable treatment options. However, based on analysis of the available literature, it is unclear whether flexible nails or open reduction and internal fixation with plates should be recommended as a superior technique. Adequate understanding of the subtleties of either technique is necessary to ensure optimal outcomes, including the limitations of each technique and possible complications. In general, severe comminution and bone loss should be considered as indications for plate fixation, while intramedullary nailing offers better cosmesis, and decreased soft tissue disruption.
References
- 1.Cheng JC, Ng BK, Ying SY, Lam PK.A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop. 1999;19:344-50 [PubMed] [Google Scholar]
- 2.Jones K, Weiner DS.The management of forearm fractures in children: a plea for conservatism. J Pediatr Orthop. 1999;19:811-5 [PubMed] [Google Scholar]
- 3.Flynn JM, Jones KJ, Garner MR, Goebel J.Eleven years experience in the operative management of pediatric forearm fractures. J Pediatr Orthop. 2010;30:313-9 [DOI] [PubMed] [Google Scholar]
- 4.Barry M, Paterson JM.A flexible intramedullary nails for fractures in children. J Bone Joint Surg Br. 2004;86:947-53 [DOI] [PubMed] [Google Scholar]
- 5.Ligier JN, Metaizeau JP, Prevot J.[Closed flexible medullary nailing in pediatric traumatology]. Chir Pediatr. 1983;24:383-5 [Article in French]. [PubMed] [Google Scholar]
- 6.Abraham A, Kumar S, Chaudhry S, Ibrahim T.Surgical interventions for diaphyseal fractures of the radius and ulna in children. Cochrane Database Syst Rev 2011:CD007907. [DOI] [PubMed] [Google Scholar]
- 7.Sinikumpu JJ, Pokka T, Serlo W.The changing pattern of pediatric both-bone forearm shaft fractures among 86,000 children from 1997 to 2009. Eur J Pediatr Surg. 2013;23:289-96 [DOI] [PubMed] [Google Scholar]
- 8.Lyons RA, Delahunty AM, Kraus D, et al. Children’s fractures: a population based study. Inj Prev. 1999;5:129-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ceroni D, Martin X, Delhumeau-Cartier C, et al. Is bone mineral mass truly decreased in teenagers with a first episode of forearm fracture? A prospective longitudinal study. J Pediatr Orthop. 2012;32:579-86 [DOI] [PubMed] [Google Scholar]
- 10.Ryan LM, Teach SJ, Searcy K, et al. Epidemiology of pediatric forearm fractures in Washington, DC. J Trauma. 2010;69:S200-5 [DOI] [PubMed] [Google Scholar]
- 11.Khosla S, Melton LJ, 3rd, Dekutoski MB, et al. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290:1479-85 [DOI] [PubMed] [Google Scholar]
- 12.Rivara FP, Grossman DC, Cummings P.Injury prevention. First of two parts. N Engl J Med. 1997;337:543-8 [DOI] [PubMed] [Google Scholar]
- 13.Zionts LE, Zalavras CG, Gerhardt MB.Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediatr Orthop. 2005;25:507-12 [DOI] [PubMed] [Google Scholar]
- 14.Franklin CC, Robinson J, Noonan K, Flynn JM.Evidence-based medicine: management of pediatric forearm fractures. J Pediatr Orthop. 2012;32:S131-4 [DOI] [PubMed] [Google Scholar]
- 15.Price CT.Acceptable alignment of forearm fractures in children: open reduction indications. J Pediatr Orthop. 2010;30:S82-4 [Google Scholar]
- 16.Noonan KJ, Price CT.Forearm and distal radius fractures in children. J Am Acad Orthop Surg. 1998;6:146-56 [DOI] [PubMed] [Google Scholar]
- 17.Tarmuzi NA, Abdullah S, Osman Z, Das S.Paediatric forearm fractures: functional outcome of conservative treatment. Bratisl Lek Listy. 2009;110:563-8 [PubMed] [Google Scholar]
- 18.Richter D, Ostermann PA, Ekkernkamp A, et al. Elastic intramedullary nailing: a minimally invasive concept in the treatment of unstable forearm fractures in children. J Pediatr Orthop. 1998;18:457-61 [PubMed] [Google Scholar]
- 19.Shah AS, Lesniak BP, Wolter TD, et al. Stabilization of adolescent both-bone forearm fractures: a comparison of intramedullary nailing versus open reduction and internal fixation. J Orthop Trauma. 2010;24:440-7 [DOI] [PubMed] [Google Scholar]
- 20.Qairul IH, Kareem BA, Tan AB, Harwant S.Early remodeling in children’s forearm fractures. Med J Malaysia. 2001;56:34-7 [PubMed] [Google Scholar]
- 21.Smith VA, Goodman HJ, Strongwater A, Smith B.Treatment of pediatric both-bone forearm fractures: a comparison of operative techniques. J Pediatr Orthop. 2005;25:309-13 [DOI] [PubMed] [Google Scholar]
- 22.Kamat AS, Pierse N, Devane P, et al. Redefining the cast index: the optimum technique to reduce redisplacement in pediatric distal forearm fractures. J Pediatr Orthop. 2012;32:787-91 [DOI] [PubMed] [Google Scholar]
- 23.Do TT, Strub WM, Foad SL, et al. Reduction versus remodeling in pediatric distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop B. 2003;12:109-15 [DOI] [PubMed] [Google Scholar]
- 24.Holmes JH, Wiebe DJ, Tataria M, et al. The failure of nonoperative management in pediatric solid organ injury: a multi-institutional experience. J Trauma. 2005;59:1309-13 [DOI] [PubMed] [Google Scholar]
- 25.Alpar EK, Thompson K, Owen R, Taylor JF.Midshaft fractures of forearm bones in children. Injury. 1981;13:153-8 [DOI] [PubMed] [Google Scholar]
- 26.Randsborg PH, Sivertsen EA.Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthop. 2009;80:585-589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmuck T, Altermatt S, Buchler P, et al. Greenstick fractures of the middle third of the forearm. A prospective multi-centre study. Eur J Pediatr Surg. 2010;20:316-20 [DOI] [PubMed] [Google Scholar]
- 28.Wright PB, Crepeau AE, Herrera-Soto JA, Price CT.Radius crossover sign: an indication of malreduced radius shaft greenstick fractures. J Pediatr Orthop. 2012;32:e15-9 [DOI] [PubMed] [Google Scholar]
- 29.Iobst CA, Tidwell MA, King WF.Nonoperative management of pediatric type I open fractures. J Pediatr Orthop. 2005;25:513-7 [DOI] [PubMed] [Google Scholar]
- 30.Wyrsch B, Mencio GA, Green NE.Open reduction and internal fixation of pediatric forearm fractures. J Pediatr Orthop. 1996;16:644-50 [DOI] [PubMed] [Google Scholar]
- 31.Bhaskar AR, Roberts JA.Treatment of unstable fractures of the forearm in children. Is plating of a single bone adequate? J Bone Joint Surg Br. 2001;83:253-8 [DOI] [PubMed] [Google Scholar]
- 32.Peterson HA.Metallic implant removal in children. J Pediatr Orthop. 2005;25:107-15 [DOI] [PubMed] [Google Scholar]
- 33.Kim WY, Zenios M, Kumar A, Abdulkadir U.The removal of forearm plates in children. Injury. 2005;36:1427-30 [DOI] [PubMed] [Google Scholar]
- 34.Clement ND, Yousif F, Duckworth AD, et al. Retention of forearm plates: risks and benefits in a paediatric population. J Bone Joint Surg Br. 2012;94:134-7 [DOI] [PubMed] [Google Scholar]
- 35.Vopat B, Kane P, Fitzgibbons P, et al. Complications associated with retained implants after plate fixation of the pediatric forearm. J Orthop Trauma. 2014;28:360-4 [DOI] [PubMed] [Google Scholar]
- 36.Dahlin LB, Duppe H.Injuries to the nerves associated with fractured forearms in children. Scand J Plast Reconstr Surg Hand Surg. 2007;41:207-10 [DOI] [PubMed] [Google Scholar]
- 37.Prevot J.[Stable elastic nailing]. Z Unfallchir Versicherungsmed Berufskr. 1989;82:252-60 [Article in French]. [PubMed] [Google Scholar]
- 38.Lascombes P, Haumont T, Journeau P.Use and abuse of flexible intramedullary nailing in children and adolescents. J Pediatr Orthop. 2006;26:827-34 [DOI] [PubMed] [Google Scholar]
- 39.Kang SN, Mangwani J, Ramachandran M, et al. Elastic intramedullary nailing of paediatric fractures of the forearm: a decade of experience in a teaching hospital in the United Kingdom. J Bone Joint Surg Br. 2011;93:262-5 [DOI] [PubMed] [Google Scholar]
- 40.Dietz JF, Bae DS, Reiff E, et al. Single bone intramedullary fixation of the ulna in pediatric both bone forearm fractures: analysis of short-term clinical and radiographic results. J Pediatr Orthop. 2010;30:420-4 [DOI] [PubMed] [Google Scholar]
- 41.Martus JE, Preston RK, Schoenecker JG, et al. Complications and outcomes of diaphyseal forearm fracture intramedullary nailing: a comparison of pediatric and adolescent age groups. J Pediatr Orthop. 2013;33:598-607 [DOI] [PubMed] [Google Scholar]
- 42.Yuan PS, Pring ME, Gaynor TP, et al. Compartment syndrome following intramedullary fixation of pediatric forearm fractures. J Pediatr Orthop. 2024;24:370-5 [DOI] [PubMed] [Google Scholar]
- 43.Teoh KH, Chee YH, Shortt N, et al. An age-and sex-matched comparative study on both-bone diaphyseal paediatric forearm fracture. J Child Orthop. 2009;3:367-73 [DOI] [PMC free article] [PubMed] [Google Scholar]


