Abstract
Background:
A better understanding of risk factors associated with postpartum psychosis may contribute to the better management.
Aims:
This study was to identify the risk factors contributing to postpartum psychosis.
Materials and Methods:
In this cross-sectional, case control study 100 patients of postpartum psychosis (PP) were compared with the healthy controls. Risk factors explored were sociodemographic factors (age, education, occupation, income, and family type); positive family history; pregnancy and perinatal factors (number of antenatal check-up, parity, and complications during pregnancy, perinatal phase or in newborn); and presence of husband during peripartum period. Data were analyzed by graph pad instat software using chi square test and Fisher's exact test.
Results:
Total of 64% patients and 42% controls were less than 25 years of age (P = 0.001). Among the patients, 62% were primiparae compared with 46% in the controls (P = 0.02). Per capita family income was less than 5000 INR in 72% patients and 56% controls (P = 0.01). Maternal complications during perinatal period were observed in 38% patients and 22% controls (P = 0.01), while the complications in newborns were seen in 21% patients and 8% controls (P = 0.009). Husband was present in 58% patients and 76% controls. (P = 0.006).
Conclusions:
The risk factors related to PP were younger age, lower per capita income, perinatal and neonatal complications, and absence of husband in peripartum phase.
Keywords: Mental illness, Neonatal complications, Puerperal, Psychiatric illness
Introduction
Postpartum period is vulnerable for psychosis which affects a significant number of women, often ending in tragic consequences. Postpartum psychosis (PP) has been related to bipolar disorder spectrum,[1] and there is an intense debate on its nosological status.[2] Proper management of postpartum illnesses by clinical or public health intervention requires reliable identification of the risk factors. Unfortunately, the risk factors related to PP are poorly understood. Various studies have highlighted several risk factors such as primiparity,[3] pregnancy complications,[4] obstetric complications,[5] cesarean section,[6] female baby,[7] lack of social support,[8] history of affective illness,[9] stressful life events,[4] estrogen withdrawal,[10] family history of psychosis,[11] sleep loss,[12] and many others.[13]
Differences among those observations might be due to differences of study environments or geographical variations. Worldwide, there are difficult geographical terrains from which migration for livelihood is a rule rather than exception. In India, Uttarakhand is such a state where 93% of total geographical area is mountainous.[14] Most of the males residing there migrate to plain areas in neighboring states like Uttar Pradesh and Delhi in search for their livelihood. These people visit their homes once in 3-6 months for duration of 1-2 weeks. As a result, their wives are deprived of their husband's care and support in a major part of their life including perinatal phase. This may make them more vulnerable to postpartum psychosis (PP) in comparison to females living in other areas, who enjoy their husband's support and care during perinatal phase. We could not find any study exploring identification of risk factors of PP in such population, therefore, the present study was designed to fill the gap.
Materials and Methods
This cross sectional, case control study was conducted in a government tertiary care hospital in sub Himalayan region of Uttarakhand, India. The hospital is the only centre providing facilities for psychiatric care in the entire rural areas of hills. After obtaining institutional ethics committee's approval, this study was carried out from Jan 2010 to Sept 2012.
The patients presenting to the psychiatry department, who had onset of psychiatric disturbances within 42 days of delivery, were considered for study. The duration was kept 42 days to include postpartum onset definitions of both DSM IV and ICD 10 which are 4 and 6 weeks respectively.[15,16] Further, duration of puerperium is considered as 6 weeks.[17] Those with psychotic symptoms whether affective or non affective were included in the study. Exclusion criteria included non-psychotic illness, past history of psychiatric illness, and refusal to give written informed consent.
Hundred consecutive patients who met these criteria were enrolled in the study. Complete psychiatric history was followed by physical and mental status examination in all patients. All patients were subjected to a questionnaire for socio-demographic factors, past history of medical or psychiatric illness, and details of pregnancy and childbirth including pregnancy complications, perinatal complications and neonatal complications. Pregnancy complications included any medical illness having onset or exacerbation during pregnancy like infections, preeclampsia, and hematological, endocrinal, or cardiac abnormalities. Perinatal complications included antepartum hemorrhage, birth canal injuries, puerperal sepsis, postpartum hemorrhage and eclampsia. Neonatal complications included preterm birth, birth trauma, birth asphyxia, jaundice, respiratory distress, neonatal death or any other illness requiring hospitalization of infant. Questionnaire also enquired about the presence of husband during peripartum period. Husband was considered present, if he was present during the delivery or arrived within 48 hours of delivery.
All such patients were seen by consultant psychiatrist, and diagnoses were made as per the Diagnostic and Statistical Manual of Mental Disorders-Fourth edition-Text Revision (DSM IV-TR). Meanwhile, similar number of controls, such as healthy women who did not develop psychiatric illness, were recruited from women visiting to the Department of Obstetrics and Gynecology for their second routine postnatal care, which is conducted at end of six weeks postpartum.[17] Controls were also subjected to the same questionnaire.
Statistical analysis
Statistical analysis was done using GraphPad InStat version 3.06 software. The categorical data were expressed as percentages, and their difference were compared using Chi Square test and Fisher's exact test. P < 0.05 was considered statistically significant.
Results
During the study period, 146 patients presented to Psychiatry Department for postpartum psychiatric illnesses. Total of 27 patients had non-psychotic illnesses, 15 patients had past history of psychiatric illness, and 4 patients refused to participate in the study.
Out of 100 patients of PP, 24 patients were referred from the same institute, 53 were referred from peripheral centers and 33 presented directly. Mean age for patients was 22.3 years and for controls was 26.3 years.
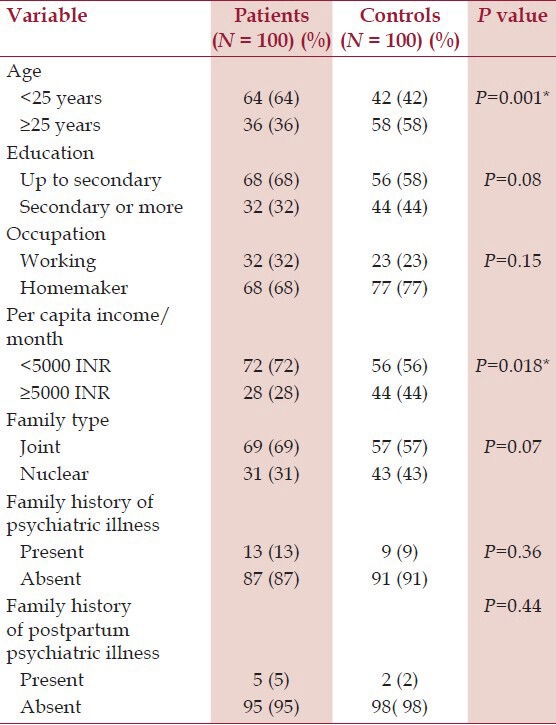
Socio-demographic factors like marital status, education, occupation, and family type had no impact, but lower age and lower per-capita income were significantly associated with PP. Positive family history of psychiatric illness or postpartum psychiatric illness was not associated with PP [Table 1].
Table 1.
Socio-demographic and illness related factors
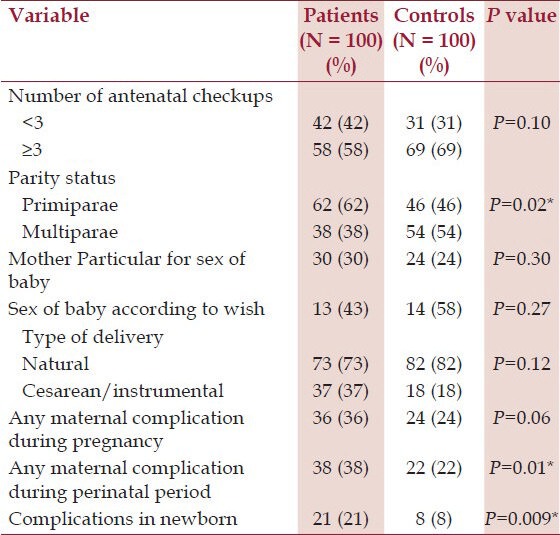
Among pregnancy and perinatal factors, primiparity, maternal complication during perinatal period, and complication in newborn were significantly associated with PP. Thirty patients and 22 controls were particular about the sex of the baby, of which only 13 (43%) and 14 (58%) had their wish fulfilled, respectively. It did not have any influence on PP [Table 2].
Table 2.
Pregnancy related and perinatal factors
Husband was present in 58% of patients and 76% controls imparting a statistically significant difference (P = 0.006). Affective, schizophrenic, schizoaffective and unspecified symptoms were seen in 32%, 15%, 9%, and 44% patients, respectively.
Discussion
We observed that PP was significantly more common in less than 25 year age group compared with controls. Past studies have revealed variable reports regarding relationships between age and onset of PP. In a study of psychiatric disorder in pregnant and postpartum women in United States, Lopez OV et al.,[4] observed that PP was more common in 18 to 25 years age group. In contrast, Valdimarsdottir et al.,[18] found that mothers at age of 35 years or older have double fold increase risk of PP, compared with mothers at age of 19 years or younger. Therefore, it is likely that, in addition to age of mother, PP depends on interaction of many other factors.
We did not find any difference related to education, occupation or family type, but lower per capita income had significant role in the development of PP. Role of low socioeconomic status as a risk factor for psychosis is well established in literature.[19] One study even observed that poor socio-economic environment of the neighborhood might contribute to the development of PP.[20] It was seen that PP was significantly more common in primiparae in comparison with multiparae. This fact is well established in earlier research that primiparae are more prone to PP.[3,5]
We observed that mother's wish for a particular sex of baby and its non-fulfilment did not have any impact. We could not find any study of PP exploring mother's wish for a particular sex, however, John J et al.[21] observed that those who were particular about sex of the child were more prone to develop postpartum depression. Studies from India[22] and China[23] also suggested that disappointment with the sex of the baby was significantly associated with development of postpartum depression. Therefore, disappointment with sex of child may possibly result in postpartum depression, but not psychosis.
In our study, the number of antenatal checkups and the type of delivery did not influence PP. Some authors related cesarean section with postpartum psychosis,[24,25] but other studies did not support it.[18]
Complications during pregnancy had no impact, although the perinatal maternal complications and neonatal complications had significant association with PP. The similar trends were observed in a recent population based retrospective study, which revealed that although prenatal complications were not associated with PP, women with puerperium complications were twice as likely as those without them to develop PP.[26] In a Swedish study, it was found that neonatal complications like respiratory disorder in the neonate, severe birth asphyxia, preterm birth, and perinatal death were associated with an increased risk of PP.[25]
Absence of husband during the delivery had significant association with development of PP. Some studies have showed that single mothers or those women not cohabitating with father of the child are more prone to PP.[27] Literature also reveals that marital discord or intimate partner violence has negative impact on postpartum mental health.[28] Our study emphasizes another aspect of this partner support spectrum in which husband is legal father of the child, and his absence is the determining factor. This factor is important in our study which was conducted in a hilly area where males migrate from their native places in search for jobs leaving their wives behind to take care of their parents and property. Thus, young couples get very less time to spend together. Lack of social support has been established as a strong risk factor for postpartum depression,[29] and severe depression may be associated with psychotic symptoms.
We conclude that risk factors related to development of PP were young age, low per capita income, perinatal complications, neonatal complications and absence of husband during the peripartum phase.
Limitations of study
This is a cross-sectional study so we are unable to precisely link the risk factors with effect. The sample size was relatively small as the sample included only the cases who presented to the Psychiatry Department, thus, our findings need to be confirmed by a large scale community survey. Further, there are many other biological, hormonal, genetic, environmental, and cultural factors which might be related to postpartum psychosis, but not included because of feasibility limitations. It focused only on exploration of most consistently reported variables. The retrospective nature of the study was another limitation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Di Florio A, Forty L, Gordon-Smith K, Heron J, Jones L, Craddock N, et al. Perinatal episodes across the mood disorder spectrum. JAMA Psychiatry. 2013;70:168–75. doi: 10.1001/jamapsychiatry.2013.279. [DOI] [PubMed] [Google Scholar]
- 2.Jones I, Cantwell R. Nosology Working Group, Royal College of Psychiatrists, Perinatal Section. The classification of perinatal mood disorders--suggestions for DSMV and ICD11. Arch Womens Ment Health. 2010;13:33–6. doi: 10.1007/s00737-009-0122-1. [DOI] [PubMed] [Google Scholar]
- 3.Bergink V, Lambregtse-van den Berg MP, Koorengevel KM, Kupka R, Kushner SA. First-onset psychosis occurring in the postpartum period: A prospective cohort study. J Clin Psychiatry. 2011;72:1531–7. doi: 10.4088/JCP.10m06648. [DOI] [PubMed] [Google Scholar]
- 4.Lopez OV, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65:805–15. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blackmore ER, Jones I, Doshi M, Haque S, Holder R, Brockington I, et al. Obstretic variables associated with bipolar affective psychosis. Br J Psychiatry. 2006;188:32–6. doi: 10.1192/bjp.188.1.32. [DOI] [PubMed] [Google Scholar]
- 6.Bener A, Gerber LM, Sheikh J. Prevalence of psychiatric disorder and associated risk factors in women during their postpartum period: A major public health problem and global comparison. Int J Womens Health. 2012;4:191–200. doi: 10.2147/IJWH.S29380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agrawal P, Bhatia MS, Malik SC. Postpartum psychosis: A study of indoor cases in a general hospital psychiatric clinic. Acta Psychiatr Scand. 1990;81:571–5. doi: 10.1111/j.1600-0447.1990.tb05501.x. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez MA, Valentine J, Ahmed SR, Elsenman DP, Sumner LA, Heilemann MV, et al. Intimate partner violence and maternal depression during the perinatal period: A longitudinal investigation of Latinas. Violence Against Women. 2010;16:543–59. doi: 10.1177/1077801210366959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Topiwala A, Hothi G, Ebmeier KP. Identifying patients at risk of perinatal mood disorders. Practitioner. 2012;256:15–8. [PubMed] [Google Scholar]
- 10.Saleh el-S, EL-Bahei W, Del El-Hadidy MA, Zayed A. Predictors of postpartum depression in a sample of Egyptian women. Neuropsychiatr Dis Treat. 2013;9:15–24. doi: 10.2147/NDT.S37156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones I, Craddock N. Familiality of the puerperal trigger in bipolar disorder: Results of a family study. Am J Psychiatry. 2001;158:913–7. doi: 10.1176/appi.ajp.158.6.913. [DOI] [PubMed] [Google Scholar]
- 12.Sharma V, Smith A, Khan M. The relationship between duration of labour, time of delivery, and puerperal psychosis. J Affect Disord. 2004;83:215–20. doi: 10.1016/j.jad.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Halbreich U. Postpartum disorders: Multiple interacting underlying mechanisms and risk factors. J Affect Disord. 2005;88:1–7. doi: 10.1016/j.jad.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Dehradun, India: [Last accessed 2013 Nov 10]. Indian State of Forest Report 2011. Published by Forest Survey of India. (Ministry of Environment & Forests) Available from: http://www.fsi.org.in/cover_2011/uttarakhand.pdf . [Google Scholar]
- 15.Washington, DC: Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) American Psychiatric Association; 1994. [Google Scholar]
- 16.Geneva: WHO; 1992. World Health Organisation. International statistical classification of diseases and related health problems, 10th revision (ICD-10) [Google Scholar]
- 17.Dutta DC. Normal puerperium. In: Konar H, editor. Text Book of Obstetrics. 6th ed. Kolkata: New central book agency private limited; 2004. pp. 145–54. [Google Scholar]
- 18.Valdimarsdóttir U, Hultman CM, Harlow B, Cnattingius S, Sparén P. Psychotic illness in first-time mothers with no previous psychiatric hospitalizations: A population-based study. PLoS Med. 2009;6:e13. doi: 10.1371/journal.pmed.1000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tiikkaja S, Sandin S, Malki N, Modin B, Sparén P, Hultman CM. Social class, social mobility and risk of psychiatric disorder - A population- based longitudinal study. PLoS One. 2013;8:e77975. doi: 10.1371/journal.pone.0077975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nager A, Johansson LM, Sundquist K. Neighborhood socioeconomic environment and risk of postpartum psychosis. Arch Womens Ment Health. 2006;9:81–6. doi: 10.1007/s00737-005-0107-7. [DOI] [PubMed] [Google Scholar]
- 21.John J, Seetalakshmi, Charles SX, Varghese A. Psychiatric disturbance during the postpartum period – A prospective study. Indian J Psychiatry. 1977;19:40–3. [Google Scholar]
- 22.Patel V, Rodriques M, DeSouza N. Gender, poverty, and postnatal depression: A study of mothers in Goa, India. Am J Psychiatry. 2002;159:43–7. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 23.Lee DT, Yip AS, Leung TY, Chung TK. Identifying women at risk of postnatal depression: Prospective longitudinal study. Hong Kong Med J. 2000;6:349–54. [PubMed] [Google Scholar]
- 24.Kendell RE, Rennie D, Clarke JA, Dean C. The social and obstetric correlates of psychiatric admission in the puer-perium. Psychol Med. 1981;11:341–50. doi: 10.1017/s0033291700052156. [DOI] [PubMed] [Google Scholar]
- 25.Nager A, Sundquist K, Ramýrez-Leo´n V, Johansson LM. Obstetric complications and postpartum psychosis: A follow-up study of 1.1 million first-time mothers between 1975 and 2003 in Sweden. Acta Psychiatr Scand. 2008;117:12–9. doi: 10.1111/j.1600-0447.2007.01096.x. [DOI] [PubMed] [Google Scholar]
- 26.Hellerstedt WL, Phelan SM, Cnattingius S, Hultman CM, Harlow BL. Are prenatal, obstetric, and infant complications associated with postpartum psychosis among women with pre-conception psychiatric hospitalisations? BJOG. 2013;120:446–55. doi: 10.1111/1471-0528.12073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nager A, Johansson LM, Sundquist K. Are sociodemographic factors and year of delivery associated with hospital admission for postpartum psychosis? A study of 500,000 first-time mothers. Acta Psychiatr Scand. 2005;112:47–53. doi: 10.1111/j.1600-0447.2005.00525.x. [DOI] [PubMed] [Google Scholar]
- 28.Marks MN, Wieck A, Checkley SA, Kumar R. Contribution of psychological and social factors to psychotic and non-psychotic relapse after childbirth in women with previous histories of affective disorder. J Affect Disord. 1992;24:253–63. doi: 10.1016/0165-0327(92)90110-r. [DOI] [PubMed] [Google Scholar]
- 29.Nielsen Forman D, Videbech P, Hedegaard M, Dalby Salvig J, Secher NJ. Postpartum depression: Identification of women at risk. BJOG. 2000;107:1210–7. doi: 10.1111/j.1471-0528.2000.tb11609.x. [DOI] [PubMed] [Google Scholar]


