Abstract
INTRODUCTION:
Single-port laparoscopy is prospected as the future of minimal invasive surgery. It is hypothesised to cause less post operative pain, with a shorter hospitalisation period and improved cosmetic results. Population- and patient-based opinion is important for the adaptation of new techniques. This study aimed to assess the opinion and perception of a healthy population and a patient population on single-port laparoscopy compared with conventional laparoscopy.
MATERIALS AND METHODS:
An anonymous 33-item questionnaire, describing conventional and single-port laparoscopy, was given to 101 patients and 104 healthy volunteers. The survey participants (median age 44 years; range 17-82 years) were asked questions about their personal situation and their expectations and perceptions of the two different surgical techniques; conventional multi-port laparoscopy and single-port laparoscopy.
RESULTS:
A total of 72% of the participants had never heard of single-port laparoscopy before. The most important concern in both groups was the risk of surgical complications. When complication risks remain similar, 80% prefers single-port laparoscopy to conventional laparoscopy. When the risk of complications increases from 1% to 10%, 43% of all participants prefer single-port laparoscopy. A total of 70% of the participants are prepared to receive treatment in another hospital if single-port surgery is not performed in their hometown hospital. The preference for single-port approach was higher in the female population.
CONCLUSION:
Although cure and safety remain the main concerns, the population and patients group have a favourable perception of single-port surgery. The impact of public opinion and patient perception towards innovative techniques is undeniable. If the safety of the two different procedures is similar, this study shows a positive attitude of both participant groups in favour of single-port laparoscopy. However, solid scientific proof for the safety and feasibility of this new surgical technique needs to be obtained before this procedure can be implemented into everyday practice.
Keywords: NOTES, single-port laparoscopy, questionnaire
INTRODUCTION
Innovative surgical techniques are evolving rapidly. A result of these innovations is the rise of single-port laparoscopy in the past 20 years.[1,2] Currently, in some hospitals single-port laparoscopy has already been implemented as standard of care for laparoscopic cholecystectomy and appendectomy. Additionally, other procedures like hysterectomy, staging laparoscopy, salpingectomy, appendectomy, right hemicolectomy, prostatectomy, nephrectomy and pyeloplasty have been described, using this single-port laparoscopic technique, but these are not yet common practices.[3,4,5]
Single-port laparoscopy reduces the number of trans-parietal incisions made from numerous to only one access. The postulated advantages over conventional laparoscopy include reduction of post operative pain, faster recovery, less impact on quality of life and improved cosmetic results.[6]
In today's society, where cosmetics are of increasing importance, minimally invasive procedures are an attractive alternative for the public. Recent publications have shown the positive attitude of the general population towards these innovative techniques.[7,8,9] Comparable to the favourable public opinion on laparoscopic cholecystectomy in the 20th century, we might expect that public demand for even less invasive techniques will increase.[9,10] This influence of the public opinion and the success and adoption of innovative techniques should not be underestimated and is one of the factors that direct future developments.
In exploring the public's attitude, not only the opinion of actual patients but also of those who might become such, is important. Therefore we performed an opinion-questionnaire for both patient population and general population to assess their perceptions toward this new approach.
MATERIALS AND METHODS
Survey Structure and Design
A 33-item survey [Appendix 1] was designed to assess the public opinion on single-port laparoscopy. Both techniques, conventional laparoscopy and single-port laparoscopy, were described in non-medical terms and illustrated using pictures of the incision sites. A cholecystectomy procedure was used as the referent procedure. The medical — ethical committee approved the study and informed consent was obtained from every participant. Items in the questionnaire included age, sex, education, employment status and surgical history. The questionnaire also included questions about expectations and importance of several factors (including cosmetic results, hospitalisation period and post operative pain).
Survey Population
This study was a cross-sectional survey during a period of 20 weeks. In order to obtain diversity in the general population group, we invited people travelling by train, on a variety of routes through the Netherlands, to participate. The patient group was collected at the surgical outpatient clinic of the Maastricht University Medical Centre. This group was asked to fill out the questionnaire while waiting for the appointment with their surgeon. The investigators directly contacted all participants. The study excluded participants aged younger than 16 years as well as illiterate people and legally incapable people.
Survey Procedure
Participation in this study was completely voluntary and no reward was offered for participation. Participants were asked to complete the questionnaire at the time of distribution.
Survey Sample Size
Based on recent population surveys, we hypothesised that two-thirds (66%) of the participants would prefer single-port laparoscopy over conventional laparopscopy.[7,8,9,10,11,12] In order to determine whether this proportion was significantly different from the 50% distribution, a sample size of 75 participants per population group with alpha 0.05 (two-tailed) and a power of 80% was calculated.[7,8,9]
Survey Statistics
Categorical variables were reported as frequencies and percentages, and compared using the Chi-square test or analysis of variance (ANOVA) test. Adjusted odds ratios were calculated by multiple logistic regression methods. Variables of clinical significance were included in the logistic model. All P values lower than 0.05 were considered clinically significant. The statistical analysis was conducted using IBM SPSS Statistics, version 18.0.
RESULTS
Survey Respondents
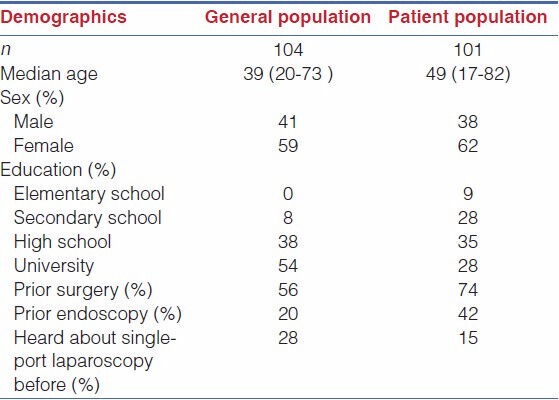
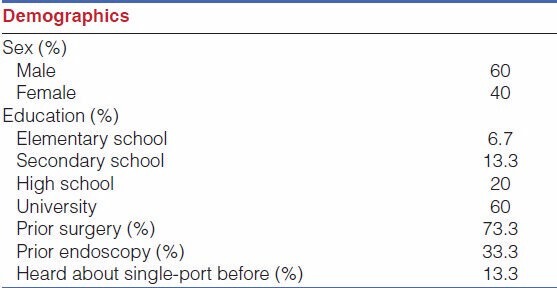
Surveys were collected from 205 participants, including general population (n=101) and patients (n=104). The demographic data of these responders are presented in Table 1.
Table 1.
Survey population demographic data
Perception of Surgical Safety and Cosmesis
When considering the possibility of single-port laparoscopy, the main concern in both groups was the risk of complications. A total of 96% of the participants placed this item first on the importance list. Age, sex, education, profession or medical history did not influence this. The second most important concern was time to recovery, followed by post operative pain, duration of hospitalisation, duration of surgery and anaesthesia. The cosmetics and cost of the procedure were scored as least important in both groups [Table 2].
Table 2.
Factors of importance for choice of surgical technique
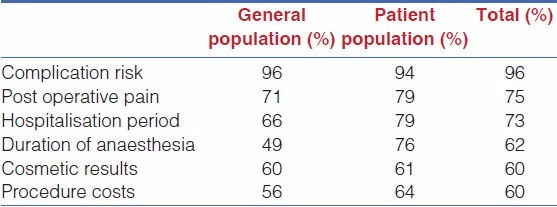
The patient group is more concerned by the immediate surgery related items compared with the population group. The duration of hospitalisation is significantly more important to the patient group (79% versus 66%, P = 0.027). Also, the procedure cost scores significantly more important to the patient group (64% versus 55%, P = 0.000). This was not related to age, sex, education level, employment status or medical history. As mentioned, cosmetic results seem to be less important but, when analysing only the female participants, it was considered more important (73.4% compared with the male participants 43.3%).
Perceptions of Single-port Laparoscopy
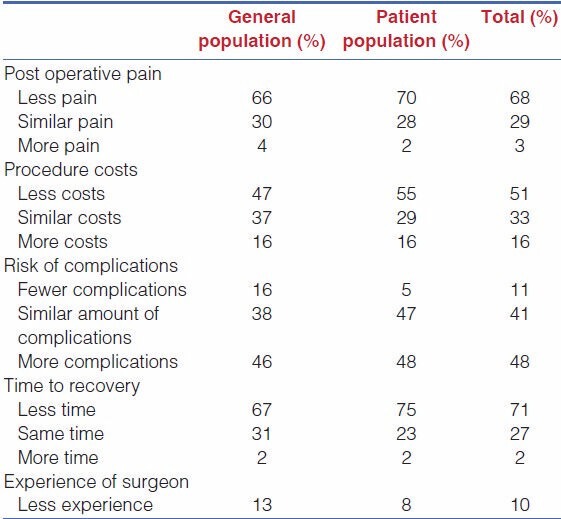
Overall the participants' (patients and population group) expectations towards single-port laparoscopy compared with conventional laparoscopy are positive. A total of 68% of the participants believe that single-port laparoscopy causes less post operative pain compared with the standard laparoscopy procedure. A total of 71% expect a quicker recovery time and 51% expect single-port laparoscopy to be cheaper.
Concerning the experience of the surgeon, the participants perceive the required experience for single-port laparoscopy to be at least similar (44%) or more (46%) compared with conventional laparoscopy. A total of 48% believe that the risk of complications will be higher for single-port laparoscopy than for standard laparoscopy [Table 3].
Table 3.
Participants' expectation about single-port laparoscopy compared with standard laparoscopic surgery
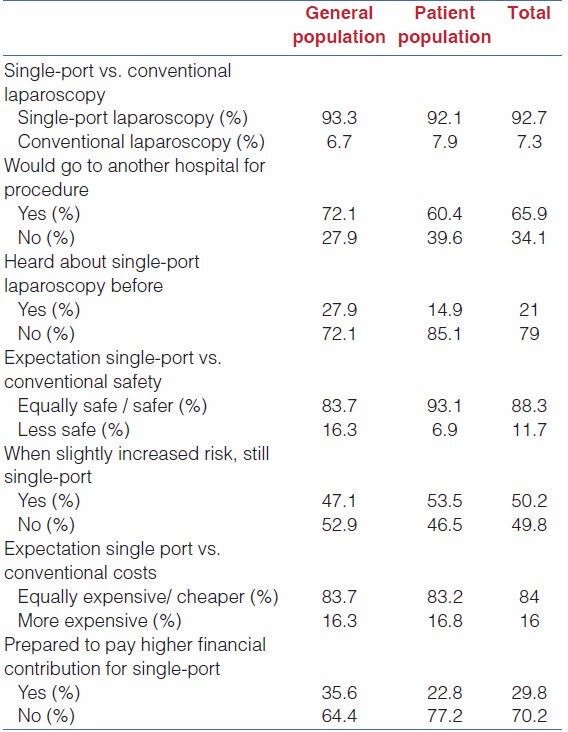
Over 90% in both groups would choose single-port laparoscopy as first choice given the information provided via the questionnaire. A total of 72% of the population group and 60% of the patient group would even be prepared to change from hospital to have single-port laparoscopy.
Even when the risk for complications is higher (10% instead of 1%), about half the group would still consider single-port laparoscopy [Table 4].
Table 4.
General considerations regarding single-port laparoscopy
The small group of participants who would not consider single-port laparoscopy, reasoned that the technique is too new (42%) and does not have enough advantages compared with the conventional laparoscopy (28%). A total of 25% of this group stated another un-defined reason.
A total of 60% of the participants who would not choose single-port laparoscopy are male. Of this group, 73.3% had prior surgery and 33.3% had an endoscopic investigation in the past. Only 13.3% of these participants had heard about single-port laparoscopy before [Table 5].
Table 5.
Demographics of participants who would not choose single-port surgery
DISCUSSION
With the emergence of further advances in minimally invasive technology, approaches such as single-port surgery and natural orifice transluminal endoscopic surgery (NOTES) are a logical further step. The concept of minimally invasive surgery is gaining popularity among medical professionals. However, these new techniques can only be implemented into everyday practice once solid scientific proof of their feasibility and safety is obtained.[12,13]
Even though scientists and clinicians tend to underestimate the influence of public opinion on the rise (and fall) of these innovative techniques, external factors, like economy, politics, industrial marketing and public opinion can interfere with the implementation of new techniques. In today's socio-economic environment, patients progressively demand for medical care that accelerates functional recovery and protects body image. This attitude might influence the need for new surgical techniques.[7,8,9]
The introduction of laparoscopic cholecystectomy 20 years ago revolutionised the surgical world and changed the approach of surgical procedures forever, despite the fact that the first study results concluded that the new surgical technique resulted into little patient benefit, besides cosmetics. Additional higher operative risks were initially reported for this new technique. The laparoscopic revolution proceeded, based only on mere expectation of reduced complication rates. In the absence of objectively derived scientific support, its widespread adoption was far from evidence based.[11,13,14] Certainly, laparoscopic cholecystectomy has since proven itself to provide our patients with great benefits.
In this era of exponential growth in technological innovation, it was only a matter of time before new technologies, such as single-port laparoscopy and NOTES, with as much promise as laparoscopic surgery in the 1990s, would emerge. Without a doubt, these new technologies can only be implemented once solid scientific proof of safety is obtained. Hence, before a technique might be adopted, public opinion could be of influence on adoption of these techniques.[8,9,10] Studies focusing on the consumer and/or patient's perceptions of the concept of laparoscopic cholecystectomy were certainly lacking in the past.[14,15,16]
Despite investment from the medical device industry and enthusiasm from medical professionals, we must analyse patient preferences and expectations of these novel techniques.
Despite the innovative character of single-port laparoscopy, 92.7% of the participants in this study prefer single-port surgery to conventional laparoscopic methods and even 65.9% would travel to another hospital if their hometown hospital did not offer this new technique. In the beginning of the survey, only 21% of the participants had heard about single-port surgery earlier.
Is there a reason for this postulated public preference of single-port laparoscopy?
Firstly, in this era the enigma of beauty certainly is epitomised.
Secondly, interest and possible adoption of new technologies by the public may be related to the lay person's confidence in the medical profession and lack of knowledge and insight into novel technologies. The common perception is that there is a high standard of safety and professionalism in the healthcare system.
Thirdly, the idea and hypothetical advantage of minimal invasive technique seems quite attractive. Most people will not be aware of the technological obstacles that are yet to be conquered by improving technology and additional training.
Definitely some remarks arose with this study:
The results of the current study suggest that there is public interest in single-port laparoscopy, considered that solid proof that the procedure can be performed with equal safety as conventional methods is available.
In order to maximise the response, the survey was designed to be easily understood and quick to complete. Surgical innovations are developing faster than the ability to prove benefit and safety. The aim of this study was to give a general overview of public and patient opinion on single-port laparoscopy. Therefore we chose to use a non-validated survey.[17]
The study population had a wide distribution of age, sexes and educational status to increase the overall representation. We noted significant differences in demographic variables such as education and employment. These differences are comparable to other survey studies on minimal invasive surgery.[7,8,9]
The authors acknowledge that the survey method is of low methodological quality because the questions used by the surveyors are inherently biased as well. We explored the subjects' preference between two supposed, predetermined outcomes; the supposed outcomes are explained briefly and still are hypothetical. The participants took our information for granted. Therefore we need to be cautious with certain statements and interpretation of numbers and figures; especially since no solid evidence-based conclusion is present yet.
Additionally, the question is raised whether the patient's surgeon and the publicity this procedure receives are biasing patients. However, the survey was conducted in a hospital where single-port laparoscopy is not yet being performed as a standard procedure. Also, the impact of publicity can be diminished by the fact that 79% of participants had never heard of the procedure type at the time they received the survey [Table 4].
Finally, the question might rise, whether or nor it is useful to conduct these patient surveys with this bias on quality and methodology instead of thoroughly validated ones. As described in other articles we believe that the advantages of surveys on patients and populations needs, interests and perceptions is that knowledge of such advancements is distributed quickly and read about around the globe, putting pressure on research. The potential benefits of innovative techniques might be of influence and could partially be the driving force behind the development of new technologies. The results of this study are equal to results of earlier published pilot studies.[7,8,9,10]
CONCLUSION
Although treatment and surgical safety remain the main concerns, the general population group and patients both have a favourable perception of single-port surgery. This study shows a positive attitude of both groups in favour of single-port laparoscopy. The fact that patients are even prepared to go to another hospital to receive the treatment and pay a higher financial contribution for the procedure makes single-port laparoscopy a marketing strategy for hospitals, since it will attract patients in need for minimal invasive surgery. This should encourage hospitals and surgeons to further investigate the feasibility and safety of this relatively new technique. When there is solid scientific proof, single-port laparoscopy might be quickly introduced into everyday practice in order to meet the growing patient demand for innovative, scarless surgery.
APPENDIX 1: QUESTIONNAIRE
PART 1: DEMOGRAPHIC QUESTIONS
Age:
Postal code:
Sex:
Education:
Employed:
-
Have you ever had surgery?
□ Yes □ No → move to question 8
Open or laparoscopic surgery?
-
Have you ever had an endoscopic examination?
□ Yes □ No
Have you ever heard of single-port surgery?
PART 2: SURGERY RELATED QUESTIONS
How important is, on a Likert scale
-
10.
The risk for complications?
-
11.
Post operative pain
-
12.
Time to recovery
-
13.
Duration of hospitalisation
-
14.
Duration of anaesthesia
-
15.
Cosmetics after surgery
-
16.
Cost of the procedure
-
17.
Comparing single-port surgery to conventional laparoscopy: How do you expect the mean pain to be, compared to conventional laparoscopy?
-
18.
How do you rate the cost of single-port laparoscopy, compared to conventional laparoscopy?
-
19.
How do you rate the risk for complications of single-port surgery, compared to conventional laparoscopy?
-
20.
How long do you estimate the time to recovery of single-port surgery, compared to conventional laparoscopy?
-
21.
How do you rate the experience of the surgeon of single-port surgery, compared to conventional laparoscopy?
-
22.
Would you choose for single-port surgery if the surgeon is experienced in laparoscopy, but less experienced in single-port surgery?
□ Yes
□ No
-
23.
Is single-port surgery suitable for children??
-
24.
Is single-port surgery suitable for the working population?
-
25.
Is single-port surgery suitable for the elderly?
-
26.
Is single-port surgery suitable for anyone?
-
27.
If you had the gallbladder to be removed, which procedure would you prefer, supposing the surgeon has experience with both techniques?
□ Conventional laparoscopy
□ Single-port laparoscopy
-
28.
If you would not consider single-port laparoscopy, what is the reason?
□ Too new
□ Too risky
□ No advantages
□ More painful
□ Other reason
-
29.
Would you choose single-port laparoscopy if the risks for complications would be slightly higher compared to conventional laparoscopy?
□ Yes □ No
-
30.
Would you choose single-port laparoscopy if the risks for complications would be much higher compared to conventional laparoscopy?
□ Yes □ No
-
31.
Would you choose single-port laparoscopy, considering you have to pay extra cost?
□ Yes □ No
-
32.
Would you choose single-port laparoscopy if you would be the first patient your surgeon performs single-port laparoscopy on (but certified after master classes.
□ Yes □ No
-
33.
Would you be willing to change from hospital in order to be operated with the single-port laparoscopic technique?
□ Yes □ No
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gettman M, Box G, Averch T, Caddedu JA, Cherullo E, Clayman RV, et al. Consensus statement on natural orifice transluminal endoscopic surgery and single-incision laparoscopic surgery: Heralding new era in urology? Eur Urol. 2008;53:1117–20. doi: 10.1016/j.eururo.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Kelley W. Single-port laparoscopic surgery. Laparosc Today. 2008;7:5–6. [Google Scholar]
- 3.Kosumi T, Kubota A, Usui N, Yamauchi K, Yamasaki M, Oyanagi H. Laparoscopic ovarian cystectomy using a single umbilical puncture method. Surg Laparosc Endosc Percutan Tech. 2001;11:63–5. [PubMed] [Google Scholar]
- 4.Kaouk JH, Palmer JS. Single-port laparoscopic surgery: initial experience in children for varicocelectomy. BJU Int. 2008;102:97–9. doi: 10.1111/j.1464-410X.2008.07584.x. [DOI] [PubMed] [Google Scholar]
- 5.Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, et al. Single port transumbilical (E-NOTES) donor nephrectomy. J Urol. 2008;180:637–41. doi: 10.1016/j.juro.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 6.Fransen S, Stassen L, Bouvy N. Single incision laparoscopic cholecystectomy: A review on the complications. J Minim Access Surg. 2012;8:1–5. doi: 10.4103/0972-9941.91771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varadarajulu S, Tamhane A, Drelichman ER. Patient perception of natural orifice transluminal endoscopic surgery as a technique for cholecystectomy. Gastrointest Endosc. 2008;67:854–60. doi: 10.1016/j.gie.2007.09.053. [DOI] [PubMed] [Google Scholar]
- 8.Bucher P, Pugin F, Ostermann S, Morel P. Patient's point of view on surgical innovations. Rev Med Suisse. 2010;6:1292–7. [PubMed] [Google Scholar]
- 9.Swanstrom L, Volckmann E, Hungness E, Soper N. Patient's attitudes and expectations regarding natural orifice translumenal endoscopic surgery. Surg Endosc. 2009;23:1519–25. doi: 10.1007/s00464-009-0431-5. [DOI] [PubMed] [Google Scholar]
- 10.Osborne DA, Alexander G, Boe B, Zervos eE. Laparoscopic cholecystectomy: Past, present and future. Surg Technol Int. 2006;15:81–5. [PubMed] [Google Scholar]
- 11.Allori AC, Leitman IM, Heitman E. Delayed assessment and eager adoption of laparoscopic cholecystectomy: Implications for developing surgical technologies. World J Gastroenterol. 2010;16:4115–22. doi: 10.3748/wjg.v16.i33.4115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bucher P, Pugin F, Ostermann S, Ris F, Chilcott M, Morel P. Population perception of surgical safety, and body image: A plea for scarless surgery? Surg Endosc. 2011;25:408–15. doi: 10.1007/s00464-010-1180-1. [DOI] [PubMed] [Google Scholar]
- 13.O'Brien PE. The endosurgical revolution: Is it under control? Aust N Z J Surg. 1994;64:588. doi: 10.1111/j.1445-2197.1994.tb02297.x. [DOI] [PubMed] [Google Scholar]
- 14.Allori AC, Leitman IM, Heitman E. Natural orifice translumenal endoscopic surgery: Lessons learned from the laparoscopic revolution. Arch Surg. 2008;143:333–4. doi: 10.1001/archsurg.143.4.333. [DOI] [PubMed] [Google Scholar]
- 15.Sawyers JL. Current status of conventional (open) cholecystectomy versus laparoscopic cholecystectomy. Ann Surg. 1996;223:1–3. doi: 10.1097/00000658-199601000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Botden S, Strijkers R, Fransen S, Stassen L, Bouvy N. The use of curved vs. straight instruments in single-port access surgery, on standardized box trainer tasks. Surg Endosc. 2011;25:2703–10. doi: 10.1007/s00464-011-1633-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rao A, Kynaston J, MacDonald ER, Ahmed I. Patient's preferences for surgical techniques: Should we invest in new approaches? Surg Endosc. 2010;24:3016–25. doi: 10.1007/s00464-010-1078-y. [DOI] [PubMed] [Google Scholar]


