Abstract
INTRODUCTION:
The ‘Rendezvous’ technique consists of laparoscopic cholecystectomy (LC) standards with intra-operative cholangiography followed by endoscopic sphincterotomy. The sphincterotome is driven across the papilla through a guidewire inserted by the transcystic route. In this study, we intended to compare the two methods in a prospective randomised trial.
MATERIALS AND METHODS:
From 2005 to 2012, we enrolled 83 patients with a diagnosis of cholecysto-choledocolithiasis. They were randomised into two groups. In ‘group-A’,41 patients were treated with two stages management, first by pre-operative endoscopic retrograde cholangiopancreatography (ERCP) and common bile duct (CBD) clearance and second by LC. In ‘group-B’, 42 patients were treated with LC and intra-operative cholangiography; and when diagnosis of choledocholithiasis was confirmed, patients had undergone one stage management of by Laparo-endoscopic Rendezvous technique.
RESULTS:
In arm-A and arm-B groups, complete CBD clearance was achieved in 29 and 38 patients, respectively. Failure of the treatment in arm-A was 29% and in arm-B was 9.5%. In arm-A, selective CBD cannulation was achieved in 33 cases (80.5%) and in arm-B in 39 cases (93%). In arm-Agroup, post-ERCP hyperamylasia was presented in nine patients (22%) and severe pancreatitis in five patients (12%) versus none of the patients (0%) in arm-B group, respectively. Mean post-operative hospital stay in arm-A and arm-B groups are 10.9 and 6.8 days, respectively.
CONCLUSION:
One stage laparo-endoscopic rendezvous approach increases selective cannulation of CBD, reduces post-ERCP pancreatitis, reduces days of hospital stay, increases patient's compliance and prevents unnecessary intervention to CBD.
Keywords: Endoscopic retrograde cholangiopancreaticography, laparoscopic cholecystectomy, rendezvous technique, sphincterotomy
INTRODUCTION
Concomitant cholelithiasis with choledocholithiasisis a common clinical problem worldwide. The most commonly used minimal invasive technique in practice is the two-stage management, which consists of pre-operative (or post-operative) endoscopic retrograde cholangiopancreatography (ERCP), sphincterotomy and common bile duct (CBD) clearance followed by laparoscopic cholecystectomy (LC). However, with this approach, a number of patients will be submitted to an unnecessary ERCP while some others will develop complications, mainly pancreatitis due to inadvertent pancreatic duct cannulation. Laparo-endoscopic rendezvous methods have been described in order to obtain selective CBD cannulation and omit the risk of post-ERCP pancreatitis.[1,2,3,4] The term Rendezvous means the meeting of a guide wire (the surgeon passes the guide wire ante-retrogradely through the cystic duct) with endoscope inside the duodenum, presence of guide wire and meeting of two instruments facilitate the cannulation of vater's papilla and also clearance of CBD from the stones.
However, Laparo-endoscopic rendezvous method has not been popularised till now. In the present study, we have initially assessed the feasibility and safety of the laparo-endoscopic rendezvous with a pilot study and then we intended to compare the two methods in a prospective randomised trial.
MATERIALS AND METHODS
This study was conducted, which included patients who were admitted, in the department of surgery, S.C.B. Medical College, Cuttack, Odisha, during the period from 2005 to 2012 with a diagnosis of cholelithiasis and choledocholithiasis. Number of patient studied is 83 (n = 83). After obtaining consent, eligible patients were randomised in arm-A or arm-B groups using sealed opaque envelopes containing computer generated random number. This method meets the criteria for unpredictability and blinding. Patients, who met the inclusion criteria, will be randomly directed to either of the following arms. In arm-A, 41 patients (n = 41) underwent two stage management of cholelithiasis and choledocholithiasis. First stage by pre-operative ERCP and CBD clearance by standard techniques and second stage is classical four port LC. Next in arm-B, 42 patients (n = 42) underwent LC and intra-operative cholangiography, followed by one stage management of cholelithiasis and choledocholithiasis by Laparo-endoscopic Rendezvous procedure as described by Cavina et al.,[1] in 1998. Both arms of all the patients were evaluated by ultrasound abdomen and MRCP.
All patients having stone more than 12 mm in CBD were excluded from the study that underwent laparoscopic CBD exploration.
We studied the following outcome measures: Success rate of CBD clearance during ERCP comparing single stage versus double, failure rate of selective CBD cannulation during ERCP, incidence of multiple endoscopic procedures within 30 days of the procedure, incidence of hyperamylasemia within 48 hours post-ERCP (in this present study we had taken three times of the normal value of serum amylase as criteria to record hyperamylasia), incidence of severe pancreatitis within 48 hours post-ERCP. Severe pancreatitis was diagnosed by combination of recording and evaluation of clinical presentation, biochemical parameters and radiological findings. Post-operative hospital stay was calculated from onset of intervention to discharge. Number of deaths occurred in our study group within 30 days of intervention was recorded. At the time of discharge, we submitted a questionnaire to the patients to analyse his/her compliance concerning the surgical procedure carried out (the questionnaire elicited a simple immediate opinion of the patient concerning his compliance towards the procedure followed, which was graded as high, moderate, low). At the end of every procedure, we submitted a questionnaire to the endoscopic surgeons to analyse his satisfaction concerning the endoscopic procedure. (The questionnaire elicited a simple immediate opinion of the endoscopic surgeon concerning his evaluation of the endoscopic difficulty of the one stage Laparo-endoscopic Rendezvous or classical two stage procedure, which was graded as simpler, comparable, more difficult when compared to other procedure (arm-A vs.arm-B or vice-versa).)
Surgical Technique
Laparo-endoscopic Rendezvous procedure
In this procedure, during LC, a guide wire is inserted through the cystic duct into the CBD, advanced into the duodenum where it is endoscopically gripped with a snare or a polypectomy loop and retrieved through the mouth. The sphincterotome is inserted over the wire and selective CBD cannulation is obtained to be followed by sphincterotomy and CBD clearance intra-operatively. The method has been described by several authors in small to moderate case series, its safety has been proven and it appears that it reduces both the length of hospital stay and the incidence of post-ERCP pancreatitis. Laparo-endoscopic Rendezvous procedure started with classical steps of 4 ports LC with camera port in Umbilicus (10 mm), right hand working port in epigastrium (10 mm), left hand working port in right sub costal region (5 mm), gall bladder retracting port (5 mm). Initial dissection was done till adequate exposure of vital anatomy. Dissection of the cholecystohepatictriangle and identification of cystic duct and artery to visualise clear anatomy was done. Cystic duct is clipped close to gall bladder neck. Without cutting the cystic duct gall bladder was dissected out of the bed keeping its last attachment of the body to liver, which was dissected at the end of the procedure. A rent was made in the cystic duct distal to the ligaclip as placed before and a catheter was entered through this rent. Intra-operative cholangiography was performed by either percutaneous technique or sometimes by cholangiogram clamps [Figure 1]. A guide wire was introduced through the catheter and advanced down through the sphincter of oddi and into the duodenum if possible. Then the guide wire was grasped with a snare or a loop and pulled through the working channel of the duodenoscope and sphincterotome was introduced over the guide wire [Figure 2]. Then sphincterotomy and stone extraction was completed with the standard ERCP techniques [Figure 3]. Then LC was completed by applying another clip distal to the neck of gall bladder along with transection and separation of cystic duct and recovery of the specimen from the abdomen.
Figure 1.
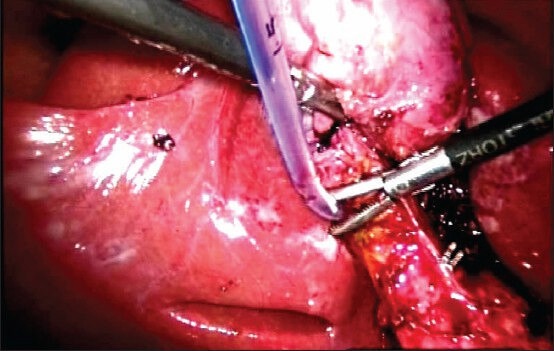
Intra-operative cholangiography being performed using catheter
Figure 2.

Sphincterotome introduced over the guide wire
Figure 3.

Sphincterotomy and stone extraction being done
RESULTS
In the present series, out of 83 patients, 53 were female and 30 were male. A total of 24 patients were found to be in the age group of 51-60 years. Mean patient age is 47.95 years and youngest in the series was aged 21 years and the oldest was aged 75 years. In the present series, pain abdomen was the most common presenting symptom (88%) followed by jaundice (71%), pruritus (37%), fever with chill and rigor (21%), nausea and vomiting (28%). No asymptomatic case has been observed in our study. There was moderate elevation of total serum bilirubin (mean is 7.2 mg/dl), raised serum alkaline phosphatise (mean is 619 IU/L) and increased CBD diameter (mean is 12.6 mm). In ‘arm-A’ (two stage ERCP + LC) group in 37 cases (90.2%) cannulation to papilla was feasible but in ‘arm-B’ (one stage RV) group in 38 cases (90.5%) procedure was feasible.
In arm-A group complete CBD clearance occurred in 29 (71%) patients but in arm-B CBDs were completely cleared of stones in 38 (90.5%) patients. Failure of the treatment in arm-A group is 29% (12 out of 41) and in arm-B group is 9.5% (4 patients out of 42).
In the present study group, in arm-A, selective CBD cannulation was achieved in 33 cases (80.5%) out of the 41 cases and in 39 cases (93%) out of 42 cases in arm-B. In arm-Agroup, post-ERCP hyperamylasia was presented in nine patients (22%) and severe pancreatitis in five patients (12%) versus none of the patients (0%) in arm-B group, respectively. Mean post-operative hospital stay in arm-A and arm-B are 10.9 and 6.8 days, respectively. Post-operative hospital stay was calculated from onset of intervention to discharge.
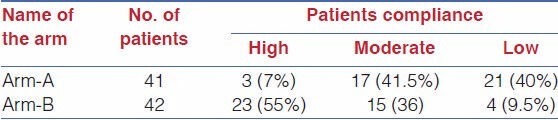
Patients' compliance is shown in Table 1.
Table 1.
Patients' Compliance
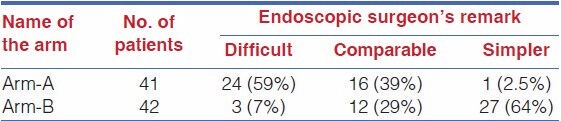
Endoscopic surgeons remark is given in Table 2.
Table 2.
Endoscopic Surgeons Remark
DISCUSSION
Cavina et al.,[1] stated that laparo-endoscopic ‘Rendezvous’ is feasible and a new technique to treat choledocholithiasis. Our study shows that feasibility of both arm-A and arm-B is nearly equal and are 90.2% and 90.5%, respectively. Presence of experienced biliary endoscopist among our surgical staff did facilitate the feasibility as well as performance of Laparo-endoscopic ‘Rendezvous’ in the present series, reducing procedural as well as organisation conflict between surgeon and gastroenterologist.
Residual stones following endoscopic treatment ranges from 17% to 35% according to Lenriot et al.,[5] and Tranter and Thompson.[6] The ‘Rendezvous method’ had higher success rate in stone clearance from CBD (95.6% vs. 80%) as shown by Morino et al.[7] Our study shows that in arm-B (Rendezvous) had higher success rate (90.5%) in stone clearance in comparison to arm-A (71%), that is (90.5% vs. 71%). The 90.5% success rate in group B patients treated with laparo-endoscopic ‘Rendezvous’ compares the favourability with success rate ranging from 90% to 100%.[2,3] We observed failure of treatment in arm-A group is 29% and arm-B group is 9.5% being comparable with other studies.[8,9,10,11] With pre-operative ERCP, there remains a risk of interval migration of additional gallbladder stones before cholecystectomy.[12] This might be one of the reasons of increased failure rate in two stage procedure. This failure in both the two groups was seen mostly in patients with stone size between 9 and 12mm. CBD stones larger than 10 mm in diameter are associated with a lower success rate of endoscopic extraction and a greater need for some form of lithotripsy to facilitate removal.[13,14] Since we have not used mechanical lithotripter in any of the patients, use of it would have reduced this failure rate.
ERCP ‘on table’ (intra-operative) does not give the endoscopist a position that they are used to, for performing ERCP. Hence in order to ease the difficulties, all patients were turned to left lateral position on table during ERCP, then vice versa after completion of ERCP. During our study we had to make some technical adjustments to solve the difficulties faced post-ERCP because gas filled bowel loop made difficult to do LC. To avoid difficulties, the laparoscopic surgeon dissected completely both the calots triangle and the attachment between gallbladder and liver to minimise the dissection needed after ERCP, that is when bowel loops distended by endoscopic insufflations. We observed the technical problems of Rendezvous techniques are related to both the supine position that could make the retrograde cannulation of the papilla more difficult as well as to the gas that is needed for endoscopy, which interfered in some of the initial cases with LC because of distension of bowel loops. During our study we did not hesitate to change the patient's position on the operating table, from supine to lateral and vice-versa so that selective cannulation of CBD was done with ease by endoscopist. This gave the endoscopist better level of satisfaction because, once they have introduced endoscope into second part of duodenum, they could easily catch hold of guide wire and selectively cannulate CBD. This introduction of endoscope would have been difficult in supine position even with best of the endoscopist. Furthermore, in some cases, an atraumatic laparoscopic bowel clamp was positioned on the first jejunal loop to reduce bowel distension with success. We observed that the endoscopic surgeon, in his opinion, considered the laparo-endoscopic Rendezvous procedure was more simpler because the procedure facilitated the identification and cannulation of the papilla, that is a guidewire was inserted through the cystic duct by the laparoscopic surgeon, so at this time the endoscopist had only to grasp the catheter and so they would not cannulate the pancreas and make any false passage. It was difficult for a endoscopist to accept a procedure as in arm-A (two stage ERCP + LC) where there was potential risk of complication and mortality for which we observed in our study that the endoscopist was getting more cautious when they did an ERCP-spincterotomy as under arm-A. Sometimes very cautious attitude leads to less motivation, to push in difficult cases, for fear of injury.
In the present study, the laparo-endoscopic Rendezvous technique presented a reduced failure rate when compared with the sequential ERCP and LC, that is 9.5% versus 29%. This significant difference in our observation might have two main explanations. Firstly that in difficult cases and in patients with low compliance, the endoscopist, knowing that there would be a second chance to cannulate the CBD during LC avoided technically risk manoeuvres during pre-operative ERCP under arm-A. Secondly during laparo-endoscopic Rendezvous, the use of a guidewire reaching the duodenum through the cystic duct via CBD facilitated the cannulation of the papilla in difficult cases.
We observed that during the Rendezavous technique, the use of guide wire, allowed an anterograde cannulation of papilla, avoided the risk of inadvertent cannulation of the pancreatic duct and reduced the rate of pancreatic complications like severe pancreatitis (12% vs. 0%) and post-ERCP hyperamylasia (22% vs. 0%).
There was no death reported of any patients in our study within 30 days of the procedure. Hence, in the present study, we observed that laparo-endoscopic Rendezvous technique is feasible and safe.
The Rendezvous method had a higher success rate, shorter hospital stay (4.3 vs. 8 days) and lesser cost as shown by Morino et al.[7] In the present study, the laparo-endoscopic Rendezvous technique (arm-B) presented a shorter hospital stay as compared with the sequential ERCP and LC (in arm-A), that is (6.8 vs. 10.9 days) comparable to other studies.[13,15] The hospital stay has been calculated from the day of admission, till the day of discharge between which patient underwent ERCP followed by LC in two sittings (i.e, patient has been kept in the hospital after ERCP procedure till cholecystectomy).
In the present study, the one stage laparo-endoscopic Rendezvous technique (arm-B) presented with a better patients compliance when compared with the sequential two stage ERCP and LC (arm-A), that is high patients compliance 55% vs. 7%. In our study high patient's compliance, in our opinion, was having following explanations. First patients had to undertake one OT procedure under anaesthesia. Secondly hospital stay was less.
CONCLUSION
Using laparo-endoscopic Rendezvous approach for the treatment of gall stones and CBD stones is both feasible and effective in stone clearance, in comparison with pre-operative ERCP and LC.
Moreover, the work of an endoscopist becomes simpler and safer in laparo-endoscopic Rendezvous approach than the standard two stage ERCP-ES + LC approach, because of reduction of steps of the endoscopic procedure and avoidance of iatrogenic risk factors. Therefore, laparo-endoscopic rendezvous in the management of cholelithiasis and concomitant choledocholithiasis increases selective cannulation of CBD, reduces post-ERCP pancreatitis, reduces days of hospital stay and increases patient's compliance which is associated with higher success rate, and prevents unnecessary interventions to CBD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Cavina E, Franceschi M, Sidoti F, Goletti O, Buccianti P, Chiarugi M. Laparo-endoscopic ‘Rendezvous’: A new technique in the choledocholithiasis treatment. Hepatogastroenterology. 1998;45:1430–5. [PubMed] [Google Scholar]
- 2.Tricarico A, Cione G, Sozio M, Di Palo P, Bottino V, Tricarico T, et al. Endolaparoscopic rendezvous treatment: A satisfying therapeutic choice for cholecystocholedocholithiasis. Surg Endosc. 2002;16:585–8. doi: 10.1007/s004640090075. [DOI] [PubMed] [Google Scholar]
- 3.Deslandres E, Gagner M, Pomp A, Rheault M, Leduc R, Clermont R, et al. Intraoperative endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy. Gastrointest Endosc. 1993;39:54–8. doi: 10.1016/s0016-5107(93)70011-5. [DOI] [PubMed] [Google Scholar]
- 4.Iodice G, Giardiello C, Francica G, Sarrantonio G, Angelone G, Cristiano S, et al. Single-step treatment of gallbladder and bile duct stones: A combined endoscopic-laparoscopic technique. Gastrointest Endosc. 2001;53:336–8. doi: 10.1016/s0016-5107(01)70409-9. [DOI] [PubMed] [Google Scholar]
- 5.Lenriot JP, Le Neel JC, Hay JM, Jaeck D, Millat B, Fagniez PL. Retrograde cholangiopancreatography and endoscopic sphincterotomy for biliary lithiasis. Prospective evaluation in surgical circle. Gastroenterol Clin Biol. 1993;17:244–50. [PubMed] [Google Scholar]
- 6.Tranter SE, Thompson MH. Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg. 2002;89:1495–504. doi: 10.1046/j.1365-2168.2002.02291.x. [DOI] [PubMed] [Google Scholar]
- 7.Morino M, Baracchi F, Miglietta C, Furlan N, Ragona R, Garbarini A. Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients withgallbladder and bile duct stones. Ann Surg. 2006;244:889–93. doi: 10.1097/01.sla.0000246913.74870.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer C, Le JV, Rohr S, Thiry LC, Duclos B, Reimund JM, et al. Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and perioperative endoscopic sphincterotomy. Surg Endosc. 1999;13:874–7. doi: 10.1007/s004649901123. [DOI] [PubMed] [Google Scholar]
- 9.Filauro M, Comes P, De Conca V, Coccia G, Prandi M, Bagarolo C, et al. Combined laparoendoscopic approach for biliary lithiasis treatment. Hepatogastroenterology. 2000;47:922–6. [PubMed] [Google Scholar]
- 10.Nakajima H, Okubo H, Masuko Y, Osawa S, Ogasawara K, Kambayashi M, et al. Intraoperative endoscopic sphincterotomy during laparoscopic cholecystectomy. Endoscopy. 1996;28:264. doi: 10.1055/s-2007-1005444. [DOI] [PubMed] [Google Scholar]
- 11.Saccomani G, Durante V, Magnolia MR, Ghezzo L, Lombezzi R, Esercizio L, et al. Combined endoscopic treatment for cholelithiasis associated with choledocholithiasis. Surg Endosc. 2005;19:910–4. doi: 10.1007/s00464-003-9314-3. [DOI] [PubMed] [Google Scholar]
- 12.Pierce RA, Jonnalagadda S, Spitler JA, Tessier DJ, Liaw JM, Lall SC, et al. Incidence of residual choledocholithiasis detected by intraoperative cholangiography at the time of laparoscopic cholecystectomy in patients having undergone preoperative ERCP. Surg Endosc. 2008;22:2365–72. doi: 10.1007/s00464-008-9785-3. [DOI] [PubMed] [Google Scholar]
- 13.Cotton PB. Non-operative removal of bile duct stones by duodenoscopic sphincterotomy. Br J Surg. 1980;67:1–5. doi: 10.1002/bjs.1800670102. [DOI] [PubMed] [Google Scholar]
- 14.Lauri A, Horton RC, Davidson BR, Burroughs AK, Dooley JS. Endoscopic extraction of bile duct stones: Management related to stone size. Gut. 1993;34:1718–21. doi: 10.1136/gut.34.12.1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Enochsson L, Lindberg B, Swahn F, Arnelo U. Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscopic cholecystectomy does not prolong hospitalization: A 2-year experience. Surg Endosc. 2004;18:367–71. doi: 10.1007/s00464-003-9021-0. [DOI] [PubMed] [Google Scholar]


