Abstract
Ciliated hepatic foregut cysts (CHFCs) are rare congenital cysts of the liver that originate from the embryologic foregut. Despite an increase in incidence, they remain rare and several key characteristics remain poorly understood, including the range of presentation and the risk of malignant conversion. Large, symptomatic cysts and small asymptomatic, atypical cysts should be resected. We present a patient who recently underwent laparoscopic excision of a CHFC, review the literature and propose the rationale for attempting removal of these cysts through a laparoscopic approach.
Keywords: Ciliated hepatic foregut cyst, foregut cyst, hepatic cyst
INTRODUCTION
Friederich is credited with describing the first case of a ciliated hepatic foregut cyst (CHFC) in 1857 and positing their congenital origin.[1] Wheeler and Edmonson were the first to use the term “CHFC” to describe the lesion.[2] They also identified specific characteristics, which differentiate it from other hepatic cysts, such as the presence of four typical layers: A pseudostratified columnar epithelium layer with interspersed mucus cells, a sub-epithelial connective tissue layer, a smooth muscle layer and an outer fibrous capsule. This lesion is thought to be the result of evagination of the foregut during embryonogenesis. In the last 150 years, approximately 103 cases have been reported in the literature world-wide, only four of which describe laparoscopic excision.[3,4] We report 5th case of a patient who recently underwent successful laparoscopic excision of a CHFC and the rationale for attempting laparoscopic removal of these lesions and review of the literatures.
CASE REPORT
This paper reports a case of a 32-year-old woman presented with a 6-month history of right upper quadrant pain. The pain was controlled with oral analgesics initially, but no response off late. There was no associated jaundice, rigors or weight loss. Apart from minimal right upper quadrant tenderness, examination was unremarkable. Full blood count, liver and renal function tests and clotting profile were normal. The CA 19-9 serum level was 18 IU/l (normal 0-37 IU/l). An abdominal ultrasound scan reported thin walled 10 cm × 7.6 cm × 5.8 cm cyst in the superior part of the right lobe of liver raising a suspicion of a simple cyst of liver. There was no intra-hepatic biliary dilatation or gallstones. Computed tomography [Figure 1] revealed cystic lesion in the segment VIII. The cystic lesion did not enhance postcontrast and appeared to be well circumscribed without evidence of hepatic invasion suggestive of a simple cyst. Therefore, a laparoscopic deroofing of the cyst was planned. At the time of surgery, general anaesthesia was induced and the patient was placed in a supine position. The operation was undertaken as in routine laparoscopic cholecystectomy. Port placement was initiated with a 10-mm infraumbilical trocar followed by two 5-mm ports inferior to the right costal margin along the anterior and midaxillary lines. A 10-mm port was then placed in the epigastrium. Intraoperatively [Figure 2], the 10 cm × 8 cm cyst was found adherent to the superior surface of liver compressing segments VII and VIII. On further dissection, it was noted that the cyst was actually free from the liver parenchyma and was adherent to the liver by a small pedicle. Cyst fluid was aspirated without spillage. Since there was only a pedicle, it was decided to do a complete excision instead of a de-roofing. Pedicle was cauterized using bipolar and resected completely. Pathologic review of the cyst showed an inner layer of ciliated pseudo stratified mucin secreting columnar epithelium with scattered goblet cells surrounded by loose connective tissue, a discontinuous smooth muscle layer and an outer fibrous capsule these findings were consistent with a ciliated foregut cyst of hepatic origin without evidence of epithelial dysplasia or invasive malignancy.
Figure 1.
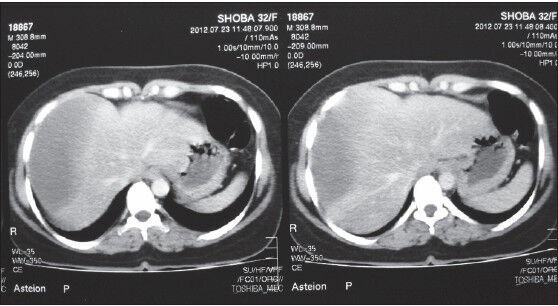
Contrast enhanced computed tomography shows non-enhancing cystic lesion in segment VIII of right lobe of liver
Figure 2.

Laparoscopic view of ciliated hepatic foregut cyst in segment VIII
DISCUSSION
CHFCs are rare, with only 103 cases reported since first described as a congenital malformation by Friederich in 1857.[1] The majority (55) of these cases have been reported in the last 25 years as imaging techniques have improved. The term CHFC was coined to indicate the origin of this lesion as being a detached hepatic diverticulum or detachment and migration of buds from the oesophageal and bronchial regions of the foregut and subsequent entrapment by the liver during the early embryonic development of the foregut. It is found most commonly in segment IV of the left lobe just beneath the hepatic capsule. The cyst size ranges from <1 cm to 24 cm in greatest diameter, the mean greatest dimension is 4 cm and the median is 3 cm. The average age of presentation is 52 years, ranging from 3 months to 82 years, with a slight female predominance. Nearly 40% of the reported cases have been found incidentally on imaging studies, 26% incidentally at autopsy, 6% incidentally at surgery and 22% presented with abdominal symptoms. CHFC are most frequently located superficially in the median segments of the liver (segments IV, V, VIII), are rarely multi-loculated or septated and are mostly asymptomatic.[2] The characteristic position of the lesion can potentially be explained by embryologic histogenesis. They also identified specific characteristics, which differentiate it from other hepatic cysts, such as the presence of four typical layers: A pseudostratified columnar epithelium layer with interspersed mucus cells, a sub-epithelial connective tissue layer, a smooth muscle layer and an outer fibrous capsule. Friederich[1] initially suggested a congenital origin, but currently it is suspected that the CHFC is a detached hepatic diverticulum or abnormal tracheobronchial bud that may have migrated caudally to be included with the liver during the early embryological development of the foregut. Although, sludge-like bile and viscid mucoid content of the cyst have been described, no communication with the biliary tree could be demonstrated in any reported cases. The imaging appearances of CHFC's are variable and appear as anechoic or hypoechoic cysts with spotty hyperechoic areas on ultrasound. CT findings are of a non-enhancing, rounded lesion of varying density depending on the contents of the cyst, which can include calcium crystals and cholesterol. Typical magnetic resonance imaging features are a hyperintense cyst on T2-weighted images and a variable appearance on T1-weighted images.[5] Pathologically, the cysts are typically solitary and unilocular, and have four layers: an outer fibrous rim, a layer of smooth muscle (often incomplete), subepithelial connective tissue and a lining of ciliated, pseudo-stratified, mucinsecreting columnar epithelium.[6]. Presence of unique histological features indicates CHFC with a reasonable degree of confidence, although a rare morphologic variant of CHFC without smooth muscle layer has reported. Histologically, the differential diagnosis of a hepatic cyst included simple cyst, hydatid cyst, biliary cystadenoma, cystadenocarcinoma and bronchogenic cyst. The main differential diagnosis can be bronchogenic cyst because both cystic lesions share a common embryonic origin. Simple cysts are usually located in the right hepatic lobe and are more prevalent in women. Serologic tumour markers can be confounding, as elevated CA19-9 levels have been found in association with benign CHFC[7]. An aspirate of hepatocytes admixed with ciliated cells and mucus cells distinguish CHFC from other radiologically benign-appearing entities among many of the considered lesions, which are easily differentiated by their typical epithelial lining, cyst. Of concern are reports of CHFC harbouring squamous cell carcinoma (4.4% in reported cases).[8] CHFC was previously thought to be a benign condition. This fact may mandate exploration of all CHFC's diagnosed preoperatively. There is also a single report of portal vein compression secondary to the mass-effect of the CHFC.[9] Until date, the major risk factor associated with diagnosing a CHFC with malignant transformation is size. All the three cases of carcinoma had cystic masses-12 cm in diameter.[10] The recommended treatment of CHFC described in the literature has varied from observation to aspiration to surgical excision However, given the recent cases of CHFC malignant transformation, serial imaging may be required for those patients undergoing cyst sclerosis. Most of the authors agree that CHFCs should be surgically excised for cysts larger than 4 cm to 5 cm, symptomatic or enlarging lesions and asymptomatic lesions with wall abnormalities on imaging or in patients with otherwise unexplained abnormal liver function tests.[10] Until date, there has been no report of a cyst recurrence or metastasis after excision. Several authors have also noted that laparoscopic approach of aspiration and injection of a sclerosing agent can be utilised effectively to stop cyst growth, but the definitive approach is excision of cyst but minimally invasive approach.[11] Treatment options of liver cysts include laparoscopic fenestration, aspiration to formal resection. Laparoscopic approaches have also been validated in the treatment of hepatic cysts. This technique is best suited to lesions in segments II to VI, the anterolateral portion of the liver where visualisation and access are easiest. Lesions located centrally or in the posterior aspects of segments VI, VII, or IVa are less accessible and render laparoscopic therapy more challenging. In general, the patient is positioned in lithotomy, allowing the surgeon to stand between the legs with assistants at the sides. A 30° laparoscope is placed at the umbilicus. Two operating ports surround the umbilicus in a triangulated fashion. A subxiphoid port allows introduction of a fan retractor or suction device. The cyst wall is excised with harmonic scalpel; hemostasis may be obtained with electrocautery. For patients with lesions in segment VII or VIII, positioning and port placement similar to that used for laparoscopic right adrenalectomy may afford improved exposure. Laparoscopic surgery is an ideal modality for benign or marginally dysplastic disease of CHFC. Uncomplicated CHFCs are quite amenable to laparoscopic excision for several reasons. First, the small size and anterior subcapsular location allow for easy access to the cyst with minimal dissection to isolate the lesion. Second, the benign nature of the process allows the cyst to be enucleated from is hepatic bed with little concern for adequate circumferential margins. Third, the CHFC traditionally has a thick cyst wall that permits easy handling with laparoscopic instruments. The subcapsular location and the presence of thick outer fibrous layer in the cyst wall makes it amenable to laparoscopic excision with minimal morbidity.[11] The rarity of CHFC underscores the importance of re-porting individual cases, as illustrated by the case presented here, which may be few reported cases of CHFC presenting with abdominal pain in her early 30 s. It should be noted that although the size and location of the cystic mass were characteristic of CHFC, this patient's cyst demonstrated imaging features that are less common for a CHFC, leading to the decision to excise the cyst. By utilising a minimally invasive approach to excise the CHFC, the patient benefited from an effective ambulatory procedure for the removal of a lesion with risk for malignant transformation[12]. CHFC should be considered as a diagnosis for a superficially located unilocular hepatic cystic mass that presents incidentally or asymptomatically and laparoscopic excision should be considered as a first-line treatment to remove this benign cyst.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Friederich Cyst emit Flimmerepithel in der Leber. Virchows Arch Pathol Anat Physiol Klin Med. 1857;11:446–69. [Google Scholar]
- 2.Wheeler DA, Edmondson HA. Ciliated hepatic foregut cyst. Am J Surg Pathol. 1984;8:467–70. doi: 10.1097/00000478-198406000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan KJ, Escobar M, Alonzo M, Berlin JW. Ciliated hepatic foregut cyst: Report of a case on fine-needle aspiration. Diagn Cytopathol. 2007;35:245–9. doi: 10.1002/dc.20622. [DOI] [PubMed] [Google Scholar]
- 4.Ben Mena N, Zalinski S, Svrcek M, Lewin M, Fléjou JF, Wendum D, et al. Ciliated hepatic foregut cyst with extensive squamous metaplasia: Report of a case. Virchows Arch. 2006;449:730–3. doi: 10.1007/s00428-006-0320-4. [DOI] [PubMed] [Google Scholar]
- 5.Fang SH, Dong DJ, Zhang SZ. Imaging features of ciliated hepatic foregut cyst. World J Gastroenterol. 2005;11:4287–9. doi: 10.3748/wjg.v11.i27.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stringer MD, Jones MO, Woodley H, Wyatt J. Ciliated hepatic foregut cyst. J Pediatr Surg. 2006;41:1180–83. doi: 10.1016/j.jpedsurg.2006.01.068. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan KJ, Escobar M, Alonzo M, Berlin JW. Ciliated hepatic foregut cyst: report of a case on fine-needle aspiration. Diagn Cytopathol. 2007;35:245–49. doi: 10.1002/dc.20622. [DOI] [PubMed] [Google Scholar]
- 8.Furlanetto A, Dei Tos AP. Squamous cell carcinoma arising in a ciliated hepatic foregut cyst. Virchows Arch. 2002;441:296–8. doi: 10.1007/s00428-002-0668-z. [DOI] [PubMed] [Google Scholar]
- 9.Harty MP, Hebra A, Ruchelli ED, Schnaufer L. Ciliated hepatic foregut cyst causing portal hypertension in an adolescent. AJR Am J Roentgenol. 1998;170:688–90. doi: 10.2214/ajr.170.3.9490954. [DOI] [PubMed] [Google Scholar]
- 10.Jakowski JD, Lucas JG, Seth S, Frankel WL. Ciliated hepatic foregut cyst: A rare but increasingly reported liver cyst. Ann Diagn Pathol. 2004;8:342–6. doi: 10.1053/j.anndiagpath.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Goodman MD, Mak GZ, Reynolds JP, Tevar AD, Pritts TA. Laparoscopic excision of a ciliated hepatic foregut cyst. JSLS. 2009;13:96–100. [PMC free article] [PubMed] [Google Scholar]
- 12.Weber T, Sendt W, Scheele J. Laparoscopic unroofing of nonparasitic liver cysts within segments VII and VIII: Technical considerations. J Laparoendosc Adv Surg Tech A. 2004;14:37–42. doi: 10.1089/109264204322862342. [DOI] [PubMed] [Google Scholar]


