Abstract
Objective
Coaction refers to the extent to which taking action on one behavior increases the odds of taking action on a second behavior. This integrative study examines the generalization of coaction in three studies on weight-related behaviors.
Methods
Data from three randomized trials of tailored interventions (n=1277, n=1800, and n=6000) were examined to determine if coaction of behavior change occurred differentially in treatment and control groups. In each analysis, the likelihood of progressing to the Action or Maintenance stages for the target behaviors was evaluated using logistic regression.
Results
Despite differences in populations, targeted behaviors, levels of tailoring in interventions, and timing of follow-up assessments, 17 out of 24 (70.8%) logistic regressions revealed significant coaction in the treatment group as opposed to only 3 out of 24 (12.5%) in the control condition. In 23/24 analyses, coaction of behavior change was larger on an absolute basis in the treatment group. Individuals in the treatment group progressing to Action/Maintenance for one behavior were 1.4 – 5 times more likely to make progress on another behavior compared to those in the treatment group who did not make such progress on the first behavior.
Conclusions
This study demonstrates that despite considerable variability in study design, coaction reliably occurs more in the presence of Transtheoretical-Model based multiple behavior change interventions. Additional studies are needed to replicate these results in other behavioral areas and to examine the predictors of differential coaction. The ability to consistently create coaction within multiple behavior interventions can increase the efficacy and cost-effectiveness of multiple behavior change interventions.
Keywords: multiple behavior interventions, weight management, obesity prevention, Transtheoretical Model, coaction, stage of change
Effective weight management interventions hinge on changing multiple behaviors. The need for multiple behavior change interventions has been highlighted in several studies. Reeves and Rafferty (2005), for example, reported that only 3% of US adults report engaging in regular exercise, non-smoking, being at a healthy weight, and consuming adequate fruit and vegetables. Over 96% of a sample of 434 primary care patients with hypertension or diabetes had 3 or more health behavior risks (Lawler, Winkler, Reeves, Owen, Graves, & Eakin, 2010), which is an all too common finding among overweight primary care patients (Sanchez et al., 2008).
Two recent studies (Appel et al., 2011; Wadden et al., 2011) demonstrate the effectiveness of interventions targeting dietary intake and physical activity among patients recruited from such practices. Appel et al. (2011) reported that two behavioral interventions for obesity comprised of telephonic support and an online weight management program offered with or without in-person support led to significant weight loss among the treatment groups relative to the comparison group who received only brief advice. The Look AHEAD Research Group (2010) examined the effectiveness of a multiple behavior change intervention in over 5100 overweight or obese adults with type 2 diabetes over a four-year period. The intensive lifestyle intervention, which included dietary modification (calorie and fat reduction facilitated by a portion controlled diet) and 175 minutes of physical activity per week, with an emphasis on behavioral strategies such as self-monitoring, goal setting, and problem solving, was compared to standard diabetes education. As expected, the lifestyle intervention led to significant improvements on weight loss, fitness, and a number of clinical outcomes.
While those studies underscore the viability and effectiveness of multiple behavior change interventions, they shed insufficient light on potential mechanisms of multiple behavior change (MBC). Research on maximizing the effect of multiple behavior change MBC interventions is becomingly increasingly common and sophisticated (Prochaska, Spring, & Nigg, 2008) and is a high priority for NIH (NIH, 2010). Numerous studies (e.g., Jones, et al., 2003; Prochaska et al., 2004; 2005; Johnson et al., 2006; Johnson et al., 2008) indicate that the Transtheoretical Model of Behavior Change (TTM) is an effective model for tailoring MBC interventions. The TTM is an integrative model of behavior change that incorporates process oriented variables to explain and predict how and when individuals change behaviors. In addition to the central organizing construct, stage of change, the TTM tailors interventions based on other behavior change constructs including decisional balance, processes of change, and self-efficacy (Prochaska, Redding, & Evers, 2002). Previous research on the generalizable and consistent relationships between TTM constructs, such as stage and decisional balance (Prochaska, 2004; Prochaska et al., 1994; Hall & Rossi, 2008), has informed the development of evidence-based interventions.
Beyond the use of a guiding theoretical model for tailoring interventions, best practices that will allow us to maximize the potential and cost-effectiveness of MBC interventions are only beginning to emerge. Prochaska (2008) identified co-variation, or coaction, of behavior change as a promising innovation for advancing the field. Coaction refers to the finding that taking action on one treated behavior significantly increases the odds of taking effective action on a second treated behavior. Rather than comparing between groups who received treatment or no treatment, assessments of coaction examine the likelihood of success in changing a second targeted behavior once one behavior has been changed within treatment or control groups. Coaction assumes co-occurrence clusters in at-risk individuals at baseline, but focuses on how behaviors within such clusters change together or independently at follow-up. Potential theoretical mechanisms that might contribute to coaction include increased self-efficacy (Bandura, 1974) for one behavior increasing self-efficacy to change another; the Theory of Triadic Influence (Flay & Petraitis, 1994); transfer effects (Lippke, Nigg, & Maddock, 2012); or generalizing principles of behavior change from the Transtheoretical Model.
Research on MBC interventions revealed that adults receiving fully tailored Transtheoretical-Model (TTM)-based interventions for smoking, dietary fat reduction, and sun exposure were 1.63–1.85 times more likely to take action on a second behavior at 24 months if they took action on any one of the treated behaviors. In contrast, individuals in the usual care comparison group were less likely than those in the treatment group to take action on a second behavior if they took action on one (odds ratio (OR) = 1.1–1.2) (Paiva et al., 2012).
While other single studies (e.g., Johnson et al., 2008; Mauriello et al. 2010) have reported that coaction occurs in the context of TTM-based tailored MBC interventions and Paiva et al. (2012) reported coaction among adult samples in studies employing the same intervention protocol, this study represents the first to systematically examine the consistency and magnitude of coaction across three randomized trials involving different populations (i.e., adults, high school students and middle school students); tailoring protocols (i.e., fully tailored interventions for all behaviors and a combination of fully and optimally tailored interventions; different timing); delivery channels (home-based vs. school based); follow-up assessment schedules (i.e., 12–24 months); and target behaviors. Thus, the results will provide unique insights into the stability of coaction. Demonstrating the consistent presence of coaction despite the considerable variability in study designs and targeted populations could inform future studies and interventions and lead to an even greater public health impact of MBC interventions. The results will also permit comparisons of the magnitude of coaction effects on behaviors that are integrated around a theme (energy balance) to behaviors that are considered less related (e.g., smoking and exercise). All three studies addressed one of the leading public health challenges of our time: intervening on multiple behaviors related to weight management in adults or obesity prevention in youth. Each of the three studies addressed two crucial behaviors for obesity prevention or weight management: dietary modification (calorie reduction and dietary fat reduction for the adults; fruit and vegetable intake for the adolescents) and physical activity. The adult weight management study also addressed reducing emotional eating, whereas the adolescent obesity prevention studies included an intervention to reduce TV time.
Methods
Subjects & Procedure
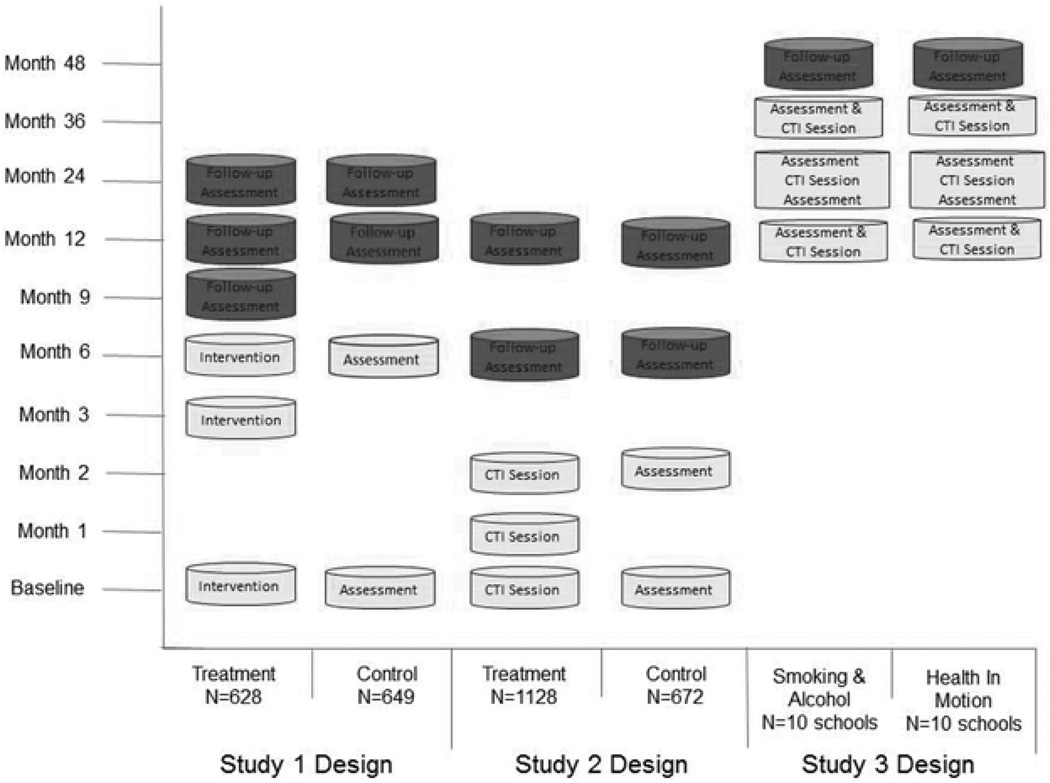
Data from three studies (Johnson et al., 2008; Mauriello et al., 2010; Velicer et al., 2011) are reported here. In Study 1 (Johnson et al., 2008), a national sample of 1277 overweight and obese adults (mean age = 45.37; mean BMI = 30.75; (BMI range = 25–39.9); 48% female; 79.1% White, 6.5% Black, 7% Hispanic, 7.2% Other) were randomized to receive either usual care or fully tailored TTM-based feedback reports for up to three risk behaviors based on the national guidelines at the time: healthy eating (reducing caloric intake by 500 calories per day and total fat intake to less than 30% of calories), regular exercise (30 minutes of moderate exercise on at least 5 days a week), and managing emotions without eating. Fully tailored reports provided feedback on stage of change, decisional balance, self-efficacy, and up to 6 stage matched processes. A participant received a fully tailored report for each of the behaviors for which they were in Precontemplation, Contemplation, Preparation, or Action (i.e., those who were not engaging in regular exercise, healthy eating, and/or managing emotional distress or who had recently adopted the behavior(s) were classified as “at risk” and received an intervention for those behavior(s)). Therefore, they could have received between one and three reports at each timepoint. Intervention materials, including a stage-matched manual addressing the targeted behaviors, were delivered by mail based on assessments at baseline, 3, 6, and 9 months. Control participants completed assessments at baseline and 6 months. Follow-up assessments were conducted with all participants at 12 and 24 months (see Figure 1). Additional details about the participants and design are reported elsewhere (Johnson et al., 2008).
Figure 1.
Study Designs
In Study 2 (Mauriello et al., 2010), 1800 high school students from 8 schools in the US (mean age = 15.97; 50.8% female; 71.5% White, 10.5% Black, 5.5% Hispanic, 12.4% Other; 74.7% normal weight) were randomized to receive either assessment only (baseline and 2 months) or an Internet delivered, TTM-based multiple behavior change obesity prevention program (Health In Motion) targeting exercise (60 minutes on at least 5 days of the week), fruit and vegetable consumption (5 servings daily), and reducing TV time (less than 2 hours per day) at baseline, 1 month, and 2 months. The interventions included a combination of fully tailored interventions for exercise and alternating optimally tailored and stage-matched interventions for fruit and vegetable intake and TV time. Optimally tailored interventions, offered first for fruit and vegetable intake, included feedback on stage of change, decisional balance (pros), and stage-matched feedback on processes of change. Stage-matched interventions included feedback on stage and stage-matched feedback on processes of change. Each student received intervention messages for all three behaviors. As Figure 2 depicts, follow-up assessments were administered to all participants at 6 and 12 months. Additional details about the study have been reported previously (Mauriello et al., 2010).
Study 3 (Velicer et al., in press) included 4,151 middle school students from 20 schools in Rhode Island (mean age = 11.40; 52.3% male; 62.3% White, 3.8% Black, 12.5% Hispanic, 21.4% Other; 88.5% normal weight). The Health in Motion obesity prevention program (described above) was offered to the comparison group of students in an alcohol and smoking prevention study. Students completed annual assessments of stage of change for each behavior and participated in one multi-media intervention session during Year 1, three sessions during Year 2, and one session in Year 3. Students participating in Health In Motion received intervention messages for all three behaviors at each intervention timepoint as is shown in Figure 3. Final follow-up assessment is ongoing. Analyses reported here will be restricted to complete case data from the first two years of the study.
For each study, all procedures were approved by the Institutional Review Board at Pro-Change Behavior Systems, Inc. or the University of Rhode Island.
Statistical Analyses
To determine if coaction of behavior change occurred differentially in treatment and control groups, the likelihood of progressing to Action or Maintenance (A/M) for each pair of target behaviors was evaluated by logistic regression analyses that provided odds ratios (OR) with 95% confidence intervals for each group. Only individuals in a pre-action stage (i.e., Precontemplation, Contemplation, or Preparation) for both behaviors at baseline were included in each logistic regression for each timepoint. In Study 1, for example, coaction was assessed at 6, 12, and 24 months among individuals who at baseline were in a pre-action stage for two behaviors. In all analyses, failing to progress was the referent category. While results are reported in one direction, the converse of each odds ratio is also true. In Study 1, for example, the OR at six months for a participant taking action on healthy eating if they took action on exercise is 2.52 (1.4–4.5), which is equivalent to the OR that a participant taking action on healthy eating would take action on exercise at that timepoint. Thus, the logistic regressions are not comparing individuals in the treatment group to those in the comparison group, but rather comparing within each group the probability of taking action on a second behavior if a participant took action on one behavior.
Results
Tables 1–3 present the results of the logistic regressions for each behavior combination for each of the studies.
Table 1.
Study 1- Coaction Odds Ratios at 6, 12, and 24 months
| Exercise and Healthy Eating | ||
|---|---|---|
| Coactiona Odds Ratio (confidence interval) |
||
| Treatment | Comparison | |
| 6 months | 2.52 (1.4–4.5)* | 1.68 (0.9–3.1) |
| 12 months | 2.63 (1.4–5.0)* | 2.28 (1.3–4.2)* |
| 24 months | 3.91 (2.0–7.5)* | 2.63 (1.4–5.1)* |
| Exercise and Emotional Distress | ||
| Treatment | Comparison | |
| 6 months | 3.56 (1.3–9.4)* | 1.62 (0.6–4.3) |
| 12 months | 2.80 (1.0–7.8)* | 1.24 (0.5–3.1) |
| 24 months | 2.56 (0.9–7.6) | 2.61 (0.9–8.0) |
| Healthy Eating and Emotional Distress | ||
| Treatment | Comparison | |
| 6 months | 3.57 (1.7–7.4)* | 1.4 (0.6–3.2) |
| 12 months | 5.18 (2.3–11.7)* | 2.38 (1.1–5.0)* |
| 24 months | 3.04 (1.3–7.3)* | 1.44 (0.6–3.6) |
p< .05.
Odds of Change on Second Behavior given Change on a First Behavior.
Table 3.
Study 3- Coaction Odds Ratios at 12 and 24 months
| Physical Activity and Nutrition | ||
|---|---|---|
| Coactiona Odds Ratio (confidence interval) |
||
| Treatment | Comparison | |
| 12 months | 2.67 (1.8–3.9)*** | 1.46 (1.0 , 2.2) |
| 24 months | 2.33 (1.5–3.6)*** | 1.61 (0.9 , 3.0) |
| Physical Activity and TV Time | ||
| Treatment | Comparison | |
| 12 months | 1.74 (1.2–2.6)** | 0.88 (0.511 , 1.5) |
| 24 months | 1.81 (1.2–2.7)** | 0.91 (0.525 , 1.6) |
| Nutrition and TV Time | ||
| Treatment | Comparison | |
| 12 months | 1.33 (1.0 , 1.9) | 1.27 (0.8 , 2.1) |
| 24 months | 1.05 (0.7 , 1.6) | 0.80 (0.4 , 1.6) |
p< .01,
p <.001
Odds of Change on Second Behavior given Change on a First Behavior.
Study 1
Receiving fully-tailored interventions for up to three behaviors related to weight management produced odds ratios from 2.52–5.18 that taking action on one behavior would lead to taking action on a second treated behavior. Smaller odds ratios (1.24 to 2.63) emerged among those in the usual care comparison group. Eight out of 9 logistic regressions conducted among those in the treatment group revealed significant co-action, as compared to only 3 out of 9 in the usual care comparison group. On an absolute basis, the ORs for those in the treatment group were higher in 8/9 analyses (see Table 1).
Study 2
Taking action on a single behavior increased the likelihood of taking action on another behavior among participants in the treatment group, but not among those in the comparison group. The ORs were higher among the treatment group than among the comparison group on an absolute basis in all logistic regressions. The ORs for coaction of all behavior pairs were significant at 2 months (end of intervention) and at 6 months among treatment group participants. The OR for coaction of fruit and vegetable intake and physical activity was also significant at 12 months in the treatment group. Those progressing to A/M in the treatment group were 1.4 – 4.2 times more likely to progress to A/M for a second behavior and had significant ORs in 7/9 analyses, while the ORs for coaction in the comparison group were not significant for any behavior pair at any time point (0/9) (see Table 2).
Table 2.
Study 2- Coaction Odds Ratios at 2, 6 & 12 months
| Physical Activity and Nutrition | ||
|---|---|---|
| Coactiona Odds Ratio (confidence interval) |
||
| Treatment | Comparison | |
| 2 months | 4.20 (2.7–6.7)*** | 1.02 (0.3–3.7) |
| 6 months | 3.36 (2.1–5.3)*** | 1.04 (0.4–2.6) |
| 12 months | 2.66 (1.5–4.6)** | 0.80 (0.2–2.9) |
| Physical Activity and TV Time | ||
| Treatment | Comparison | |
| 2 months | 2.60 (1.5–4.4)*** | 0.51 (0.1–1.9) |
| 6 months | 2.08 (1.2–3.5)** | 0.50 (0.2–1.1) |
| 12 months | 1.40 (0.8–2.6) | 0.77 (0.3–1.8) |
| Nutrition and TV Time | ||
| Treatment | Comparison | |
| 2 months | 2.13 (1.3–3.4)** | 0.97 (0.4–2.4) |
| 6 months | 1.99 (1.3–2.2)** | 0.91 (0.4–2.3) |
| 12 months | 1.35 (0.8–2.3) | 0.88 (0.3–2.6) |
p< .01,
p <.001;
Odds of Change on Second Behavior given Change on a First Behavior.
Study 3
At 12 months, the treatment group ORs for moving to action on one behavior if moved on another behavior was higher than those of control group participants for all behavior pairs. The coaction was significant for either behavior paired with exercise, but not for the fruit and vegetable and TV time pairing. Similar results were seen at 24 months. In total, 2 out of 6 analyses revealed significant coaction among treatment group participants, as opposed to 0/6 for comparison group participants. As Table 3 outlines, in 6 out of 6 analyses, the treatment group had higher OR on an absolute basis.
Across all three studies, the odds of taking action on one behavior after having taken on another behavior were higher for treatment group participants receiving tailored interventions in 23 out of 24 analyses. Significant co-action occurred in 17 out of 24 of the analyses among treatment group participants as opposed to 3 out of 24 analyses for the comparison group participants.
Discussion
Few previous studies have documented the effect changing one behavior can have on the potential to change another. In this study, coaction was consistently demonstrated across three studies intervening on a range of energy balance behaviors that involved diverse populations (overweight adults, high school students, and middle school students ) and conducted follow-ups as far out as 24 months. Clear commonalities regarding coaction included significant ORs for the likelihood of treatment group participants moving to A/M for one behavior when they progressed to A/M on a behavior in 17 out of 24 analyses, as opposed to only 3 out of 24 analyses for comparison group participants.
The consistency with which coaction occurred offers exciting innovations for MBC research because of the potential for coaction to increase treatment impact and reduce response burden and costs of MBC interventions. This increased impact does not, however, have to increase demand or cost exponentially in that the results in Studies 2 and 3 indicated that briefer optimally tailored or stage-matched interventions resulted in coaction when paired with fully tailored interventions. In other words, coaction occurs in the context of fully tailored interventions for all behaviors (Study 1), as well as when fully tailored interventions are paired with optimally or minimally tailored materials (Studies 2 & 3). Thus, the results have implications for beginning to establish best practices in MBC interventions. Given that various intensities of tailoring (full tailoring in the adult weight study and a combination of full, optimal, and minimal tailoring in the high school and middle school obesity prevention studies) produced consistently higher ORs in the treatment group than in the comparison group, tailoring on relevant behavior change variables may be a minimum requirement for successful MBC interventions. Noar, Benac & Harris (2007) reported that tailoring on 5–7 variables in TTM-based interventions is as effective as tailoring on 6–9 behavior change constructs, lending further support to an optimal tailoring approach. Future research needs to explore what the most efficacious combinations of tailored interventions are.
Various explanations for the consistent demonstration of coaction have been suggested (Noar, Chabot, & Zimmerman, 2008; Fleig, Lippke, Pomp, & Schwarzer, 2011; Lippke, Nigg & Maddock, 2012). One such explanation hypothesizes that individuals have increased self-efficacy as a result of changing one behavior that spills over onto another behavior. Fleig et al. (2011) reported that transfer effects offer another plausible explanation. Transfer refers to the process when lessons learned in one context are applied to another context (Barnett & Ceci, 2002)—or in this case, the extent to which knowledge and skills from one behavior change assists with another (Nigg, Lee, Hubbard, & Min-Sun, 2009; Barnett & Ceci, 2002). Transfer might be attributable in part to the habituation of one behavior freeing up self-regulatory resources to work on another behavior (Fleig et al., 2011). The consistently smaller odds ratios in the usual care comparison groups, however, indicate that successfully adopting one behavior does not have the same effect as adopting a behavior in the context of receiving tailored behavior change interventions. If increased self-efficacy or straightforward transfer effects were responsible for the coaction, coaction would not be consistently higher among treatment group participants: In that case, individuals in the control groups would demonstrate the same transfer effect. Individualized MBC interventions tailored to TTM constructs may have a unique potential to create synergistic effects on behavior change in part because they are teaching participants principles of behavior change that can be generalized across behaviors (Noar et al., 2008), such as increasing the awareness of the benefits of changing in Precontemplation, reducing barriers in Contemplation, and increasing use of stimulus control and counter-conditioning in Action. It is yet to be determined if other types of MBC interventions (e.g., interventions guided by other theoretical frameworks) would produce similar levels of coaction.
This study is limited to a review of three studies related to energy balance behaviors. Additional research is needed to further explore the consistency and magnitude of coaction in studies targeting additional behaviors and behaviors that are not as clearly linked by a specific over-arching theme, such as weight management. The potential for coaction among smoking and other behaviors is of particular interest given that smokers are more likely to engage in other unhealthy behaviors (Paiva et al., 2012; Chiolero, Wietlisbach, Ruffieux, Paccaud, & Cornuz, 2006; Fine, Philogene, Gramling, Coups, & Sinha, 2004; Berrigan et al., 2003).
While in other contexts variability in study designs, target populations, intervention tailoring and delivery protocols, and target behaviors (weight loss versus obesity prevention) could be viewed as a drawback, it is a strength of this study. The consistency and generalizability of coaction in varying study designs highlights the robustness of this finding. It also underscores the need to more systematically investigate the circumstances under which coaction occurs to inform future MBC interventions.
In summary, this study demonstrates that coaction is a reliable phenomenon in the context of tailored, theoretically driven MBC interventions related to weight management and obesity prevention. In the interest of cost-effectiveness, ease of dissemination, and maximizing effectiveness, future research on multiple behavior interventions should examine potential predictors of coaction; what level and combinations of tailoring will produce the optimal balance between response burden and outcomes; and whether similar effects can be obtained when targeting more diverse combinations of behaviors. An increased understanding of how to maximize coaction to facilitate MBC can inform future intervention development in several areas. MBC interventions targeting energy balance behaviors are particularly crucial given that the prevalence of obesity is 35.7% and the combined prevalence of overweight and obesity is 68.8%. Though the previous dramatic increases in prevalence have leveled off in recent years, these epidemic rates show no evidence of decline (Flegal, Carroll, Kit, & Ogden, 2012). Evidence-based MBC interventions that produce coaction could well be one component of effective treatments to address those all too common conditions.
Acknowledgments
This research was supported by Grant Numbers R44 HL070549 and R44 HL074482 from the National Heart, Lung, and Blood Institute and Grant Number R01DA020112 from the National Institute on Drug Abuse. The authors affiliated with Pro-Change Behavior Systems, Inc. are employees of said company, which is currently licensing the programs described herein. Janice Prochaska, Ph.D. is the company’s President and CEO.
Contributor Information
Sara S. Johnson, Pro-Change Behavior Systems, Inc.
Andrea L. Paiva, Cancer Prevention Research Center, University of Rhode Island
Leanne Mauriello, Pro-Change Behavior Systems, Inc.
James O. Prochaska, Cancer Prevention Research Center, University of Rhode Island
Colleen A. Redding, Cancer Prevention Research Center, University of Rhode Island
Wayne F. Velicer, Cancer Prevention Research Center, University of Rhode Island
References
- Appel LJ, Clart JM, Yeh HC, Wang N, Coughlin JW, Daumit G, Brancati FL. Comparative effectiveness of weight-loss interventions in clinical practice. New England Journal of Medicine. 2011;365(21):1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett SM, Ceci SJ. When and where do we apply what we learn? A taxonomy for far transfer. Psychological Bulletin. 2002;128:612–637. doi: 10.1037/0033-2909.128.4.612. [DOI] [PubMed] [Google Scholar]
- Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Preventive Medicine. 2003;36:615–623. doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- Chiolero A, Wietlisbach V, Ruffieux, Paccaud C, Cornuz F. Clustering of risk behaviors with cigarette consumption: A population-based survey. Preventive Medicine. 2006;42:348–353. doi: 10.1016/j.ypmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. American Journal of Preventive Medicine. 2004;27(Suppl. 2):18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among U.S. adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Fleig L, Lippke S, Pomp S, Schwarzer R. Intervention Effects of Exercise Self-regulation on Physical Exercise and Eating Fruits and Vegetables: A Longitudinal Study in Orthopedic and Cardiac Rehabilitation. Preventive Medicine. 2011;53(3):182–187. doi: 10.1016/j.ypmed.2011.06.019. [DOI] [PubMed] [Google Scholar]
- Hall KL, Rossi JS. Meta-analytic examination of the strong and weak principles across 48 health behaviors. Preventive Medicine. 2008;46:266–274. doi: 10.1016/j.ypmed.2007.11.006. [DOI] [PubMed] [Google Scholar]
- Johnson SS, Driskell MM, Johnson J, Dyment S, Prochaska JO, Prochaska JM, Bourne L. Transtheoretical model intervention for adherence to lipid-lowering drugs. Disease Management. 2006;9:102–114. doi: 10.1089/dis.2006.9.102. [DOI] [PubMed] [Google Scholar]
- Johnson SS, Paiva AL, Cummins CO, Johnson JL, Dyment S, Wright JA, Sherman K. Transtheoretical Model-basedmultiple behavior intervention for weight management: Effectiveness on a population basis. Preventive Medicine. 2008;46:238–246. doi: 10.1016/j.ypmed.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones H, Edwards L, Vallis TM, Ruggiero L, Rossi SR, Rossi JS, Zinman B. Changes in diabetes self-care behaviors make a difference in glycemic control: the diabetes stages of change (DISC) study. Diabetes Care. 2003;26(3):732–737. doi: 10.2337/diacare.26.3.732. [DOI] [PubMed] [Google Scholar]
- Lawler S, Winkler W, Reeves M, Owen N, Graves N, Eakin E. Multiple Health Behavior Changes and Co-variation in a Telephone Counseling Trial. Annals of Behavioral Medicine. 2010;39:250–257. doi: 10.1007/s12160-010-9188-2. [DOI] [PubMed] [Google Scholar]
- Lippke S, Nigg C, Maddock J. Health-promoting and health-risk behaviors: Theory-driven analyses of multiple health behavior change in three international samples. International Journal of Behavioral Medicine. 2012;19(1):1–13. doi: 10.1007/s12529-010-9135-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauriello LM, Ciavatta MM, Paiva AL, Sherman KJ, Castle PH, Johnson JL, Prochaska JM. Results of a multi-media multiple behavior obesity prevention program for adolescents. Preventive Medicine. 2010;51:451–456. doi: 10.1016/j.ypmed.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Health. Common Fund Makes New FY2010 Awards to Advance the Science of Behavior Change. 2010 Retrieved from: http://nihroadmap.nih.gov/behaviorchange/
- Nigg CR, Lee H, Hubbard AE, Min-Sun K. Gateway Health Behaviors in College Students: Investigating Transfer and Compensation Effects. Journal of American College Health. 2009;58:39–44. doi: 10.3200/JACH.58.1.39-44. [DOI] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Noar SM, Chabot M, Zimmerman RS. Applying health behavior theory to multiple behavior change: Considerations and approaches. Preventive Medicine. 2008;46:275–280. doi: 10.1016/j.ypmed.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Paiva AL, Prochaska JO, Yin H, Redding CA, Rossi JS, Blissmer B, Horiuchi S. Treated individuals who progress to action or maintenance for one behavior are more likely to make similar progress on another behavior: Coaction results of a pooled data analysis of three trials. Preventive Medicine. 2012;54(5):331–334. doi: 10.1016/j.ypmed.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska J, Spring B, Nigg C. Multiple health behavior change research: an introduction and overview. Preventive Medicine. 2008;46(3):181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO. Multiple health behavior research represents the future of preventive medicine. Preventive Medicine. 2008;46:281–285. doi: 10.1016/j.ypmed.2008.01.015. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Rossi JS, Redding CA, Greene GW, Rossi SR, Plummer BA. Multiple risk expert systems interventions: impact of simultaneous stage-matched expert system interventions for smoking, high-fat diet, and sun exposure in a population of parents. Health Psychology. 2004;23:503–516. doi: 10.1037/0278-6133.23.5.503. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Redding CA, Rossi JS, Goldstein M, DePue J, Sun X. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Preventive Medicine. 2005;41:406–416. doi: 10.1016/j.ypmed.2004.09.050. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Redding CA, Evers K. Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education: Theory, Research, and Practice. 3rd edition. San Francisco, CA: Jossey-Bass, Inc.; 2002. The transtheoretical model and stages of change. Chapter 5; pp. 99–120. [Google Scholar]
- Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, Rossi SR. Stages of change and decisional balance for 12 problem behaviors. Health Psychology. 1994;13:39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Reeves MJ, Rafferty AP. Healthy Lifestyle Characteristics Among Adults in the United States, 2000. Archives of Internal Medicine. 2005;165:854–857. doi: 10.1001/archinte.165.8.854. [DOI] [PubMed] [Google Scholar]
- Sanchez A, Norman GJ, Sallis JF, Calfas KJ, Rock C, Patrick K. Preventive Medicine. 2008;46:196–202. doi: 10.1016/j.ypmed.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF, Redding CA, Paiva AL, Mauriello L, Blissmer B, Oatley K, Fernandez AC. Multiple risk factor intervention to prevent substance abuse and increase energy balance behaviors in middle school students. Translational Behavioral Medicine. doi: 10.1007/s13142-013-0197-0. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI, Moore RH. A two-year randomized trial of obesity treatment in primary care practice. New England Journal of Medicine. 2011;365(21):1969–1979. doi: 10.1056/NEJMoa1109220. [DOI] [PMC free article] [PubMed] [Google Scholar]