Abstract
Aggressive angiomyxoma (AA) is a rare, slow-growing mesenchymal neoplasm of vulvo-perineal region. Although AA is common in females of reproductive age, only a few cases during pregnancy have been documented in the English literature. It carries a high risk of local recurrence but rarely metastasizes. The high recurrence rate can partially be due to inadequate excision, which may be due to an incorrect preoperative diagnosis. We present a case of 25-year-old pregnant female presenting with a painless and soft mass attached to left labia majora by a stalk. This mass was clinically thought to be a lipoma. It was completely excised and was diagnosed as AA on histopathology. Gynecologists should consider the diagnosis of AA when a young female especially during her pregnancy presents with a vulvo-perineal mass. Incorrect diagnosis may lead to incomplete excision and recurrence.
Key words: aggressive angiomyxoma, pregnancy, vulva, mesenchymal neoplasm, lipoma
Introduction
Aggressive angiomyxoma (AA) is a rare, locally aggressive mesenchymal neoplasm that commonly involves the vulvo-perineal region of females in reproductive age.1 AA commonly presents as a painless, gelatinous soft mass of varying size. It carries a high risk of local recurrence and can rarely metastasize.2,3 The high recurrence rate may partially be due to inadequate excision, which may be due to an incorrect preoperative diagnosis.2 There are only a few cases reported in English literature about its association with pregnancy. We, hereby, report a rare case of AA of vulva in pregnant woman, which was earlier misdiagnosed as lipoma.
Case Report
A 25-year-old, gravida 3, para 2, pregnant woman, presented with a painless mass over left labia majora since 3 months. The patient’s history revealed menarche at the age of twelve years with regular menstrual cycle of 3-4 days duration having an average flow. Her family and past history was not significant. Local examination revealed a non-tender, pedunculated mass measuring 8×6×5 cm, attached to left labia majora by a 2.5 cm long stalk. Ultrasound abdomen showed single live fetus with gestation age of 18 weeks 4 days. The mass was clinically presumed to be lipoma and was completely excised under caudal block and was sent for histopathological examination.
Pathological findings
On gross examination of the specimen, skin covered oval pedunculated mass measuring 8×6×5 cm in size, with the stalk measuring 2.5 cm in length and 2 cm in diameter was identified (Figure 1A). The cut surface was solid, gray-white, glistening, and soft in consistency with no areas of necrosis and hemorrhage (Figure 1B).
Figure 1.

A) Skin covered soft mass with a short stalk; B) Mass showing solid, grey-white glistening and myxoid cut surface.
Microscopic examination revealed a non-encapsulated but relatively well-circumscribed, hypocellular neoplasm composed of widely dispersed, uniform population of spindle to stellate cells with round to oval bland nuclei in abundant loose myxoid matrix. The blood vessels of variable caliber were seen throughout the tumor (Figure 2). No cellular pleomorphism, mitosis or necrosis was observed. Resection margin was free of tumor. Based on histopathological findings, final diagnosis of an aggressive angiomyxoma of vulva was made.
Figure 2.
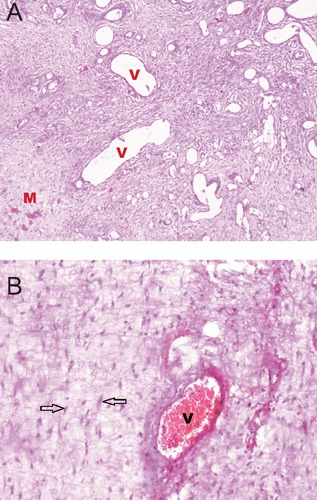
A) Spindle to stellate cells in loose myxoid matrix (labeled as M) with variable sized blood vessels (labeled as V) (Hematoxylin & Eosin, 40×); B) Spindle to stellate cells (denoted by arrows) with round to oval bland nuclei and indistinct cytoplasmic borders with blood vessel (labeled as V) (Hematoxylin & Eosin, 100×).
Discussion
AA is a rare, slow-growing and distinctive myxoid neoplasm which occurs almost exclusively in the pelvic-perineal region of pre-menopausal women, but has occasionally also been reported in men.1 AA commonly occurs in the reproductive age group, but can be seen over a wide age range from 16 to 70 years.4
Vulva is the most common site of involvement; however its occurrence in vagina, retroperitoneum, buttock, urinary bladder in females and scrotum, epididymis, testis, spermatic cord, inguinal region and bladder in males has also been documented in the literature.4 AA commonly presents as painless, gelatinous soft mass clinically simulating Bartholin cyst, Gartner duct cyst, vaginal polyp, vaginal cyst, vaginal prolapse, abscess, pelvic floor hernia, fibromatosis, lipoma (as in our case) and other soft tissue neoplasm.5,6 On CT scan, AA has a well-defined margin with attenuation less than that of the muscles. On MRI, AA shows high signal intensity on T2 weighted images. The attenuation on CT-scan and high signal intensity on MRI are likely to be related to the loose myxoid matrix and high water content of AA.7 On gross examination, AA usually appears as lobulated, soft to rubbery, solid and poorly demarcated mass of varying size, measuring between 3 and 60 cm. The cut surface has a glistening smooth homogenous gray-white appearance with or without areas of necrosis and hemorrhage. Microscopically, AA is usually hypocellular to moderately cellular with abundant myxoid matrix. The tumor consists of bland stellate and spindle cells with round or ovoid nuclei and pale eosinophilic cytoplasm with thin cytoplasmic processes. Clusters of thick blood vessels of various calibers are characteristically present. AA must be distinguished from the more common benign and malignant myxoid tumors including myxoma, myxoid liposarcoma, myxoid variant of malignant fibrous histiocytoma and other soft tissue tumors with myxoid changes.8
The term aggressive emphasizes the tumor’s infiltrative nature and its association with local recurrence in about 30-72% cases in spite of wide local excision.5 Usually AA does not metastasize but there are 3 reports of AA with metastases in literature.3 So, AA should be kept in category of neoplasm with borderline or intermediate malignancy.3
The neoplastic cells of AA exhibit fibroblastic and myofibroblastic features and appear to be hormonally influenced. Most of the tumor cells are positive for smooth muscle actin, desmin, estrogen receptor (ER), and progesterone receptor (PR).9 There are only few cases reported about its coexistence with pregnancy as in our case.1,2,9-11 The presence of ER and PR in AA and its enlargement or recurrence in pregnancy suggests the possibility of hormone dependence of this neoplasm.10 Recurrence may occur during the ongoing pregnancy or during subsequent pregnancy.1 Our patient delivered normally at term and was followed up for 9 months after surgery. There is no evidence of recurrence till date.
Surgery with wide excision is the first line of treatment in both pregnant and non-pregnant patients, although, in few studies wide excision does not lead to a significant lower recurrence rate of AA as compared to incomplete resection.1,5 Some adjuvant treatments such as hormonal therapy with tamoxifen, raloxifene and gonadotrophin releasing hormone agonists have been used for primary treatment in cases where an extensive surgical procedure will lead to great morbidity and for treatment against tumor recurrence. However, these hormonal therapies are not recommended for pregnant patients. Radiotherapy and chemotherapy are considered less suitable options due to low mitotic activity of the tumor. Pre-operative angiographic embolization may help in resection by shrinking the tumor and making it easily identifiable from surrounding normal tissue.12 However, recurrences after embolization may also occur as the tumor might derive its blood supply from multiple sources rather than a single source.13 Despite high recurrence rate, the prognosis for patients with AA is generally considered good. Long-term follow-up and careful monitoring with imaging techniques like MRI are essential for timely identification of recurrence and repeat resection or hormonal therapy or embolization may be considered in case of recurrence.2
Conclusions
The condition of our patient together with review of previous articles reveals that AA should be kept in mind when a painless, soft slow-growing vulvar mass is detected in young female especially during pregnancy. Wide local excision with long term follow-up is necessary due to high rate of local recurrence.
References
- 1.Han-Geurts IJ, van Geel AN, van Doorn L, et al. Aggressive angiomyxoma: multi-modality treatments can avoid mutilating surgery. Eur J Surg Oncol 2006;32:1217–21 [DOI] [PubMed] [Google Scholar]
- 2.Bagga R, Keepanasseril A, Suri V, et al. Aggressive angiomyxoma of the vulva in pregnancy: a case report and review of management options. Med Gen Med 2007;9:16. [PMC free article] [PubMed] [Google Scholar]
- 3.Geng J, Cao B, Wang L.Aggressive angiomyxoma: an unusual presentation. Korean J Radiol 2012;13:90–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magtibay PM, Salmon Z, Keeney GL, et al. Aggressive angiomyxoma of the female pelvis and perineum: a case series. Int J Gynecol Cancer 2006;16:396–401 [DOI] [PubMed] [Google Scholar]
- 5.Sutton BJ, Laudadio J.Aggressive angiomyxoma. Arch Pathol Lab Med 2012;136:217–21 [DOI] [PubMed] [Google Scholar]
- 6.Gungor T, Zengeroglu S, Kaleli A, et al. Aggressive angiomyxoma of the vulva and vagina. a common problem: misdiagnosis. Eur J Obstet Gynecol Reprod Biol 2004;112:114–6 [DOI] [PubMed] [Google Scholar]
- 7.Outwater EK, Marchetto BE, Wagner BJ, et al. Aggressive angiomyxoma: findings on CT and MR imaging. AJR Am J Roentgenol 1999;172:435–8 [DOI] [PubMed] [Google Scholar]
- 8.Metin A, Nese CD, Nagihan C, et al. Aggressive angiomyxoma of the vulva: a case report and review of the literature. Aegean Pathol J 2006;3:1–4 [Google Scholar]
- 9.Ghose S, Maurya DK, Narasimhan R, et al. Bilateral aggressive angiomyxoma in pregnancy. J Evol Med Dent Sci 2013;2:52–4 [Google Scholar]
- 10.Danesh A, Sanei MH. Aggressive angiomyxoma of the vulva: dramatic response to gonadotropin-releasing hormone agonist therapy. JRMS 2007;12:217–21 [DOI] [PubMed] [Google Scholar]
- 11.Mandal S, Dhingra K, Roy S, et al. Aggressive angiomyxoma of the vulva presenting as a pedunculated swelling. Indian J Pathol Microbiol 2008;51:259–60 [DOI] [PubMed] [Google Scholar]
- 12.Han-Geurts IJ, van Geel AN, van Doorn L, et al. Aggressive angiomyxoma: multi-modality treatments can avoid mutilating surgery. Eur J Surg Oncol 2006;32:1217–21 [DOI] [PubMed] [Google Scholar]
- 13.Chan IM, Hon E.Aggressive angiomyxoma in females: is radical resection the only option? Acta Obstet Gynecol Scand 2000;79:216–20 [PubMed] [Google Scholar]


