Abstract
Ansa cervicalis (AC) frequently shows its variations in the formation and distribution pattern. However, variation in its looping pattern associated with abnormal topographic disposition is relatively rare. Knowledge on the possible deviations in the looping pattern is clinically important, to avoid iatrogenic injuries in surgical procedures. We report here a concurrent rare case of double looped AC located deep to internal jugular vein. Anatomy of its superior root was normal, but the usual appearance of inferior root had gone astray due to formation of double loop. AC is being popularly used for nerve reconstructive surgery in treating paralyzed larynx, tongue hemiatrophy. Anatomical variation of it may potentially jeopardize the surgical procedures. Therefore, it is essential to the surgeons to be familiar with its unusual variations.
Keywords: Ansa cervicalis, Double loop, Nerve muscle transplant, Variation
Introduction
Ansa cervicalis (AC) is a loop of nerves formed in the side of the neck by the union of superior and inferior roots and lies in carotid sheath. Superior root (SR) arises from the hypoglossal nerve (HN), in the carotid triangle. It carries C1 nerve fibers and descends on the internal and common carotid arteries (CCAs). On the other hand, inferior root arises from the union of ventral rami of C2 and C3 spinal nerves behind the internal jugular vein (IJV). It curves forward on the lateral surface of IJV, passes downwards on the CCA. Little below the middle of the neck, it joins SR (ansa hypoglossi) to form the AC. AC supplies all the infrahyoid muscles except thyrohyoid.[1,2]
The AC nerve formation is relatively complex, as its course and location along the great vessels of the neck often vary. Because of its closeness with the major vessels and nerves of the neck, any variation in its morphology is of great clinical and surgical importance. AC often shows the great degree of variation in its origin and distribution. Studies have reported the multiple prevalence of presence of its superior and inferior roots.[3,4] When compared to diverse origin among the roots, inferior root being most popular to present variant origin. This has been documented in standard anatomy text books.[2] AC with double loop (DL) associated with its deep location in the carotid triangle of the neck is a rare phenomenon and it is hardly ever reported.
Case Report
During routine cadaveric dissection of anterior triangles of the neck for the medical undergraduate students, we observed a concurrent variation in the morphology and topographic disposition of the AC. The classical form of AC was lacking in the right side of the neck of a male cadaver aged about 55 years. Variant AC existing to be double looped and both loops were hidden by IJV [Figure 1]. SR of the AC arose from the C1 nerve and travelled through the HN as usual. It joined the C2 fibers by forming a distinct loop beneath the IJV [Figure 2]. Single nerve trunk about 1.5 cm long emerged from this loop and descended downwards. It joined C3 nerve in the looped manner under cover of IJV. Due to this, the normal appearance of inferior root had gone astray. A solid elongated branch incorporating fibers of C1-C3 nerves arose from this loop and ran obliquely downwards superficial to CCA and branched out to supply the infrahyoid muscles.
Figure 1.
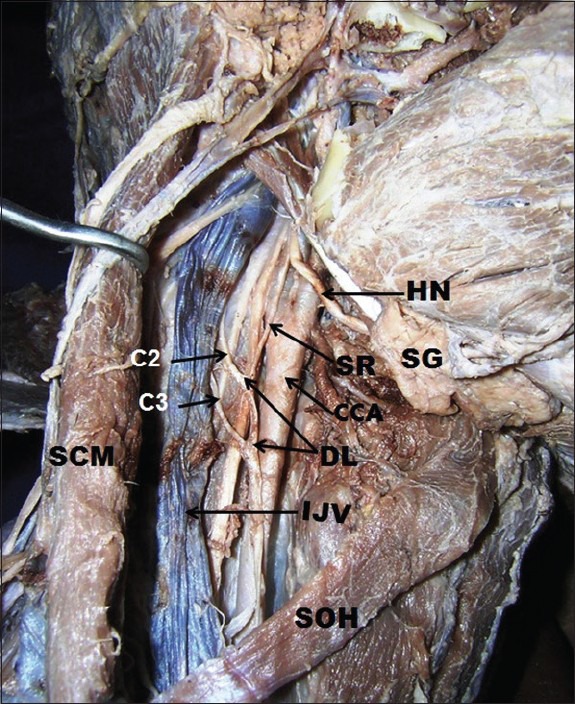
Dissection of carotid triangle to show double looped ansa cervicalis associated with its deep topographical disposition beneath internal jugular vein. HN: Hypoglossal nerve, SG: Submandibular gland, CCA: Common carotid artery, SR: Superior root of ansa cervicalis, SCM: Sternocleidomastoid muscle (retracted backwards), SOH: Superior belly of omohyoid muscle, C2, C3: Second and third cervical nerves, respectively
Figure 2.
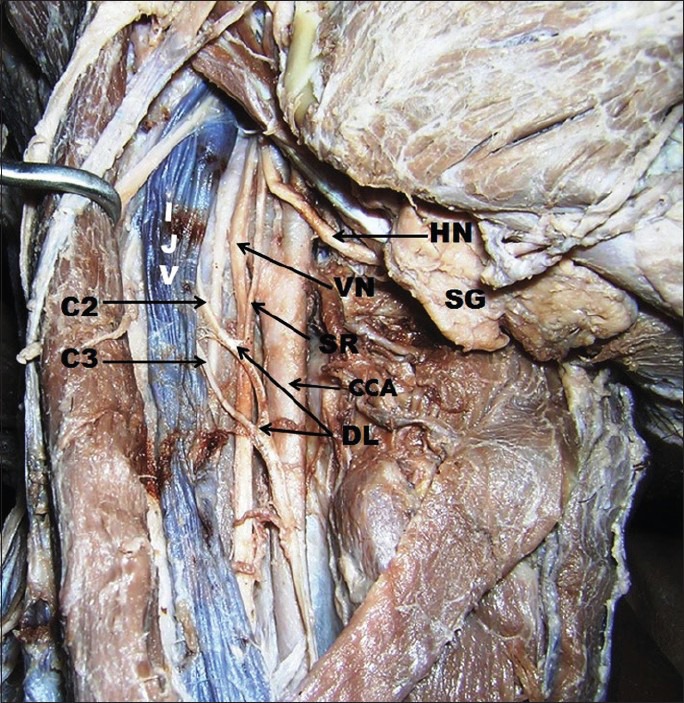
Closer view of variant ansa cervicalis associated with double loop. IJV: Internal jugular vein, HN: Hypoglossal nerve, SR: Superior root, VN: Vagus nerve, CCA: Common carotid artery, C2, C3: Second and third cervical nerves, respectively, SG: Submandibular gland
Discussion
The anatomic course and morphology of the AC are intricate by its variable course and branching pattern. Many reports support the fact that, AC known to show its variations in the origin of its roots and eventual pattern of distribution. However, variations in its morphology and topographical dispositions are seldom reported.
AC is gaining much popularity in nerve muscle transplantation approach in the treatment of paralyzed larynx resulted by the resection of recurrent laryngeal nerve.[4,5] As AC lies very close to the larynx, its usage generally does not cause any functional or cosmetic penalty.[6,7] Crumley et al. have recommended the AC branch to the sternothyroid because this branch is located very near to the recurrent laryngeal nerve.[8] In addition to this, the AC is also useful in the treatment of hemiatrophy of tongue after facial-hypoglossal anastomosis.[9,10]
Mwachaka et al. have studied discrepancies in the SR of the AC between right and left sides. They reported that the prevalence of presence of SR was 100% on right side and 97% on left side, while inferior root was present in 89.5% on right side and 81.6% on left side of the neck. Nearly 56% of cases SR was lying superior to posterior belly of digastric muscle and in 81.5% cases the inferior root was located lateral to IJV.[3]
Loukas reported the origin of SR above the digastric muscle in 92% cases. In the same study, the prevalence of origin of inferior root from C2, C3 was found to be 38%, from C2, C3, C4 in 10%, only from C3 and C2 was 40% and 12%, respectively. Incidence of inferior root lying posterolateral to IJV was 74% and anteromedial to it was 26%.[4]
SR of AC contributed by HNs and vagus nerves (VNs) was reported.[11,12] SR solely formed by the vagus without any contribution from HN was reported by Antony and Biswabina.[13] Absence of inferior root of AC was reported by Babu.[14] Study conducted by Antony and Biswabina reported the cases with total absence of AC. In this situation, the strap muscles were supplied by the VN.[13]
Morphological study done by Ahmed reported four types of looping pattern of the AC. Type 1 with U shaped loop was accounted for 84% of prevalence. Type 2 with Y shaped loop present in 8% of cases; double and fused Y shaped loop were categorized as type 3 with the prevalence of 4% and double and separated Y shaped loop has been classified as type 4 and its incidence was reported to be 4%.[15] Present case falls under type 4 category of loop. However, the concurrent variations presenting DL and the deep course of the AC are rarest among all its variations and reports on such variations are not available in any of the literature at our best of knowledge. Variations in the pattern of distribution associated with unusual branching pattern was also documented by the investigators.[15,16]
Knowledge on the variant form of AC does not only helps in preventing iatrogenic injuries during procedures of thyroplasty, arytenoid adduction, and teflon injection[11] but also aid during operations in the neck, so as to circumvent injuring the great vessels that are intimately related to it.[3]
Conclusion
Awareness of coexistence of variations of AC in its morphological and topographical position as reported here unquestionably helps the surgeons in avoidance of unintentional injury during surgical procedures of the neck specifically during nerve reconstructive surgery.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Romanes GJ. Cunningham's Manual of Practical Anatomy. 15th ed. Vol. 3. New York: Oxford Medical Publication; 1986. Head and neck and brain; pp. 41–3. [Google Scholar]
- 2.Standring S. 39th ed. Edinburgh: Churchill Livingstone Elsevier; 2005. Gray's Anatomy: The Anatomical Basis of Clinical Practice; pp. 532–5593. [Google Scholar]
- 3.Mwachaka PM, Ranketi SS, Elbusaidy H, Ogeng’o J. Variations in the anatomy of ansa cervicalis. Folia Morphol (Warsz) 2010;69:160–3. [PubMed] [Google Scholar]
- 4.Loukas M, Thorsell A, Tubbs RS, Kapos T, Louis RG, Jr, Vulis M, et al. The ansa cervicalis revisited. Folia Morphol (Warsz) 2007;66:120–5. [PubMed] [Google Scholar]
- 5.Chhetri DK, Berke GS. Ansa cervicalis nerve: Review of the topographic anatomy and morphology. Laryngoscope. 1997;107:1366–72. doi: 10.1097/00005537-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Vacher C, Caix P. Anatomy of the hypoglossal nerve and the hypoglossal ansa cervicalis. Rev Stomatol Chir Maxillofac. 2004;105:160–4. doi: 10.1016/s0035-1768(04)72296-2. [DOI] [PubMed] [Google Scholar]
- 7.Natsugoe S, Okumura H, Matsumoto M, Ishigami S, Owaki T, Nakano S, et al. Reconstruction of recurrent laryngeal nerve with involvement by metastatic node in esophageal cancer. Ann Thorac Surg. 2005;79:1886–9. doi: 10.1016/j.athoracsur.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 8.Crumley RL, Izdebski K, McMicken B. Nerve transfer versus Teflon injection for vocal cord paralysis: A comparison. Laryngoscope. 1988;98:1200–4. doi: 10.1288/00005537-198811000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Kukwa A, Marchel A, Pietniczka M, Rakowicz M, Krajewski R. Reanimation of the face after facial nerve palsy resulting from resection of a cerebellopontine angle tumour. Br J Neurosurg. 1994;8:327–32. doi: 10.3109/02688699409029621. [DOI] [PubMed] [Google Scholar]
- 10.Laurentjoye M, Ricard AS, Caix P, Siberchicot F, Majoufre-Lefebvre C. Tongue reconstruction with a bilateral infrahyoid flap innervated by Ansa Cervicalis after total glossectomy. Rev Stomatol Chir Maxillofac. 2011;112:337–41. doi: 10.1016/j.stomax.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Jyothi SR, Dakshayani KR. Variation in the formation of ansa cervicalis on right side. Anat Karnataka. 2013;7:81–3. [Google Scholar]
- 12.Ranajna V, Srijit D, Rajesh S. Unusual organization of the ansa cervicalis-A case report. Braz J Morphol Sci. 2005;22:175–7. [Google Scholar]
- 13.Antony SD, Biswabina R. Study of the formation and distribution of the ansa cervicalis and its clinical significance. Eur J Anat. 2010;14:143–8. [Google Scholar]
- 14.Babu PB. Variant inferior root of ansa cervicalis. Int J Morphol. 2011;29:240–3. [Google Scholar]
- 15.Ahmed MS. Anatomical study of the human ansa cervicalis nerve and its variations. Int J Anat Physiol. 2013;2:014–9. [Google Scholar]
- 16.Koizumi M, Horiguchi M, Sekiya S, Isogai S, Nakano M. A case of the human sternocleidomastoid muscle additionally innervated by the hypoglossal nerve. Okajimas Folia Anat Jpn. 1993;69:361–7. doi: 10.2535/ofaj1936.69.6_361. [DOI] [PubMed] [Google Scholar]


