Abstract
Self-Determination Theory (SDT) provides a model for understanding motivation deficits in schizophrenia, and recent research has focused on problems with intrinsic motivation. However, SDT emphasizes that motivated behavior results from three different factors: intrinsic motivators (facilitated by needs for autonomy, competency, and relatedness), extrinsic motivators (towards reward or away from punishment), or when intrinsic and extrinsic motivators are absent or thwarted a disconnect/disengagement occurs resulting in behavior driven by boredom or ‘passing time’. Using a novel approach to Ecological Momentary Assessment, we assessed the degree to which people with schizophrenia were motivated by these factors relative to healthy control participants. Forty-seven people with and 41 people without schizophrenia were provided with cell phones and were called four times a day for one week. On each call participants were asked about their goals, and about the most important reason motivating each goal. All responses were coded by independent raters (blind to group and hypotheses) on all SDT motivating factors, and ratings were correlated to patient functioning and symptoms. We found that, relative to healthy participants, people with schizophrenia reported goals that were: 1) less motivated by filling autonomy and competency needs, but equivalently motivated by relatedness; 2) less extrinsically rewarding, but equivalently motivated by punishment; 3) more disconnected/disengaged. Higher disconnected/disengaged goals were significantly associated with higher negative symptoms and lower functioning. These findings indicate several important leverage points for behavioral treatments and suggest the need for vigorous psychosocial intervention focusing on autonomy, competence, and reward early in the course of illness.
Keywords: Experience sampling method, intrinsic motivation, extrinsic motivation, amotivation, avolition
1. Introduction
Early definitions of schizophrenia highlighted motivation deficits as a crucial feature of the disorder (Bleuler, 1911; Kraepelin, 1919), and recently there has been an increase in focus on understanding these deficits (e.g., Barch, 2008). Several studies have since highlighted the importance of motivation in the disorder, finding that lower motivation is associated with poorer neurocognition, functioning, and outcome (Foussias et al., 2009; Gard et al., 2009; Nakagami et al., 2008). Perhaps the most prominent macrotheory on what drives human goal pursuit is Self-Determination Theory (SDT; Deci and Ryan, 2000; Ryan and Deci, 2000), which provides an important explanatory framework for understanding why individuals pursue specific goals and behaviors. Broadly, SDT emphasizes that individuals set goals and engage in behaviors in order to meet intrinsic psychological needs (intrinsic motivation), in order to move towards external reward or away from punishment (extrinsic motivation), or, when intrinsic and extrinsic factors are thwarted, individuals can develop a disconnection-disengagement with their motivated behavior and its relationship with the environment (Deci and Ryan, 2000).
1.1. Intrinsic Motivation
Thus far, research in schizophrenia using SDT has focused on deficits in intrinsic motivation (e.g., Barch et al., 2008; Choi et al., 2010) (but see Silverstein, 2010). For example, in a recent Ecological Momentary Assessment (EMA) study with people with schizophrenia, intrinsic motivation was positively related to momentary experiences of positive emotion and negatively related to negative emotion (McCormick et al., 2012). Elsewhere, observer ratings of lower intrinsic motivation have been significantly associated with poorer outcome, neurocognition, and occupational functioning (Gard et al., 2009; Nakagami et al., 2008; Saperstein et al., 2011). Importantly, SDT emphasizes that intrinsic motivation is a broad construct facilitated by three ‘psychological needs’ autonomy (motivated behavior towards agency and self-expression), competence (motivated behavior towards knowledge, skill or learning), and relatedness (interpersonal connection) (Ryan and Deci, 2000). To our knowledge, there has not been a systematic assessment of these specific facilitators of intrinsic motivation in schizophrenia.
1.2. Extrinsic Motivation
SDT defines extrinsic motivation as behavior being motivated by external forces specifically through praise, or other rewards (including monetary), or through avoidance of punishment or criticism (Deci and Ryan, 2000). People with schizophrenia are clearly responsive to rewards in treatment settings (Dickerson et al., 2005), and to monetary incentives in laboratory settings (Gold et al., 2012; Summerfelt et al., 1991). However, patients may have difficulty representing the value of reward when the rewarding stimulus is not present (Gold et al., 2008; Heerey and Gold, 2007). We have previously shown that people with schizophrenia have difficulty anticipating pleasurable experiences especially when those experiences are goal-directed or effortful (Gard et al., 2007; Gard et al., in revision). Whether this difficulty in representing or anticipating reward translates into deficits in extrinsic motivation is unclear. As for avoidance of punishment or criticism in schizophrenia, the research in this area is limited. Most research on ‘punishment’ has been completed in the context of monetary reward loss (e.g., Waltz et al., 2013), which is distinct from the avoidance of criticism/punishment as described in SDT (Deci and Ryan, 2000). Some work has been completed on the self-report of the sensitivity of the Behavioral Inhibition System (BIS; involving the avoidance of threat and punishment) in schizophrenia, with one study showing heightened BIS sensitivity in people with schizophrenia (Scholten et al., 2006), and another showing a positive relationship between self-reported BIS sensitivity and negative symptom reports in a large healthy population (Engel et al., 2013).
1.3. Disconnected/disengaged
Finally, when psychological intrinsic needs are hindered, or when extrinsic rewards or punishments are not clear or available, one can experience a disconnected-disengagement with the environment (Ryan and Deci, 2000). In this state, (sometimes referred to as an ‘impersonal-amotivated’ orientation) the individual feels that his or her behavior is not connected to an outcome and that he or she lacks agency, choice, or direction. When an individual experiences a great deal of disconnected-disengagement, they often report that their behavior is driven by boredom or a desire to ‘pass the time’ (Deci and Ryan, 2000). Disconnected-disengagement appears to most closely map on to the negative symptom ‘avolition’, of the DSM (American Psychiatric Association, 2013). Given this, we would predict that people with schizophrenia would report more goals that lack agency, direction, or that are driven by boredom.
1.4. Present Study
To our knowledge, no previous study has assessed the specific reasons underlying motivated behavior in people with schizophrenia relative to healthy individuals in a real world setting. We used EMA to assess the short-term goals that people with and without schizophrenia reported in their daily lives. We provided cell phones to participants and had trained research assistants (blind to participant group and study hypotheses) call with semi-structured questions. This approach has been used with other complex populations (Galloway et al., 2008; Lanzi et al., 2007), and is ideal because it minimizes the cognitive/motivational burden of traditional EMA, and allows for truly idiographic and open-ended responses to questions. We asked participants about their short-term goals and about the most important reason for engaging in these goals. Independent raters (also blind to group and hypotheses) then coded all goals on psychological needs, extrinsic motivators, and disconnected/disengagement. We hypothesized that relative to healthy participants, people with schizophrenia would have goals that were rated lower on psychological needs for autonomy, competence, and relatedness, and higher on levels of disconnected/disengagement. Given the mixed evidence of extrinsic motivation in schizophrenia, we did not have an a priori hypothesis on this factor.
2. Method
2.1. Participants
All participants with schizophrenia were recruited from outpatient clinics and day treatment centers in the Bay Area. Exclusion criteria for all participants included a history of head trauma/loss of consciousness, substance abuse in the last six months, neurological disorders, and non-fluency in English, participants with schizophrenia were excluded if there were significant changes in medication or dosage in the previous 30-days, or hospitalization in the previous three months. Healthy comparison subjects were recruited through community postings and bulletin boards. Forty-seven outpatients with schizophrenia (n=31) or schizoaffective disorder (n=16) and 41 healthy comparison subjects participated in the study. Diagnoses for all participants were confirmed using the SCID DSM-IV-Clinician Version (First et al., 1997). People with schizophrenia were also given the Positive and Negative Syndrome Scale interview (PANSS; Kay et al., 1987). There were no differences in any demographic measure between groups (see Table 1).
Table 1.
Demographic characteristics for people with and without schizophrenia. There were no differences between groups on any variable.
| Characteristic | Schizophrenia N=47 |
Healthy Comparison N=41 |
p-value |
|---|---|---|---|
| Age | 39.55 (13.95) | 36.83 (14.89) | .38 |
| Education – years (SD) | 13.9 (2.55) | 14.55 (2.05) | .21 |
| Parental Education – years (SD) | 13.95 (2.75) | 14.25 (3.46) | .68 |
| Gender, n, % | .20 | ||
| Male | 35, 74% | 26, 63% | |
| Female | 12, 26% | 15, 37% | |
| Ethnicity, n, % | .39 | ||
| African American | 6, 13% | 5, 12% | |
| Caucasian/ White | 18, 38% | 21, 51% | |
| Asian American | 9, 19% | 8, 19% | |
| Latino | 8, 17% | 6, 15% | |
| Other | 6, 13% | 1, 2% | |
| Diagnosis – n: | |||
| Schizophrenia | 31 | NA | |
| Schizoaffective | 16 | NA | |
| Chlorpromazine Eq. (SD) | 418.14 (555.67) | NA | |
| PANSS-Total, Sum Average (SD) | 64.42 (13.11) | NA | |
| PANSS – Positive, Average (SD) | 15.27 (4.97) | NA | |
| PANSS – Negative, Average (SD) | 16.69 (5.27) | NA | |
2.2. Procedures
The EMA procedure was fully explained to participants during an orientation, and each participant provided written informed consent. All participants were provided with, and used a study cell phone (for call consistency). All participants were given a thorough orientation to be sure that they understood the questions about goals and reasons motivating the goals, and at least one test call was conducted to confirm that each participant fully understood the task. Starting 1–3 days later, participants were called by trained research assistants four times a day (at pseudorandom times) for seven days between the hours of 9am–9pm. If calls were missed participants were called again within 15 minutes. The number and timing of calls is similar to other EMA designs (Granholm et al., 2013, 2008; Myin-Germeys et al., 2000). Also in line with previous research, participants were paid both for returning the phone ($44-) and $2- per phone call responded to (Galloway et al., 2008). After the EMA procedure was complete, the research assistant met with the participant, retrieved the phone, and paid the participant. In a second meeting at the laboratory, people with schizophrenia returned to complete functioning assessments. This study received IRB approval from the three institutions where the authors are affiliated.
2.3. EMA semi-structured interview
Each call consisted of several questions about the participants’ experiences and goals for the day. For the purpose of this study, we were interested in the underlying motivation of the participants’ goals. Participants were asked what goals they had for the upcoming few hours and were allowed to list up to four goals. The research assistant did not question the goals or prompt for any additional information unless the goal was unclear. Participants were then asked, “What is the most important reason for this goal?” Participants often had several important reasons for their goals. For example, if the goal was ‘to exercise’ the most important reason may have been ‘to get into better shape to compete in a sport, and maybe meet someone.’ In this case the research assistant queried which of those reasons was the ‘most important’ one guiding the behavior. Research assistants were trained on semi-structured interviewing through mock calls and through weekly training sessions.
2.4. EMA Goal Coding
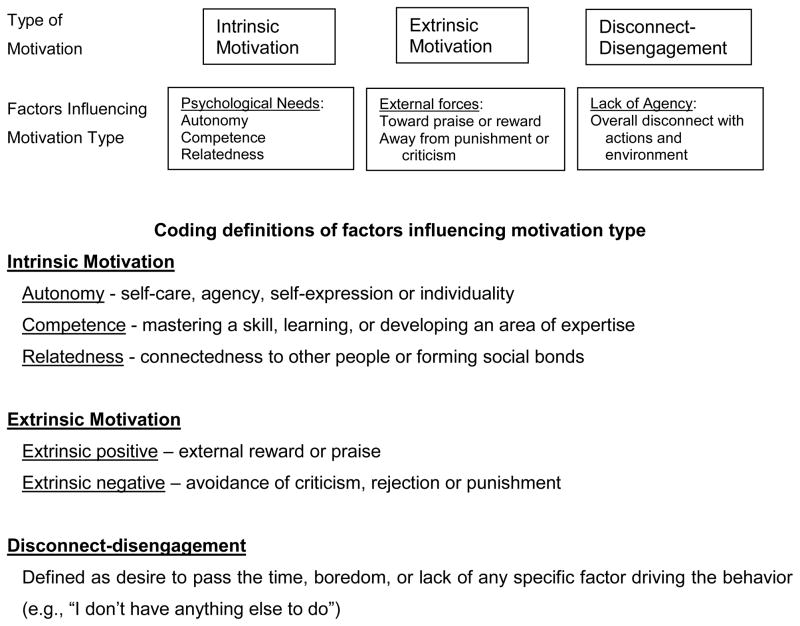
All goals and important reasons from all participants were then compiled such that each participant goal and important reason was together, but randomized so that coders rated each goal/reason individually, blind to participant group. Four coders were used for this task and were blind to study hypotheses. Each goal/reason was rated on a scale of specific anchors (0–3). See Figure 1 for coding anchor definitions. Intra-class correlations (ICC) were computed for inter-rater reliability and all were very good (>.71); rater disagreement was handled such that 1 point differences were averaged. When raters differed by more than 1 point, consensus ratings were completed (by DEG and AHS; less than 5% of the ratings differed by more than 1 point).
Figure 1.
Self-Determination Theory components of motivated behavior, including coding descriptions of each factor influencing the motivation type. Research assistants blind to study hypotheses and group rated each individual goal on each factor driving the SDT motivation type based on the participant’s response to “What goal do you have in the coming few hours?” and “What is the most important reason for having this goal?” Coders rated each goal 0=not at all the motivating factor, 1=slight or incidental aspects to this goal, 2=moderate driving factor for this goal, to 3=primary factor driving the goal. Figure adapted from Deci and Ryan, 2000.
2.5. Functioning
Participants with schizophrenia were rated on the abbreviated version of the Quality of Life Scale (Bilker et al., 2003). To assess overall functioning we averaged the ‘acquaintances’, ‘social initiative’, ‘extent of occupational role functioning’, and ‘capacity for empathy’ items (ICC for the QLS and PANSS ratings were all very good at >.73).
2.6. Data Analysis
All analyses were conducted using Hierarchical Linear Modeling (HLM), which is recommended for EMA studies due to nested nature of the data (Bryk et al., 1992; Schwartz and Stone, 1998). Specifically, HLM treats the multiple observations gathered for each participant (coders ratings of each individual goal) as ‘Level 1’ data (within subjects) that are nested within individuals at ‘Level 2’ (between subjects variable of group: people with or without schizophrenia). Separate models were estimated for each analysis of underlying goal motivation.
3. Results
3.1. Feasibility
All cell phones were returned in working order, except for one lost phone and one phone that was water damaged. The response rates were similar between the two groups: people with schizophrenia responded to 80.62% of the calls, compared to 81.27% for people without schizophrenia. There were no differences in the response rates between the groups, t(86)=−0.91, p=.85, and these response rates are well within the suggested guidelines of response rates for EMA studies (deVries, 1992).
3.2. Group Differences on EMA-Coded Dependent Variables
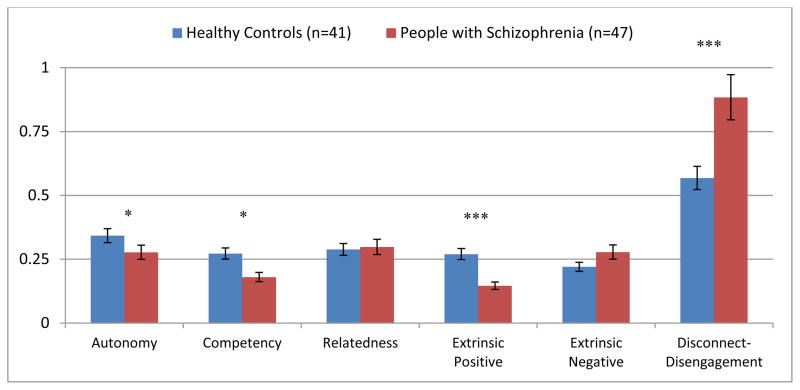
In line with hypotheses, people with schizophrenia reported goals that were driven less by autonomy t(86)= −2.20, p=.03, d=−0.48, and competence t(86)= −2.41, p=.02, d=−0.52. Surprisingly, people with schizophrenia did not differ in the degree to which they set goals driven by relatedness needs t(86)=1.39, p=.17. In terms of goals motivated by external factors (extrinsic motivation), people with schizophrenia set goals that were less motivated by praise or reward t(86)= −5.98, p<.001, d=−1.29, but there were no group differences on whether goals were set to avoid criticism or punishment t(86)=1.39, p=.17. Finally, as predicted, people with schizophrenia reported higher levels of disconnected/disengagement than people without schizophrenia t(86)=5.98, p<.001, d=1.29. See Figure 1 for a summary.
3.3. Relationship of EMA Dependent Variables to Symptoms and Functioning
There were no significant relationships between psychological needs, extrinsic motivation, or disconnected/disengagement to: PANSS positive symptoms, PANSS negative symptoms, or functioning with the following exceptions: people with schizophrenia who had higher disconnected/disengagement were more likely to be rated as having poorer functioning t(40)= −2.98, p=.005, d=−0.94, and more negative symptoms t(43)=2.35, p=.02, d=0.72.
4. Discussion
4.1.1 Psychological needs facilitating intrinsic motivation
We found that people with schizophrenia set goals that were motivated less by the psychological needs of autonomy and competence, though surprisingly, set goals that were motivated by the psychological need for relatedness. This finding shows that it is important to parse out the specific factors that may be contributing to overall deficits in intrinsic motivation in developing effective behavioral treatments. Our findings suggest that a deficit in the drive for autonomy and competence is an important intervention target. It is highly plausible that the lack of drive in these areas observed in people with schizophrenia with established illness results at least in part from a lifetime of failure in achieving “autonomy” and a lack of environmental support for skill development. The clinical implications here are that it might be particularly important to help young people early in the course of illness systematically achieve success in these domains. Second, our results indicate that people with schizophrenia want and value social connections with others (despite suffering from impairments in social cognitive processes), and that this may be an important motivating factor in helping patients set adaptive goals. It is well-established that social skills training in schizophrenia are highly effective in schizophrenia (e.g., Combs et al., 2007; Eack et al., 2011), and interventions that leverage group interactions are also quite effective (e.g., Roder et al., 2011). Surprisingly, psychological needs that facilitate intrinsic motivation were not related to negative symptoms. This may be due in part to the use of the PANSS, which is more limited in its measurement of amotivation (focusing on volition and initiation of movement). On the other hand, our results are consistent with recent research in schizophrenia that did not find a relationship between intrinsic motivation and the BPRS measure of negative symptoms (Choi et al., 2010).
4.1.2 Extrinsic motivational factors
We also found that schizophrenia participants set fewer goals that were driven by extrinsic rewards, such as praise or monetary reward. Although this is not consistent with research on token economies, research on reward-representation has indicated that people with schizophrenia have difficulty with engaging in goal-directed behavior when the rewarding stimulus is not present (Gard et al., 2007; Heerey and Gold, 2007). Participants with schizophrenia were, however, equally motivated by the avoidance of punishment or criticism when setting their short-term goals. In other words, as people with schizophrenia set their goals, they appear to be aware of the potential of rejection or criticism, even when the specific threat is not present. This is consistent with the research on heightened BIS sensitivity where people with schizophrenia have self-reported higher levels of sensitivity to punishment (Scholten et al., 2006). Our results do not indicate that people with schizophrenia are setting goals that are higher in sensitivity to perceived criticism or failure; however, since needs for competency, autonomy, and reward appear to be lower in schizophrenia, it is possible that punishment becomes more salient. Thus, treatments that emphasize increased competence or reward should also direct attention to helping people with schizophrenia avoid over-focusing on criticism or perceived failures.
4.1.3 Disconnected/disengagement
Finally, people with schizophrenia were more likely to refer to their goals as being driven by boredom or a desire to ‘pass time’, that is, more disconnected/disengaged, and not surprisingly, this factor was significantly associated with negative symptoms and patient functioning. We propose that, as people with schizophrenia experience repeated episodes of failure achieving autonomy and competence, perhaps in conjunction with a deficit in reward representation, that they enter what Ryan and Deci label as an enduring “impersonal-amotivated” state. It is also possible that repeated failure experiences early in the course of illness lead to withdrawal from potentially rewarding experiences and a heightened sensitivity to punishment—creating a self-defeatist position that in turn leads to negative symptoms (Beck et al., 2013). If this is shown to be the case successful behavioral treatments should be initiated early to help people with schizophrenia to articulate and focus on actionable goals that meet psychological needs and that lead to success in obtaining extrinsic rewards (Medalia and Brekke, 2010).
4.2. Limitations and overall treatment implications
The focus of this study was on goals, rather than activities. Thus, we do not know if participants’ activities actually reflect the goals they set. For example, it may be that the challenges of forming social bonds and engaging in social activities hinders people with schizophrenia from actually engaging in social activities, even though they are able to set relatedness goals. Another consequence of using ‘goals’ as a proxy for motivated behavior, is that participants may have focused more on what SDT refers to as ‘identified regulation’ or ‘integrated regulation’, which refers to behavior that is done along the spectrum of extrinsic to intrinsic motivation, but that is not fully done for the inherent satisfaction of the activity (e.g., Ryan and Deci, 2000). Although this is possible, it is important to note that psychological needs were referenced as reasons for ‘why’ goals were set as often as extrinsic factors were referenced in both participant groups. An additional limitation was the use of a live caller for obtaining information from participants. Although it seems unlikely that social desirability influenced participants’ responses (as participants could not know what would be a ‘good’ response), we cannot rule out that there was some influence on the data of having a live human caller. In addition, we cannot determine whether the group differences are due to trait differences, substantive environmental group differences (e.g., fewer environmental opportunities for rewards for people with schizophrenia), or both. In the general population, psychological needs can be thwarted or enhanced by both situational and dispositional factors (Deci and Ryan, 2008). Indeed, a great deal of SDT research has shown that an over-reliance on extrinsic motivating factors can undermine intrinsic motivation (e.g., Deci et al., 2001). Thus, future studies should determine the role of the environment on motivation in schizophrenia. Finally, although there is some evidence that motivation impairment exists early in the illness (Schlosser et al., under review), it is unclear from the current cross-sectional study what component of motivation is initially impaired, and thus which element of motivation should be targeted first. For example, it may be that people with schizophrenia have deficits in reward representation or reward anticipation which leads to problems in meeting psychological needs of autonomy or competence. Alternatively, it may be that problems with autonomy or competence (or factors that hinder these needs) make it difficult for extrinsic factors to become as meaningful for patients. Future studies should look longitudinally, to discern the developmental course of the role of intrinsic and extrinsic motivators relative to psychosocial successes and failures in schizophrenia.
Regardless, there are several important treatment implications from this study. In addition to helping people with schizophrenia set actionable goals that have personal meaning and that build specific skills, our field must continue to leverage social connectedness as an important motivating factor (Granholm et al., 2013). Further, our findings underscore the importance of helping people with schizophrenia attend to and seek out extrinsically rewarding experiences (and perhaps, lessening their reliance on avoiding punishment). Specifically, patients may need help calling to mind, noticing opportunities, or setting goals that have a praise or financial reward element, as extrinsic reward can be important to the development of intrinsic motivation (Silverstein, 2010). In summary, our findings highlight the importance of intervening early and at each level of motivated behavior, with the aim of helping people with schizophrenia avoid over-engagement in disconnected-disengaged behaviors, thereby assisting them to increase their functioning and quality of life.
Supplementary Material
Figure 2.
Relative to healthy control participants people with schizophrenia’s goals are motivated significantly less by autonomy, competency, extrinsic positive factors (e.g., praise and money), but goals were more driven by a disconnected-disengagement (e.g., desire to pass the time or boredom).
Acknowledgments
Portions of this research were presented at the Society for Research in Psychopathology in Oakland, California in September, 2013. We would like to thank the following research assistants for their hard work on this project: Vallena Bircheff, Elma Caplin, Yasmin Campos, Kathryn Cooper, Devyn Difilippo, Jennifer DiJoseph, Yvette Fama, Meredith Frank, Claudia Gara, Heidi Iseman, Lindsey Lavaysse, Samantha Mitchell, Sunny Pence, and Courtney Stich.
Funding
The project described was supported by Award Number R21MH086801 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
Conflict of Interest
All authors declare that they have no conflicting interests.
Contributors
David Gard and Sophia Vinogradov designed the study and wrote the protocol. David Gard wrote the first draft of the manuscript. Amy Sanchez and David Gard managed the literature searches and analyses. Amy Sanchez, Jessica Starr and Shanna Cooper worked on the implementation of the EMA procedure, and Melissa Fisher and Abby Rowand worked on the functioning and symptom measures. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. American Psychiatric Publishing, Inc; Arlington, VA US: 2013. [Google Scholar]
- Barch DM. Emotion, motivation, and reward processing in schizophrenia spectrum disorders: what we know and where we need to go. Schizophr Bull. 2008;34:816–8. doi: 10.1093/schbul/sbn092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barch DM, Yodkovik N, Sypher-Locke H, Hanewinkel M. Intrinsic motivation in schizophrenia: Relationships to cognitive function, depression, anxiety, and personality. J Abnorm Psychol. 2008;117:776. doi: 10.1037/a0013944. [DOI] [PubMed] [Google Scholar]
- Beck AT, Grant PM, Huh GA, Perivoliotis D, Chang NA. Dysfunctional attitudes and expectancies in deficit syndrome schizophrenia. Schizophr Bull. 2013;39:43–51. doi: 10.1093/schbul/sbr040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilker WB, Brensinger C, Kurtz MM, Kohler C, Gur REC, Siegel SJ. Development of an abbreviated schizophrenia quality of life scale using a new method. Neuropsychopharmacology. 2003;28:773–7. doi: 10.1038/sj.npp.1300093. [DOI] [PubMed] [Google Scholar]
- Bleuler E. Dementia praecox or the group of schizophrenias. International Universities Press; Oxford, England: 1911. [Google Scholar]
- Bryk AS, Raudenbush SW, Raudenbush DSW. Hierarchical linear models: Applications and data analysis methods. 2. Sage Publications Inc; Thousand Oaks, CA: 1992. [Google Scholar]
- Choi J, Mogami T, Medalia A. Intrinsic motivation inventory: an adapted measure for schizophrenia research. Schizophr Bull. 2010;36:966–976. doi: 10.1093/schbul/sbp030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combs DR, Adams SD, Penn DL, Roberts D, Tiegreen J, Stem P. Social Cognition and Interaction Training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr Res. 2007;91:112–6. doi: 10.1016/j.schres.2006.12.010. [DOI] [PubMed] [Google Scholar]
- Deci EL, Koestner R, Ryan RM. Extrinsic Rewards and Intrinsic Motivation in Education: Reconsidered Once Again. Rev Educ Res. 2001;71:1–27. [Google Scholar]
- Deci EL, Ryan RM. The” what” and” why” of goal pursuits: Human needs and the self-determination of behavior. Psychol Inq. 2000;11:227–268. [Google Scholar]
- Deci EL, Ryan RM. Facilitating optimal motivation and psychological well-being across life’s domains. Can Psychol Can. 2008;49:14–23. [Google Scholar]
- deVries MW. The experience of psychopathology: Investigating mental disorders in their natural settings. Cambridge University Press; New York, NY,US: 1992. [Google Scholar]
- Dickerson FB, Tenhula WN, Green-Paden LD. The token economy for schizophrenia: review of the literature and recommendations for future research. Schizophr Res. 2005;75:405–16. doi: 10.1016/j.schres.2004.08.026. [DOI] [PubMed] [Google Scholar]
- Eack SM, Pogue-Geile MF, Greenwald DP, Hogarty SS, Keshavan MS. Mechanisms of functional improvement in a 2-year trial of cognitive enhancement therapy for early schizophrenia. Psychol Med. 2011;41:1253–61. doi: 10.1017/S0033291710001765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel M, Fritzsche A, Lincoln TM. Anticipatory pleasure and approach motivation in schizophrenia-like negative symptoms. Psychiatry Res. 2013:1–5. doi: 10.1016/j.psychres.2013.07.025. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders Clinician Version (SCID-CV) American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Foussias G, Mann S, Zakzanis KK, van Reekum R, Remington G. Motivational deficits as the central link to functioning in schizophrenia: A pilot study. Schizophr Res. 2009;115:333–337. doi: 10.1016/j.schres.2009.09.020. [DOI] [PubMed] [Google Scholar]
- Galloway GP, Didier R, Garrison K, Mendelson J. Feasibility of ecological momentary assessment using cellular telephones in methamphetamine dependent subjects. Subst Abus Res Treat. 2008;1:9–14. doi: 10.4137/sart.s428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gard DE, Fisher M, Garrett C, Genevsky A, Vinogradov S. Motivation and its relationship to neurocognition, social cognition, and functional outcome in schizophrenia. Schizophr Res. 2009;115:74–81. doi: 10.1016/j.schres.2009.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gard DE, Kring AM, Germans Gard M, Horan WP, Green MF. Anhedonia in schizophrenia: Distinctions between anticipatory and consummatory pleasure. Schizophr Res. 2007;93:253–260. doi: 10.1016/j.schres.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gard DE, Sanchez AH, Cooper K, Fisher M, Garrett C, Vinogradov S. Difficulty Engaging in Effortful Behavior in Daily Life in Schizophrenia. doi: 10.1037/abn0000005. In revision. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold JM, Waltz JA, Matveeva TM, Kasanova Z, Strauss GP, Herbener ES, Collins AGE, Frank MJ. Negative symptoms and the failure to represent the expected reward value of actions: behavioral and computational modeling evidence. Arch Gen Psychiatry. 2012;69:129–138. doi: 10.1001/archgenpsychiatry.2011.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold JM, Waltz JA, Prentice KJ, Morris SE, Heerey EA. Reward processing in schizophrenia: A deficit in the representation of value. Schizophr Bull. 2008;34:835–47. doi: 10.1093/schbul/sbn068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Ben-Zeev D, Fulford D, Swendsen J. Ecological Momentary Assessment of social functioning in schizophrenia: Impact of performance appraisals and affect on social interactions. Schizophr Res. 2013;145:120–124. doi: 10.1016/j.schres.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Loh C, Swendsen J. Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophr Bull. 2008;34:507–514. doi: 10.1093/schbul/sbm113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heerey EA, Gold JM. Patients with schizophrenia demonstrate dissociation between affective experience and motivated behavior. J Abnorm Psychol. 2007;116:268–278. doi: 10.1037/0021-843X.116.2.268. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Dementia praecox and paraphrenia. E & S Livingstone; Edinburgh: 1919. [Google Scholar]
- Lanzi RG, Ramey SL, Lefever JB, Guest KC, Atwater J, Hughes K. Cell phone methodology for research and service with high risk mothers and children. NHSA Dialog. 2007;10:58–66. [Google Scholar]
- McCormick BP, Snethen G, Lysaker PH. Emotional episodes in the everyday lives of people with schizophrenia: the role of intrinsic motivation and negative symptoms. Schizophr Res. 2012;142:46–51. doi: 10.1016/j.schres.2012.09.002. [DOI] [PubMed] [Google Scholar]
- Medalia A, Brekke J. In search of a theoretical structure for understanding motivation in schizophrenia. Schizophr Bull. 2010;36:912–8. doi: 10.1093/schbul/sbq073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myin-Germeys I, Delespaul PAEG, deVries MW. Schizophrenia patients are more emotionally active than is assumed based on their behavior. Schizophr Bull. 2000;26:847–853. doi: 10.1093/oxfordjournals.schbul.a033499. [DOI] [PubMed] [Google Scholar]
- Nakagami E, Xie B, Hoe M, Brekke JS. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: Testing mediator and moderator effects. Schizophr Res. 2008;105:95–104. doi: 10.1016/j.schres.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Roder V, Mueller DR, Schmidt SJ. Effectiveness of integrated psychological therapy (IPT) for schizophrenia patients: a research update. Schizophr Bull. 2011;37(Suppl 2):S71–9. doi: 10.1093/schbul/sbr072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan RMRM, Deci ELEL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Sacks S, Fisher M, Garrett C, Alexander P, Holland C, Rose D, Hooker C, Vinogradov S. Combining computerized social cognitive training with neuroplasticity-based auditory training in schizophrenia. Clin Schizophr Relat Psychoses. 2013;7:78–86A. doi: 10.3371/CSRP.SAFI.012513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saperstein AM, Fiszdon JM, Bell MD. Intrinsic motivation as a predictor of work outcome after vocational rehabilitation in schizophrenia. J Nerv Ment Dis. 2011;199:672–677. doi: 10.1097/NMD.0b013e318229d0eb. [DOI] [PubMed] [Google Scholar]
- Schlosser DA, Fisher M, Gard DE, Fulford D, Loewy RL, Vinogradov S. Motivational deficits in individuals at-risk for psychosis and across the course of schizophrenia. doi: 10.1016/j.schres.2014.06.024. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholten MRM, van Honk J, Aleman A, Kahn RS. Behavioral inhibition system (BIS), behavioral activation system (BAS) and schizophrenia: relationship with psychopathology and physiology. J Psychiatr Res. 2006;40:638–45. doi: 10.1016/j.jpsychires.2006.03.005. [DOI] [PubMed] [Google Scholar]
- Schwartz JE, Stone AA. Strategies for analyzing ecological momentary assessment data. Heal Psychol. 1998;17:6–16. doi: 10.1037//0278-6133.17.1.6. [DOI] [PubMed] [Google Scholar]
- Silverstein SM. Bridging the gap between extrinsic and intrinsic motivation in the cognitive remediation of schizophrenia. Schizophr Bull. 2010;36:949–56. doi: 10.1093/schbul/sbp160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summerfelt AT, Alphs LD, Wagman AM, Funderburk FR, Hierholzer RM, Strauss ME. Reduction of perseverative errors in patients with schizophrenia using monetary feedback. J Abnorm Psychol. 1991;100:613–6. doi: 10.1037//0021-843x.100.4.613. [DOI] [PubMed] [Google Scholar]
- Waltz Ja, Kasanova Z, Ross TJ, Salmeron BJ, McMahon RP, Gold JM, Stein Ea. The roles of reward, default, and executive control networks in set-shifting impairments in schizophrenia. PLoS One. 2013;8:e57257. doi: 10.1371/journal.pone.0057257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.