Abstract
Background
Carotid and coronary atherosclerosis are associated to each other in imaging and autopsy studies. We evaluated whether carotid artery plaque seen on carotid ultrasound can predict incident coronary artery calcification (CAC).
Materials and Methods
We repeated Agatston calcium score measurements in 5445 participants of the Multi-Ethnic Study of Atherosclerosis (MESA) (mean age 57.9 years; 62.9% female). Internal carotid artery lesions were graded as 0%, 1-24%, >25% diameter narrowing and intima-media thickness (IMT) was measured. Plaque was present for any stenosis > 0%. CAC progression was evaluated with multivariable relative risk regression in cases with CAC = 0 at baseline and with multivariable linear regression for CAC > 0 adjusting for cardiovascular risk factors, body mass index, ethnicity, and common carotid IMT.
Results
CAC was positive at baseline in 2708/5445 (49.7%) participants and became positive in 458/2837 (16.1%) at mean interval of 2.4 years between repeat examinations. Plaque and ICA IMT were both strongly associated with presence of CAC. After statistical adjustment, presence of carotid artery plaque significantly predicted incident CAC with a relative risk(RR) of 1.37 (95% Confidence Intervals: 1.12, 1.67). Incident CAC was associated with ICA IMT with an RR of 1.13 (95% Confidence Intervals: 1.03, 1.25) for each mm increase. Progression of CAC was also significantly associated (p < 0.001) with plaque and ICA IMT.
Conclusions
In individuals free of cardiovascular disease, subjective and quantitative measures of carotid artery plaques by ultrasound imaging are associated with CAC incidence and progression.
INTRODUCTION
The presence of atherosclerotic lesions in the carotid arteries is correlated with the presence of coronary artery disease on imaging studies1-3. The presence of carotid and coronary artery lesions also correlates in autopsy studies although they do not necessarily share the same associations with cardiovascular risk factors4.
Atherosclerotic plaques go through structural changes as they progressively enlarge. During the later stages, these plaques are composed of lipid rich deposits and fibrous tissue intermixed with areas of necrotic thrombus and calcium deposition5. Coronary artery calcifications expressed as a calcium score are recognized as a marker of coronary artery disease as well as of coronary artery disease outcomes6. A calcium score of zero is associated with a very low risk of cardiovascular outcomes7, 8. Factors leading to the development of a positive calcium score would therefore be of importance.
Given that plaque deposits at the carotid artery bifurcation are correlated with coronary artery lesions, calcified or not, it seems plausible that the presence of carotid artery lesions might be associated with a higher likelihood of developing a positive calcium score.
We studied this hypothesis in the Multi-Ethnic Study of Atherosclerosis, a longitudinally followed cohort composed of whites, black, Chinese and Hispanics by investigating the associations between carotid artery lesions seen on ultrasound imaging and the short-term likelihood of developing a positive calcium score.
Methods
Population
MESA (Multi-Ethnic Study of Atherosclerosis) is composed of a multiethnic population of 6814 men and women aged 45-84 years without a history of clinical cardiovascular disease at baseline enrolled between July 2000 and August 2002 at six sites in the United States. The MESA cohort includes whites, African-American, Hispanic, and Chinese participants. Participants were excluded at baseline if they had physician diagnosis of heart attack, stroke, transient ischemic attack, heart failure, angina, atrial fibrillation or history of any cardiovascular procedure9. Participants with weight above 300 lbs, pregnancy, or any medical conditions that would prevent long-term participation were also excluded. MESA protocols and all studies described herein have been approved by the Institutional Review Boards of all collaborating institutions. All participants gave informed consent.
Risk factors and anthropomorphic variables
Age, gender, race/ethnicity, and medical history were self-reported. Use of anti-hypertensive and lipid lowering medications (statins) was also recorded. Current smoking was defined as self-report of one or more cigarettes in the last 30 days and prior smoking as any smoking history before this interval. Body mass index was calculated from the participant's weight divided by height2 (kg/m2). Resting systolic and diastolic blood pressures (BP) were measured three times in the seated position using a Dinamap model Pro 100 automated oscillometric sphygmomanometer (Critikon, Tampa, Florida).
Glucose and lipids were measured after a twelve-hour fast. Serum glucose was measured by rate reflectance spectrophotometry on the Vitros analyzer (Johnson & Johnson Clinical Diagnostics, Inc., Rochester, NY). Diabetes mellitus was determined using the 2003 ADA fasting criteria algorithm10. Total cholesterol was measured using a cholesterol oxidase method (Roche Diagnostics), as was HDL after precipitation of non-HDL cholesterol with magnesium/dextran, triglycerides using Triglyceride GB reagent (Roche Diagnostics).
Carotid artery measures
The patients were supine with their head rotated 45° towards the side opposite to the side being imaged. A transverse sweep was recorded from the low neck through the carotid artery bifurcation into the internal carotid artery. Doppler velocity measurements were made at the site of any bulb or proximal internal carotid artery lesion or in the proximal internal carotid artery if no lesions were seen. A common carotid artery was then imaged at 45 degrees from the vertical with the beginning of the bulb shown on the image (to the left). Three views centered on the internal carotid artery bulb were taken: one anterior, one lateral (at 45 degrees) and one posterior. Images were acquired on the right and on the left. A matrix array probe (M12L, General Electric, Milwalkee, WI) was used with the frequency set at 13 MHz for the common carotid artery and 9 MHz for the internal carotid artery and with two focal zones at a frame rate of 32 frames-per-second.
All carotid artery measurements were blinded and made at the ultrasound reading center in Boston, MA. The two common and six internal carotid artery images were used to measure the intima-media thickness of both the near and far walls. Common carotid artery IMT was calculated as the mean of the maximum IMT on each of the two common carotid artery images. Maximum internal carotid artery IMT was calculated as the maximum wall thickness seen on any of the internal carotid artery images11. Images of the internal carotid artery (3 per side) and the videotaped transverse sweep were further reviewed to determine the presence and severity of any lesion in the internal carotid artery, either near or far walls. These lesions were graded with a semi-quantitative scale of 0% (absent lesion) and lesions causing relative narrowing of 1-24% and >25%. Doppler velocity measurements at the site of the lesions with peak-systolic velocities ≥ 125 cm/sec were considered to be greater than 50% diameter narrowing12. The 43 lesions detected in this fashion were included in the > 25% group. The greater of the right and left sides was used for final grading of lesion severity. Readers were reviewed every 2 to 3 weeks during sessions to establish uniformity of interpretations by having the principal investigator (JFP) review selected studies. All carotid artery interpretations were blinded to demographics.
Blinded replicate scans were performed and read on 112 participants. Agreement for the presence of plaque was measured as a kappa of 0.92 (standard error of 0.03). The correlation coefficient for replicate ICA IMT measurements was 0.88 (n = 110) and 0.91 (n = 112) for CCA IMT
Outcomes
Two separate coronary artery studies were acquired on each participant at baseline (2000-2002) with either ECG-gated electron beam (EBCT) or multidetector (MDCT) computed tomography during a breath hold13, 14. Presence of coronary artery calcium was determined by the Agatston method. Scans were read centrally at the Los Angeles Biomedical Research Institute at Harbor-UCLA. Calcification was considered as positive when the Agatston score was greater than zero.
Separate coronary artery scans were repeated on a randomly selected half of the cohort at a second cohort examination (September 2002 through January 2004) and on the other half at the third examination (March 2004 through July 2005)15. Median interval between visits for the whole cohort was of 2.4 years after the baseline examination. All coronary artery calcium scoring was blinded to demographics.
We restricted our analyses to individuals with complete risk factors. Of the original 6814 participants, information was missing on risk factors in 157 and 5 had baseline cardiovascular disease. Further information was missing on plaque in 11, common carotid IMT in 83, and internal carotid artery IMT in 106.
All of these 6552 participants had baseline coronary artery calcium studies. Follow-up CAC studies were available in 5445. Of the 107 participants without CAC follow-up studies, follow-up was maintained in 607 through phone interviews or clinic visits while follow-up was lost for 400 participants.
The development of a CAC score greater than zero was deemed a positive outcome in individuals without a positive calcium score at baseline (n = 2837). Change in calcium score was considered the outcome in individuals with a calcium score > 0 at baseline (n = 2708).
Statistical analyses
The mean (and standard deviation) values of continuous variables and the distribution of dichotomous variables as a percentage in each group were shown.
Analysis of variance and the Chi-square test were used to compare individuals with repeat CAC examinations to individuals without a CAC examination, stratified as individuals with follow-up after the scheduled clinic visit as well as individuals lost to follow-up.
We compared the demographics of individuals with a positive calcium score to those with a calcium score of zero at baseline using Chi-square and Student's t-tests.
The rate of developing a positive calcium score has been reported as being approximately 16% in MESA15. Because the odds ratios derived from logistic regression models tend to overestimate the relative risk estimates in situations where the event rates are high, we used relative risk regression models16. We used a modified Poisson approach to estimate the relative risk and confidence intervals. Cardiovascular risk factors, time interval between the two coronary artery calcium studies, and common carotid artery IMT were predictor variables in multivariable risk regression models to which were added measurements of plaque.
In cases with a positive calcium score at baseline, CAC change over time was used as outcome in multivariable linear regression models that included the same risk factors as the multivariable risk regression models.
Figures were generated showing the prevalence of positive CAC scores at baseline for each plaque category and each ICA IMT quartile. Similar figures were generated for new onset CAC > 0 and change in CAC over the follow-up period.
Statistical analyses were performed using STATA 11.2 (StataCorp, College Station, Texas). Level of statistical significance was set to be two-sided at p ≤ 0.05.
Results
At baseline, the average age of the 5445 participants with follow-up CAC studies (Table 1) was 61.8 years, younger than for individuals with no follow-up studies. Significant differences were seen between the groups without repeat scans and those with, mostly for sex, race/ethnicity, smoking status, diabetes, use of hypertensive medications, and systolic blood pressures. No differences were seen for BMI, total cholesterol, HDL-cholesterol levels, and use of statins. Overall, the study cohort had more favorable risk factor levels.
Table 1.
Demographics of cohort members and exclusions due to missing coronary artery calcium (CAC) scores
| Variable | Follow-up without CAC | No follow-up | Study cohort | p-value |
|---|---|---|---|---|
| Age (years) | 63.3±10.4 | 65.0±10.4 | 61.8±10.2 | < 0.0001 |
| Sex (women) | 57.7% | 51.5% | 52.2% | 0.03 |
| Race/Ethnicity | < 0.0001 | |||
| White | 36.4% | 26.2% | 39.9% | |
| Chinese | 11.9% | 11.0% | 12.2% | |
| Blacks | 29.0% | 33.5% | 26.6% | |
| Hispanic | 22.7% | 29.3% | 21.3% | |
| Smoking Status | 0.003 | |||
| Never smoked | 51.1% | 45.5% | 50.6% | |
| Prior smoker | 33.3% | 36.5% | 36.9% | |
| Current smoker | 15.7% | 18.0% | 12.5% | |
| Diabetes (yes) | 15.7% | 22.3% | 13.09 | < 0.0001 |
| Hypertensive medications (yes) | 40.2% | 44.5% | 35.8% | < 0.0001 |
| Statin Medication (yes) | 13.8% | 14.5% | 14.9% | 0.77 |
| Body mass index (kg/m2) | 28.4±5.6 | 28.6±5.6 | 28.2±5.4 | 0.31 |
| Systolic pressure (mmHg) | 129.1±23.3 | 131.5±23.9 | 125.8±21.0 | < 0.0001 |
| Total cholesterol (mg/dL) | 195.7±37.9 | 192.7±39.3 | 194.2±35.2 | 0.95 |
| HDL-cholesterol (mg/dL) | 51.1±15.9 | 50.5±15.0 | 51.0±14.7 | 0.79 |
| Stenosis | P < 0.0001 | |||
| No plaque | 54.4% | 49.0% | 59.2% | |
| 1-24% narrowing | 30.3% | 32.0% | 28.3% | |
| > 25% narrowing | 15.3% | 19.0% | 12.5% | |
| Common carotid IMT* | 0.88±0.20 | 0.91±0.23 | 0.87±0.19 | 0.0001 |
| Maximum Internal carotid | ||||
| IMT* | 1.67±1.06 | 1.80±1.11 | 1.57±1.03 | < 0.0001 |
| CAC positive (>0) | 51.6% | 62.5% | 48.8% | < 0.0001 |
| Number | 607 | 400 | 5445 |
Intima-media thickness (IMT)
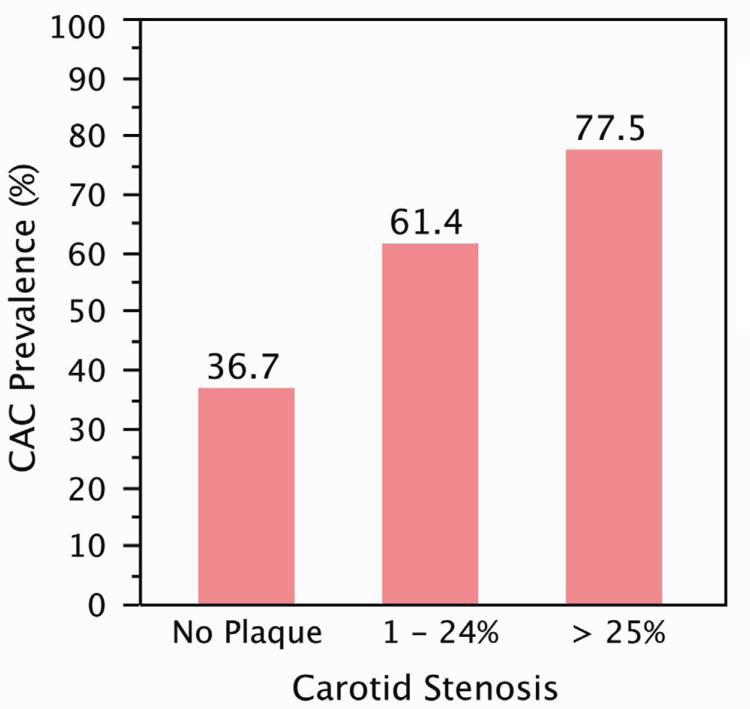
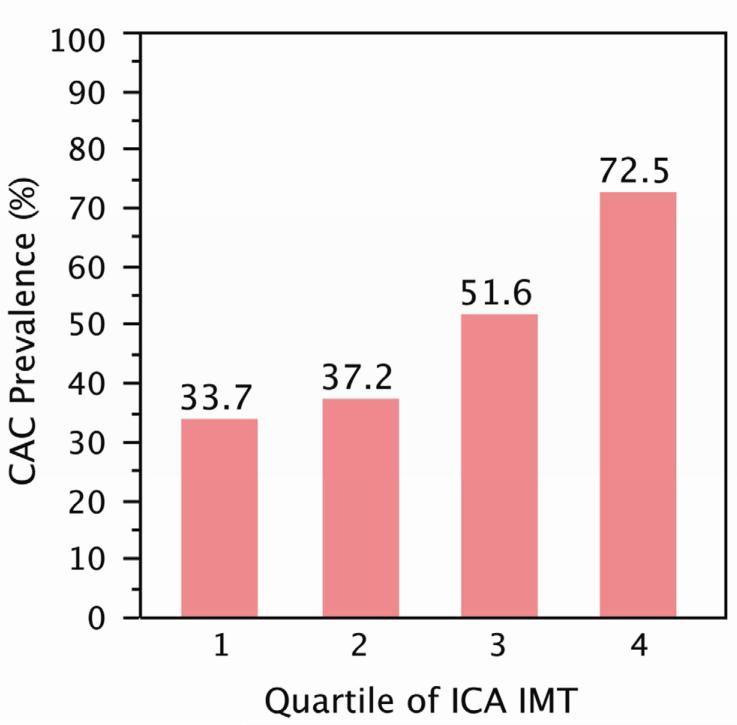
Comparing individuals with positive baseline CAC scores and those with a score of 0 showed significant differences for all risk factors with the exception of BMI and total cholesterol (Table 2). The prevalence of CAC > 0 is shown in figure 1a as a function of the degree of plaque formation and as a function of quartiles of internal carotid IMT in figure 1b. There is a progressive increase in the likelihood of having a positive calcium score as the degree of plaque formation and ICA IMT increases.
Table 2.
Demographics of participants with Coronary Artery calcium (CAC) score of 0 at baseline as compared to participants with a CAC > 0.
| CAC = 0 | CAC > 0 | p-value | |
|---|---|---|---|
| Age (years) | 57.8±9.1 | 66.0±9.5 | < 0.001 |
| Sex (women) | 62.5% | 41.4% | < 0.001 |
| Race/Ethnicity | < 0.001 | ||
| White | 34.6% | 45.4% | |
| Chinese | 12.2% | 12.1% | |
| Black | 30.2% | 22.8% | |
| Hispanic | 22.9% | 19.7% | |
| Smoking status | < 0.001 | ||
| Never | 56.3% | 44.7% | |
| Previous | 31.1% | 43.0% | |
| Current | 12.7% | 12.3% | |
| Diabetes (yes) | 9.8% | 16.6% | < 0.001 |
| Hypertensive medications (yes) | 27.7% | 44.4% | < 0.001 |
| Statin medication (yes) | 9.5% | 20.6% | < 0.001 |
| Body mass index (kg/m2) | 28.2±5.6 | 28.2±5.2 | 0.69 |
| Systolic pressure (mmHg) | 121.9±20.1 | 129.9±21.2 | < 0.001 |
| Total cholesterol (mg/dL) | 193.8±34.5 | 194.5±35.9 | 0.43 |
| HDL cholesterol (mg/dL) | 52.5±15.0 | 49.5±14.1 | < 0.001 |
| Stenosis | < 0.001 | ||
| No plaque | 73.2% | 44.5% | |
| 1 – 24% | 21.3% | 35.6% | |
| > 25% | 5.5% | 19.9% | |
| Common carotid IMT* (mm) | 0.82±0.16 | 0.90±0.20 | < 0.001 |
| Maximum internal carotid IMT* (mm) | 1.27±0.77 | 1.90±1.16 | < 0.001 |
| Total | 2837 | 2708 |
Intima-media thickness
Figure 1a.
Baseline prevalence of positive CAC score for each degree of stenosis with corresponding mean of maximum internal carotid artery intima-media thickness values of 0.95, 2.02 and 3.50 mm.
Figure 1b.
Baseline prevalence of positive CAC score for maximum internal carotid artery intima-media thickness (IMT) quartiles with corresponding mean values of 0.72, 0.99, 1.51, and 3.10 mm.
The average age of individuals without a positive coronary artery calcium score was 57.8 years (9.1 years SD) and composed of 62.5% women and had a varied ethnic composition of 34.6% non-Hispanic Whites, 12.2% Chinese, 30.2% African American and 22.9% Hispanics. After an average follow-up of 2.4 years, there were 458 cases of a new positive calcium score (16.1%).
At follow-up, 24.1% of individuals with a carotid plaque and 13.3% of individuals without plaque developed a positive calcium score. Stratifying by the mean time interval of 2.4 years, only 8.9% of individuals without carotid artery plaque (95/1073) and less than 2.4 years of follow-up developed a positive calcium score whereas 18.0% of individuals without carotid artery plaque and 2.4 years or more of follow-up (180/1003) developed a positive calcium score.
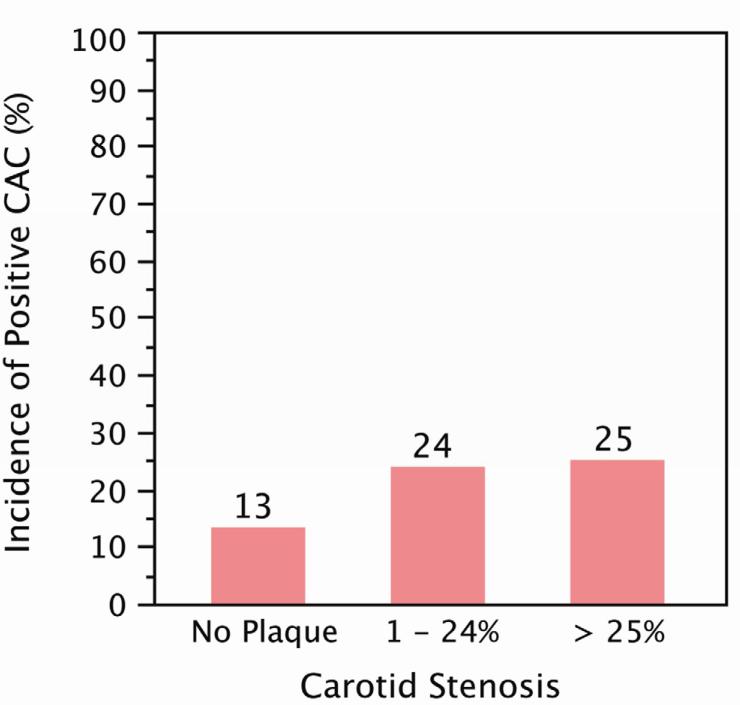
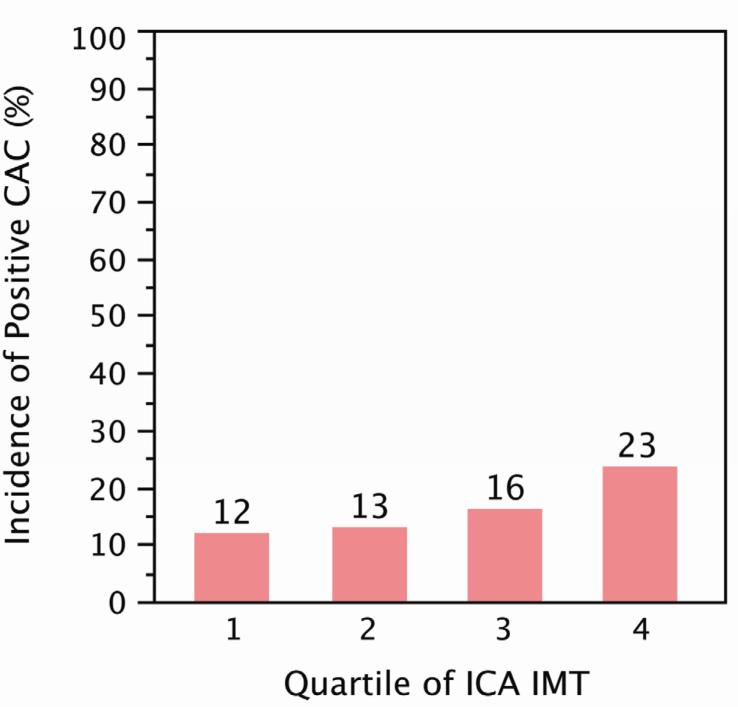
Multivariable risk regression model (Table 3) with internal carotid artery plaque coded as presence of plaque (relative risk ratio 1.37;1.12, 1.67) showed that smoking was not associated with CAC progression, nor was use of statin medication, systolic blood pressure or common carotid IMT. A similar pattern was seen when new models were generated with plaque grade, ICA IMT, and quartiles of IMT substituted for presence of plaque. The model with plaque grades showed a RR of 1.37 (95% CI: 1.11, 1.69) for the 1-24% stenosis category versus absence of plaque whereas the relative risk of a 25 to 49% stenotic lesion was non-significant at 1.37 (95% confidence intervals: 0.97, 1.93). Addition of ultrasound reader, participant level of education, level of activity, did not alter the association between incident positive coronary calcium score and carotid artery plaque (data not shown). Internal carotid artery IMT was a significant predictor of incident CAC with a RR of 1.14 (95% CI: 1.03, 1.25) for each 1 mm increase. When stratified by quartiles, only the highest quartile of ICA IMT was significant with a RR of 1.41 (95% CI: 1.07, 1.87). The diagrams of figure 2 exemplify these findings, showing an association between incident CAC and the two measures of carotid plaque.
Table 3.
Multivariable associations of risk factors with the development of a positive calcium score as outcome using risk regression modeling (n = 2837).
| Variable | Relative Risk (RR) | RR Lower 95% confidence interval | RR Upper 95% confidence interval | p-value |
|---|---|---|---|---|
| Age (years) | 1.03 | 1.02 | 1.04 | < 0.001 |
| Sex (male) | 1.43 | 1.15 | 1.76 | 0.001 |
| Race /ethnicity | ||||
| Whites (referent) | ||||
| Chinese | 0.75 | 0.52 | 1.08 | 0.12 |
| Black | 0.75 | 0.59 | 0.95 | 0.02 |
| Hispanic | 0.78 | 0.61 | 1.01 | 0.06 |
| Smoking | ||||
| none (referent) | ||||
| previous | 1.12 | 0.91 | 1.37 | 0.29 |
| current | 1.21 | 0.91 | 1.63 | 0.19 |
| Diabetes (yes) | 1.23 | 0.94 | 1.61 | 0.13 |
| Blood pressure lowering medications (yes) | 1.32 | 1.07 | 1.63 | 0.01 |
| Statin therapy | 1.28 | 0.97 | 1.69 | 0.08 |
| Body mass index (kg/m2) | 1.034 | 1.015 | 1.052 | < 0.001 |
| Systolic pressure (mmHg) | 1.005 | 1.000 | 1.010 | 0.07 |
| Cholesterol (mg/dL) | 1.003 | 1.001 | 1.006 | 0.01 |
| HDL-cholesterol (mg/dL) | 0.990 | 0.983 | 0.998 | 0.01 |
| Time (years) | 1.41 | 1.27 | 1.57 | < 0.001 |
| Common carotid IMT* (mm) | 0.92 | 0.50 | 1.71 | 0.80 |
| Plaque (yes) | 1.37 | 1.12 | 1.67 | 0.002 |
Intima-media thickness
Our multivariable linear regression model (Table 4) shows a strong association between change in CAC as outcome (Table 4) and carotid plaque, even after adjusting for common carotid artery IMT. Substituting ICA maximum IMT for plaque in the model also showed strong association between ICA IMT and CAC progression. In both cases, use of statins was not associated with CAC progression. Common carotid IMT was no longer a predictor of CAC progression once internal carotid artery IMT was present in the model. This is likely due to the correlation between internal and common carotid artery IMT. These findings also suggest that internal carotid artery IMT is a stronger predictor of CAC progression than common carotid artery IMT.
Table 4.
Multivariable linear regression model applied to change in coronary artery calcium (CAC) as outcome in participants with CAC > 0 at the baseline visit (n = 2708).
| Variable | Beta coefficient | Standardized beta | P-value |
|---|---|---|---|
| Age (years) | 0.099 | 2.4 | < 0.001 |
| Sex (male) | 0.109 | 50.8 | < 0.001 |
| Race /ethnicity | |||
| Whites (referent) | |||
| Chinese | −0.018 | −12.8 | 0.36 |
| Black | −0.022 | −12.2 | 0.27 |
| Hispanic | −0.057 | −32.8 | 0.004 |
| Smoking | |||
| none (referent) | |||
| previous | 0.035 | 16.4 | 0.071 |
| current | 0.020 | 14.1 | 0.31 |
| Diabetes (yes) | 0.142 | 88.0 | < 0.001 |
| Blood pressure lowering | |||
| medications (yes) | 0.054 | 25.2 | 0.005 |
| Statin therapy | 0.028 | 15.7 | 0.14 |
| Body mass index (kg/m2) | 0.041 | 1.8 | 0.046 |
| Systolic pressure (mmHg) | 0.030 | 0.3 | 0.12 |
| Cholesterol (mg/dL) | −0.001 | −0.009 | 0.94 |
| HDL-cholesterol (mg/dL) | 0.004 | 0.070 | 0.83 |
| Time (years) | 0.252 | 68.0 | < 0.001 |
| Common carotid IMT* (mm) | 0.050 | 57.5 | 0.014 |
| Plaque (yes) | 0.118 | 54.4 | < 0.001 |
Intima-media thickness
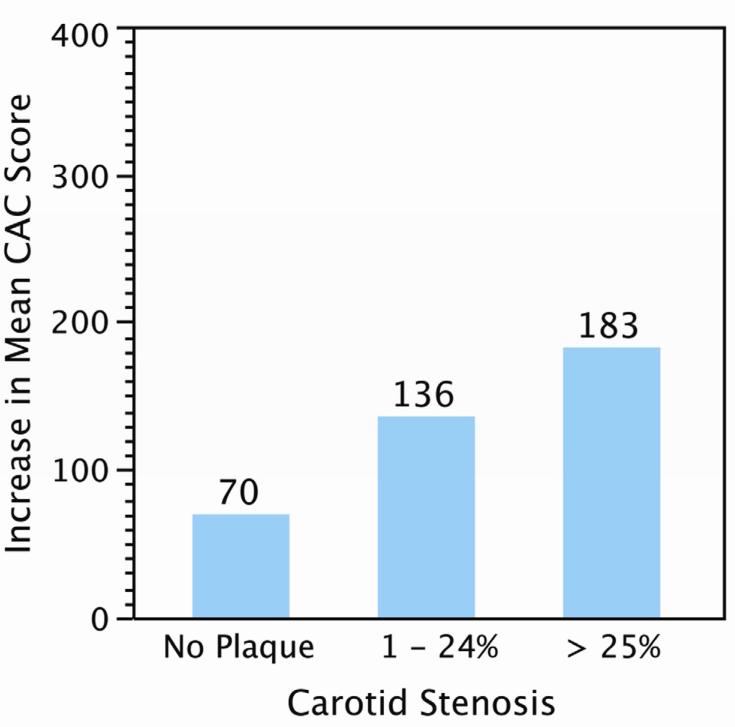
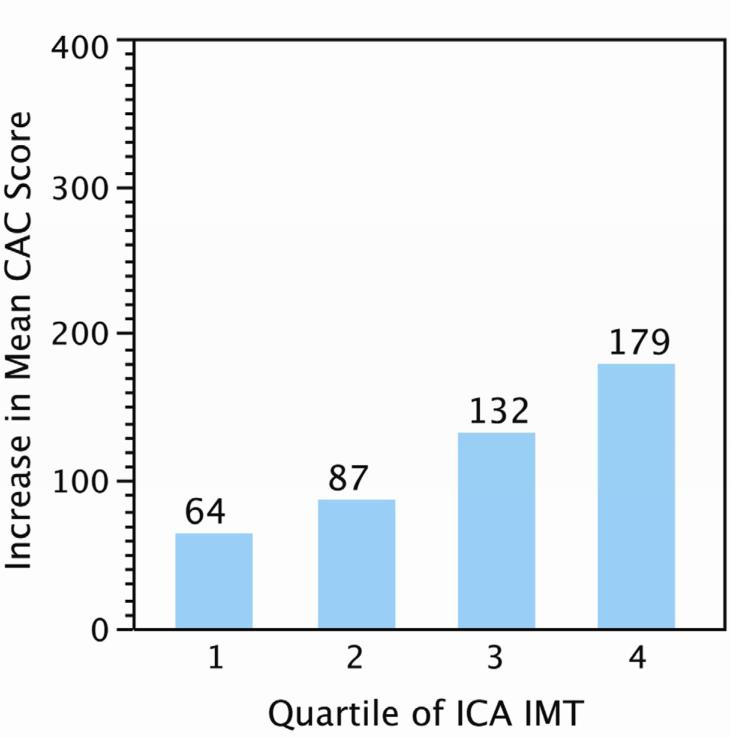
We graphically show the average change in CAC as a function of plaque severity (as % stenosis) and by quartiles of ICA IMT in Figure 3. The increased likelihood of CAC progression with the amount of plaque is clearly depicted.
Discussion
We have found that carotid artery bifurcation lesions are associated with the development of a positive coronary artery calcium score after taking into account cardiovascular risk factors, body mass index, and ethnicity.
The association between coronary artery lesions and carotid artery lesions is well known. Autopsy studies have shown co-existence of lesions in both arterial beds4, 17-19. Studies have shown the presence of coronary lesions in patients with carotid artery disease1, 3 and the presence of carotid artery stenoses in patients with coronary artery disease2, 20.
The aim of our investigation was to evaluate the possibility that a positive coronary artery calcium score is more likely to develop in individuals who have evidence of plaque formation in the carotid artery. This is under the general hypothesis that atherosclerosis tends to develop in a systemic fashion and that the presence of plaque in the carotid artery acts as a marker of coronary artery plaque. The processes responsible for the transformation of non-calcified to calcified coronary artery plaque would then come into play5.
We first observe that the presence of CAC is associated with the presence of carotid plaque and that there is a gradation of CAC burden that is a function of the amount of carotid plaque (Figure 1). We find similar observations for incidence CAC (Figure 2) and progression of a positive CAC score (Figure 3).
While we have found that the presence of carotid artery plaque is a statistically significant marker of the new onset of a positive coronary artery calcium score, a positive calcium score often develops in individuals who do not have evidence of carotid artery plaque formation. For example, after a mean 2.4 years of follow-up, 13.3% of individuals without carotid artery plaque develop a positive calcium score. The likelihood of developing a positive calcium score is lower in individuals without carotid artery plaques at baseline over a follow-up of 2.4 years or less as compared to those with a follow-up longer than 2.4 years (8.9% versus 18.0%). While it is plausible that after 2.4 years, individuals can develop plaques in their carotid and coronary arteries and then these new non-calcified coronary artery plaques go on to calcify, this seems unlikely to have occurred over the short time span of 2.4 years or less. It is still possible that this pathological process took place in some of the individuals who had more than 2.4 years of follow-up, These findings do not suggest a one to one correspondence between carotid and coronary artery plaque formation. Differences in plaque prevalence and incidence in both arterial systems may be related to the marked hemodynamic and geometric differences between the coronary and carotid arteries.
Our study is limited since not all individuals who had a coronary artery CT scan at baseline went on to be have a repeat examination. Of the total 6452 individuals with calcium scores and complete risk factor profiles at baseline, 1007 did not have a follow-up coronary artery calcium study. On average, the participants with follow-up coronary artery calcium scores tended to be younger and healthier that the participants who did not have follow-up (Table 1). This bias cannot be corrected for.
Most cardiovascular risk factors are strong predictors of a future positive coronary artery score. However, although the absence of a carotid plaque does not exclude the presence of coronary artery plaques, the presence of carotid plaque is strongly associated with the development of a positive coronary artery calcium score. For example, data in Table 3 show that the presence of carotid artery plaque has a higher relative risk for incident coronary calcification than diabetes while smoking is not a significant predictor. We have also noted that CAC progresses more rapidly in individuals who have carotid plaque. In this situation, it is likely that the presence of plaque indicates substantial non-calcified plaque in the coronary circulation. Verification of this hypothesis would require the measurement of non-calcified plaque in the coronary artery system simultaneous with carotid ultrasound. We were not able to perform such measurements.
A major strength of our study is the absence of prevalent cardiovascular disease at baseline. As such, our results might be applicable to the primary prevention of cardiovascular disease. If our findings are confirmed in other cohorts, then the presence of plaque on a carotid ultrasound examination might have a value in identifying individuals at risk for developing a positive calcium score in the short term.
We tested the hypothesis that two approaches to the measurement of carotid artery plaque might help predict the development of a positive CAC score or its’ progression.
The first is a completely subjective one. This approach is simple and does not require any specialized measurement processes such as edge detection for intima-media thickness of the common carotid artery21 or time intensive tracing of intima-media thickness contours for plaque area measurements22. It does, however, rely on the ability of a trained reader for detecting and qualitatively grading these early lesions. This, we believe, is achievable by most trained sonographers who have experience with clinical carotid artery examinations. Identifying lesions of less that 50% diameter narrowing is already an element of the clinical ultrasound examination23. While we were able to classify plaques into grades of carotid stenosis, these finer grades did not add much to the observed association between incident positive coronary artery calcium score and the presence of any carotid artery lesion. A dynamic sweep of the carotid artery through the bifurcation was performed in a transverse plane in addition to the acquisition of longitudinal images of the carotid bifurcation. The different readers involved with the carotid artery plaque readings reported that this maneuver facilitated the interpretation of the carotid images.
Our second approach is the selection of the maximum internal carotid artery IMT in any of the internal carotid artery images. This approach does require tracing the contour of the intimalumen and media-adventitia interfaces. Once done, these contours are processed using an automated algorithm to give an IMT value. This approach has been shown to generate ICA IMT values that are associated with risk factors and add to the predictive value of the Framingham Risk scores for cardiovascular events11, 24.
It is possible that more advances imaging approaches might improve the value of plaque measurements for predicting coronary artery disease prevalence and progression25.
Other limitations of our study are that: 1. Studies were acquired at six separate sites and, 2. Studies were subjectively scored and therefore reader dependent. We tested whether these factors affected our results by adjusting our statistical model for clinic site and reader and did not find them to be significant predictors of the development of a positive calcium score (data not shown).
In conclusion, we have found that the presence of carotid artery lesions is associated with incident positive coronary artery calcium score and, from a statistical point of view, more significant than diabetes and smoking. We have also found that more rapid progression of coronary artery calcium is associated with the presence of plaque. These associations should be taken into consideration when plaque is identified during a carotid artery examination. Absence of carotid artery plaque does not, however, exclude the possibility that a positive coronary artery calcium score will develop over a two year period.
Figure 2a.
Follow-up CAC incidence in participants with CAC = 0 at baseline as a function of degree of stenosis with corresponding mean of maximum internal carotid artery intima-media thickness of IMT 0.93, 1.92 and 3.22 mm.
Figure 2b.
Follow-up CAC incidence in participants with CAC = 0 at baseline as a function of internal carotid artery intima-media thickness (IMT) quartiles with corresponding mean IMT values of 0.68, 0.90, 1.13. 2.34 mm.
Figure 3a.
Follow-up change in CAC score in participants with CAC > 0 at baseline as a function of degree of stenosis with corresponding mean of maximum internal carotid artery intima-media thickness values of 0.98, 2.10 and 3.56 mm.
Figure 3b.
Follow-up change in CAC score in participants with CAC > 0 at baseline as a function of internal carotid artery intima-media thickness (IMT) quartiles with corresponding mean IMT values of 0.78, 1.19, 2.05, and 3.54 mm.
Acknowledgements and Funding
The authors would like to thank the investigators, the staff, and the participants of the Multi-Ethnic Study of Atherosclerosis (MESA) study for their valuable contributions. This research was supported by contracts N01- HC-95159 through N01-HC-95165 and N01-HC-95167 as well as R01 HL069003 and R01 HL081352 (Dr Polak).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Disclosures:
Daniel H. O'Leary owns stock in Medpace, Inc.
Data access and responsibility:
JFP had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Kallikazaros I, Tsioufis C, Sideris S, Stefanadis C, Toutouzas P. Carotid artery disease as a marker for the presence of severe coronary artery disease in patients evaluated for chest pain. Stroke. 1999;30:1002–1007. doi: 10.1161/01.str.30.5.1002. [DOI] [PubMed] [Google Scholar]
- 2.Khoury Z, Schwartz R, Gottlieb S, Chenzbraun A, Stern S, Keren A. Relation of coronary artery disease to atherosclerotic disease in the aorta, carotid, and femoral arteries evaluated by ultrasound. American Journal of Cardiology. 1997;80:1429–1433. doi: 10.1016/s0002-9149(97)00701-7. [DOI] [PubMed] [Google Scholar]
- 3.Nowak J, Nilsson T, Sylven C, Jogestrand T. Potential of carotid ultrasonography in the diagnosis of coronary artery disease: a comparison with exercise test and variance ECG. Stroke. 1998;29:439–446. doi: 10.1161/01.str.29.2.439. [DOI] [PubMed] [Google Scholar]
- 4.Holme I, Enger SC, Helgeland A, Hjermann I, Leren P, Lund-Larsen PG, et al. Risk factors and raised atherosclerotic lesions in coronary and cerebral arteries. Statistical analysis from the Oslo study. Arteriosclerosis. 1981;1:250–256. doi: 10.1161/01.atv.1.4.250. [DOI] [PubMed] [Google Scholar]
- 5.Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, Jr., et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation. 1995;92:1355–1374. doi: 10.1161/01.cir.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 6.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. New England Journal of Medicine. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 7.Blaha MJ, Blumenthal RS, Budoff MJ, Nasir K. Understanding the utility of zero coronary calcium as a prognostic test: a Bayesian approach. Circulation. 2011 Mar;4:253–256. doi: 10.1161/CIRCOUTCOMES.110.958496. Cardiovascular Quality & Outcomes. [DOI] [PubMed] [Google Scholar]
- 8.Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;378:684–692. doi: 10.1016/S0140-6736(11)60784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-ethnic study of atherosclerosis: objectives and design. American Journal of Epidemiology. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 10.Genuth S, Alberti KGMM, Bennett P, Buse J, Defronzo R, Kahn R, et al. Follow-up report on the diagnosis of diabetes mellitus.[see comment]. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 11.Polak JF, Pencina MJ, Meisner A, Pencina KM, Brown LS, Wolf PA, et al. Associations of carotid artery intima-media thickness (IMT) with risk factors and prevalent cardiovascular disease: comparison of mean common carotid artery IMT with maximum internal carotid artery IMT. Journal of Ultrasound in Medicine. 2010;29:1759–1768. doi: 10.7863/jum.2010.29.12.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Polak JF, Dobkin GR, O'Leary DH, Wang AM, Cutler AS. Internal carotid artery stenosis: accuracy and reproducibility of color-Doppler-assisted duplex imaging. Radiology. 1989;173:793–798. doi: 10.1148/radiology.173.3.2682776. [DOI] [PubMed] [Google Scholar]
- 13.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr., et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 14.Detrano RC, Anderson M, Nelson J, Wong ND, Carr JJ, McNitt-Gray M, et al. Coronary calcium measurements: effect of CT scanner type and calcium measure on rescan reproducibility--MESA study. Radiology. 2005;236:477–484. doi: 10.1148/radiol.2362040513. [DOI] [PubMed] [Google Scholar]
- 15.Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, et al. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2007;115:2722–2730. doi: 10.1161/CIRCULATIONAHA.106.674143. [DOI] [PubMed] [Google Scholar]
- 16.Zou G. A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 17.Young W, Gofman JW, Tandy R, Malamud N, Waters ES. The quantitation of atherosclerosis. II. Quantitative aspects of the relationship of blood pressure and atherosclerosis. American Journal of Cardiology. 1960;6:294–299. doi: 10.1016/0002-9149(60)90318-0. [DOI] [PubMed] [Google Scholar]
- 18.Young W, Gofman JW, Tandy R, Malamud N, Waters ESG. The quantitation of atherosclerosis: III. The extent of correlation of degrees of atherosclerosis within and between the coronary and cerebral vascular beds. Amer J Cardiol. 1960;6:300–308. doi: 10.1016/0002-9149(60)90318-0. [DOI] [PubMed] [Google Scholar]
- 19.Molnar S, Kerenyi L, Ritter MA, Magyar MT, Ida Y, Szollosi Z, et al. Correlations between the atherosclerotic changes of femoral, carotid and coronary arteries: a post mortem study. Journal of the Neurological Sciences. 2009;287:241–245. doi: 10.1016/j.jns.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Craven TE, Ryu JE, Espeland MA, Kahl FR, McKinney WM, Toole JF, et al. Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. A case-control study. Circulation. 1990;82:1230–1242. doi: 10.1161/01.cir.82.4.1230. [DOI] [PubMed] [Google Scholar]
- 21.Touboul PJ, Prati P, Scarabin PY, Adrai V, Thibout E, Ducimetiere P. Use of monitoring software to improve the measurement of carotid wall thickness by B-mode imaging. Journal of Hypertension - Supplement. 1992;10:S37–41. [PubMed] [Google Scholar]
- 22.Spence JD, Eliasziw M, DiCicco M, Hackam DG, Galil R, Lohmann T. Carotid plaque area: a tool for targeting and evaluating vascular preventive therapy. Stroke. 2002;33:2916–2922. doi: 10.1161/01.str.0000042207.16156.b9. [DOI] [PubMed] [Google Scholar]
- 23.Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI, et al. Carotid artery stenosis: gray-scale and Doppler US diagnosis--Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003;229:340–346. doi: 10.1148/radiol.2292030516. [DOI] [PubMed] [Google Scholar]
- 24.Polak JF, Pencina MJ, Pencina KM, O'Donnell CJ, Wolf PA, D'Agostino RB., Sr. Carotid-wall intima-media thickness and cardiovascular events. New England Journal of Medicine. 2011;365:213–221. doi: 10.1056/NEJMoa1012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johri AM, Chitty DW, Matangi M, Malik P, Mousavi P, Day A, et al. Can carotid bulb plaque assessment rule out significant coronary artery disease? A comparison of plaque quantification by two- and three-dimensional ultrasound. Journal of the American Society of Echocardiography. 2013;26:86–95. doi: 10.1016/j.echo.2012.09.005. [DOI] [PubMed] [Google Scholar]