Abstract
Background
The aim of this study is to investigate the anatomic changes in the shoulder joints responsible for omalgia after the clavicular hook plate fixation under arthroscope.
Methods
Arthroscopic examination was carried out for 12 omalgia patients who underwent clavicular hook plate fixation due to distal clavicle fractures. Functional outcome of shoulder was measured by the Japanese Orthopaedic Association (JOA) score before and after the withdrawal of the fixation plate.
Results
The rotator cuff compression by the clavicular hook was arthroscopically observed in 11 of the 12 cases. The JOA scores of the shoulder were significantly improved at 1 month after the withdrawal of the fixation plate (pain, 28 ± 2.4 vs. 15 ± 5.2; function, 19.2 ± 1.0 vs. 11.7 ± 1.9; range of movements, 26.8 ± 2.6 vs. 14.8 ± 3.4) compared with before.
Conclusions
The impingement of the hook to the rotator cuff may be the main cause for the omalgia. The appropriate hook and plate that fit to the curve of the clavicle as well as the acromion are necessary to decrease the severity of omalgia.
Keywords: Clavicular hook plate, Distal clavicle fractures, Shoulder arthroscopy
Introduction
Distal clavicle fractures account for approximately 10%–26% of all the clavicle fractures, which can be mainly caused by car accidents and sports injuries [1]. Neer further divides the distal clavicle fractures into three types according to the relation of the fracture line to the coracoclavicular ligaments, among which type II fractures occur medially (IIA) or laterally (IIB) to the coracoclavicular ligaments and often result in major displacement because of complete or incomplete rupture of the coracoclavicular ligaments [2]. Although non-surgical strategies can be effective for the treatment of type II distal clavicle fractures, they lead to higher non-union rates (> 30%) [3-5]. Therefore, a series of surgical techniques have been developed in order to reduce the non-union rate and improve functional outcome, including clavicular hook plate [6-8]. Recent studies suggest that the use of a clavicular hook plate is a reasonable option for fixation of unstable distal clavicle fractures, providing a high rate of union and satisfactory functional results [9,10]. However, several patients complain of postoperative omalgia [11] which may be relieved after removal of the hook plate [12].
Recently, it is hypothesized that the omalgia after the clavicular hook plate fixation results from the mechanical hook impingement on the subacromial shoulder and rotator cuff based on radiography [13], magnetic resonance imaging (MRI) [14,15], and sonography [11,16]. In this study, we aimed to further evaluate the anatomic changes in 12 patients who underwent AO clavicular hook plate fixation for distal clavicle fractures and suffered from postoperative omalgia using arthroscopy. Compared with radiography, MRI, and sonography, arthroscopy is not only effective to diagnose but minimally invasive to visualize and treat the shoulder problems.
Patients and methods
Our study was conducted on 12 patients who suffered from trauma-induced distal clavicle pain and limited movements and then were diagnosed in our hospital as distal clavicle fractures (Neer II) (seven males and five females, average age 46.1 years, range 31–68 years). Open reduction and clavicular hook plate (AO, Synthes, Bettlach, Switzerland) internal fixation was performed within 2 weeks (mean time, 3.1 days) after the injuries. Patients received moderate suspension fixation for 2 weeks and then functional exercise. Postoperatively, all patients complained of omalgia, limited shoulder movements, or friction. After being followed up until fractures healed, the patients were requested to undergo arthroscopy to check clavicle hook position and status of rotator cuff and then received removal of hook plate (Synthes, Oberdorf, Switzerland). The patients were further followed up to observe the recovery of shoulder function after the removal of the implant. This study was conducted with the approval of the ethics committee of Shanghai Tenth People's Hospital, and all patients gave written informed consent.
Our surgical procedure was performed with the patient in the beach chair position after general anesthesia and routine disinfection. A 3.5-mm 30° arthroscope (Stryker, Warsaw, IN, USA) was placed through the posterior and anterior portals of the shoulder joint to observe the coracoclavicular ligaments, distal clavicle, acromioclavicular joints, acromion, subacromial clavicular hook, and rotator cuff. The contact and compression between the clavicular hook and rotator cuff were also recorded under the safe range of movements. Adhesiolysis was performed for the subacromial soft tissue adhesion after the removal of the plate. Ice compression was applied postoperatively, passive functional exercise was allowed 1 day postoperatively and for 3 weeks, and then active functional exercise permitted. Physiotherapy was given during the whole process.
The Japanese Orthopaedic Association (JOA) scoring system was used to evaluate the shoulder joint function [17], and the scores were taken before and at 1 month after the removal of plate. The JOA scoring system includes shoulder pain assessment (30 points), shoulder function (20 points), range of movement (ROM) (30 points), radiographic evaluation (5 points), and shoulder stability (15 points). The pain, shoulder function, and ROM scores were compared before and after the removal of plate using the paired t test with the SPSS 10.0 software (SPSS, Chicago, IL, USA). P < 0.05 was considered statistically significant.
Results
The 12 patients had suffered from shoulder pain and limited movement since distal clavicle was fractured and after the plate internal fixation. The scores for shoulder pain, shoulder function, and ROM before the removal of plate were 15 ± 5.2, 11.7 ± 1.9, and 14.8 ± 3.4, which were significantly improved at 1 month after the removal of plate (shoulder pain, 28 ± 2.4; shoulder function, 19.2 ± 1.0; ROM, 26.8 ± 2.6) (Table 1). Ten patients were able to do slight physical activities.
Table 1.
Average JOA score of the shoulder before and 1 month after removal of fixation plate
| |
JOA score of shoulder joint |
||||
|---|---|---|---|---|---|
| Pain | Function | ROMs (elevating + external rotation + internal rotation) | Radiographic evaluation | Stability | |
| Preoperative |
15 ± 5.2 |
11.7 ± 1.9 |
14.8 ± 3.4 |
5 |
15 |
| Postoperative |
28 ± 2.4 |
19.2 ± 1.0 |
26.8 ± 2.6 |
5 |
15 |
|
t |
11.8 |
12.1 |
10.5 |
|
|
| p | < 0.001 | < 0.001 | < 0.001 | ||
ROM range of movement, JOA the Japanese Orthopaedic Association.
Arthroscopy indicated that except one patient manifested subacromial osteophytosis-induced impingement on the acromion; other patients exhibited compression of the clavicular hook on the supraspinatus, obstructing the external rotation of the shoulder. The proximal clavicular hook was the main part compressing the supraspinatus tendon. Even, in one patient whose posterior tip of the clavicle hook went downwards, the whole clavicle hook contacted with the rotator cuff. In another case, tear notch was observed in the rotator cuff against the compression of the clavicle hook. The general information for the 12 patients is shown in Table 2, and a typical case is shown in Figures 1 and 2.
Table 2.
Details of the 12 patients
|
Number |
Gender/age |
Plate (number of holes, height (mm)) |
Weeks of healing |
Preoperative JOA scores (scores for radiographic evaluation and stability were not shown) |
Arthroscopy |
Postoperative JOA scores (scores for radiographic evaluation and stability were not shown) |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pain | Function | ROM (elevating + external rotation + internal rotation) | Pain | Function | ROM (elevating + external rotation + internal rotation) | |||||
| 1 |
M/31 |
6, 15 |
12 |
20 |
12 |
9 + 1 + 2 |
Rotator cuff involvement by proximal hook, subacromial osteophytes |
30 |
20 |
12 + 6 + 6 |
| 2 |
F/56 |
8, 18 |
11 |
20 |
11 |
6 + 3 + 2 |
Rotator cuff involvement by proximal hook |
30 |
20 |
12 + 9 + 6 |
| 3 |
M/49 |
6, 18 |
13 |
10 |
13 |
9 + 3 + 4 |
Rotator cuff involvement by proximal hook |
30 |
18 |
12 + 6 + 6 |
| 4 |
M/62 |
6, 18 |
10 |
10 |
9 |
6 + 1 + 2 |
Rotator cuff involvement by the whole hook |
25 |
18 |
12 + 6 + 6 |
| 5 |
F/37 |
6, 15 |
14 |
20 |
14 |
9 + 3 + 4 |
Subacromial osteophytes, scar adhesions |
30 |
17 |
15 + 9 + 6 |
| 6 |
F/42 |
8, 18 |
12 |
10 |
12 |
6 + 2 + 2 |
Rotator cuff involvement by proximal hook, partial injury |
30 |
20 |
15 + 9 + 6 |
| 7 |
M/38 |
6, 18 |
11 |
10 |
11 |
9 + 3 + 4 |
Rotator cuff involvement by proximal hook |
25 |
20 |
15 + 9 + 4 |
| 8 |
M/40 |
6, 18 |
12 |
10 |
9 |
9 + 6 + 2 |
Rotator cuff involvement by proximal hook |
25 |
19 |
15 + 6 + 4 |
| 9 |
M/33 |
6, 18 |
12 |
20 |
12 |
9 + 3 + 4 |
Rotator cuff involvement by proximal hook |
30 |
19 |
15 + 9 + 6 |
| 10 |
F/38 |
6, 15 |
14 |
20 |
14 |
9 + 6 + 4 |
Rotator cuff involvement by proximal hook |
30 |
20 |
15 + 6 + 4 |
| 11 |
M/59 |
6, 18 |
9 |
10 |
9 |
9 + 6 + 4 |
Rotator cuff involvement by proximal hook |
25 |
19 |
15 + 9 + 6 |
| 12 | F/68 | 4, 15 | 14 | 20 | 14 | 9 + 3 + 4 | Rotator cuff involvement by proximal hook | 30 | 20 | 15 + 6 + 4 |
ROM range of movement, JOA the Japanese Orthopaedic Association, M male, F female.
Figure 1.
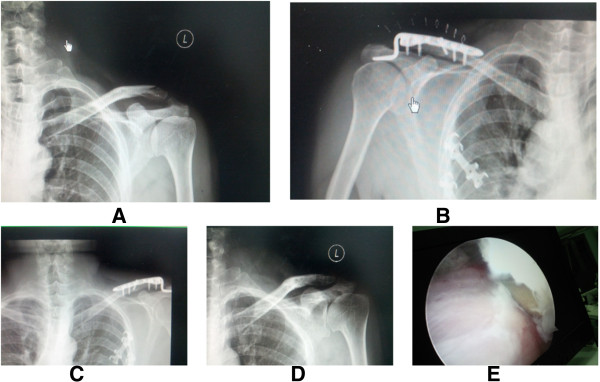
Injury and preoperative and postoperative status of a 56-year-old man. Left distal clavicle fracture (Neer type II) (A). Hook plate fixation (B). The bone was healed 1 month after surgery, but the patient still complained of omalgia (C). After removal of internal fixation (D), extrusion of clavicular hook on supraspinatus was observed (E) under shoulder arthroscopy.
Figure 2.
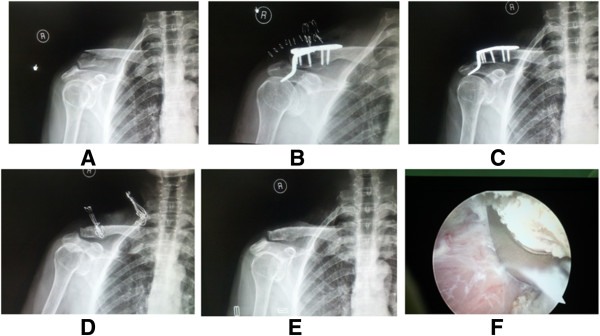
Injury and preoperative and postoperative status of a 68-year-old woman. Right distal clavicle fracture (Neer type II) (A). Clavicular hook plate fixation was performed, but the hook plate was not modulated well (B). Patient complained of omalgia after internal fixation for 3 months (C). After removal of internal fixation (D) and 1 month later (E), omalgia was relieved. The arthroscopy revealed that the hook plate compressed the supraspinatus muscle (F).
Discussion
According to the Neer classification, in the type II distal clavicle fractures, the proximal fragment is very unstable and has no ligamentous attachment, and the muscle forces and weight of the arm tend to displace the fracture fragments, which are difficult to be reset by non-operative management and cause the high rate of non-union compared with other types [2]. Therefore, a number of surgical procedures have been developed to reduce the occurrence of non-union and the morbidity period, such as fixations via Kirschner wires and tension band on the acromion and acromioclavicular joint [18] and fixation between the clavicle and coracoid using screw [19], suture anchor, and plate [20-23]. Among them, the clavicular hook plate fixation is the most widely adopted and reported approach [9,11,24].
The AO plate introduced in 1997 in Europe [25] and in 2002 in Asia is the most widely used clavicular hook plate [11-13,23,26,27] (Table 3). The clavicle hook is inserted below the acromion posterior to the acromioclavicular joint and resets the distal clavicle by the lever principle to disperse the stress of fracture displacement to the acromion, thus providing a good stability. It is reported that there is a small rotation between the scapula and clavicle during abduction and flexion of the upper arm [28]. The rigid fixation of the acromioclavicular joint may lead to a shifting and loosening of the internal fixation. Clavicular hook plate is designed to reduce the interference with the acromioclavicular joint but allow micromotion [28,29]. However, clavicular hook placed under the acromion also can lead to various complications: Rotator cuff and shoulder joint capsule would be impinged if the clavicle hook is placed deeply or the subacromial space is small. Subacromial osteolysis and even unhooking take place if the subacromial stress is too concentrated. Among them, acromial impingement is the most common complication. Renger and others indicate that the incidence of shoulder joint friction is as high as 68%, and shoulders cannot reach approximately 90° of abduction [1]. In the present study, omalgia was also reported in all of the 12 patients who mainly complained of limited movements in lifting and joint friction. Arthroscopy indicated that rotator cuff supraspinatus was compressed in 11 of the 12 patients, and the main part for application of a force was the proximal clavicular hook, which was in accordance with the study described by ElMaraghy et al. [30].
Table 3.
AO hook plate for the treatment of the Neer type II distal clavicle fractures
| Author | Year | Country | Case number (M/F) | Type of hook plate | Hardware removal (time after fixation operation, N ) | Impingement rate | Impingement diagnosis method |
|---|---|---|---|---|---|---|---|
| Flinkkilä et al. [26] |
2002 |
Finland |
17 (16/1) |
AO plate (Stratec Medical, Oberdorf, Switzerland) |
5 months, 17 |
- |
- |
| Muramatsu et al. [13] |
2007 |
Japan |
15 (13/2) |
Synthes AO plate |
4.5 months, 12 |
0% |
Radiography |
| Lee et al. [27,34] |
2009 |
Taiwan |
32 (14/18) |
Synthes AO plate |
4.8 months, 32 |
0% |
Radiography |
| Hsu et al. [23] |
2010 |
Taiwan |
35 (23/12) |
AO plate (Synthes, West Chester, PA, USA) |
1 year, 35 |
25.7% (9/35) |
Radiography |
| Leu et al. [11] |
2012 |
Taiwan |
25 (13/12) |
AO plate (Synthes, Bettlach, Switzerland) |
5.8 months, 25 |
36% (9/25) |
Sonography |
| Tan et al. [12] | 2012 | China | 23 (15/8) | AO plate | 3–14 months, 15 | – | – |
M male, F female, N number of patients who underwent the hardware removal.
To reduce the interference with the acromioclavicular joint, the AO hook plate should be designed to fit anatomically to the acromion and clavicle [31]. In this study, we observed that the whole clavicular hook was imposed on the supraspinatus due to the downward bending of the hook in one case, which led to soft tissue adhesion and small ROM. Smaller hook has been suggested by some researchers to reduce subacromial influence, but it increases the pressure on acromion as well as the risks of acromial osteolysis, unhooking, and stress fractures. By now, there are no standard data for the length, width, thickness, and coracoclavicular distance [30,32,33] because of the individual variance. There are only two types of plate according to the height of the hook (15 or 18 mm), which do not match completely with the different individuals and contributes to the high incidence of complications.
Shoulder arthroscopic examination can be an effective tool to detect rotator cuff tissue injury and thus helps to recover the shoulder function. Rotator cuff compression was observed in 11 of the 12 patients in the present study, and partial tear of the rotator cuff was seen in 1 case. In cadaveric specimens, ElMaraghy et al. find that clavicle hook can pierce the subacromial bursa and induce bursitis, which ultimately results in impingement [30]. Since arthroscopic examination was conducted after the fractures were healed, subacromial bursitis disease could not be investigated, but soft tissue adhesion was detected in our study. Recently, arthroscopy is also introduced to clavicular plate fixation surgery to adjust the plate location and avoid impingement complication. For example, Lee et al. used the arthroscopic-assisted locking compression plate fixation for the treatment of unstable fractures of the lateral end of the clavicle, and only 1 of 23 patients reported shoulder pain due to bursitis [34]. Gille et al. combined arthroscopy and hook plate fixation to treat acromioclavicular joint dislocation and decrease risks related to open surgery [35]. Nourissat et al. raise an arthroscopic-assisted surgical procedure to stabilize the fracture and reconstruct the ligament, which allows for total recovery of shoulder function without inconvenience from device [36]. Takase and others also develop a similar surgical solution [37].
Moreover, rapid improvements in the shoulder function were observed for all the patients after the removal of the plate. It proved that subacromial interference of clavicular hook plate was the main source of postoperative omalgia. Nowadays, most researchers believe that moderate activity restriction is necessary after clavicular hook plate fixation surgery and removal of the plate should be conducted as soon as the fracture is healed [1,38,39].
However, there are some limitations in this study. Firstly, this study is a retrospective case series, and the evidence level of which is lower than that of a cohort study and prospective study. Secondly, because Neer type II distal clavicle fractures are less common, it was difficult to obtain a sufficient number of patients. Small sample size leads to only one case showing the rotator cuff tear. Thus, the classifications and etiopathogenesis of rotator cuff tears were not investigated [15,40,41]. Thirdly, the follow-up period was short for the evaluation of shoulder joint function after the removal of plate. Therefore, future studies need to be performed with longer-term monitoring and larger study populations from multiple medical centers to verify our results.
Conclusion
Overall, our study investigated the detailed impact of clavicular hook plate on acromion with arthroscopy, which provided information for future improvements to reduce the incidence of complications, especially omalgia. Applying a plate completely fitting the acromion and clavicle minimizes subacromial interference and the stress on acromion. Since preoperative X-ray cannot show the three-dimensional structure of the acromioclavicular joint, digital construction of the structure and development of individualized clavicular hook plate in terms of shape and location are the directions of future researches.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
XG and BC participated in the design of this study, and they both performed the statistical analysis. JS carried out the study, together with KT, collected important background information, and drafted the manuscript. BC conceived of this study, participated in the design, and helped draft the manuscript. All authors read and approved the final manuscript.
Contributor Information
Xin Gu, Email: xingug@163.com.
Biao Cheng, Email: chengbiaobiaocheng@hotmail.com.
Jian Sun, Email: jianjsun@163.com.
Kun Tao, Email: kuntaot@163.com.
References
- Renger RJ, Roukema GR, Reurings JC, Raams PM, Font J, Verleisdonk EJ. The clavicle hook plate for Neer type II lateral clavicle fractures. J Orthop Trauma. 2009;23:570–574. doi: 10.1097/BOT.0b013e318193d878. [DOI] [PubMed] [Google Scholar]
- Neer CS 2nd. Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002;61:32. [PubMed] [Google Scholar]
- Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg. 2004;86:778–782. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- Virtanen KJ, Malmivaara AO, Remes VM, Paavola MP. Operative and nonoperative treatment of clavicle fractures in adults: a systematic review of 1,190 patients from the literature. Acta Orthop. 2012;83:65–73. doi: 10.3109/17453674.2011.652884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein SM, Badman BL, Keating CJ, Devinney DS, Frankle MA, Mighell MA. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19:1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131:525–533. doi: 10.1007/s00402-010-1196-y. [DOI] [PubMed] [Google Scholar]
- Stegeman SA, Nacak H, Huvenaars KH, Stijnen T, Krijnen P, Schipper IB. Surgical treatment of Neer type-II fractures of the distal clavicle: a meta-analysis. Acta Orthop. 2013;84:184–190. doi: 10.3109/17453674.2013.786637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C-K, Kao F-C, Hsu K-Y, Wu C-H, Yen C-Y, Tu Y-K. Evaluation of a clavicle hook plate for fixation of unstable distal end comminuted clavicle fractures: seven case reports. Formosan J Musculoskelet Disord. 2011;2:102–105. [Google Scholar]
- Good DW, Lui DF, Leonard M, Morris S, McElwain JP. Clavicle hook plate fixation for displaced lateral-third clavicle fractures (Neer type II): a functional outcome study. J Shoulder Elbow Surg. 2012;21:1045–1048. doi: 10.1016/j.jse.2011.07.020. [DOI] [PubMed] [Google Scholar]
- Leu T-H, Ho W-P, Wong P-K, Chuang T-Y, Wong C-C. Clavicular hook plate, a better implant choice for fixation of unstable distal clavicle fractures? J Exp Clin Med. 2012;4:270–274. [Google Scholar]
- Tan H-L, Zhao J-K, Qian C, Shi Y, Zhou Q. Clinical results of treatment using a clavicular hook plate versus a T-plate in Neer type II distal clavicle fractures. Orthopedics. 2012;35:e1191–e1197. doi: 10.3928/01477447-20120725-18. [DOI] [PubMed] [Google Scholar]
- Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127:191–194. doi: 10.1007/s00402-006-0284-5. [DOI] [PubMed] [Google Scholar]
- Schaeffeler C, Mueller D, Kirchhoff C, Wolf P, Rummeny EJ, Woertler K. Tears at the rotator cuff footprint: prevalence and imaging characteristics in 305 MR arthrograms of the shoulder. Eur Radiol. 2011;21:1477–1484. doi: 10.1007/s00330-011-2066-x. [DOI] [PubMed] [Google Scholar]
- Osti L, Buda M, Del Buono A. Fatty infiltration of the shoulder: diagnosis and reversibility. Muscles Ligaments Tendons J. 2013;3:351. [PMC free article] [PubMed] [Google Scholar]
- Lin H-Y, Wong P-K, Ho W-P, Chuang T-Y, Liao Y-S, Wong C-C. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion-dynamic sonographic evaluation. J Orthop Surg Res. 2014;9:6. doi: 10.1186/1749-799X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takagishi N, Nobuhara K, Fukuda H, Matsuzaki A, Mikasa M, Yamamoto R. Shoulder evaluation sheet (in Japanese) J Jpn Orthop Assoc. 1987;61:623–629. [Google Scholar]
- Kao F-C, Chao E-K, Chen C-H, Yu S-W, Chen C-Y, Yen C-Y. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma Acute Care Surg. 2001;51:522–525. doi: 10.1097/00005373-200109000-00016. [DOI] [PubMed] [Google Scholar]
- Ballmer F, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg (Br) 1991;73:291–294. doi: 10.1302/0301-620X.73B2.2005158. [DOI] [PubMed] [Google Scholar]
- Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40:236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- Yang S-W, Lin LC, Chang SJ, Kuo SM, Hwang L-C. Treatment of acute unstable distal clavicle fractures with single coracoclavicular suture fixation. Orthopedics. 2011;34:436. doi: 10.3928/01477447-20110427-10. [DOI] [PubMed] [Google Scholar]
- Madsen W, Yaseen Z, LaFrance R, Chen T, Awad H, Maloney M, Voloshin I. Addition of a suture anchor for coracoclavicular fixation to a superior locking plate improves stability of type IIB distal clavicle fractures. Arthroscopy. 2013;29:998–1004. doi: 10.1016/j.arthro.2013.02.024. [DOI] [PubMed] [Google Scholar]
- Hsu T-L, Hsu S-K, Chen H-M, Wang S-T. Comparison of hook plate and tension band wire in the treatment of distal clavicle fractures. Orthopedics. 2010;33:879. doi: 10.3928/01477447-20101021-04. [DOI] [PubMed] [Google Scholar]
- Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15:419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR. Type 2 fractures of the distal clavicle: a new surgical technique. J Shoulder Elbow Surg. 1997;6:380–382. doi: 10.1016/s1058-2746(97)90006-9. [DOI] [PubMed] [Google Scholar]
- Flinkkilä T, Ristiniemi J, Hyvönen P, Hämäläinen M. Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop. 2002;73:50–53. doi: 10.1080/000164702317281404. [DOI] [PubMed] [Google Scholar]
- Lee Y-S, Lau M-J, Tseng Y-C, Chen W-C, Kao H-Y, Wei J-D. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33:1401–1405. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung M, Kato S, Barrance PJ, Elias JJ, McFarland EG, Nobuhara K, Chao EY. Scapular and clavicular kinematics during humeral elevation: a study with cadavers. J Shoulder Elbow Surg. 2001;10:278–285. doi: 10.1067/mse.2001.114496. [DOI] [PubMed] [Google Scholar]
- Jupiter JB, Leffert RD. Non-union of the clavicle. Associated complications and surgical management. J Bone Joint Surg Am. 1987;69:753–760. [PubMed] [Google Scholar]
- ElMaraghy AW, Devereaux MW, Ravichandiran K, Agur AM. Subacromial morphometric assessment of the clavicle hook plate. Injury. 2010;41:613–619. doi: 10.1016/j.injury.2009.12.012. [DOI] [PubMed] [Google Scholar]
- Liu Q, Miao J, Lin B, Lian K. Surgical treatment for unstable distal clavicle fracture with micromovable and anatomical acromioclavicular plate. Int J Med Sci. 2012;9:301. doi: 10.7150/ijms.4425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigliani LU, Ticker JB, Flatow EL, Soslowsky LJ, Mow VC. The relationship of acromial architecture to rotator cuff disease. Clin Sports Med. 1991;10:823–838. [PubMed] [Google Scholar]
- Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5:1–11. doi: 10.1016/s1058-2746(96)80024-3. [DOI] [PubMed] [Google Scholar]
- Lee KW, Lee SK, Kim KJ, Kim YI, Kwon WC, Choy WS. Arthroscopic-assisted locking compression plate clavicular hook fixation for unstable fractures of the lateral end of the clavicle: a prospective study. Int Orthop. 2010;34:839–845. doi: 10.1007/s00264-009-0925-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gille J, Heinrichs G, Unger A, Riepenhof H, Herzog J, Kienast B, Oheim R. Arthroscopic-assisted hook plate fixation for acromioclavicular joint dislocation. Int Orthop. 2012;37(1):77–82. doi: 10.1007/s00264-012-1691-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nourissat G, Kakuda C, Dumontier C, Sautet A, Doursounian L. Arthroscopic stabilization of Neer type 2 fracture of the distal part of the clavicle. Arthroscopy. 2007;23:674.e1–674.e4. doi: 10.1016/j.arthro.2006.08.028. [DOI] [PubMed] [Google Scholar]
- Takase K, Kono R, Yamamoto K. Arthroscopic stabilization for Neer type 2 fracture of the distal clavicle fracture. Arch Orthop Trauma Surg. 2012;132:399–403. doi: 10.1007/s00402-011-1455-6. [DOI] [PubMed] [Google Scholar]
- Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–164. doi: 10.1097/01.blo.0000203469.66055.6a. [DOI] [PubMed] [Google Scholar]
- Chaudry SN, Waseem M. Clavicular hook plate: complications of retaining the implant. Injury. 2006;37:665. doi: 10.1016/j.injury.2005.11.020. [DOI] [PubMed] [Google Scholar]
- Via AG, De Cupis M, Spoliti M, Oliva F. Clinical and biological aspects of rotator cuff tears. Muscles Ligaments Tendons J. 2013;3:70. doi: 10.11138/mltj/2013.3.2.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castagna A, Cesari E, Garofalo R, Gigante A, Conti M, Markopoulos N, Maffulli N. Matrix metalloproteases and their inhibitors are altered in torn rotator cuff tendons, but also in the macroscopically and histologically intact portion of those tendons. Muscles Ligaments Tendons J. 2013;3:132. [PMC free article] [PubMed] [Google Scholar]


