Abstract
Objectives
This research examines the differences in estimated risk of developing hypertension in whites, blacks, and Mexican-Americans age 50 and over for a period of 11 years.
Design, Setting, and Participants
Data came from 9,259 respondents who reported being hypertension-free at the baseline in the Health and Retirement Study with up to five time intervals (1998-2006). Discrete-time survival models were used to analyze ethnic variations in the probability of developing hypertension.
Main Outcome Measure
Estimated odds of developing hypertension.
Results
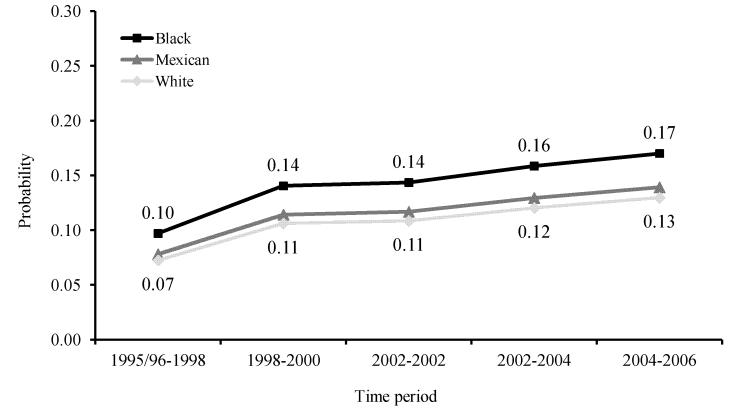
The risk of newly diagnosed hypertension increased between 1995 and 2006 for HRS participants over age 50 years. After adjusting for demographic and health status, the probability of incident hypertension among black Americans was 0.10 during the period of 1995/96-1998, which increased steadily to 0.17 in 2004-2006, and cumulative incidence over the 11-year period at 51%. In contrast, among white Americans the risk was 0.07 during 1995/96-1998 and 0.13 in 2004-2006, with cumulative incidence at 43%. For Mexican-Americans, the probability also increased from 0.08 during 1995/96-1998 to 0.14 during 2004-2006, and cumulative incidence at 42%.
Conclusions
Relative to white and Mexican-Americans, black Americans had an elevated risk of incident hypertension throughout the 11-year period of observation. These variations persisted even when differences in health behaviors, socioeconomic status, demographic, and time-varying health characteristics are accounted for.
Keywords: Ethnic differences, hypertension incidence, discrete-time survival analysis
Introduction
Hypertension continues to be the most prevalent form of CVD, and an important contributor to mortality in the U.S.1-2 Associated with these increases in morbidity are rising health care costs. This makes efforts to better elucidate trends in hypertension risk and ramp up prevention efforts a policy imperative.1-3 Despite national goals to reduce and eliminate ethnic disparities in health outcomes4 disparities in cardiovascular conditions persist. Surveillance data reveal high prevalence of hypertension among black adults, and identify Hispanics and persons of low socioeconomic status to be most at risk for developing cardiovascular disease.5 Although control of well-established clinical risk factors has improved for adults that age into Medicare, ethnic and socioeconomic disparities in cardiovascular disease burden have not diminished.6 To the contrary, recent findings7 cite greater increases in hypertension prevalence for black Americans, with widening disparities over working ages.
Less is known about the incidence of hypertension among older adults. The risk factors for hypertension onset are frequently studied for young adults and the elderly alike.8 However, why racial disparities in hypertension exist is not fully understood. High residual lifetime risk of hypertension, even among older Americans3, represents a large public health burden and dictates a need for primary prevention not to be limited to middle-aged and younger individuals. This study aims to contribute to current understanding of health disparities by examining newly diagnosed hypertension differences over a period of 11 years for middle-aged and older white, black and Mexican-Americans.
Methods
Data and Measures
This study used biennial data from the Health and Retirement Study (HRS). HRS respondents are a nationally-representative sample of community-based adults aged 51 and over. The HRS has been approved by the University of Michigan’s Health Sciences IRB. Consistent with on-going HRS practice respondents are read a confidentiality statement when first contacted, and give oral or implied consent by agreeing to be interviewed. Due to wave incompatibility of key independent variables, these analyses are limited to HRS data from 1995-2006. Data management and analysis is conducted with Stata 10.0.9
Hypertension
Self-reported hypertension was constructed as a binary variable. Self-reported health and disease status have been well established and validated in earlier studies10-11 The HRS asks respondents if they have been diagnosed with hypertension by a physician each interview year. In subsequent interviews, individuals could dispute preloaded responses from the previous interview. In order to deal with conflicting disease reports over time, we examine additional information reported by respondents. Each dispute was corroborated with prior wave information on use of hypertensive medication to verify diagnosis.
Health status
Time-varying health covariates were included to partially account for population heterogeneity. We included self-rated health (SRH), functional limitations, depressive symptoms, chronic disease comorbidities, BMI and current smoker status covariates as time-varying lagged values and change scores. Both, previous period health information and net health changes were conceptualized as contributing unique predictive information in models of new hypertension cases.
Lagged covariates were constructed as health status at time (t-1) and predict hypertension risk at time t. Lagged SRH was measured with a 5-item scale (1=excellent, 2=very good, 3=good, 4=fair and 5=poor). Lagged functional status (0-11) incorporates activities of daily living (ADL, 0-6) and instrumental activities of daily living (IADL, 0-5), with higher scores reflecting increasing number of difficulties. Lagged depressive symptoms were measured with the Center for Epidemiological Studies Depression Scale (CES-D, 0-9) with higher scores reflecting higher depressive symptoms. Lagged comorbidity was a count of chronic diseases (stroke, heart disease, arthritis, lung disease, diabetes and cancer, 0-6). Lagged BMI was calculated using respondent self-reported weight and height. Lagged current smoker was included as a binary variable. Change scores for these measures were constructed as the difference between time t and time (t-1). Positive change scores reflected an increase in health grievances, while negative scores denoted improvement. A change score of zero denoted no change in health conditions across adjacent periods.
Demographic
We constructed binary variables for non-Hispanic white, non-Hispanic black and Mexican-ethnicity individuals. Age was a continuous variable measured at each interval. Education was measured as a continuous variable denoting years of schooling (range 0-17). Lagged and change in income was inflation-adjusted to 2006 levels, and re-scaled (reported per 1000s of dollars). Marital status was constructed as a lagged time-varying covariate. The change in marital status (range −1 to 1) reflected dissolution/widowhood, no change, and acquisition of partners at each point in time over the study period, respectively.
Data analysis
We estimated the incidence of hypertension among non-hypertensives during the 11 years of observation (1995-2006). Date of hypertension diagnosis is not readily available in the HRS, therefore it is problematic to directly calculate incidence rates or estimate continuous time survival models of incidence. However, our analyses result in estimates of risk onset comparable to a continuous time model12.
Discrete-time survival analysis was used to model the onset of hypertension diagnosis. The discrete-time hazard represents the risk of event occurrence in each discrete time period among people in the risk set. The risk of hypertension was estimated for those respondents who have not been previously diagnosed.12 There were 7719 participants (46% of total individuals at baseline; 43% of whites, 62% of blacks, and 43% of Mexican Americans) who were already diagnosed with hypertension and therefore excluded from the discrete-time survival analyses.
We used Stata macros developed by Dinno13 to estimate the model using the logit link and adjust for clustering within households. In estimating discrete time hazard models, the logistic transformation yields the conditional log-odds of the risk of hypertension onset. Model 0 (M0) was estimated to determine the shape of the baseline hypertension hazard. Model 1 (M1) included covariates for race/ethnic group. Model 2 (M2) built on M1 to include demographic and socioeconomic covariates. Model 3 (M3) built on M2 to include health status covariates. Table 2 reports the model results as fitted odds ratios. Model coefficients are transformed into predicted probabilities of the hazard.13 We employed multiple imputation14 of incomplete multivariate data under a normal model software (NORM) to handle missing data. Specifically, three complete data sets were imputed, analyses were replicated on each of these data sets and estimates were averaged to generate a single point-estimate.
Table 2. Hypertension Diagnosis Discrete-Time Survival Results.
| M0 | M1 | M2 | M3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | (se) | p-value | OR | (se) | p-value | OR | (se) | p-value | OR | (se) | p-value | |
| Period 1995/96-1998 | 0.098 | (0.036) | *** | 0.092 | (0.037) | *** | 0.103 | (0.271) | *** | 0.014 | (0.340) | *** |
| Period 1998-2000 | 0.123 | (0.036) | *** | 0.117 | (0.037) | *** | 0.157 | (0.250) | *** | 0.018 | (0.317) | *** |
| Period 2000-2002 | 0.128 | (0.040) | *** | 0.121 | (0.041) | *** | 0.161 | (0.252) | *** | 0.018 | (0.321) | *** |
| Period 2002-2004 | 0.138 | (0.044) | *** | 0.132 | (0.045) | *** | 0.182 | (0.256) | *** | 0.020 | (0.325) | *** |
| Period 2004-2006 | 0.155 | (0.054) | *** | 0.147 | (0.055) | *** | 0.197 | (0.260) | *** | 0.022 | (0.332) | *** |
| Black | 1.483 | (0.057) | *** | 1.377 | (0.069) | *** | 1.278 | (0.073) | *** | |||
| Mexican-American | 1.303 | (0.082) | *** | 1.086 | (0.105) | 0.966 | (0.111) | |||||
| Proxy, tt-1 | 1.110 | (0.100) | 1.249 | (0.112) | * | |||||||
| Δ Proxy | 1.621 | (0.113) | *** | 1.656 | (0.126) | *** | ||||||
| Age | 0.997 | (0.003) | 1.007 | (0.003) | * | |||||||
| Education | 0.979 | (0.008) | ** | 0.987 | (0.009) | |||||||
| Female | 1.164 | (0.046) | *** | 1.209 | (0.049) | *** | ||||||
| Married, tt-1 | 0.971 | (0.053) | 0.963 | (0.057) | ||||||||
| Δ Married | 1.063 | (0.099) | 1.113 | (0.109) | ||||||||
| Income, tt-1 | 0.999 | (0.000) | * | 1.000 | (0.000) | |||||||
| Δ Income | 0.999 | (0.000) | * | 0.999 | (0.000) | |||||||
| BMI, tt-1 | 1.038 | (0.005) | *** | |||||||||
| Δ BMI | 1.030 | (0.012) | ** | |||||||||
| SRH, tt-1 | 1.153 | (0.030) | *** | |||||||||
| Δ SRH | 1.276 | (0.030) | *** | |||||||||
| CESD, tt-1 | 1.011 | (0.015) | ||||||||||
| Δ CESD | 1.013 | (0.014) | ||||||||||
| Functional, tt-1 | 0.966 | (0.025) | ||||||||||
| Δ Functional | 0.962 | (0.023) | ||||||||||
| Comorbidities, tt-1 | 1.043 | (0.027) | ||||||||||
| Δ Comorbidities | 1.458 | (0.051) | *** | |||||||||
| Smoker, tt-1 | 0.846 | (0.069) | * | |||||||||
| Δ Smoker | 0.824 | (0.127) | ||||||||||
|
| ||||||||||||
| LL | −10560.04 | −9739.32 | −6887.80 | |||||||||
| Wald χ2 | −10560.04 | −9739.32 | −8184.35 | |||||||||
| Probability> χ2 | 0.000 | 0.000 | 0.000 | |||||||||
Results
Table 1 details sample descriptive statistics collected at the baseline interview. The mean age for our total sample is 66 years, and 56% are female. The ethnic composition of our sample shows 10% of respondents are black and 5% are of Mexican origin. Table 1 also details the number of excluded individuals with prevalent hypertension at baseline.
Table 1. Characteristics at First Interval.
| Total N= 9259 |
White N= 7880 |
Black N= 936 |
Mexican N= 443 |
|||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| mean | (sd) | mean | (sd) | mean | (sd) | mean | (sd) | |
| Age | 66.25 | (10.26) | 66.49 | (10.27) | 65.20 | (10.40) | 64.23 | (9.48) |
| Female | 0.56 | (0.50) | 0.56 | (0.50) | 0.58 | (0.50) | 0.52 | (0.50) |
| Education (years) | 12.30 | (3.20) | 12.71 | (2.79) | 11.17 | (3.54) | 7.50 | (4.59) |
| Proxy, tt-1 | 0.06 | (0.24) | 0.06 | (0.23) | 0.07 | (0.26) | 0.13 | (0.34) |
| Married, tt-1 | 0.76 | (0.43) | 0.77 | (0.42) | 0.59 | (0.49) | 0.79 | (0.41) |
| Income, tt-1 | 66.00 | (94.46) | 70.78 | (99.21) | 44.24 | (61.62) | 28.11 | (27.80) |
| Functional, tt-1 | 0.31 | (114) | 0.27 | (107) | 0.50 | (143) | 0.52 | (159) |
| SRH, tt-1 | 2.42 | (109) | 2.36 | (108) | 2.70 | (108) | 2.97 | (114) |
| CESD, tt-1 | 1.49 | (178) | 1.42 | (173) | 1.79 | (1.87) | 2.12 | (2.19) |
| Comorbidities, tt-1 | 0.76 | (0.85) | 0.73 | (0.80) | 0.89 | (108) | 0.67 | (0.71) |
| BMI, tt-1 | 27.71 | (5.34) | 27.32 | (5.09) | 29.56 | (6.20) | 28.85 | (5.42) |
| Smoker, tt-1 | 0.14 | (0.35) | 0.14 | (0.34) | 0.17 | (0.38) | 0.14 | (0.35) |
| Δ Proxy | 0.02 | (0.21) | 0.02 | (0.19) | 0.04 | (0.26) | 0.00 | (0.30) |
| Δ Marital | −0.02 | (0.14) | −0.02 | (0.13) | −0.02 | (0.15) | −0.02 | (0.13) |
| Δ Income | 0.75 | (114.78) | 0.92 | (123.11) | −1.93 | (50.32) | 3.47 | (29.07) |
| Δ Functional | 0.13 | (1.15) | 0.12 | (109) | 0.20 | (144) | 0.16 | (140) |
| Δ SRH | 0.27 | (0.94) | 0.26 | (0.91) | 0.27 | (104) | 0.21 | (113) |
| Δ CESD | 0.36 | (195) | 0.34 | (1.87) | 0.45 | (2.19) | 0.48 | (2.66) |
| Δ Comorbidities | 0.13 | (0.36) | 0.12 | (0.34) | 0.22 | (0.47) | 0.00 | (0.33) |
| Δ BMI | −0.03 | (2.06) | −0.02 | (1.91) | −0.07 | (2.65) | −0.02 | (2.47) |
| Δ Smoker | −0.01 | (0.20) | −0.01 | (0.19) | −0.01 | (0.23) | −0.01 | (0.23) |
Table 2 presents the discrete-time hazard model results for the risk of developing hypertension. The baseline hazard for hypertension in M0 (unadjusted by any predictors) demonstrates a steady increase in the risk of incident hypertension over time. The probability of being diagnosed with hypertension in the first period is 0.098 and rises to 0.155 by the final time period. In examining models M1-M3, we are able to determine pronounced differences in the probability of newly diagnosed hypertension for black relative to white Americans. Results detail significantly higher odds of hypertension for blacks (in M1, OR=1.483, p<.001; in M2, OR=1.377, p<.001; in M3, OR =1.278, p=.001). The odds attenuated across the models, yet remain significantly higher relative to whites after accounting for differences socioeconomic covariates and health status changes, respectively.
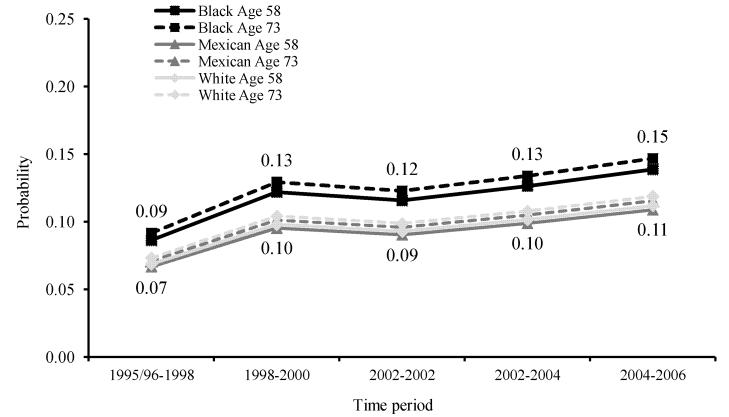
Figure 1 plots the probability of developing hypertension for black, white and Mexican-Americans using model M3 estimates. Overall, the risk of newly diagnosed hypertension increased from 1995-2006 for HRS participants with hypertension risk highest for black Americans. The probability of newly diagnosed hypertension among black Americans was 0.10 in the first period and increased steadily to 0.17 by the final period. In contrast, among white Americans, the risk was 0.07 at the first period and rose to 0.13 by the last period. For Mexican-Americans, the probability increased from 0.08 to 0.13. Figure 2 plots model M3 estimates by race/ethnic group as well as by age. We examine differences in new diagnoses at the 25th and 75th percentile of the age distribution. Both middle-aged and older black Americans exhibit significantly higher probabilities of hypertension than all other age/ethnic groups examined.
Figure 1.
Conditional Probability of Developing Hypertension (M3) By Ethnic Group†
Figure 2.
Conditional Probability of Developing Hypertension (M3) By Ethnic Group and Age†
† Conditional probabilities evaluated at zero change scores and the mean of other covariates
Model M1 details higher odds of hypertension for Mexican-ethnicity individuals (OR=1.303, p=.001); however, once we account for socioeconomic differences (in M2, OR=1.086, p=.429), and changing health status (in M3, OR=0.966, p=.752), Mexican-Americans no longer have significantly different odds of incident hypertension in comparison to whites. We also examined the risk of mortality through separate discrete-time survival models of non-hypertensive persons at the baseline (not shown). Middle-aged and older Mexican-Americans who are hypertension-free at study entry have lower risk of mortality compared to whites. We found no differences in the risk of dying between black and white Americans.
Discussion
This study moves beyond the cross-sectional designs and determines how interval-by-interval changes in hypertension risk differ for middle-aged and older black, Mexican, and white Americans over an 11-year period. The cumulative incidence of developing hypertension over the entire period for the aggregate sample is 44%, with cumulative incidence of 43% for white Americans, 51% for black Americans, and 42% for Mexican-Americans.
The risk of incident hypertension increases over time for individuals in the HRS. To a significant extent, increases in incident hypertension were a result of changing demographic and health attributes. Relative to white and Mexican-Americans, black Americans were 30% more likely to develop hypertension throughout the 11-year period of observation. These variations persisted even when differences in health behaviors, socioeconomic status, demographic, and time-varying health characteristics were adjusted. These results largely support previous studies of increasing hypertension incidence with age8 and extend beyond these studies by tracing persistent ethnic disparities in disease incidence into old age.
Examination of model findings by age groups also reveals interesting results. Although we plot 25th and 75th age percentiles expecting a clear pattern of higher odds accruing to older age groups, this was not the case. Both, younger and older blacks in our sample had highest odds of developing hypertension relative to Mexican and white Americans of any age.
This study was able to examine hypertension risk for Mexican-Americans. The results indicate that hypertension onset for Mexican ethnicity individuals broadly aligns with the concept of the Hispanic Paradox15. Mexican individuals in our study exhibit similar risk of developing hypertension compared to whites despite lower average income and education levels (Table 1).
However, findings for Mexican-Americans should be interpreted with caution. Bias may be introduced by socioeconomic differences in return migrants. Wong, Palloni and Soldo16 suggest that older Mexican-origin individuals emigrating back to Mexico from the U.S. are more likely to be in the wealthiest strata of the income distribution. It is possible that we are not observing higher rates of newly diagnosed hypertension if HRS Mexican-origin participants with greater means are no longer captured in our study sample. In addition, in recent studies, differences in the control of cardiovascular risk factors between predominantly Spanish-speaking and English-speaking Hispanics are discernible.17 Although we examined Spanish-language interview (not shown) we find no differences in hypertension risk. Further study of immigration dynamics and cultural orientation for Mexican-Americans is needed.
There are a few additional limitations that need to be acknowledged. First, an important concern to using self-reported health measures, and specifically, self-reported hypertension indicators, is the reliability of responses and consistency in subsequent respondent re-interviews.18 Specific procedures to explore the extent of inconsistencies across an individual’s longitudinal record and provide more time-consistent disease indicators is reflected in these analyses. In addition, individuals may be unaware or underreport diagnoses of hypertension due to age and race/ethnicity biases and differential access to good quality clinical practitioners. Ostchega and colleagues19 find some substantiation for this concern. Initial comparison of self-reported and measured blood pressure data in the HRS indicate that the two are well correlated.20
Second, these findings are largely reliant on individuals in the HRS having access to a hypertension diagnosis through physician visits and health care system use. Although the majority of the study population is Medicare age-eligible, additional analyses (not shown) included time-varying health insurance coverage. Even after controlling for potential shifts in and out of health insurance coverage, incident hypertension remains elevated for black relative to white Americans, and statistically similar for white and Mexican-Americans.
Finally, it is difficult to ascertain a clear picture of minority health with the HRS sample since the study tracks individuals from middle age into old age and is not able to capture earlier-life selective mortality and hypertension onset. Health disadvantages and differential mortality that may have occurred before middle age are not traced here, and are an important consideration when interpreting the findings. The analyzed sample of black, Mexican and white Americans that survive to middle and old age without diagnosed hypertension is very different than their respective representative populations due to differential morbidity and mortality that occurs earlier in the lifecourse. Still, these results indicate that hypertension prevention efforts for middle aged and older black populations in the U.S. lag behind those for whites.
Aggressive prevention of hypertension even into old age is essential, particularly for black minorities in the U.S. Similar to the recommendations from Mosley and Lloyd-Jones,10 the dissemination of information and aggressive treatment of hypertension and risk factors for hypertension need not be targeted only to young adults. Targeted efforts are needed to reduce hypertension burden for older aged Americans, and to older aged black Americans in particular.
Potential complications arising from new hypertension diagnosis have vast implications on the treatment and management of multiple diseases for elderly Americans.21 Understanding chronic disease burden patterns and severity of conditions for aging minority Americans are important areas for further study.
Acknowledgements
This work was supported by the National Institute on Aging grants F31-AG029783 (Ana Quiñones, PI), R01-AG015124 and R01-AG028116 (Jersey Liang, PI). The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health. We thank Joan Bennett, Xiao Xu, and Alexis Dinno.
References
- 1.Mensah GA, Brown DW. An Overview Of Cardiovascular Disease Burden In The United States. Health Affair. 2007;26(1):38–48. doi: 10.1377/hlthaff.26.1.38. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart Disease and Stroke Statistics—2011 Update: A Report From the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasan RS, Beiser A, Seshadri S, et al. Residual Lifetime Risk for Developing Hypertension in Middle-Aged Women and Men—The Framingham Heart Study. JAMA. 2002;287:1003–1010. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 4.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; Washington D.C.: 2003. pp. 29–79. [PubMed] [Google Scholar]
- 5.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of Disparities in Cardiovascular Health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 6.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity and education: US trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med. 2009;150:505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 7.Geronimus AT, Bound J, Keene D, Hicken M. Black-white differences in age trajectories of hypertension prevalence among adult women and men, 1999-2002. Ethn Dis. 2007;17:40–48. [PubMed] [Google Scholar]
- 8.Mosley WJ, Lloyd-Jones DM. Epidemiology of Hypertension in the Elderly. Clin Geriatr Med. 2009;25:179–189. doi: 10.1016/j.cger.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 9.StataCorp . Stata Statistical Software: Release 10. StataCorp LP; College Station, TX: 2007. [Google Scholar]
- 10.Johnson RJ, Wolinsky FD. The Structure of Health Status Among Older Adults: Disease, Disability, Functional Limitation, and Perceived Health. Journal and Health and Social Behavior. 1993 Jun;34:105–121. [PubMed] [Google Scholar]
- 11.Ferraro KF, Wilmoth JM. Measuring morbidity: disease counts, binary variables, and statistical power. Journals of Gerontology: Social Science. 2000;55B(3):S173–S189. doi: 10.1093/geronb/55.3.s173. [DOI] [PubMed] [Google Scholar]
- 12.Singer JD, Willett JB. It’s About Time: Using Discrete-Time Survival Analysis to Study Duration and the Timing of Events. J Educ Behav Stat. 1993;18(2):155–195. [Google Scholar]
- 13.Dinno A. DTHAZ: Stata module to compute discrete-time hazard and survival probability. 2002 Available in: http://ideas.repec.org/c/boc/bocode/s420701.html.
- 14.Schafer JL, Graham JW. Missing Data: Our View of the State of the Art. Psychol Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 15.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic Paradox in Biological Risk Profiles. Am J Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wong R, Palloni A, Soldo BJ. Wealth in Middle and Old Age in Mexico: The Role of International Migration. Intl Migr Rev. 2007;41(1):127–151. doi: 10.1111/j.1747-7379.2007.00059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eamranond PP, Legedza ATR, Diez-Roux AV, et al. Association between language and risk factor levels among Hispanic adults with hypertension, hypercholesterolemia, or diabetes. Am Heart J. 2009;57(1):53–59. doi: 10.1016/j.ahj.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beckett M, Weinstein M, Goldman N, Yu-Hsuan L. Do Health Interview Surveys Yield Reliable Data on Chronic Illness among Older Respondents? Am J Epidemiol. 2000;151(3):315–323. doi: 10.1093/oxfordjournals.aje.a010208. [DOI] [PubMed] [Google Scholar]
- 19.Ostchega Y, Yoon SS, Hughes J, Louis T. Hypertension awareness, treatment, and control— continued disparities in adults: United States 2005-2006. National Center for Health Statistics; Hyattsville, MD: 2008. NCHS Data Brief No. 3. [PubMed] [Google Scholar]
- 20.Hauser RM, Weir D. Recent Developments in Longitudinal Studies of Aging in the United States. Demography. 2010;47:S111–S130. doi: 10.1353/dem.2010.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paez KA, Zhao L, Hwang W. Rising Out-Of-Pocket Spending For Chronic Conditions: A Ten-Year Trend. Health Affair. 2009;28(1):15–25. doi: 10.1377/hlthaff.28.1.15. [DOI] [PubMed] [Google Scholar]