Abstract
The objective of this study was to measure willingness-to-accept (WTA) reductions in risks for HIV and other sexually transmitted infections (STI) using conditional economic incentives (CEI) among men who have sex with men (MSM), including male sex workers (MSW) in Mexico City. A survey experiment was conducted with 1,745 MSM and MSW (18-25 years of age) who received incentive offers to decide first whether to accept monthly prevention talks and STI testing; and then a second set of offers to accept to stay free of STIs (verified by quarterly biological testing). The survey used random-starting-point and iterative offers. WTA was estimated with a maximum likelihood double-bounded dichotomous choice model. The average acceptance probabilities were: 73.9% for the monthly model, and 80.4% for the quarterly model. The incentive-elasticity of participation in the monthly model was 0.222, and it was 0.515 in the quarterly model. For a combination program with monthly prevention talks, and staying free of curable STI, the implied WTA was USD$288 per person per year, but it was lower for MSW: USD$156 per person per year. Thus, some of the populations at highest risk of HIV infection (MSM & MSW) seem well disposed to participate in a CEI program for HIV and STI prevention in Mexico. The average willingness-to-accept estimate is within the range of feasible allocations for prevention in the local context. Given the potential impact, Mexico, a leader in conditional cash transfers for human development and poverty reduction, could extend that successful model for targeted HIV/STI prevention.
Keywords: Willingness-to-accept, conditional economic incentive, HIV/AIDS and STI prevention, contingency management/conditional cash transfers, Mexico
Introduction
Effective means for reducing HIV risks exist, but they are underutilized: the challenge is how to improve the uptake of effective technologies [1-3]. Because of the high mortality of HIV and the potential negative externalities at the societal level, conditional economic incentives (CEI) have been tested recently as an innovative option to consider for enhancing HIV prevention [4,5]. The main hypothesis of these emerging studies is that economic incentives with or without conditionality [6] can contribute to reduce risk exposures to sexually transmitted infections (STI), increase correct prevention knowledge, and ultimately reduce HIV infections. More generally, conditional cash transfers (CCT) in the developing world (Latin America, and Mexico in particular) have been found successful [7,8] in improving the utilization of prevention health services [9]; various intermediate outcomes [10,11], and health status [12-16]. However, how to best measure, a priori, the optimal level of incentives has not been thoroughly studied.
The optimal level of incentives is not immediately obvious and needs to be set within a particular socio-economic, risk- and vulnerability-context for each target population. The incentive needs to be high enough to potentially spur meaningful behavior change, but it cannot be too high as to be considered coercive, dangerous, or economically inefficient.
The objectives of this study were: 1) to estimate the minimum (optimal) amount that individuals at high risk would be willing to accept to uptake HIV/STI prevention; 2) to identify variables associated with the acceptance rates; and 3) to provide an incentive-elasticity of participation. To the best of our knowledge, this is the first empirical study measuring ex ante the optimal levels of CEI for populations at high-risk of HIV infection.
Theoretical Considerations
In theory, individuals at high risk of HIV infection would participate in CEI prevention programs if the disutility of reducing sexual risk behaviors is at least compensated with an increase in utility derived from the economic incentive. Contextualizing the health capital approach [17] for sex capital, a person’s assets to avoid STI include habits to select sex partners and the social networks from which those partners are selected, as well as protective practices such as condom use [18]. Persons at high risk can exhibit hyperbolic discounting by which valuations are heavily discounted for the short term, but are discounted at much lower rates for outcomes farther in the future [19]. Potential participants value risk behaviors as a source of utility; they may know that the behaviors can have long-term health implications, but the short-term gains (in utility) may be stronger. CEI make the costs associated with risk behaviors more salient and relevant in the present.
Consider a CEI program that would pay individuals at high risk if they are free of curable STI. (The program would test for HIV but not condition on HIV results, as this could have negative programmatic and ethical implications). There would be two states of the world: one with sexually transmitted infection and another without. STI status is directly observable, but sexual risk behaviors are not. There is a probability (P) associated with the risk of contracting a STI, which is dependent on sexual risk behaviors (B); thus, expected utility is represented as follows:
| (1) |
where G are general goods positively affecting the utility function and where individuals adjust sexual risk behaviors so as to maximize utility at the point where the expected marginal utility of reducing B is equal to the marginal utility of compensation payment (α*) plus utility from not having an STI. Thus, incentive payments for negative STI test results may be consistent with reducing risk behaviors: increasing condom use and reducing number of sexual partners. Staying STI free does not imply complete reduction in HIV risk but it suggests reductions in unprotected sexual activity, which can potentially also reduce HIV infection. A highly vulnerable group such as male sex workers may perceive clearer links between financial incentives to stay free of STI and the prices charged from commercial sex where they receive higher payments for unprotected, riskier sex [20,21], though this hypothesis remains to be tested in field trials. A second independent equation specifies the total budget for incentive payments determining the total reduction in STI risks obtainable under practical fiscal constraints. This constraint is not used to define the bid structure for eliciting WTA values:
| (2) |
where the total fixed budget (τ) is exhausted with N program participants at high-risk of HIV infection.
Methods
Survey data collection
We collected information from men who have sex with men (including male sex workers), ages 18-25, in Mexico City during October-December 2008. The survey was conducted by the National Institute of Public Health (INSP), in collaboration with members of the local community and civil society associations [coordinated by La Manta de México A.C. (“Mexican Quilt”)] with in-depth knowledge of the formal and informal meeting places for MSM and MSW. The study was approved by the Institutional Review Board committees at the University of California, Berkeley, and at the Mexican National Institute of Public Health.
We used a time-and-place sampling technique, successfully used in hard-to-reach populations [22-24]. Based on a previous study [25], we chose formal and non-formal meeting places for MSM and MSW that fulfilled attendance, safety and logistical criteria including bars, discotheques, metro stations, and specific streets in the red district. We fielded 84 questions through hand-held computers. The interviews lasted about 40 minutes, and they were self-administered to keep the responses anonymous and confidential and increase the veracity of the information. A set of introductory questions assessed knowledge, attitudes and practices regarding HIV and other STIs; and informed potential participants of the time and inconvenience involved in participating in monthly talks and quarterly biological tests.
The survey experiment
We used an embedded survey experiment to produce exogenous variation in the responses [26] to estimate the minimum incentive necessary for respondents to participate in prevention talks and reduce risk behaviors so that they would stay free of STIs. We used a random-starting-point and iterative bidding, and did not ask open-ended questions [27]: each subject was asked a closed-ended (yes/no) question about whether they would participate given a specific incentive offer. The computer picked a random number $α1 from a programmatically feasible range (USD$1-$15), which was based on previous qualitative work developed with this population [28]. The first question was: “Would you accept $α1 per month as a compensation for your time in participating in monthly HIV prevention talks and tests? A follow-up bargaining question ensued, raising the offer if the respondent did not accept the first offer, or lowering it if the respondent accepted the first offer. A second set of questions asked if participants would stay free of STIs for a quarterly compensation of $α3 (verified by STI testing). Appendix Exhibit A presents the WTA questions and the formulae for the follow-up incentive offers. All incentive offers in the survey were made to participant in current Mexican pesos during the period 1 October – 15 December 2008. In this paper, all incentive offers were converted to US dollars (USD) at the data-collection period average exchange rate of 12.97 Mexican pesos per USD$1 [29].
Willingness-to-accept: single and double-bounded models
Adapting a general framework in resource economics [30] to HIV prevention, consider the single-bounded model (with only one question), where the probability of obtaining a “yes” or a “no” response, given the compensation offer (α), is represented by some distribution function F with parameter θ as follows:
Utility maximization implies that:
Let be the offer in the single-bounded experiment for N participants; the log-likelihood function is given by:
| (3) |
where is 1 if the ith response is “yes” and 0 otherwise; and is 1 if the ith response is “no” and 0 otherwise. The maximum likelihood estimator is the solution to the equation . Using the follow-up, bargaining questions in the WTA experiment means that the responses to the initial and follow-up questions are correlated. Thus, we need to account for the shared error structure in a model to obtain unbiased estimates. For that purpose, we modify the double-bounded dichotomous choice model [30] as follows. If the ith participant responds “no” to αi in the first offer, then in the second higher-up offer; whereas if the ith participant responds “yes” to αi of the first offer, then in the second lowered-down offer. Thus, there are four possible responses in the bargaining game with their respective likelihood outcomes as follows:
“No” in the first offer and again “no” in the second offer: πnn
“Yes” in the first offer and again “yes” in the second offer: πyy
“No” in the first offer and “yes” in the second offer: πny
“Yes” in the first offer and “no” in the second offer: πyn
Following the utility maximization framework, for the first outcome, we have that:
| (4) |
where the third equality follows, by definition, as the conditional probability equals unity: . Similarly, for the second outcome, the likelihood is:
| (5) |
For the third outcome, assuming a symmetric distribution, we have that the likelihood is:
| (6) |
Following the same logic for the fourth outcome, we have that:
| (7) |
The expressions in Eqs. (4) and (5) provide upper and lower bounds of the WTA estimate; whereas Eqs. (6) and (7) sharpen the true estimate of the WTA of the first offer by increasing the lower bound or reducing the upper bound. Now, with N respondents in the double-bounded experiment, and αi, and being the offers to the ith respondent, the log likelihood function is:
| (8) |
where , , and are dichotomous indicator variables with their corresponding response probabilities given by Eqs. (4)-(7). The maximum likelihood estimator for the double-bounded WTA model is the solution to equation: .
Determinants of the acceptance rates
To estimate the determinants of the acceptance rates, we used probit regression models to find significant factors associated with participation. Congruent with the latent Eq. (1), we modeled the probability of accepting HIV/STI prevention as a combination of predictors of the form:
| (9) |
where Pr=probability, and Φ is the cumulative distribution function of the standard normal function. The binary indicator for accepting was yi=1 and =0 otherwise. The parameters β1, β2, and the vector μ were parameters to be estimated. We included the squared term of the incentive offer to allow for non-linearity.
The vector of controls (VC) included: age (in years), age squared, whether the individual has HIV or other STI, whether any condoms were used at the last sexual intercourse, the number of sexual partners per month, whether the last sexual intercourse occurred with someone who the respondent had just met, whether he has a stable partner, whether sex work is his main income source, whether he is a student, the highest level of education (primary=1, secondary=2, high school=3, college=4, graduate school=5), and a wealth index (which represented a continuous measure of assets and economic status constructed using the availability of: vehicle and house ownership, more than five rooms in the house, laptop and desktop computers, cable television, Internet access, and household help).
Elasticities of accepting HIV/STI prevention
The elasticity (ε) of accepting HIV/STI prevention with respect to the incentive offers was defined as the percentage change in acceptance probability divided by the percent change in the incentive offer:
| (10) |
where PrI and PrF were the probabilities of accepting the program at the initial and follow-up incentive offer levels, respectively. We estimated the elasticity for the monthly and quarterly models for all the MSM sample, and then for specific sub-groups (including MSW).
Results
Descriptive statistics
Table 1 presents the descriptive statistics for the full sample of 1,745 MSM in Mexico City. The median age was 21 years (range 18-25 years). The number of sexual partners in the last month was 3.2 men on average (median: 2). More than a third of the respondents (37%) had just met the person with whom they had the last sex act. About 12% of the sample did not use a condom at all during their last anal sexual intercourse (neither the respondent, nor their partner). A total of 37% of the respondents had a stable partner. Over 5% of the sample reported sex work as their main source of income; and 46% of respondents were students. On average, the respondents had completed high school.
Table 1.
Descriptive statistics: men who have sex with men (MSM) in Mexico Citya
| N | Mean | Median | SD | Min | Max | |
|---|---|---|---|---|---|---|
| Covariate | ||||||
| Age (in years) | 1,745 | 21.4 | 21 | 2.3 | 18 | 25 |
| Has HIV or other STIb | 1,683 | 0.094 | 0 | 0.292 | 0 | 1 |
| Any condom use at last sexual actb,c | 1,610 | 0.876 | 1 | 0.33 | 0 | 1 |
| Male sex partners (last month) | 1,745 | 3.2 | 2 | 6.1 | 1 | 139 |
| Last sex act with a partner whom respondent had just metb | 1,617 | 0.366 | 0 | 0.48 | 0 | 1 |
| Has a stable partnerb | 1,648 | 0.365 | 0 | 0.48 | 0 | 1 |
| Sex workerb | 1,487 | 0.051 | 0 | 0.22 | 0 | 1 |
| Studentb | 1,598 | 0.461 | 0 | 0.50 | 0 | 1 |
| Highest level of educationd | 1,745 | 3.1 | 3 | 0.64 | 1 | 5 |
| Wealth indexe | 1,596 | 0.00 | −0.05 | 0.77 | − 0.89 |
2.53 |
| Willingness-to-accept & economic incentive offersf,g | ||||||
| Accept monthly talks & STI tests for “α1” | 1,628 | 0.714 | 1 | 0.45 | 0 | 1 |
| α1: random monthly incentive offer (USD/month) | 1,729 | 4.66 | 4.24 | 2.90 | 0.77 | 13.88 |
| Accept monthly talks & STI tests for “α2” | 1,626 | 0.739 | 1 | 0.44 | 0 | 1 |
| α2: bargaining monthly incentive offer (USD/month) | 1,729 | 5.46 | 4.05 | 3.75 | 0.54 | 14.65 |
| Accept quarterly compensation “α3” to stay free of STI | 1,645 | 0.774 | 1 | 0.42 | 0 | 1 |
| α3: random quarterly incentive offer (USD/quarter) | 1,729 | 13.98 | 12.72 | 9 | 2.31 | 41.63 |
| Accept quarterly compensation “α4” to stay free of STI | 1,636 | 0.804 | 1 | 0.40 | 0 | 1 |
| α4: bargaining quarterly incentive offer(USD/quarter) | 1,729 | 14.92 | 10.52 | 15.31 | 1.62 | 83.27 |
Notes: SD=standard deviation; STI=sexually transmitted infection; USD=United States dollars
The full sample consists of 1,745 men who have sex with men (MSM), including male sex workers (MSW). MSM defined as a man who has had sex with another man with anal penetration within the last year.
Binary variable.
Any condom use refers to use of condoms by respondent or male partner during last anal sex.
Educational levels were: Primary =1; Middle School=2; High School=3; College=4; Graduate=5.
The wealth index was constructed using data on availability of: vehicle, own house, more than five rooms in the house, laptop and desktop computers, cable television, Internet access, and household help.
Acceptance variables were binary responses =1 if respondent says he was willing to participate in the program, and =0 if he was not. The conditional incentive offers were random offers for α1 and α3. The incentive offers for α2, and α 4 were follow-up questions: a bargaining experimental game to increase participation and/or reduce program costs by increasing the incentive offer (for those who initially said “no”) or to lower the incentive offer (for those who initially said “yes”).
Conditional incentive offer amounts are expressed in US dollars (USD) of 2008. Data collection took place during October 1-December 15, 2008 in Mexico City; the average exchange rate was 12.97 pesos per USD [29].
A total of 71.4% of respondents would attend monthly talks and undergo STI testing for an average conditional economic incentive offer α1 of $4.66 per month (range: $0.77- $13.88). Similarly, in the first bargaining question, 73.9% of respondents would attend monthly talks and undergo STI tests for an average α2 incentive of $5.46 per month (range: $0.54 - $14.65). Over three quarters of the respondents (77.4%) would (attempt to) stay free of STIs for an average compensation α3 of $13.98 (range: $2.31 - $41.63). After the second bargaining question, 80.4% of the respondents would stay free of STIs for an average compensation α4 of $14.94 per quarter (range: $1.62 - $83.27).
Graphical analysis
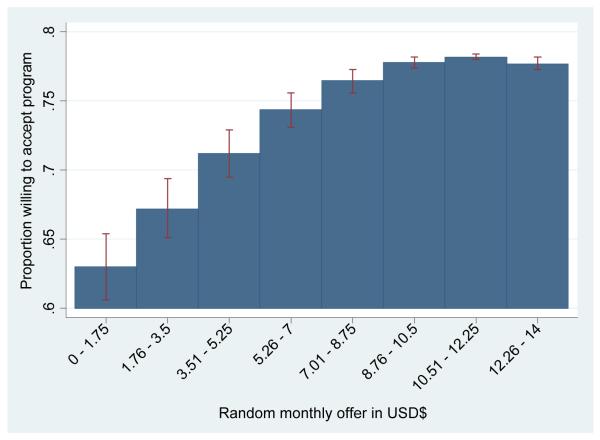
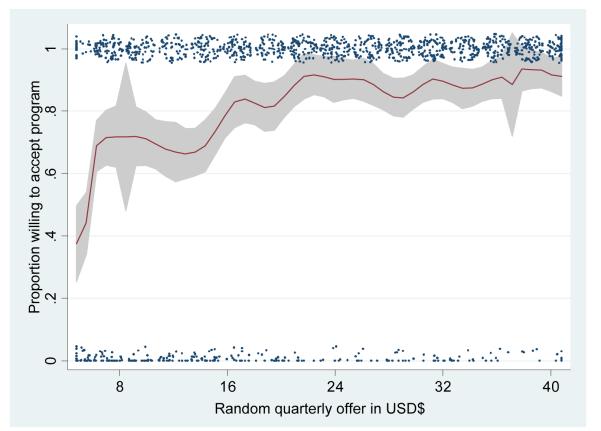
Figure 1 shows the proportion of participants willing to attend prevention talks and STI testing at different random incentive offer levels (α1). The figure shows an increasing but diminishing relation between the incentive offer levels and the willingness to participate in prevention talks and testing. At low levels of incentives ($0 - $1.75/month) the percentage willing to participate is less than 64%. Willingness to participate increases steadily to over 76% with offers of $7.1 - $8.75, but then it grows more slowly to 77% with offers of $8.76 - $10.5, to then flatten out, and even slightly decrease with the highest offers. (Appendix Figure A1 shows a nonparametric estimation, using locally weighted regression [31] for the willingness to stay free of STI as verified by quarterly tests. We can see a pattern of increasing take-up as the random incentive offer α3 increases, but then there is also evidence of decreasing marginal participation to the incentive offers).
Figure 1. Proportion willing to accept conditional economic incentives as compensation to participate in monthly HIV prevention talks and STI testing.
Notes: Analytical sample includes 1,628 individuals who stated their willingness to participate in 2-hour prevention talks each month and undergo testing for sexually transmitted infections (STI) receiving as compensation an incentive of USD$ α1 per month. The bars represent the proportion of individuals willing to accept the HIV prevention program. Error lines reflect ±1.96 standard errors.
The survey experiment
Separate incentive offer levels were distributed randomly across the participants in the survey. For example, an initial offer α3 was followed by a lowered-down offer α4=α3d if the initial response was positive; and an increased- up offer α4=α3u if the initial response was negative (see Appendix Table A1). The feasible ranges were selected on the basis of other comparable social programs in Mexico City.
The incentive offers were uncorrelated with sexual risk behaviors and other characteristics. To test if the randomization worked, we ran regressions where the dependent variables were the “treatments” (different levels and modalities of conditional economic incentive offers) and the covariates were variables that may be related to health risk and sexual risk behavior preferences. For the randomized offers (monthly incentive α1 and quarterly incentive α3), none of the regressors was significant, meaning that there was balance on observables across the randomized treatments. For the follow-up (non-random) bargaining questions (monthly incentive α2 and quarterly incentive α4) some variables were significant, as expected, because they are correlated with the propensity to accept or reject the first bid (see Appendix Table A2).
Willingness-to-accept: main results
Table 2 presents the results from the maximum likelihood estimation of Eq. (8). The results from the monthly models are presented in Panel A for an analytical sample of n=1,573 MSM participants who responded to the relevant questions, followed by the quarterly model in Panel B for n=1,599 participants. In the implied yearly model, Panel C, for the entire sample of MSM the optimal willingness-to-accept was $297.8/year and it was reduced to $287.9 when covariates were introduced. The optimal willingness-to-accept was lower for the MSW only subgroup: $155.5/year in the unadjusted model, and $148.3 when adjusting for covariates. In the MSW+ group (MSW plus respondents with 5 or more sexual partners/month) the optimal willingness-to-accept was $213 and $215 in the unadjusted and the adjusted models respectively.
Table 2.
Double-bounded dichotomous choice model estimates of willingness-to-accept conditional incentives (USD$) for prevention of HIV & other STIs among MSM in Mexico City
| Point estimate (USD$) |
95% Confidence interval (USD$) |
N | Covariates | ||
|---|---|---|---|---|---|
| Monthly model: prevention talks and STI testing | |||||
| All MSM participants | 9.5 | 9.1 | 9.9 | 1,573 | No |
| All MSM participants | 9.3 | 7.3 | 11.6 | 1,120 | Yes |
| Male sex workers | 6.8 | 5.9 | 7.8 | 75 | No |
| Male sex workers | 7.4 | 2.5 | 20.2 | 64 | Yes |
| MSW or sex partners/month >=5 | 8.1 | 7.3 | 8.9 | 214 | No |
| MSW or sex partners/month >=5 | 8.0 | 6.2 | 9.7 | 180 | Yes |
| Quarterly Model: staying free of STIs verified by STI testing | |||||
| All MSM participants | 46.0 | 42.9 | 49.0 | 1,599 | No |
| All MSM participants | 44.0 | 37.5 | 50.7 | 1,130 | Yes |
| Male sex workers | 18.4 | 15.0 | 21.8 | 76 | No |
| Male sex workers | 15.0 | – | 45.8 | 64 | Yes |
| MSW or sex partners/month >=5 | 29.0 | 24.6 | 33.3 | 215 | No |
| MSW or sex partners/month >=5 | 29.8 | 18.7 | 41.1 | 178 | Yes |
| Implied combination yearly model: prevention talks, staying free of STIs, and STI testing | |||||
| All MSM participants | 297.8 | 281.2 | 314.4 | 1,573 | No |
| All MSM participants | 287.9 | 238.4 | 342.4 | 1,120 | Yes |
| Male sex workers | 155.5 | 130.6 | 180.3 | 75 | No |
| Male sex workers | 148.3 | 30.6 | 426.3 | 64 | Yes |
| MSW or sex partners/month >=5 | 213.0 | 186.5 | 239.6 | 214 | No |
| MSW or sex partners/month >=5 | 215.1 | 149.1 | 280.4 | 178 | Yes |
Notes: MSM= men who have sex with men; MSW=male sex worker
Amounts expressed in USD$ of October-December 2008 using average exchange rate of 12.97 pesos per $1 USD.
Table presents results from double-bounded dichotomous choice model estimated in Stata 11 MP, 64 bit.
Models estimated by maximum likelihood based with a modified “doubleb” Stata ado file for willingness to pay [50].
Monthly model data refers to random incentive offer α1 and bargaining incentive offer α2 to attend HIV/STI prevention talks and STI testing.
Quarterly model data refers to random incentive offer α3 and bargaining incentive offer α4 to stay free of STIs, verified by quarterly STI testing.
Determinants of the acceptance of HIV/STI prevention
Table 3 reports marginal effects from probit regression models of the responses (0=no and 1=yes) of whether participants would accept different modalities of HIV/STI prevention programs on the conditional incentive offers (expressed in USD$), their squares, and the full set of covariates. Column (1) shows the results of whether the participants would attend monthly prevention talks and undergo STI testing for the incentive offer of α1 for a smaller analytical sample with covariates of n=1,153. The sample size is reduced because not all participants responded to all the questions for the covariates (we discuss this issue in detail below). The coefficient on the incentive offer was positive and significant; and the effect of the incentives on participation was non-linear: the squared term was negative and significant. In addition, men who said that they had HIV or another STI were significantly less likely to accept, whereas those whose last sexual partner was someone they had just met were more likely to accept.
Table 3.
Determinants of willingness-to-accept HIV/STI prevention with conditional economic incentives among MSMa in Mexico City
| (1) Accept monthly talks & STI tests for random $α1 per month |
(2) Accept monthly talks & tests for bargaining incentive $α2 per month |
(3) Accept to stay free of STIs for random incentive $α3 per quarter |
(4) Accept to stay free of STI for bargaining incentive $α4 per quarter |
|
|---|---|---|---|---|
| Conditional incentive | 0.0750 | 0.0519 | 0.0326 | −0.0085 |
| [0.015]** | [0.015]** | [0.005]** | [0.003]** | |
| Conditional incentive squared | −0.0066 | −0.0069 | −0.0009 | −0.0000 |
| [0.001]** | [0.001]** | [0.000]** | [0.000] | |
| Age (in years) | 0.0248 | 0.0030 | −0.0304 | −0.0232 |
| [0.118] | [0.117] | [0.106] | [0.105] | |
| Age squared | −0.0009 | −0.0002 | 0.0005 | 0.0005 |
| [0.003] | [0.003] | [0.002] | [0.002] | |
| Has HIV or STIb | −0.1470 | 0.0276 | −0.0432 | 0.0155 |
| [0.053]** | [0.044] | [0.046] | [0.040] | |
| Any condom use at last sexual act b,c |
−0.0015 | 0.0314 | 0.0097 | 0.0561 |
| [0.041] | [0.040] | [0.037] | [0.038] | |
| Male sex partners (last month) | 0.0005 | 0.0137 | 0.0020 | −0.0013 |
| [0.002] | [0.004]** | [0.002] | [0.002] | |
| Last sex act with a partner whom respondent had just metb |
0.0622 | −0.0420 | −0.0133 | −0.0168 |
| [0.028]* | [0.028] | [0.026] | [0.025] | |
| Has a stable partnerb | −0.0287 | 0.0023 | 0.0022 | −0.0105 |
| [0.029] | [0.028] | [0.026] | [0.025] | |
| Sex workerb | −0.0202 | −0.1735 | −0.0648 | −0.0039 |
| [0.066] | [0.090]+ | [0.064] | [0.057] | |
| Studentb | −0.0043 | −0.0300 | −0.0058 | 0.0303 |
| [0.029] | [0.027] | [0.026] | [0.025] | |
| Highest level of educationd | −0.0192 | −0.0158 | −0.0231 | −0.0005 |
| [0.023] | [0.024] | [0.021] | [0.021] | |
| Wealth indexe | −0.0020 | −0.0158 | −0.0171 | −0.0142 |
| [0.019] | [0.017] | [0.017] | [0.016] | |
| Observations | 1,153 | 1,148 | 1,158 | 1,149 |
| Pseudo R-squared | 0.0483 | 0.147 | 0.0651 | 0.137 |
| Probability | 0.735 | 0.763 | 0.788 | 0.815 |
Notes: Table presents probit regression marginal effects. Robust standard errors in brackets:
p<0.01,
p<0.05,
p<0.1
The analytical samples consist of men who have sex with men (MSM), including male sex workers (MSW) with all the relevant covariate information. MSM defined as a man who has had sex with another man with anal penetration within the last year. The conditional incentive offers were random offers for α1 and α3. The incentive offers for α2, and α 4 were follow-up questions: a bargaining experimental game to increase participation and/or reduce program costs by increasing the incentive offer (for those who initially said “no”) or to lower the incentive offer (for those who initially said “yes”). Conditional incentive offer amounts are expressed in US dollars (USD) of 2008. Data collection took place during October 1-December 15, 2008 in Mexico City; the average exchange rate was 12.97 pesos per USD [29]
Binary variable.
Any condom use refers to use of condoms by respondent or male partner during last anal sex.
Educational levels were: Primary =1; Middle School=2; High School=3; College=4; Graduate=5.
The wealth index was constructed using data on availability of: vehicle, own house, more than five rooms in the house, laptop and desktop computers, cable television, Internet access, and household help.
In the second column, we can see the results of the first bargaining question. Those who accepted the program at the first random incentive were given a lower incentive offer, and those who rejected the program at first were offered a higher incentive. The marginal effect of the incentive offer was still positive, slightly smaller in magnitude, and non-linear as before. Those with more partners were more willing to participate in the program, while those whose main source of income was sex work were less likely to have a positive response.
Column (3) presents the model for n= 1,158 for the question on willingness to stay free of STIs verified with quarterly STI testing. Here also the incentive offer levels were positively related to the willingness to participate, and there was evidence of diminishing participation rates. The fourth column presents the results of the second bargaining question. The correlation between the follow-up offer and the willingness to participate was negative, suggesting that higher incentives led generally to lower participation rates. This result can be explained in terms of the endogeneity of the higher offers in α4, which were by design, more likely to be received among those who initially rejected the initial offers α3.
The possible differences between the full and the analytical samples deserve further analyses. Even though individually we did not lose a lot of sample for each covariate (Table 1), when all of the covariates were taken together there was considerable loss of sample (almost a third of the initial respondents): the analytical sample with covariates includes only 1,153 participants. Thus, we tested if those not included in the analyses were different from the included. The participants included in the analytical sample were less likely to have HIV or another STI (8.24% vs. 11.9%, p=0.0172); they were more likely to have more sexual partners in the last month (3.4 vs. 2.7, p=0.037); they had slightly lower level of formal education (3.01 vs. 3.12, p=0.0009), though both groups still had just completed high school; and they were better off in terms of the material assets index (0.0279 vs. -0.0727, p=0.01). Taken together the differences between the full sample and the analytical samples did not seem to exhibit a general tendency towards a more or less healthy or risky group (since they had less HIV/STI, but more sexual partners), or a more or less disadvantaged group (given they had slightly lower level of education, but also they were slightly better off in terms of material assets). Perhaps most importantly, the WTA estimates did not seem to be greatly affected: in Table 2, the point estimates were very close when comparing full sample (without covariates) and analytical sample (with covariates) for both the monthly and the quarterly models, although as expected the confidence intervals were larger in the models with covariates (and smaller sample size).
Elasticitiy of accepting HIV/STI prevention programs
Table 4 presents the incentive elasticities of participation demand. The estimated elasticity took full advantage of the experimental change in the incentive offers and the corresponding change in participation probabilities. For the monthly model (prevention talks and STI testing) the elasticity was 0.222; while in the quarterly model (to stay free of STIs verified with testing) it was 0.515.
Table 4.
Elasticity of accepting HIV/STI prevention program activities with respect to conditional economic incentive offers
| Unadjusted modelsa |
Adjusted modelsb |
|
|---|---|---|
| Monthly model: elasticity of accepting talks and STI tests | ||
| Percentage change in acceptance probability | 0.035 | 0.038 |
| Percentage change in incentive offer | 0.172 | 0.172 |
| Elasticity 1 | 0.203 | 0.222 |
| Quarterly model: elasticity of accepting to stay free of STIs | ||
| Percentage change in acceptance probability | 0.038 | 0.034 |
| Percentage change in incentive offer | 0.067 | 0.067 |
| Elasticity 2 | 0.569 | 0.515 |
Notes: In the unadjusted model probabilities and incentives are taken directly from descriptive statistics in Table 1.
For the adjusted models, the marginal effects are from probit regressions columns that control for all covariates as presented in Table 5: columns (1) and (2) for the monthly model, and (3) and (4) for the quarterly model.
Heterogeneity Analysis
Table 5 presents stratified analyses for: A) participants at highest risk: MSW+ defined as male sex workers or those with five or more sexual partners per month; B) respondents who currently have an STI or live with HIV; C) the low-wealth sample: below 25 percentile in the wealth index; D) participants without appropriate condom use; and E) those without correct knowledge about HIV/STI.
Table 5.
Heterogeneity Analysis
|
A. Sub-sample 1: MSW+ at highest
risk b |
(1) Accept monthly talks & STI tests for random $α1 per month |
(2) Accept monthly talks & tests for bargaining incentive $α2 per |
(3) Accept to stay free of STIs for random incentive $α3 per quarter month |
(4) Accept to stay free of STI for bargaining incentive $α4 per quarter |
|---|---|---|---|---|
| Conditional incentive | 0.0838 | 0.0674 | 0.0470 | −0.0098 |
| [0.0346]* | [0.0361]+ | [0.0115]** | [0.0077] | |
| Conditional incentive squared | −0.0037 | −0.0071 | −0.0009 | 0.0001 |
| [0.0025] | [0.0031]* | [0.0003]** | [0.0001] | |
| Observations | 184 | 182 | 185 | 178 |
| Pseudo R-squared | 0.120 | 0.170 | 0.135 | 0.088 |
| Acceptance probability | 0.734 | 0.791 | 0.757 | 0.809 |
| Elasticities | 0.436 | −1.545 | ||
| B. Sub-sample 2: Has HIV or STI c | ||||
|
| ||||
| Conditional incentive | 0.1333 | 0.0905 | 0.0679 | 0.0390 |
| [0.074]+ | [0.042]* | [0.019]** | [0.018]* | |
| Conditional incentive squared | −0.0084 | −0.0088 | −0.0017 | −0.0011 |
| [0.006] | [0.003]** | [0.001]** | [0.000]* | |
| Observations | 94 | 94 | 95 | 97 |
| Pseudo R-squared | 0.189 | 0.280 | 0.215 | 0.351 |
| Acceptance probability | 0.606 | 0.777 | 0.747 | 0.835 |
| Elasticities | 0.953 | 1.87 | ||
| C. Sub-sample 3:Low-wealth population d | ||||
|
| ||||
| Conditional incentive | 0.1734 | 0.0795 | 0.0520 | −0.0049 |
| [0.032]** | [0.030]** | [0.009]** | [0.006] | |
| Conditional incentive squared | −0.0140 | −0.0087 | −0.0014 | −0.0000 |
| [0.003]** | [0.002]** | [0.000]** | [0.000] | |
| Observations | 266 | 260 | 266 | 259 |
| Pseudo R-squared | 0.129 | 0.188 | 0.165 | 0.106 |
| Acceptance probability | 0.729 | 0.804 | 0.793 | 0.834 |
| Elasticities | 0.506 | 2.03 | ||
| D. Sub-sample 4: without “appropriate” condom use e | ||||
|
| ||||
| Conditional incentive | 0.0538 | 0.0555 | 0.0328 | −0.0089 |
| [0.032]+ | [0.029]+ | [0.009]** | [0.006] | |
| Conditional incentive squared | −0.0056 | −0.0073 | −0.0010 | −0.0000 |
| [0.002]* | [0.002]** | [0.000]** | [0.000] | |
| Observations | 315 | 312 | 321 | 313 |
| Pseudo R-squared | 0.0475 | 0.185 | 0.109 | 0.203 |
| Acceptance probability | 0.717 | 0.756 | 0.791 | 0.792 |
| Elasticities | 0.307 | 0.014 | ||
| E. Sub-sample 5: Only those without appropriate knowledge of HIV/STI f | ||||
|
| ||||
| Conditional incentive | 0.0784 | 0.0521 | 0.0323 | −0.0040 |
| [0.019]** | [0.019]** | [0.006]** | [0.004] | |
| Conditional incentive squared | −0.0062 | −0.0068 | −0.0009 | −0.0001 |
| [0.002]** | [0.001]** | [0.000]** | [0.000] | |
| Observations | 712 | 709 | 717 | 712 |
| Pseudo R-squared | 0.0461 | 0.149 | 0.0647 | 0.153 |
| Observed probability (WTA) | 0.711 | 0.769 | 0.787 | 0.820 |
| Elasticities | 0.41 | 1.36 | ||
Notes: Table presents probit regression marginal effects. Robust standard errors in brackets:
p<0.01,
p<0.05,
p<0.1
The analytical subsamples consist of men who have sex with men (MSM), including male sex workers (MSW). MSM defined as a man who has had sex with another man with anal penetration within the last year. The conditional incentive offers were random offers for α1 and α3. The incentive offers for α2, and α 4 were follow-up questions: a bargaining experimental game to increase participation and/or reduce program costs by increasing the incentive offer (for those who initially said “no”) or to lower the incentive offer (for those who initially said “yes”). Conditional incentive offer amounts are expressed in US dollars (USD) of 2008. Data collection activities took place during October 1-December 15, 2008 in Mexico City; the average exchange rate was 12.97 pesos per USD [29]
Sample population at the highest risk was defined as male sex workers or those with 5 or more sexual partners per month.
Participants who declared to currently having been infected with HIV or with other sexually transmitted infection (STI).
Low-wealth sample were participants with a wealth index below the 25 percentile of the distribution; the wealth index was constructed using data on availability of: vehicle, own house, more than five rooms in the house, laptop and desktop computers, cable television, Internet access, and household help.
Appropriate condom use during the last sex act was defined as when respondent used a condom when he had a penetrative role only, or when partner used it when respondent had a receptive role only, or when both used it regardless of sexual roles.
Correct knowledge (yes/no) was based on a battery of questions about HIV and sexually transmitted infections (STIs).
The elasticities summarize the information on the response coefficients for the first and the second incentive offers under each model, for each sub-sample. Note that for all the subgroups the elasticities were higher in magnitude than those for full sample of MSM participants. The elasticity to attend monthly prevention talks and undergo STI tests with respect to the incentive offer was highest (0.953) among those who already have an STI or live with HIV. The incentive offer elasticity for accepting to stay free of STIs verified by quarterly STI testing was highest (2.03) for the low-wealth population; and it was negative (−1.545) for the group at highest risk (MSW+).
Discussion
Although effective HIV prevention interventions exist, low take-up rates are a common problem, particularly among populations of limited resources where other competing needs are pressing. Conditional economic incentives seem to be a potentially useful tool to complement traditional approaches. Thornton (2008) has shown that small economic incentives ($0.1 - $0.2) can double HIV test-result learning from a baseline of 34% in rural Malawi [32]. Baird and colleagues (2010 & 2012) showed that incentives of about $10/month to stay in secondary school also in rural Malawi reduced onset of sexual activity by 38% among young women [33]; and their more recent results suggest the program is protective in terms of STI and HIV prevalence [4]. Similarly, in rural Tanzania among a heterosexual population, de Walque et al (2012) showed that the combined prevalence of four curable STI was reduced in a high CEI group [5]. Although some CEI targeted specifically for HIV prevention have been implemented, the methods to estimate ex ante the optimal incentive levels are still being developed. Also, we need to test CEI among groups with the highest HIV risks and prevalence rates such as MSM and MSW in concentrated epidemics. Although the CEI were not shown to be protective for HIV in Tanzania with a heterosexual population, with a relatively low HIV incidence and prevalence rate, an incentives program may be effective among MSM and MSW in Mexico where the incidence rates are much higher, and where prevalence has been documented to be in the 20-30% range [34].
The present study contributes to the literature by adapting the willingness to pay / willingness-to-accept methodology to the context of HIV/STI prevention with incentives. We implement WTA methods for the groups most at risk in Mexico showing the minimum CEI levels needed for participants to sign-up, get tested, attend prevention workshops and possibly reduce HIV risk behaviors. The results show preliminary evidence for policy development in the HIV prevention field in Mexico, with potential implications for other concentrated epidemic settings, focusing particularly on MSM and MSW. As CEI for HIV prevention are implemented more widely, it will be important that the appropriate levels of incentives are set taking into account the particular characteristics of the populations and the socio-economic context.
In general the models show a positive coefficient between incentives and the acceptance probabilities. The overall results seem to be robust to different types of analyses (parametric and non-parametric) as well as stratification. The optimal willingness-to-accept for the full MSM sample was estimated at $9.3/month for monthly talks and testing; $44/qtr. for staying free of STIs and quarterly STI testing; with an implied $288/year for a combined yearly program. Nevertheless, there was considerable heterogeneity, with male sex workers and those with five or more sexual partners actually exhibiting lower willingness-to-accept estimates. While the incentive elasticity of participation for monthly talks was 0.222; that for quarterly STI testing and staying free of STIs was of 0.515, meaning that a 10% increase in the incentive offer increased potential participation rates by 5.15%. However, again, there was considerable heterogeneity across different sub-groups. Not surprisingly, for some of the sub-groups (e.g., those with lowest wealth) the acceptance rates were highly elastic.
The counter intuitive negative elasticity for MSW+ in the quarterly model was likely due to a combination of the relatively small sample size, the inherently endogenous nature of the follow-up questions, question ordering, and the perceived high need by the most at risk populations. The sample size for the MSW+ subgroup was n=178 and thus “the law of small numbers” may apply [35], whereby outliers and unusual responses may be more prevalent. Also, recall that α4 is a follow up bargaining game, so if MSW said “no” to α3 then they would have been offered a higher-up α4; but given the constrained nature of the bargaining game, perhaps not high enough to make them switch to yes. This creates a selection issue or endogeneity by which those who initially refused quarterly testing may be more likely to refuse again the follow up question. In addition, one of the drawbacks of the present study is that the question order was not random, so that the sequence was always the same: ask first about offers for monthly talks and checkups, and then quarterly testing to stay free of STIs. Hence, MSW may rationally prefer only monthly visits without STI test conditionality given their higher likelihood of testing positive for STIs. Finally, the some of the effect may come from initially positive responses to α3 followed by also positive responses to α4 because some MSW may be very conscious of the need and potential benefit that quarterly STI testing and treatment may have for them: thus, they would accept the testing (and free treatment) even at very low incentive offers.
In HIV epidemics, it is possible that transmission can be driven by a small group of high-risk individuals who could render ineffective an otherwise seemingly successful intervention (with, say, 90% take-up). Appendix Table A3 shows the characteristics of the “never-takers” (those who refused all programs presented to them) and compares it to the “sometime-takers”. The never-takers were 9% of the sample. Any condom use was lower among the never-takers (81% vs. 88%, p=0.0172); however, appropriate condom use was not statistically different (not shown). Never-takers were less likely to be students (38% vs. 47%, p=0.0433); and more likely to have higher levels of education (3.16 vs. 3.04, p=0.029). Hence, a clear policy recommendation emerging from the results would be not to target CEI to the small proportion of never-takers (MSM of higher socio economic status). Instead, CEI may be more effective if targeted to MSM of lower socio-economic status including street-based male sex workers, who are more likely to have less education and may be generally more interested in financial incentives.
Within the sampled population, there is a relatively large group without appropriate knowledge of HIV/STI (about 700 individuals in a sample of 1,745). Thus, lack of accurate information seems to continue to be an important issue in this community, and thus, the effective provision of it should be part of prevention programs. Nevertheless, correct knowledge is only a necessary, and not a sufficient condition for effective HIV prevention [36]. Knowledge alone may not be enough to spur protective behaviors to reduce HIV risks and that is why information, education and communication efforts should be tested in conjunction with other structural approaches such as conditional economic incentives.
It is not straight forward to compare our results with previous literature. The literature on HIV prevention among MSM/MSW in concentrated epidemics is relatively scarce. Systematic reviews in the HIV prevention field generally suggest that behavioral effects are more common, while HIV incidence effects are more difficult to document [37-39]. The literature on prevention with male sex workers is also limited, particularly as it refers to economic interventions [40,41]. Hence, additions to the literature, particularly on incentives and other structural interventions should be a welcome development. There is not much against to compare in terms of effectiveness of HIV prevention for MSM/MSW, much less in terms of cost-effectiveness [42]. More research is needed documenting the effectiveness of structural approaches for HIV prevention among MSM and MSW, as well as its cost-effectiveness.
Similarly, to the best of our knowledge, no other estimates exist for the HIV-prevention-program-uptake elasticity with respect to the incentive offer. In the broader literature of CCT and education, one study using data from PROGRESA/Oportunidades shows the effects of doubling and halving the incentive levels, and finds that mean years of schooling completed are linearly increasing with the incentive amounts, but at a decreasing rate [43]. Moreover, for Brazil, another study finds nonlinear effects after doubling and quadrupling the incentive level, but with successively smaller effects on the probability of attending school [44]. Similarly, for Cambodia, there is evidence of diminishing marginal returns to the transfer size [45].
The current research has limitations. First, the sample may not be representative of the entire MSM or MSW populations in Mexico City, but only of the persons present at the meeting places and times where data collection took place. Second, uncertainty about the possibility of eliciting true preferences is an inherent limitation in this type of research, including “hypothetical bias” whereby WTA studies may produce ‘inflated’ estimates of the amounts the individuals might accept in real life; and conversely, actual compliance in an intervention may be importantly different than that anticipated from responses during a survey experiment [46-48]. Still, these stated-preference techniques may be useful for prospective valuation of non-tangible goods and services with missing or incomplete markets, and we have adapted them to gauge the prospects for behavior change related to HIV risks. Also, some biases may occur as a positive response may be given simply because that is the “socially desirable” answer. Some of those biases were reduced in this research by letting the respondents use computer-assisted self-interview technology. Third, this study was not able to collect biomarkers for HIV and STI, which would have given an important perspective to understand the responses to the survey experiment. Lastly, as mentioned before, the WTA question order was not randomized, which may have created some biases or framing effects [49,27], particularly for one of the most at risk subgroups: MSW.
The present study has important implications. First, new and innovative methods for HIV prevention, particularly those improving take-up of known effective technologies could be implemented using CEI among populations at high risk of infection in concentrated HIV epidemics. Second, WTA methods can be tailored to inform specific prevention programs including, as presented here, participation in workshops and remaining free of STIs (verified through periodic STI testing) among populations at high risk and low socio-economic status. Third, the preliminary results suggest that the target population would accept HIV/STI prevention programs and potential reductions in sexual risk behaviors in exchange for CEIs; this quantitative research corroborates formative qualitative work conducted earlier [28].
Conclusions
Methods from resource economics and contingent valuation can be adapted to help inform HIV prevention programs using economic incentives. The results of this survey experiment confirm that demand for HIV prevention can be positively incentivized using conditional cash transfer programs specifically targeted to populations at the highest risk of infection. The potential impact of economic incentives and their initial acceptance can vary considerably based on socio-economic situation and the type of population being targeted. The proposed incentive levels are feasible amounts in comparison to other social assistance programs in Mexico City, including programs for other marginalized populations such as low-income single mothers and elderly adults. Mexico, a global leader in conditional cash transfers for human development and poverty reduction, could extend that successful model for targeted HIV/STI prevention.
Because appropriate knowledge may be lacking among some of the populations at highest risk, correct information and condom distribution should be considered as essential in HIV prevention programs, but may work best coupled with structural interventions such as conditional economic incentives. Given the evidence presented, CEI may work best among specific, populations at high risk of HIV infection, such as street-based male sex workers. Testing and education alone may not be sufficient for HIV prevention; thus there is a need to rigorously test conditional economic incentives programs in concentrated epidemics in general, and with male sex workers in particular. These programs have the potential to confer health benefits to individual sex workers, but may also generate wider benefits given the potential impact on male clients as well as male and female non-commercial partners.
Acknowledgments
Useful comments were provided by Jim Berry, Will Dow, Jason Fletcher, Ralph Gonzales, Sandi McCoy, Kevin Volpp, two anonymous referees, and participants at seminars (Mexican School of Public Health, University of California-San Francisco, University of Pennsylvania, Yale University, and University of North Carolina-Chapel Hill) and conferences (7th World Congress of the International Health Economics Association –iHEA--, 3rd biennial American Society of Health Economists –ASHE--, and the XVIII AIDS International Conference). We particularly thank the survey respondents in Mexico City; as well as Luis Pozo-Urquizo, Paola Olivieri, Edgar ávila and Moisés Calderón of La Manta de México for their involvement in data collection and field work. Research assistance was provided by Fernando Alarid-Escudero. The questionnaire was programmed into the hand-held devices by Edgar Díaz and his team at CEO/Mexico. Alejandro López-Feldman provided additional background material to adapt the Stata ado file “doubleb.” The project benefitted from input of faculty and staff at the Institute of Business and Economic Research (IBER) and the Experimental Social Science Laboratory (X-Lab) at UC Berkeley.
We gratefully acknowledge funding from the U.S. National Institutes of Health/Fogarty International Center (Grant No. K01-TW008016-04 PI: Galárraga); and Mexican National Center for HIV/AIDS Control and Prevention (CENSIDA, Prevention Grant 2008).
APPENDICES. Appendix Exhibit A: Willingness-to-accept Questions (Survey Instrument)
Intro1
We are designing a new prevention program where we would invite you to monthly talks on HIV prevention. We would offer you a payment whenever you attend the talk. If we offered you this program, would you be interested in participating?
Yes =1 No =0
Intro2
Another type of program that we are considering would be similar to the previous one, but in addition to the payment for attending monthly talks & testing, we would offer you a compensation every 3 months if you were free of any curable sexually transmitted infections (verified with quarterly testing). If we offered you this program, you would be interested in participating?
Yes =1 No =0
PLEASE REMEMBER THAT THE FUNDING FOR THIS TYPE OF PROGRAM IS LIMITED; IF A FUTURE PROGRAM HAS HIGH COSTS, IT MAY NOT BE IMPLEMENTED. PLEASE THINK HARD ABOUT THE MINIMUM PAYMENT OR COMPENSATION THAT WOULD ALLOW YOU TO PARTICIPATE AND TO TRY TO STAY FREE OF SEXUALLY TRANSMITTED INFECTIONS BY USING CONDOMS MORE FREQUENTLY OR REDUCING THE NUMBER OF SEXUAL PARTNERS.
1. WOULD YOU ACCEPT “α1” PESOS PER MONTH AS A COMPENSATION FOR YOUR TIME IN PARTICIPATING IN MONTHLY HIV PREVENTION TALKS AND TESTS?
Yes =1 or No =0
computer will randomly pick number “α1” from list: 0-200 pesos in 25-peso intervals
if answer to Q.1 is yes, then computer proposes a lowered-down incentive α1d = α2 = α1 * 0.7
if answer to Q.1 is no, then computer proposes a higher-up incentive: α1u = α2 = (200 + α1) /2
2. WOULD YOU ACCEPT “α2” PESOS PER MONTH AS A COMPENSATION TO PARTICIPATE IN MONTHLY HIV PREVENTION TALKS AND TESTS?
Yes =1 No =0
3. WOULD YOU ACCEPT “α3” PESOS EVERY THREE MONTHS AS A COMPENSATION TO STAY FREE OF STIs (VERIFIED BY BIOLOGICAL TESTS)?
Yes =1 No =0
computer will provide random number “α3”as follows: α3 = α1*3
if answer to Q.3 is yes, then computer proposes a lowered-down incentive: α3d = α4= α3*0.7
if answer to Q.4 is no, then computer proposes a higher-up incentive such that: α3u = α4= α3*2
4. WOULD YOU ACCEPT “α4” PESOS EVERY THREE MONTHS AS A COMPENSATION TO STAY FREE OF STIs (VERIFIED BY BIOLOGICAL TESTS)?
Yes =1 No =0
Appendix Table A1.
Alternative incentive offers to stay free of STI, verified by quarterly testing
| (In Mexican pesos) | (in USD$) | ||||
|---|---|---|---|---|---|
|
α4 |
α4 |
||||
| α3 | α3d | α3u | α3 | α3d | α3u |
| 30 | 21 | 60 | 2.3 | 1.6 | 4.6 |
| 45 | 31.5 | 90 | 3.5 | 2.4 | 6.9 |
| 60 | 42 | 120 | 4.6 | 3.2 | 9.3 |
| 75 | 52.5 | 150 | 5.8 | 4.0 | 11.6 |
| 90 | 63 | 180 | 6.9 | 4.9 | 13.9 |
| 105 | 73.5 | 210 | 8.1 | 5.7 | 16.2 |
| 120 | 84 | 240 | 9.3 | 6.5 | 18.5 |
| 135 | 94.5 | 270 | 10.4 | 7.3 | 20.8 |
| 150 | 105 | 300 | 11.6 | 8.1 | 23.1 |
| 165 | 115.5 | 330 | 12.7 | 8.9 | 25.4 |
| 180 | 126 | 360 | 13.9 | 9.7 | 27.8 |
| 195 | 136.5 | 390 | 15.0 | 10.5 | 30.1 |
| 210 | 147 | 420 | 16.2 | 11.3 | 32.4 |
| 225 | 157.5 | 450 | 17.3 | 12.1 | 34.7 |
| 240 | 168 | 480 | 18.5 | 13.0 | 37.0 |
| 255 | 178.5 | 510 | 19.7 | 13.8 | 39.3 |
| 270 | 189 | 540 | 20.8 | 14.6 | 41.6 |
| 285 | 199.5 | 570 | 22.0 | 15.4 | 43.9 |
| 300 | 210 | 600 | 23.1 | 16.2 | 46.3 |
| 315 | 220.5 | 630 | 24.3 | 17.0 | 48.6 |
| 330 | 231 | 660 | 25.4 | 17.8 | 50.9 |
| 345 | 241.5 | 690 | 26.6 | 18.6 | 53.2 |
| 360 | 252 | 720 | 27.8 | 19.4 | 55.5 |
| 375 | 262.5 | 750 | 28.9 | 20.2 | 57.8 |
| 390 | 273 | 780 | 30.1 | 21.0 | 60.1 |
| 405 | 283.5 | 810 | 31.2 | 21.9 | 62.5 |
| 420 | 294 | 840 | 32.4 | 22.7 | 64.8 |
| 435 | 304.5 | 870 | 33.5 | 23.5 | 67.1 |
| 450 | 315 | 900 | 34.7 | 24.3 | 69.4 |
| 465 | 325.5 | 930 | 35.9 | 25.1 | 71.7 |
| 480 | 336 | 960 | 37.0 | 25.9 | 74.0 |
| 495 | 346.5 | 990 | 38.2 | 26.7 | 76.3 |
| 510 | 357 | 1020 | 39.3 | 27.5 | 78.6 |
| 525 | 367.5 | 1050 | 40.5 | 28.3 | 81.0 |
| 540 | 378 | 1080 | 41.6 | 29.1 | 83.3 |
Notes: The table presents the full set of quarterly incentive offers to stay free of STIs verified by quarterly STI testing. Converted from Mexican pesos of Oct-Dec. 2008 to USD$ at the average exchange rate of 12.97 pesos per USD. Initial incentive offer (α3) followed by a lowered-down offer (α3d) if initial response was yes, or followed by an increased-up offer (α3u) if initial response was no.
Appendix Table A2.
Testing the balance of observables across incentive offersa
| (1) Random monthly incentive offer (α1) |
(2) Bargaining monthly incentive offer (α2) |
(3) Random quarterly incentive offer (α3) |
(4) Bargaining quarterly incentive offer (α4) |
|
|---|---|---|---|---|
| Age (in years) | 0.0042 | 0.0986 | 0.0127 | 0.0466 |
| [0.0444] | [0.0538]+ | [0.1332] | [0.1909] | |
| Has HIV or STIb | −0.0009 | 1.1611 | −0.0026 | 1.0348 |
| [0.3255] | [0.3956]** | [0.9766] | [1.6794] | |
| Any condom use at last sexual actb,c | −0.2149 | 0.0239 | −0.6447 | −1.9480 |
| [0.3066] | [0.4097] | [0.9198] | [1.7390] | |
| Male sex partners (last month) | −0.0025 | −0.0150 | −0.0076 | −0.0958 |
| [0.0124] | [0.0234] | [0.0372] | [0.0449]* | |
| Last sex with someone just metc | 0.0495 | −0.5031 | 0.1484 | −0.0454 |
| [0.2010] | [0.2587]+ | [0.6030] | [0.9773] | |
| Has a stable partnerb | 0.1083 | 0.2501 | 0.3249 | −0.2354 |
| [0.2067] | [0.2664] | [0.6202] | [1.0207] | |
| Sex workerb | −0.5113 | −0.0329 | −1.5339 | −2.5095 |
| [0.3560] | [0.4870] | [1.0680] | [1.1144]* | |
| Studentb | −0.0160 | 0.0170 | −0.0479 | −0.8064 |
| [0.2126] | [0.2556] | [0.6377] | [0.9912] | |
| Highest level of educationc | 0.2344 | 0.6055 | 0.7031 | 1.4872 |
| [0.1787] | [0.2137]** | [0.5362] | [0.8940]+ | |
| Has correct knowledgeb,f | −0.2326 | −0.4491 | −0.6977 | −0.6633 |
| [0.2539] | [0.2994] | [0.7617] | [1.2009] | |
| Wealth indexe | 0.1586 | 0.1500 | 0.4759 | 1.6207 |
| [0.1429] | [0.1760] | [0.4287] | [0.7414]* | |
| Constant | 4.0089 | 1.4348 | 12.0268 | 11.0874 |
| [0.9790]** | [1.2247] | [2.9369]** | [4.7299]* | |
| Observations | 900 | 900 | 900 | 900 |
| R-squared | 0.011 | 0.042 | 0.011 | 0.025 |
Notes: Table presents results from linear regression where dependent variables were the conditional incentive offers in USD.
Robust standard errors in brackets:
p<0.01,
p<0.05,
p<0.1
The analytical sample consists of men who have sex with men (MSM), including male sex workers (MSW) with the relevant covariates. MSM defined as a man who has had sex with another man with anal penetration within the last year. The conditional incentive offers were random offers for α1 and α3. The incentive offers for α2, and α 4 were follow-up questions: a bargaining experimental game to increase participation and/or reduce program costs by increasing the incentive offer (for those who initially said “no”) or to lower the incentive offer (for those who initially said “yes”). Conditional incentive offer amounts are expressed in US dollars (USD) of 2008. Data collection took place during October 1-December 15, 2008 in Mexico City; the average exchange rate was 12.97 pesos per USD [29]
Binary variable.
Any condom use refers to use of condoms by respondent or male partner during last anal sex.
Educational levels were: Primary =1; Middle School=2; High School=3; College=4; Graduate=5.
The wealth index was constructed using data on availability of: vehicle, own house, more than five rooms in the house, laptop and desktop computers, cable television, Internet access, and household help.
Correct knowledge (yes/no) was based on a battery of questions about HIV and sexually transmitted infections (STIs).
Appendix Table A3.
Characteristics of respondents who do not accept any of the programs versus those who accept one or more of the proposed programs
| Sometime-takersa |
Never-takersa |
|||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std.Dev. | N | Mean | Std.Dev. | N | t- test* |
Prob | |
| Age (in years) | 21.33 | 2.34 | 1558 | 21.71 | 2.21 | 143 | −1.85 | 0.06 |
| Has HIV or other sexually transmitted infection (STI)b |
0.09 | 0.29 | 1508 | 0.09 | 0.28 | 136 | 0.25 | 0.80 |
| Any condom use at last sexual actb,c |
0.88 | 0.32 | 1453 | 0.81 | 0.39 | 126 | 2.39 | 0.02 |
| Male sex partners (last month) | 3.25 | 6.40 | 1558 | 2.43 | 2.10 | 143 | 1.53 | 0.13 |
| Last sex act with a partner whom respondent had just metb |
0.37 | 0.48 | 1455 | 0.33 | 0.47 | 129 | 0.98 | 0.33 |
| Has a stable partnerb | 0.36 | 0.48 | 1482 | 0.37 | 0.49 | 134 | −0.22 | 0.83 |
| Sex workerb | 0.05 | 0.23 | 1344 | 0.03 | 0.16 | 116 | 1.32 | 0.19 |
| Studentb | 0.47 | 0.50 | 1437 | 0.38 | 0.49 | 129 | 2.02 | 0.04 |
| Highest level of educationd | 3.04 | 0.64 | 1558 | 3.16 | 0.65 | 143 | −2.19 | 0.03 |
| Wealth indexe | −0.01 | 0.76 | 1434 | 0.05 | 0.85 | 131 | −0.87 | 0.38 |
Notes: t-test of the differences in means between the two groups: “never-takers” vs. “sometime-takers.” Prob refers to the probability from the null hypothesis of “no difference.”
The sample of “never-takers” is that of respondents who said “no” to every one of the programs offered at all incentive offer levels; whereas “sometime-takers” are those who said yes to one or more of the programs being offered
Binary variable.
Any condom use refers to use of condoms by respondent or male partner during last anal sex.
Educational levels were: Primary =1; Middle School=2; High School=3; College=4; Graduate=5.
The wealth index was constructed using data on availability of: vehicle, own house, more than five rooms in the house, laptop and desktop computers, cable television, Internet access, and household help.
Appendix Figure A1. Willingness to stay free of sexually transmitted infections, verified by quarterly STI testing as a function of random quarterly incentive offers.
Notes: Non-parametric, locally-weighted regressions [31] with a sample of 1,645 individuals who stated their willingness-to-accept quarterly STI testing and a quarterly conditional economic incentive of USD$ α3 for staying free of sexually transmitted infections (STI). The line represents the proportion of individuals willing to accept the HIV prevention program. The dots represent (no/yes) responses, jittered for visualization purposes. The gray area reflects the 95% confidence intervals.
REFERENCES
- 1.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372(9639):669–684. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Padian NS, Buve A, Balkus J, Serwadda D, Cates W., Jr. Biomedical interventions to prevent HIV infection: evidence, challenges, and way forward. Lancet. 2008;372(9638):585–599. doi: 10.1016/S0140-6736(08)60885-5. [DOI] [PubMed] [Google Scholar]
- 3.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–775. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 4.Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012 doi: 10.1016/S0140-6736(11)61709-1. doi:10.1016/S0140-6736(11)61709-1. [DOI] [PubMed] [Google Scholar]
- 5.de Walque D, Dow WH, Nathan R, Abdul R, Abilahi F, Gong E, Isdahl Z, Jamison J, Jullu B, Krishnan S, Majura A, Miguel E, Moncada J, Mtenga S, Mwanyangala MA, Packel L, Schachter J, Shirima K, Medlin CA. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ open. 2012;2:e000747. doi: 10.1136/bmjopen-2011-000747. doi:10.1136/bmjopen-2011-000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baird SJ, McIntosh C, Ozler B. Cash or Condition? Evidence from a Cash Transfer Experiment. Q J Econ. 2011;126:1709–1753. [Google Scholar]
- 7.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. Jama. 2007;298(16):1900–1910. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]
- 8.Adato M, Hoddinott J. Conditional cash transfers in Latin America. Johns Hopkins University Press; Baltimore: 2010. [Google Scholar]
- 9.Gertler P. Do Conditional Cash Transfers Improve Child Health? Evidence from PROGRESA’s Control Randomized Experiment. Am Econ Rev. 2004;94(2):336–341. doi: 10.1257/0002828041302109. [DOI] [PubMed] [Google Scholar]
- 10.Barber SL, Gertler PJ. Empowering women to obtain high quality care: evidence from an evaluation of Mexico’s conditional cash transfer programme. Health Policy Plan. 2009;24(1):18–25. doi: 10.1093/heapol/czn039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barham T, Maluccio JA. Eradicating diseases: The effect of conditional cash transfers on vaccination coverage in rural Nicaragua. J Health Econ. 2009;28(3):611–621. doi: 10.1016/j.jhealeco.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Barber SL, Gertler PJ. The impact of Mexico’s conditional cash transfer programme, Oportunidades, on birthweight. Trop Med Int Health. 2008;13(11):1405–1414. doi: 10.1111/j.1365-3156.2008.02157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fernald LC, Gertler PJ, Neufeld LM. Role of cash in conditional cash transfer programmes for child health, growth, and development: an analysis of Mexico’s Oportunidades. Lancet. 2008;371(9615):828–837. doi: 10.1016/S0140-6736(08)60382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernald LC, Gunnar MR. Poverty-alleviation program participation and salivary cortisol in very low-income children. Soc Sci Med. 2009;68(12):2180–2189. doi: 10.1016/j.socscimed.2009.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernald LC, Gertler PJ, Neufeld LM. 10-year effect of Oportunidades, Mexico’s conditional cash transfer programme, on child growth, cognition, language, and behaviour: a longitudinal follow-up study. Lancet. 2009;374(9706):1997–2005. doi: 10.1016/S0140-6736(09)61676-7. [DOI] [PubMed] [Google Scholar]
- 16.Leroy JL, Garcia-Guerra A, Garcia R, Dominguez C, Rivera J, Neufeld LM. The Oportunidades program increases the linear growth of children enrolled at young ages in urban Mexico. J Nutr. 2008;138(4):793–798. doi: 10.1093/jn/138.4.793. [DOI] [PubMed] [Google Scholar]
- 17.Grossman M. Concept of Health Capital and Demand for Health. J Polit Econ. 1972;80(2):223–225. [Google Scholar]
- 18.Michael RT. Sexual Capital: An Extension of Grossman’s Concept of Health Capital. J Health Econ. 2004;23(4):643–652. doi: 10.1016/j.jhealeco.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Laibson D. Golden Eggs and Hyperbolic Discounting. Q J Econ. 1997;112(2):443–477. [Google Scholar]
- 20.Rao V, et al. Sex Workers and the Cost of Safe Sex: The Compensating Differential for Condom Use among Calcutta Prostitutes. Journal of Development Economics. 2003;71(2):585–603. [Google Scholar]
- 21.Gertler P, Shah M, Bertozzi SM. Risky Business: The Market for Unprotected Commercial Sex. J Polit Econ. 2005;113(3):518–550. [Google Scholar]
- 22.Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. Aids. 2005;19(Suppl 2):S67–72. doi: 10.1097/01.aids.0000172879.20628.e1. [DOI] [PubMed] [Google Scholar]
- 23.MacKellar D, Valleroy L, Karon J, Lemp G, Janssen R. The Young Men’s Survey: methods for estimating HIV seroprevalence and risk factors among young men who have sex with men. Public Health Rep. 1996;111(Suppl 1):138–144. [PMC free article] [PubMed] [Google Scholar]
- 24.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men--a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47. doi: 10.1177/00333549071220S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gutierrez JP. Profile of gay men in Mexico City: results of a survey of meeting sites. Trop Med Int Health. 2011 doi: 10.1111/j.1365-3156.2011.02934.x. doi:10.1111/j.1365-3156.2011.02934.x. [DOI] [PubMed] [Google Scholar]
- 26.McFadden DL, Bemmaor AC, Caro FG, Dominitz J, Jun BH, Lewbel A, Matzkin RL, Molinari F, Schwarz N, Willis RJ, Winter JK. Statistical analysis of choice experiments and surveys. Market Lett. 2005;16(3-4):183–196. doi:DOI 10.1007/s11002-005-5884-2. [Google Scholar]
- 27.DeShazo JR. Designing transactions without framing effects in iterative question formats. J Environ Econ Manag. 2002;43(3):360–385. doi:10.1006/jeem.2000.1185. [Google Scholar]
- 28.Infante C, Sosa-Rubi SG, Cuadra SM. Sex work in Mexico: vulnerability of male, travesti, transgender and transsexual sex workers. Cult Health Sex. 2009;11(2):125–137. doi: 10.1080/13691050802431314. [DOI] [PubMed] [Google Scholar]
- 29.IMF [Accessed 14 September 2010];International exchange rates. 2008 http://www.imf.org/external/data.htm.
- 30.Hanemann M, Loomis J, Kanninen B. Statistical Efficiency of Double-Bounded Dichotomous Choice Contingent Valuation. Am J Agr Econ. 1991;73(4):1255–1263. [Google Scholar]
- 31.Fan JQ. Design-Adaptive Nonparametric Regression. J Am Stat Assoc. 1992;87(420):998–1004. [Google Scholar]
- 32.Thornton RL. The Demand for, and Impact of, Learning HIV Status. Am Econ Rev. 2008;98(5):1829–1863. doi: 10.1257/aer.98.5.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baird S, Chirwa E, McIntosh C, Ozler B. The short-term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Econ. 2010;19(Suppl):55–68. doi: 10.1002/hec.1569. doi:10.1002/hec.1569. [DOI] [PubMed] [Google Scholar]
- 34.Bautista-Arredondo S, Colchero MA, Sosa-Rubí SG, Romero M, Conde C. Informe sobre la encuesta en sitios de encuentro de HSH. National Institute of Public Health (INSP); Cuernavaca, Mexico: 2012. Diagnóstico situacional, mapeo de sitios de encuentro y evaluación de impacto de las estrategias de prevención en México. [Diagnostic assessment, mapping of meeting places, and impact evaluation of HIV prevention strategies in Mexico: Report on the survey for meeting places for men who have sex with men] [Google Scholar]
- 35.Tversky A, Kahneman D. Belief in Law of Small Numbers. Psychological Bulletin. 1971;76(2):105–110. [Google Scholar]
- 36.Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: A meta-analysis. Psychological Bulletin. 1999;125(1):90–132. doi: 10.1037/0033-2909.125.1.90. doi:Doi 10.1037//0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- 37.Michielsen K, Chersich MF, Luchters S, De Koker P, Van Rossem R, Temmerman M. Effectiveness of HIV prevention for youth in sub-Saharan Africa: systematic review and meta-analysis of randomized and nonrandomized trials. Aids. 2010;24(8):1193–1202. doi: 10.1097/QAD.0b013e3283384791. [DOI] [PubMed] [Google Scholar]
- 38.Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, Malow R, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008;(3):CD001230. doi: 10.1002/14651858.CD001230.pub2. doi:10.1002/14651858.CD001230.pub2 [doi] [DOI] [PubMed] [Google Scholar]
- 39.Sangani P, Rutherford G, Wilkinson D. Population-based interventions for reducing sexually transmitted infections, including HIV infection. Cochrane Database of Systematic Reviews. 2004;(2):CD001220. doi: 10.1002/14651858.CD001220.pub2. doi:10.1002/14651858.CD001220.pub2. [DOI] [PubMed] [Google Scholar]
- 40.Wariki WM, Ota E, Mori R, Koyanagi A, Hori N, Shibuya K. Behavioral interventions to reduce the transmission of HIV infection among sex workers and their clients in low- and middle-income countries. Cochrane Database Syst Rev. 2012;2:CD005272. doi: 10.1002/14651858.CD005272.pub3. doi:10.1002/14651858.CD005272.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ota E, Wariki WM, Mori R, Hori N, Shibuya K. Behavioral interventions to reduce the transmission of HIV infection among sex workers and their clients in high-income countries. Cochrane Database Syst Rev. 2011;(12):CD006045. doi: 10.1002/14651858.CD006045.pub3. doi:10.1002/14651858.CD006045.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Galárraga O, Colchero A, Wamai R, Bertozzi S. HIV Prevention Cost Effectiveness: A Review of the Recent Literature. BMC Public Health. 2009;9(Suppl 1):S5. doi: 10.1186/1471-2458-9-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Todd PE, Wolpin KI. Assessing the impact of a school subsidy program in Mexico: Using a social experiment to validate a dynamic behavioral model of child schooling and fertility. American Economic Review. 2006;96(5):1384–1417. doi: 10.1257/aer.96.5.1384. [DOI] [PubMed] [Google Scholar]
- 44.Bourguignon F, Ferreira FHG, Leite PG. Conditional cash transfers, schooling, and child labor: Micro-simulating Brazil’s Bolsa Escola program. World Bank Econ Rev. 2003;17(2):229–254. doi:Doi 10.1093/Wber/Lhg018. [Google Scholar]
- 45.Filmer D, Schady N. Does More Cash in Conditional Cash Transfer Programs Always Lead to Larger Impacts on School Attendance? Journal of Development Economics. 2011;96(1):150–157. doi: http://www.elsevier.com/wps/find/journaldescription.cws_home/505546/description#description. [Google Scholar]
- 46.McFadden D. Contingent Valuation and Social Choice. Am J Agr Econ. 1994;76(4):689–708. doi: http://ajae.oxfordjournals.org/content/by/year. [Google Scholar]
- 47.Blumenschein K, Blomquist GC, Johannesson M, Horn N, Freeman P. Eliciting willingness to pay without bias: Evidence from a field experiment. Econ J. 2008;118(525):114–137. [Google Scholar]
- 48.Johannesson M. A note on the relationship between ex ante and expected willingness to pay for health care. Soc Sci Med. 1996;42(3):305–311. doi: 10.1016/0277-9536(95)00151-4. [DOI] [PubMed] [Google Scholar]
- 49.Kahneman D. A perspective on judgment and choice - Mapping bounded rationality. Am Psychol. 2003;58(9):697–720. doi: 10.1037/0003-066X.58.9.697. doi:Doi 10.1037/0003-066x.58.9.697. [DOI] [PubMed] [Google Scholar]
- 50.López-Feldman A. DOUBLEB: Stata module to compute Contingent Valuation using Double-Bounded Dichotomous Choice. In: IDEAS R, editor. Stata command to use maximum likelihood (under the assumption of normality) to estimate the double-bounded dichotomous choice model for contingent valuation proposed by Hanemann, Loomis and Kanninen. CIDE, División de Economía; Mexico City, Mexico: 2011. (1991) [Google Scholar]