Overview
The rapid increase in the numbers of older adults worldwide makes a focus on mental disorders and aging both timely and imperative. According to the 2010 census, in the United States, there were 40.3 million adults aged 65 years and older. This number represented an increase of 5.3 million over the 2000 census. Between 2000 and 2010, the number of elders increased at a faster rate (15.1%) than the total US population (9.7%).1 These numbers are projected to continue to diverge, and the disparity between age groups will widen further as a consequence. By 2050, an estimated 20.2% of the population will be 65 years of age and older.2
Keywords: Late life, Geriatric, Depression, Psychological, Social factors in late life
Depression, including MDD, remains a serious public health concern across the lifespan and especially in the elderly. Despite a lower overall percentage of depressed elders, when compared with their younger counterparts,3 the expected increasing numbers of seniors point to an even greater necessity for health professionals to be aware of the specialized needs of elders.
The consequences of untreated or partially treated late-life depression are dire. There are higher mortality rates from both suicide4 and medical illness.5,6 Geriatric depression is also costly. In one study, total health care costs were 47% to 51% higher and outpatient costs were 43% to 52% higher for depressed elders when compared with non-depressed patients, even after adjustment for chronic medical illness. This increase was seen in every component of health care costs, with only a small percentage caused by mental health treatment.7
This issue of the Psychiatric Clinics of North America offers a comprehensive review of late-life depression. This article appraises several facets of geriatric depression, including a description of geriatric depression and recent epidemiologic studies highlighting the incidence and prevalence of old-age depression. The evidence regarding the cause of late-life depression is addressed from a biopsychosocial perspective. This review is crafted to be extensive, although not exhaustive. Particular attention is focused on vascular depression and the relationship between depression and cognitive impairment.
Description of Depression in Older Adults
Depression in older adults can have a variety of presentations: as recurrent disease stemming from earlier life (ie, early onset depression [EOD]); as new-onset depression (ie, late-onset depression [LOD]); as a mood disorder secondary to a general medical condition; or as mood symptoms secondary to substance or medication use. LOD is generally characterized as depression initially occurring past the age of 60–65.
Clinicians and clinical investigators do not agree as to what constitutes clinically significant depression nor is there universal agreement about how depression should be further divided into subtypes. The Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) (DSM-IV-TR) has set forth the criteria for assigning a diagnosis of MDD.8 These criteria may change with the publication of the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) in May of 2013.
Depressive states that do not meet the criteria for MDD can still result in significant impairment to the individual and in debilitating psychosocial effects. Several clinical depressive geriatric disorders have been described in the literature (Table 1).8–11
Table 1. Classification of geriatric depressive disorders.
| MDD8 | Mixed anxiety-depressive disorder8 |
| Dysthymic disorder8 | Bereavement8 |
| Minor depressive disorder8 | Adjustment disorder with depressed mood8 |
| Depression without sadness9 | Mood disorder caused by a general medical condition8 |
| Subsyndromal or subthreshold depression10 | (Vascular) dementia with depressed mood8 |
| Depression–executive dysfunction syndrome11 | Substance- or medication-induced depression8 |
| Bipolar disorder, most recent episode depressed8 | — |
Minor depression or subthreshold depression is diagnosed when one of the core symptoms of depression is present along with 1 to 3 additional symptoms.8 Minor depression and subthreshold depression in elders are of particular clinical importance because they have been associated with impairment similar to that of major depression, including impaired physical function, increased disability days, poorer selfrated health, perceived low social support, and excess service utilization.10,12,13
The depression–executive dysfunction syndrome has been thought of as major depression with prominent frontostriatal dysfunction. The syndrome is based on clinical, neuropathologic, and neuroimaging findings suggesting that frontostriatal dysfunction contributes to the development of both depression and executive dysfunction and influences the course of depression. Reduced verbal fluency, impaired visual naming, paranoia, loss of interest in activities, and psychomotor retardation characterize the syndrome. There is usually a rather mild associated vegetative pattern. Depressive signs and symptoms, especially psychomotor retardation and loss of interest in activities, contribute to disability in these patients. Depression with executive dysfunction has also been found to be associated with disability, poor treatment response, relapse, and recurrence.11
Epidemiology
The point prevalence estimates for MDD in elders in the community have been reported to be 4.4% in women and 2.7% in men in the Cache County Study.14 The prevalence of either a major depressive episode or dysthymia in the Epidemiologic Catchment Area (ECA) survey was 2.5% in the geriatric age range.3 A recent meta-analysis of older adults (aged 50 years and older) found a rate of 3.29% for current and 16.52% for lifetime MDD. For depressive symptoms, the prevalence rate was higher than for MDD, at 19.47%.15 In 2012, the Institute of Medicine (IOM) published a report regarding the workforce for older adults (aged 65 years and older) with mental illness and/or substance use. The report made use of information from published research conducted in population-based samples in the United States as well as unpublished data. The committee found that the conditions with the highest prevalence among geriatric patients were depressive disorders, including a major depressive episode and dysthymic disorder. In 2010, about 1.2 million to 1.8 million community-living older adults had these conditions. The 12-month prevalence rates were as follows: depressive disorders (3.0%–4.5%), major depressive episodes (3.0%–4.3%), dysthymic disorder (0.6%–1.6%), and depressive symptoms (1.1%–11.1%).16
Depression seems to both persist into older age as well as increase in prevalence through the geriatric age range. With respect to the oldest old (ie, elders aged 75 and greater) in a systematic review and meta-analysis, the pooled point prevalence of major depression was 7.2%. The rates of depression for women were between 4.0% and 10.3% and for men between 2.8% and 6.9% in the individual studies. The pooled prevalence of clinically significant depressive symptoms was 17.1%. The prevalence of clinically significant depressive symptoms increased in the higher age groups, by almost 20% to 25% in individuals aged 85 years and older and by about 30% to 50% in individuals aged 90 years and older, compared with those between 75 and 79 years of age, although no similar trend was found for major or minor depression.17,18
In the past several decades, many studies have examined the prevalence of late-life depression; however, there have been comparatively few incidence or new case studies. Lately, the first systematic review to examine this subject was completed. Twenty studies involving people aged 70 years and greater were reviewed. The incidence rate of MDD was found to be 0.2 to 14.1 per 100 person-years, and the incidence of clinically relevant depressive symptoms was 6.8 per 100 person-years. Female incidence was mostly higher than male incidence.19
The recurrence rates of depression were calculated in a new study. More than 5650 individuals were tracked in Rotterdam, Netherlands for 8 years on average. Recurrence for depressive symptoms and syndromes combined was 65.6 per 1000 patient-years. Recurrence was higher for women (73.1 per 1000 patient-years) than men (51.6 per 1000 patient-years). Recurrent episodes of depressive syndromes were almost equal between the genders, with an overall rate of 27.5 per 1000 patient-years.20
In the hospital and long-term-care settings, the frequency of major depression is much higher than in community settings. A total of 11.5% of hospitalized elders meet the criteria for MDD and 23% have depressive symptoms.21 Major depression affects 5% to 10% of older adults in primary care settings.22 The rates of major depression among nursing home residents are even higher. In one study of a long-term-care facility,23 the prevalence estimate for probable and/or definite MDD was 14.4%. The estimate for minor depression was 16.8%. The prevalence of significant depressive signs and symptoms was 44.2%. Unfortunately, depression recognition was low; less than half of the cases diagnosed by psychiatrists were recognized as depressed by staff.23 The IOM's report found an even higher prevalence of depression, 49.6%, among nursing home residents aged 65 years and older.16
Mortality
The consequences of elder depression are grim. There is both increased suicide and nonsuicide mortality. Although suicidal ideation decreases with age,24 elders with suicidal thoughts are more likely to act on them and successfully commit suicide than their younger counterparts.25 Older age has been significantly associated with more determined and planned self-destructive acts and with fewer warnings of suicidal intent.24 Among those who attempt suicide, elders are the most likely to die. In adolescence, the ratio of attempted to completed suicides has been estimated to be 200:1, whereas the estimated risk for the general population is from 8:1 to 33:1. In contrast, there are approximately 4 attempts for each completed suicide in later life.26 The most common mechanisms for suicide in a Canadian study involved firearms, hanging, selfpoisoning, and falls from height,27 which suggests increased lethality of self-destructive behaviors in older adults.26
Elder suicide remains a major public health crisis, and suicide has been overrepresented in this population. In 2004, the aged composed 12% of the US population, but elders accounted for 16% of suicide deaths. In 2010, 16.00 of every 100 000 people aged 65 years and older died by suicide, which was higher than the rate of 11.26 per 100 000 in the general population.25 Suicide rates are highest among white men, rising in this population to a rate of more than 45 suicides per 100 000 per year. This number is 4 times the nation's overall age-adjusted rate.28
In addition to suicide, nonsuicide mortality is also a significant adverse outcome resulting from late-life depression. For adults aged 55 years and older in the New Haven ECA project,29 the odds of dying were more than 4 times greater for individuals with affective disorders than for others, controlling for age, sex, and physical health. In a 7-year longitudinal follow-up of patients referred for geriatric psychiatry consultation, 50% of patients with Geriatric Depression Scale (GDS) scores greater than 6 died by 19 months versus 54 months for patients with GDS scores less than 7.6 In a systematic review of the literature from 1997 to 2001, 72% of included studies demonstrated a positive association for depression with nonsuicide mortality, although a substantial minority did not. Depression may increase the likelihood of dying through several factors. Depressed people may be less likely to adhere to their medication regimen and maintain their cognitive and physical functioning capabilities, may be more likely to alienate their social network, and be less likely to seek out preventive and curative health care treatments.30 In addition, depression itself may be harmful to the body. One of the most robust findings in the literature is the association of depression with increased mortality in those with cardiovascular disease.6
Contributors to Elder Depression
Many factors contribute to late-life depression, including biologic (Table 2) and psychosocial (Table 3). The biopsychosocial model31 of understanding and organizing the cause of psychiatric illness has been useful in allowing mental health practitioners to more easily and thoroughly conceptualize mental illness, although it may be unintentionally misleading in its separations. Elder depression, like depression in all age groups, likely stems from a complex multidirectional interaction of biologic, psychological (including personality based), and social factors.
Table 2. Biologic risk factors for late-life depression.
| Vascular | General health |
| Myocardial infarction | Obesity |
| Coronary heart disease | New medical illness |
| Hyperhomocysteinemia | Poor health status |
| Cerebrovascular accident | Poor self-perceived health |
| Silent cerebral infarction and white matter hyperintensities | |
|
| |
| Genetic polymorphisms/mutations | Dementia |
| CADASIL | Alzheimer disease |
| MTHFR | Vascular dementia |
| CBS | |
|
| |
| Diabetes mellitus | Parkinson disease |
Abbreviations: CADASIL, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy; CBS, cystathionine beta-synthetase; MTHFR, methyltetrahydrofolate reductase.
Table 3. Psychosocial risk factors for late-life depression.
| Personality attributes | Life stressors |
| Personality disorder | Stressful life events and daily hassles |
| Neuroticism | Medical illness and disability |
| Low level of self-efficacy | Poor functional status |
| Obsessional traits | Trauma |
| Lower income | |
| Less education | |
|
| |
| Maladaptive thoughts and behaviors | Social stressors |
| Cognitive distortions | Perceived social support |
| Faulty information processing | Impaired social support |
| Loneliness | |
|
| |
| Learned helplessness | Bereavement |
Biologic Factors
Vascular depression
The vascular depression hypothesis is not new. Alexopoulos and colleagues32 observed a characteristic cognitive pattern in depressed patients with vascular disease. In 1997, he coined the term vascular depression to describe these cases. The known comorbidity of depression, vascular disease, vascular risk factors, and the association of ischemic lesions with distinctive behavioral symptoms support the vascular depression hypothesis. Disruption of prefrontal systems or their modulating pathways by single lesions or by an accumulation of lesions exceeding a threshold are hypothesized to be the central mechanisms in vascular depression.32 Symptomatically, these patients have more psychomotor retardation and less psychomotor agitation, less guilt, poorer insight, and limited depressive symptoms compared with controls. Cognitively, patients with vascular depression have greater overall cognitive impairment and disability than those with nonvascular depression. Fluency and naming are more impaired in patients with vascular depression.33
Several lines of evidence have led to the conclusion that cerebrovascular injury is linked to late-life depression. One line is the homocysteine depression hypothesis. Essentially, the hypothesis is that elevated levels of homocysteine lead to cerebral vascular disease and neurotransmitter deficiency, which then cause depressed mood. This linkage has been demonstrated in population and imaging studies. Levels of homocysteine may increase because of a multitude of factors, including dietary deficiency of B12, folate, and B6 and the genetic variation of enzymes, such as methyltetrahydrofolate reductase and cystathionine beta-synthetase, which are both essential for the metabolism of homocysteine.34 The genetically based neurologic condition known as cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) many times arises with depression as one of its initial symptoms. The initial presentation, however, is primarily from either a stroke or a migraine; but up to 6% of patients may initially present with depression. Overall, psychiatric symptoms, including depression, adjustment disorder, and subcortical dementia, are present in up to 30% of patients with this ailment. The condition is caused by a mutation of the notch 3 gene.35 Finally, several studies indicate that a large proportion of elderly persons with depression have had either a stroke or other evidence of cerebral compromise.33,36 Many studies have also found high rates of cerebrovascular disease and white matter hyperintensities (WMH) on MRIs in depressed elderly patients.37
Neuroimaging has further added to the understanding of late-life depression. As a result, several areas of the brain have been implicated in late-life depression. These areas include the anterior cingulate cortex (ACC), orbitofrontal cortex (OFC), and the hippocampus.38 In a meta-analysis of structures involved in depression, the ACC had the largest effect size. Depressed individuals had smaller ACC volumes.39 The OFC functions as part of a network, which includes the hippocampus, amygdala, and basal ganglia. In elderly samples compared with nondepressed subjects, depressed patients have had smaller OFC volumes.40 The hippocampus has been long associated with depression. As in the other implicated brain regions, studies in late-life depression have also demonstrated a reduction in hippocampal volume in the depressed elderly population.39,41 Age of onset correlates negatively with hippocampal volume; patients with LOD have smaller volumes compared with those who have EOD and with controls.41,42
Functional neuroimaging has aided in the understanding of late-life depression. Regional cerebral blood flow and cerebral metabolism studies have demonstrated that the dorsal cingulate gyrus, middle and dorsolateral prefrontal cortex (DLPFC), insula, and superior temporal gyrus are all hypoactive at rest during negative mood states and that their activity increases with selective serotonin reuptake inhibitor treatment.43 An additional network identified is a cortical-limbic network, which includes the medial and inferior frontal cortex and basal ganglia. These structures are overactive at rest and during induction of negative mood states. Their activity reduces with antidepressant treatment.44 Overall, functional neuroimaging studies in late-life depression reveal a pattern of abnormal activation of frontolimbic regions, generally characterized by hypoactivation of specific dorsal cortical regions, including the DLPFC and the dorsal ACC, and hyperactivation of some limbic structures, such as the amygdala.44 However, the bulk of the existent data are from midlife or mixedage depression studies; it is possible that as more data become available, a different pattern may emerge in late life.44
It is thought that WMH are caused by small, silent cerebral infarctions. They are characterized by arteriosclerosis, perivascular demyelination, dilated periventricular spaces, and ischemia.45,46 WMHs can predispose individuals to depression32,37 by disrupting the fiber tracts connecting cortical and subcortical structures,32 including tracts in the dorsolateral prefrontal cortex and the anterior cingulate cortex.45 They are frequently found in patients with late-life depression.37 In one study, among patients with late-life major depression, silent cerebral infarction was observed in 65.9% of those with EOD and in 93.7% of those with LOD.47 A recent systematic review48 confirmed this finding. The investigators found that WMHs are more common and severe in individuals with geriatric depression than in healthy controls and specifically in individuals with LOD. The odds of having white matter changes were more than 4 for LOD compared with EOD. Similarly, the severity of WMHs was greater in patients with LOD than in patients with EOD. The results supported the notion that LOD may be etiologically different from EOD.48
How might WMHs arise? Aside from known cerebrovascular risk factors,49 new research has looked at the interrelationship of orthostatic blood pressure and WMH. In one study, participants with depression had a significantly larger decrease in systolic blood pressure on standing from a supine position than controls. The results indicated that depression might be an independent predictor for developing systolic orthostatic hypotension. Depressed participants also had lower-frequency heart rate variability and lower baroreflex sensitivity. Because brain MRI WMH are mostly ischemic, they may be associated with orthostatic blood pressure decreases.50 In another study, an association between the degree of orthostatic systolic blood pressure decrease and WMH volume in depression was found.51 The presence of autonomic abnormalities in late-life depression could partly be associated with the development of and/or worsening of WMH and late-life depression.
Relationship of late-life depression and cognitive impairment
It has long been known that a relationship exists between memory impairment and depression,52 although the nature of this relationship has been unclear.53 Although in the past cognitive impairment related to depression has been thought to reverse with remission of depression, it now seems that there may be longer-lasting effects. In one study, over 3 years, irreversible dementia developed significantly more frequently in the depressed group with the dementia syndrome of depression (DSD) (43%) than in the group with depression alone (12%). The group with DSD had a 4.69-times higher chance of having developed dementia at follow-up than the patients with depression alone.54 A meta-analysis, which compared patients with depression with those with Alzheimer dementia, found neuropsychological deficiencies on almost every psychological test among patients with depression. Many of the deficits, such as with recall or on recognition tasks, were no different than those seen in patients suffering from dementia. These findings are not consistent with the hypothesis that depression is merely associated with deficits in effortful processing but rather suggest a more pervasive and insidious process at play in depressed elders.55 Research of this nature has led to a series of questions concerning the nature of the relationship between depression and memory impairment. A few questions include the following: Is depression a symptom of dementia? Does a history of depression constitute a risk factor for later dementia? Can depression be a prodrome of dementia?2 What is the relationship between vascular depression and vascular dementia?
Symptoms or syndromes of depression are often present in dementia and may constitute one of the many behavioral and psychological symptoms of dementia.2 A sizable minority of patients with Alzheimer disease, during the course of their disorder, will exhibit depressed mood (40%–50%) whereas actual depressive disorders are encountered in about 10% to 20%.56 Depression may occur more commonly as a symptom in vascular dementia than in Alzheimer dementia.57
Risk factor for dementia
Data regarding depression as a risk factor for dementia have been mixed53,58; however, some tentative conclusions can be drawn from the available evidence. In a recent meta-analysis of 12 longitudinal studies, patients with depression had higher rates of Alzheimer dementia (AD), vascular dementia (VD), any dementia, and mild cognitive impairment (MCI) than those without depression. The relative risk for the associations ranged from 1.55 for any dementia to 1.97 for MCI.59 Another recent large systematic review and meta-analysis confirmed this finding and found that a history of depression increased the odds of later developing AD by 2.02.60 The interval between diagnoses of depression and AD was positively related to increased risk of developing AD, suggesting that rather than a prodrome, depression may be a risk factor for AD.60 This risk also extends into later age, and depression remains a risk factor for cognitive impairment even among the oldest old.61 Recurrent depression seems to present a greater risk for dementia than a single depressive episode, such that patients with many prior hospitalizations for depression have an increased risk of developing subsequent dementia. On average, each depressive episode is associated with a 13% increased rate of dementia.62 Taken together, these findings suggest that depression is indeed a risk factor for dementia and that earlier-onset, recurrent disease confers the greatest risk for the subsequent development of cognitive impairment.
Cause of dementia
Beyond serving as a risk factor for dementia, depression could play a causative role in the development of dementia. A possible mechanism is suggested by the glucocorticoid hypothesis.63 According to this idea, a prolonged physical reaction to stress, such as that associated with a major depressive episode, elicits sustained glucocorticoid secretion. There are glucocorticoid receptors in the hippocampus. Over time, glucocorticoid hypersecretion leads to excessive activation of hippocampal glucocorticoid receptors, which is toxic to the hippocampus and leads to hippocampal atrophy. Such damage has been recorded in imaging studies41 and has been associated with dementia.64
The hypothesis that depression is a prodrome to dementia is most compatible with studies, of which there are many, in which depression occurs close in time to the onset of dementia.53,65,66 It is conceivable that many cases of late-life depression could be an early prodromal sign of dementia, especially because the pathologic changes of dementing diseases can begin long before their onset.67 However, if depression were a prodrome to dementia, then its presence should reliably predict future cognitive disturbance.2
Vascular depression
Lastly, turning to vascular depression and its relationship to vascular dementia, owing to the similarity of risk factors for the two conditions, a connection between them would seem reasonable; however, the path from vascular disease to vascular depression to vascular dementia is likely reciprocal and not direct or sequential.68 Little research has been completed to elucidate this question. A case report suggests that such a relationship may exist.69 The PAQUID study66 documented that the risk for dementia was 50% higher in depressed men with hypertension compared with depressed nonhypertensive men. It seems from this study that in some men, vascular disease leads to depressive symptoms and that a subgroup of those who develop depression progress to dementia.66 Barnes and colleagues70 found that subjects with midlife and late life symptoms had more than a 3-fold increase in vascular dementia risk, whereas subjects with late-life depressive symptoms had a 2-fold increase in AD risk. Barnes and colleagues70 also found that late-life depressive symptoms were more predictive of dementia than early life depressive symptoms, although other analyses, as mentioned, have yielded different results.58
Thus, given these findings, it seems likely that depression is a risk factor for dementia. Evidence to support this is plentiful,59,60,70 but there are also opposing studies.66 EOD may confer a greater risk of dementia than LOD,58,65 although other studies have concluded the opposite.70 The greatest risk for dementia probably exists in those with both midlife and late-life depression.70 There is also a dose-response relationship between depression and dementia, such that each depressive episode is associated with an increased rate of dementia.62 At the same time, some cases of LOD undoubtedly represent a prodromal symptom of dementia.58 Ultimately, depression probably serves as both a risk factor and at times a prodromal symptom for dementia.
Medical comorbidity
Late-life depression often arises in the context of medical and neurologic illness.71 According to the DSM-IV-TR, MDD cannot be diagnosed when symptoms are the direct physiologic result of a medical condition.8 As a result, depression may be either underdiagnosed or overdiagnosed in the presence of conditions such as cancer that can also cause weight loss, fatigue, poor appetite, and/or disruption of sleep.
Although almost any serious or chronic condition can produce a depressive reaction, the disorders that are most strongly associated with depression include cardiac conditions and neurologic illness, including cerebrovascular disease. Specific medical conditions that may be associated with geriatric depression include myocardial infarction, coronary heart disease, cardiac catheterization,72 diabetes,73 obesity, and body mass index.74 Approximately 20% to 25% of patients with heart disease experience major depression, and another 20% to 25% report symptoms of depression.72 In the IOM's report, in community-living adults aged 60 years and older who had major depression or dysthymia, the most common coexisting physical health conditions were hypertension (58%), chronic pain (57%), arthritis (56%), loss of hearing or vision (55%), urinary tract and prostate disease (39%), heart disease (28%), and diabetes (23%).16 Substances that have been linked to old-age depression include methyldopa, benzodiazepines, propranolol, reserpine, steroids, anti-Parkinsonian agents, β-blockers, cimetidine, clonidine, hydralazine, estrogens, progesterone, tamoxifen, vinblastine, vincristine, and dextropropoxyphene.75 New medical illness, poor health status, and poor self-perceived health also increase the risk for depression.76
Neurologic disorders
High rates of cerebrovascular disease and other neurologic disorders have been associated with elder depression. In patients who have had a stroke, the prevalence rate for major depression is 19.3% among hospitalized patients and 23.3% in outpatients.36 Silent cerebral infarctions are observed in many patients with EOD or LOD.47
The rate of depression among those with Parkinson disease (PD) is high. The prevalence of MDD in patients with PD varies from 7.7% in population studies to more than 25% in outpatient samples.77 Depressive symptoms occur in approximately half of the patients with PD and are a significant cause of functional impairment. There is accumulating evidence suggesting that depression in PD is secondary to underlying neuroanatomical degeneration, which results in changes in central serotonergic function and in neurodegeneration of specific cortical and subcortical pathways rather than simply a reaction to psychosocial stress and disability.78 Depression in PD may be a milder form of depression and is less frequently associated with dysphoria, anhedonia, feelings of guilt, and loss of energy but is associated with more concentration problems than depression in older adults without neurologic disease.77 In order to avoid underdiagnosing depression in PD, a study group has proposed a specific syndrome, depression of PD, and has recommended an inclusive approach that considers all symptoms as related to depression, regardless of their overlap with PD or other medical conditions.79
Psychosocial Factors
Psychological and social variables are often intertwined. They may be just as important as physical factors in understanding the elements leading to late-life depression. For example, in institutionalized elders, psychological variables, such as environmental mastery (a sense of self-efficacy and competence in managing one's environment), purpose in life, and autonomy, had a greater importance in understanding depression than traditional risk factors, such as medical illness and disability. These 3 psychological variables discriminated between patients with and without MDD 80% of the time.80 This section reviews the roles of personality attributes, behavior, cognition, psychodynamic theory, social support, and life stressors in elder depression.
Personality attributes
Neuroticism is an enduring tendency to experience negative emotional states. Those who score high on neuroticism scales are more likely to respond poorly to stress and to interpret situations as threatening or hopelessly difficult. Increasingly, it is being recognized as a significant public health concern.81 Neuroticism has been associated with late-life depression. Of 1511 nondepressed elderly respondents (aged 55–85 years at baseline) in the Longitudinal Aging Study Amsterdam, 17% developed a clinically relevant level of depressive symptoms during a 6-year follow-up period. Personality, neuroticism in particular, was found to be a consistent and important predictor of the onset of depressive symptoms in late life. It was an even more important predictor of depression than health-related and situational factors, with a relative risk for prediction of 3.6. Aging did not affect the strength of the association. Other personality factors that played an important role in predicting depression were mastery and self-efficacy.82 In a follow-up study, personality aberrations were also associated with recurrence of depression in later life. In particular, neuroticism and a low level of mastery were noted as contributing factors, along with residual depressive symptoms at the time of recovery, female gender, pain complaints, and feelings of loneliness.83
Other personality attributes that may contribute to late-life depression include the presence of a personality disorder, attachment style, and obsessional traits. The frequency of strictly diagnosable personality disorders shows only a small decline with aging.84 Patients with a personality disorder are almost 4 times more likely to experience maintenance or reemergence of significant depressive symptoms than those without a personality disorder. In addition to a personality disorder, hopelessness and ambivalence regarding emotional expression also predict the maintenance or reemergence of depressive symptoms.85 Insecure attachment is another risk factor for developing new depression. In elders and older adults, both patients with EOD and LOD showed greater insecure attachment and poorer social adaption compared with never-depressed controls. No difference was found between patients with EOD and LOD in attachment style or social adaptation.86 Obsessional traits seem to affect suicide risk, possibly because they may undermine an elder's ability to cope with the challenges of aging, which often call for substantial adaptations.87
Behavior
Learned helplessness is the idea that the cause of depression is the expectation that initiating action in a continually stressful environment is futile.88 A reformulation of the model attributes depression to the belief that highly desired outcomes are improbable or highly aversive outcomes are probable and that the individual expects that no response in their repertoire will change that likelihood. These beliefs about oneself and one's environment lead to helplessness and depression.88
Unfortunately, elders frequently face circumstances that can produce thought patterns that may lead to learned helplessness. As the result of aging, they may feel helpless against the onslaught of recurrent and uncontrollable physical illness and its effects on them and to changes in their social position. This notion has several supporting elements from the literature. For example, poor functional status secondary to physical illness is among the most important of the causes of depressive symptoms in older adults. Disability has been conceptualized as a chronic and stressful condition that may provoke reactions, such as feelings of worthlessness or hopelessness that ultimately contribute to depression.89 Next, the total number of life events and the total number of daily hassles is strongly associated with depression, although sudden unexpected events have not been related to depression.90 Again, the chronicity and perceived uncontrollability of these events could contribute to depression. Lastly, longitudinal cohort studies have identified several other significant psychosocial risk factors for late-life depressive disorders. Some of these have included long-standing situations, such as ongoing difficulties; medical illness and injuries; disability and functional decline; and lack of social contacts.91
Cognition
Cognitive behavior therapy is based on the idea that mental illness is the product of maladaptive thoughts and behaviors and that a 2-way relationship between cognition and behavior exists in which cognitive processes can influence behavior and behavioral change can influence cognitions.92 Further, it posits that faulty information processing and unhelpful behaviors lead to mental illness, including depressed mood states.93 A negative mood state is produced when information processing is highly negatively biased and frequently inaccurate94 because of distorted patterns of thinking and/or errors in logic.92 Aaron Beck and colleagues93 noted a distinctive pattern of thinking in depressed patients that was characterized by a global negative view of themselves, the outside world, and the future. This cognitive triad is the following: I am defective. The world is a hostile place. Things will never change.93 Negative thinking further influences behavior so that patients' social and interpersonal functioning deteriorates. These behavioral changes then help to confirm patients' negative viewpoints, thereby reinforcing themselves.94
There is evidence that elders with depression experience cognitive distortions. In one study, cognitive coping strategies seemed to play an important role in relation to depressive symptoms in late life. Elderly people with more depressive symptoms were reported to use rumination and catastrophizing to a significantly higher extent and positive reappraisal to a significantly lower extent than those with lower depression scores.95 Enhanced sensitivity to negative feedback also occurs in mild late-life depression96 and could stem from the belief that one is defective. Lastly, just as in learned helplessness, chronic stressors could serve to reinforce the outlook that the world is hostile and things will never change, ultimately leading to hopelessness, withdrawal, and depression.
Psychodynamic theory
A psychodynamic understanding of depression is not a unitary concept and can be approached from many different perspectives. One is that depression results from introjected (inwardly directed) anger regarding a lost relationship with an important person who has become unavailable, potentially through relocation or death. In depression, or melancholia, what feels lost or damaged is part of the self,97 such that the ego itself is seen as poor and empty rather than the world, as is the case in mourning.98
In depressed elders, loss is not an uncommon experience because loss and coping with loss are regrettably part of the aging process. Under this facet of psychodynamic theory, elders who internalize their negative emotions may be more likely to become depressed. Although grief and bereavement in elders have not been linked specifically to psychodynamic theory, one example of this may be complicated bereavement.16 Studies have found that bereavement is associated with depressive symptoms in older adults and may be one of the most significant risk factors for depression in late life.99 In one study, the risk of depression associated with the death of one's spouse increased the adjusted odds of depression by 12.1 and of dysphoria by 21.8.100 Another study looked at 1810 community-dwelling older adults who were aged 55 years and older. After 3 years, 9% of the subjects had scored beyond the thresholds for symptoms of depression and anxiety. Vulnerability for depression and anxiety was quite similar, but life events differed. The onset of depression was predicted by death of a partner or other relatives, whereas the onset of anxiety was best predicted by having a partner who developed a major illness.101 These studies did not examine psychological interpretations of these events, but it seems clear that the loss of an important relationship had an important effect, for a myriad of reasons, on the subsequent development of depression.
Social support
Social relationships, ranging from social isolation to social support, have long been implicated in the risk for depression. Social support is a multifactorial construct. It involves dimensions of perception, structure, and behavior. Social isolation and impaired social support have been associated with moderate and severe depressive symptoms in the elderly.102 The most vigorous findings involve perceived support, also called emotional support. Perceived social support has proved to be among the most robust predictors of late-life depressive symptoms.91 A study from Hong Kong103 found that a significant relationship existed between social support and depressive signs and symptoms on all dimensions of social support, including social network size, network composition, social contact frequency, satisfaction of social support, instrumental/emotional support, and helping others. However, again, satisfaction with support was a more important predictor of depression than the other objective measures of network relationships. The consequences of impaired social relationships can be significant because the absence of a friend or a confidante can contribute to suicidal behavior in elders.104
Elders may keenly feel the effects of loneliness. Loneliness has been defined by one group as the absence of a sense of integration into the social environment or as a lower level of perceived emotional togetherness in social interactions. Elders who are lonely are more depressed and experience less togetherness than those who are not lonely.105 The risk of depression caused by a lack of contact with friends has been estimated to be 2.5, and the risk of depression caused by loneliness has been calculated to be 3.6.106
Life stressors
Longitudinal cohort studies have identified several stressors that serve as risk factors for late-life depressive disorders. These stressors include adverse life events and ongoing difficulties; death of a spouse or other loved one; medical illness, especially diseases of the cardiovascular system, and injuries; and disability and functional decline.91,99 For community-dwelling older adults, the presence of disabilities, measured by an Activities of Daily Living Score of 1 to 4, increased the risk of depression by 3.7 over 1 year, after adjusting for age, gender, marital status, loneliness, contact with friends, and index depression score.106 As noted previously, the loss of a loved one is one of the most significant risk factors for late-life depression. How one copes with the loss, how traumatic or unexpected the death is, and the degree to which the death results in social isolation might be some of the linking features between loss and new-onset depression.99 Trauma and fear of victimization are relatively understudied potential sources of depression in elders. They may be related to the onset of late-life depression through the behavioral consequences of fear99 and avoidance.
Aside from acute life events, chronic stressors can also influence the development of late-life depression. Some stressors include lower income99 and less education,107 as well as those previously mentioned. Lower income is related to poorer access to health and mental health services.99 When compared with elders with more education, those with less education have a higher risk of depression, with a relative risk of 1.49.107
Life stressors can arouse negative emotional states in elders in many ways. They can be profoundly psychologically meaningful and may considerably disrupt one's life. They often necessitate change and readjustment. They can also precipitate hospitalization, reduce social activities, increase disability, shift the nature of social relationships, or even result in residential relocation.91 Maladaptive coping strategies, including unhelpful patterns of thinking and behaving, for stressful events can lead to dysphoric mood states. Symptoms may be influenced by characteristic beliefs, including the viewpoint that highly aversive outcomes are probable and that no response will change their likelihood. An elder's ability to adapt to change could be swayed by negative beliefs about oneself and one's ability to control the environment or manage future events. The presence of a personality disorder, or neuroticism, can also impair one's ability to manage. Poor social support can decrease psychological resilience and foster a depressive response to life stressors. Impairment in any of these areas could lead to the persistence of depressive symptoms and/or syndromes.
Summary
Depression in the elderly is a complex disorder. In many ways, it is the quintessential biopsychosocial disorder. There is a great deal of literature linking structural brain changes to late-life depression, but even recent meta-analyses note the heterogeneity of findings and call for further research.108 Psychological factors in depression remain salient across the lifespan, but older adults face new social challenges. For clinicians seeking to manage aging depressed patients, the multiplicity of factors contributing to the presentation is challenging and demands a holistic perspective. Researchers must also account for biologic, psychological, and social factors as they seek to understand the underpinnings of depression in the elderly. The encouraging news for clinicians and researchers is that much work has been done that not only yields clinical insights but also provides a direction for future studies.
Fig. 1.
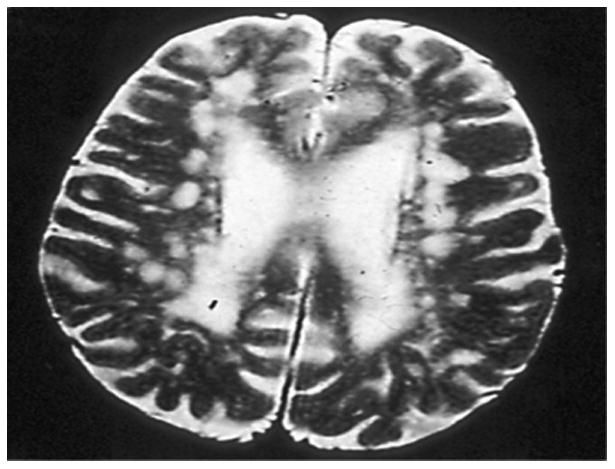
MRI brain scan of a 73-year-old woman with major depression. The scan shows extensive white matter disease.
Key Points.
Depressive symptoms in elders have been associated with impairment similar to that of major depressive disorder.
Depressive disorders in the geriatric age range are found in 3.0% to 4.5% of the population.
Late-onset depression has been prominently linked to cerebrovascular compromise.
Depression likely serves as both a risk factor and potentially an early sign of dementia.
The most significant psychosocial factors leading to depression are bereavement; perceived social support; neuroticism; personality disorders; loneliness; disability; total number of life events; total number of daily hassles; and impaired social support, including lack of a confidante.
Clinical Vignette: Elderly Woman With Depression.
Ms S was a 73-year-old widowed white woman with a past psychiatric history significant for major depressive disorder (MDD), recurrent, severe without psychotic features, and a past medical history significant for hypertension, hypercholesterolemia, and a cerebrovascular accident who was seen, at the urging of her daughters, for evaluation of depression in a geriatric psychiatry outpatient clinic. Over the previous 2 months, Ms S had become increasingly depressed. She reported frequent crying spells, poor sleep quality, difficulty falling asleep, frequent nighttime awakenings, low energy, and limited concentration. She denied psychotic symptoms or suicidal ideation. She was taking paroxetine 20 mg/d.
Ms S had a history of depression dating back approximately 15 years. Her depression had occurred in the context of significant financial distress, her husband's passing, and a left internal capsule lacunar infarct. During the course of that initial episode, she had failed to respond to several medications and ultimately received a course of 14 sessions of electroconvulsive therapy to which she had responded well. Over the years, she had also been trialed on sertraline and citalopram for recurrent, though less severe, bouts of depression.
A mental status examination revealed a melancholy older woman with little spontaneous movement and moderate psychomotor retardation. Her speech pattern had high latency. She had a constricted affect and was sporadically tearful during the interview. She described her mood as low. There was no evidence of psychosis or suicidality. She scored 28 of 30 on the Mini-Mental State Examination (MMSE).
Ms S was started on extended-release venlafaxine. Her dose was gradually increased to 75 mg daily. Paroxetine was tapered off. At her next follow-up visit, Ms S reported no depressive symptoms.
At a follow-up visit 18 months later, her mood remained euthymic. However, during the session, Ms S had difficulty processing information. Her MMSE score was 21; she had errors regarding the year, the date, the day of the week, the month, the country, and the floor of the building; spelled the word WORLD in a convoluted manner (DLROE); recalled only one of 3 items; and had difficulty placing a sheet of paper on her lap. Ms S received a brain magnetic resonance imaging (MRI) (Fig. 1). This MRI was compared to an earlier MRI, which had already established the presence of cerebrovascular disease. Ms S's MRI demonstrated extensive white matter disease, although with relatively constant total brain volume. She was started on donepezil 5 mg at bedtime. Her dose was increased to 10 mg at bedtime 4 weeks later.
At her next follow-up visit, her mood remained euthymic. Her daughters noted an improved awareness of what was going on around her. Her MMSE score was 23, with errors in orientation and in following a 3-step command. Extended-release venlafaxine and donepezil were continued.
Acknowledgments
D.C. Steffens has received grant support from the National Institutes of Health (NIH) and royalties from the American Psychiatric Association (APA) for textbooks related to geriatric psychiatry.
Abbreviations: Description of Depression in Later Life
- MMSE
Mini-Mental State Examination
- MDD
Major depressive disorder
- EOD
Early onset depression
- LOD
Late-onset depression
- DSM-IV-TR
Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision)
- ECA
Epidemiologic Catchment Area
- IOM
Institute of Medicine
- GDS
Geriatric Depression Scale
- MTHFR
Methyltetrahydrofolate reductase
- CBS
Cystathionine beta-synthetase
- CADASIL
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy
- ACC
Anterior cingulate cortex
- OFC
Orbitofrontal cortex
- rCFB
Regional cerebral blood flow
- DLPFC
Dorsolateral prefrontal cortex
- WMH
White matter hyperintensities
Footnotes
Financial Disclosures: R. Aziz has nothing to disclose.
References
- 1.Werner C. The older population: 2010. [Accessed November 21, 2012];2011 Available at: http://2010.census.gov/2010census/
- 2.Ellison JM, Kyomen HH, Harper DG. Depression in later life: an overview with treatment recommendations. Psychiatr Clin North Am. 2012;35(1):203–29. doi: 10.1016/j.psc.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 3.Regier DA, Boyd JH, Burke JD, Jr, et al. One-month prevalence of mental disorders in the United States based on five epidemiologic catchment area sites. Arch Gen Psychiatry. 1988;45(11):977–86. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- 4.Mitty E, Flores S. Suicide in late life. Geriatr Nurs. 2008;29(3):160–5. doi: 10.1016/j.gerinurse.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: impact on 6-month survival. JAMA. 1993;270(15):1819–25. [PubMed] [Google Scholar]
- 6.Royall DR, Schillerstrom JE, Piper PK, et al. Depression and mortality in elders referred for geriatric psychiatry consultation. J Am Med Dir Assoc. 2007;8(5):318–21. doi: 10.1016/j.jamda.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 7.Katon WJ, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60(9):897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Publishing, Inc; 2000. [Google Scholar]
- 9.Gallo JJ, Rabins PV, Lyketsos CG, et al. Depression without sadness: functional outcomes of nondysphoric depression in later life. J Am Geriatr Soc. 1997;45(5):570–8. doi: 10.1111/j.1532-5415.1997.tb03089.x. [DOI] [PubMed] [Google Scholar]
- 10.Lavretsky H, Kumar A. Clinically significant non-major depression. Am J Geriatr Psychiatry. 2002;10(3):239–55. [PubMed] [Google Scholar]
- 11.Alexopoulos GS, Kiosses DN, Klimstra S, et al. Clinical presentation of the “depression-executive dysfunction syndrome” of late life. Am J Geriatr Psychiatry. 2002;10(1):98–106. [PubMed] [Google Scholar]
- 12.Beekman AT, Deeg DJ, Braam AW, et al. Consequences of major and minor depression in later life- a study of disability, well-being, and service utilization. Psychol Med. 1997;27(6):1397–409. doi: 10.1017/s0033291797005734. [DOI] [PubMed] [Google Scholar]
- 13.Hybels CF, Blazer DG, Pieper CF. Toward a threshold for subthreshold depression: an analysis of correlates of depression by severity of symptoms using data from an elderly community sample. Gerontologist. 2001;41(3):357–65. doi: 10.1093/geront/41.3.357. [DOI] [PubMed] [Google Scholar]
- 14.Steffens DC, Skoog I, Norton MC, et al. Prevalence of depression and its treatment in an elderly population: the cache county study. Arch Gen Psychiatry. 2000;57(6):601–7. doi: 10.1001/archpsyc.57.6.601. [DOI] [PubMed] [Google Scholar]
- 15.Volkert J, Schulz H, Harter M, et al. The prevalence of mental disorders in older people in Western countries-a meta-analysis. Ageing Res Rev. 2012;12(1):339–53. doi: 10.1016/j.arr.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 16.IOM (Institute of Medicine) The mental health and substance use workforce for older adults: in whose hands? Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 17.Leach LS. Review: major depression affects about 7% of adults aged 75 and above. Evid Based Ment Health. 2012;15(3):64. doi: 10.1136/ebmental-2012-100694. [DOI] [PubMed] [Google Scholar]
- 18.Luppa M, Sikorski C, Luck T, et al. Age- and gender-specific prevalence of depression in latest-life–systematic review and meta-analysis. J Affect Disord. 2012;136(3):212–21. doi: 10.1016/j.jad.2010.11.033. [DOI] [PubMed] [Google Scholar]
- 19.Büchtemann D, Luppa M, Bramesfeld A, et al. Incidence of late-life depression: a systematic review. J Affect Disord. 2012;142(1–3):172–9. doi: 10.1016/j.jad.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 20.Luijendijk HJ, van den Berg JF, Dekker MJ, et al. Incidence and recurrence of late-life depression. Arch Gen Psychiatry. 2008;65(12):1394–401. doi: 10.1001/archpsyc.65.12.1394. [DOI] [PubMed] [Google Scholar]
- 21.Koenig HG, Meador KG, Cohen HJ, et al. Depression in elderly hospitalized patients with medical illness. Arch Intern Med. 1988;148(9):1929–36. [PubMed] [Google Scholar]
- 22.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58(3):M249–65. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 23.Teresi J, Abrams R, Holmes D, et al. Prevalence of depression and depression recognition in nursing homes. Soc Psychiatry Psychiatr Epidemiol. 2001;36(12):613–20. doi: 10.1007/s127-001-8202-7. [DOI] [PubMed] [Google Scholar]
- 24.Conwell Y, Duberstein PR, Cox C, et al. Age differences in behaviors leading to completed suicide. Am J Geriatr Psychiatry. 1998;6(2):122–6. [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC) Web-based injury statistics query and reporting system (WISQARS) [Accessed November 23, 2012];2010 Online. Available at: http://www.cdc.gov/injury/wisqars/index.html.
- 26.Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52(3):193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- 27.Juurlink DN, Herrmann N, Szalai JP, et al. Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004;164(11):1179. doi: 10.1001/archinte.164.11.1179. [DOI] [PubMed] [Google Scholar]
- 28.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. 2011;34(2):451–68. doi: 10.1016/j.psc.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bruce ML, Leaf PJ. Psychiatric disorders and 15-month mortality in a community sample of older adults. Am J Public Health. 1989;79(6):727–30. doi: 10.2105/ajph.79.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schulz R, Drayer RA, Rollman BL. Depression as a risk factor for non-suicide mortality in the elderly. Biol Psychiatry. 2002;52(3):205–25. doi: 10.1016/s0006-3223(02)01423-3. [DOI] [PubMed] [Google Scholar]
- 31.Engel G. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137:535–44. doi: 10.1176/ajp.137.5.535. [DOI] [PubMed] [Google Scholar]
- 32.Alexopoulos GS, Meyers BS, Young RC, et al. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54(10):915–22. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- 33.Alexopoulos GS, Meyers BS, Young RC, et al. Clinically defined vascular depression. Am J Psychiatry. 1997;154(4):562–5. doi: 10.1176/ajp.154.4.562. [DOI] [PubMed] [Google Scholar]
- 34.Folstein M, Liu T, Peter I, et al. The homocysteine hypothesis of depression. Am J Psychiatry. 2007;164(6):861–7. doi: 10.1176/ajp.2007.164.6.861. [DOI] [PubMed] [Google Scholar]
- 35.Taylor MA, Doody GA. CADASIL: a guide to a comparatively unrecognised condition in psychiatry. Adv Psychiatr Treat. 2008;14(5):350–7. [Google Scholar]
- 36.Robinson RG. Poststroke depression: prevalence, diagnosis, treatment, and disease progression. Biol Psychiatry. 2003;54(3):376–87. doi: 10.1016/s0006-3223(03)00423-2. [DOI] [PubMed] [Google Scholar]
- 37.Culang-Reinlieb ME, Johnert LC, Brickman AM, et al. MRI-defined vascular depression: a review of the construct. Int J Geriatr Psychiatry. 2011;26(11):1101–8. doi: 10.1002/gps.2668. [DOI] [PubMed] [Google Scholar]
- 38.Benjamin S, Steffens DC. Structural neuroimaging of geriatric depression. Psychiatr Clin North Am. 2011;34(2):423–35. doi: 10.1016/j.psc.2011.02.001. ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koolschijn PC, van Haren NE, Lensvelt-Mulders GJ, et al. Brain volume abnormalities in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Hum Brain Mapp. 2009;30(11):3719–35. doi: 10.1002/hbm.20801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taylor WD, Macfall JR, Payne ME, et al. Orbitofrontal cortex volume in late life depression: influence of hyperintense lesions and genetic polymorphisms. Psychol Med. 2007;37(12):1763–73. doi: 10.1017/S0033291707000128. [DOI] [PubMed] [Google Scholar]
- 41.Steffens DC, Byrum CE, McQuoid DR, et al. Hippocampal volume in geriatric depression. Biol Psychiatry. 2000;48(4):301–9. doi: 10.1016/s0006-3223(00)00829-5. [DOI] [PubMed] [Google Scholar]
- 42.Lloyd AJ, Ferrier IN, Barber R, et al. Hippocampal volume change in depression: late- and early-onset illness compared. Br J Psychiatry. 2004;184:488–95. doi: 10.1192/bjp.184.6.488. [DOI] [PubMed] [Google Scholar]
- 43.Fitzgerald PB, Laird AR, Maller J, et al. A meta-analytic study of changes in brain activation in depression. Hum Brain Mapp. 2008;29(6):683–95. doi: 10.1002/hbm.20426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gunning FM, Smith GS. Functional neuroimaging in geriatric depression. Psychiatr Clin North Am. 2011;34(2):403–22. doi: 10.1016/j.psc.2011.02.010. viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thomas AJ, O'Brien JT, Davis S, et al. Ischemic basis for deep white matter hyperintensities in major depression: a neuropathological study. Arch Gen Psychiatry. 2002;59(9):785. doi: 10.1001/archpsyc.59.9.785. [DOI] [PubMed] [Google Scholar]
- 46.Fazekas F, Kleinert R, Offenbacher H, et al. Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology. 1993;43(9):1683–9. doi: 10.1212/wnl.43.9.1683. [DOI] [PubMed] [Google Scholar]
- 47.Fujikawa T, Yamawaki S, Touhouda Y. Incidence of silent cerebral infarction in patients with major depression. Stroke. 1993;24(11):1631–4. doi: 10.1161/01.str.24.11.1631. [DOI] [PubMed] [Google Scholar]
- 48.Herrmann LL, Le Masurier M, Ebmeier KP. White matter hyperintensities in late life depression: a systematic review. J Neurol Neurosurg Psychiatry. 2008;79(6):619–24. doi: 10.1136/jnnp.2007.124651. [DOI] [PubMed] [Google Scholar]
- 49.Greenwald BS, Kramer-Ginsberg E, Krishnan RR, et al. MRI signal hyperintensities in geriatric depression. Am J Psychiatry. 1996;153(9):1212. doi: 10.1176/ajp.153.9.1212. [DOI] [PubMed] [Google Scholar]
- 50.Vasudev A, O'Brien JT, Tan MP, et al. A study of orthostatic hypotension, heart rate variability and baroreflex sensitivity in late-life depression. J Affect Disord. 2011;131(1–3):374–8. doi: 10.1016/j.jad.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 51.Colloby SJ, Vasudev A, O'Brien JT, et al. Relationship of orthostatic blood pressure to white matter hyperintensities and subcortical volumes in late-life depression. Br J Psychiatry. 2011;199(5):404–10. doi: 10.1192/bjp.bp.110.090423. [DOI] [PubMed] [Google Scholar]
- 52.Burt DB, Zembar MJ, Niederehe G. Depression and memory impairment: a meta-analysis of the association, its pattern, and specificity. Psychol Bull. 1995;117(2):285. doi: 10.1037/0033-2909.117.2.285. [DOI] [PubMed] [Google Scholar]
- 53.Jorm AF. History of depression as a risk factor for dementia: an updated review. Aust N Z J Psychiatry. 2001;35(6):776–81. doi: 10.1046/j.1440-1614.2001.00967.x. [DOI] [PubMed] [Google Scholar]
- 54.Alexopoulos GS, Meyers BS, Young RC, et al. The course of geriatric depression with “reversible dementia”: a controlled study. Am J Psychiatry. 1993;150:1693–9. doi: 10.1176/ajp.150.11.1693. [DOI] [PubMed] [Google Scholar]
- 55.Christensen H, Griffiths K, MacKinnon A, et al. A quantitative review of cognitive deficits in depression and Alzheimer-type dementia. J Int Neuropsychol Soc. 1997;3(06):631–51. [PubMed] [Google Scholar]
- 56.Wragg RE, Jeste DV. Overview of depression and psychosis in Alzheimer's disease. Am J Psychiatry. 1989;146(5):577–87. doi: 10.1176/ajp.146.5.577. [DOI] [PubMed] [Google Scholar]
- 57.Newman SC. The prevalence of depression in Alzheimer's disease and vascular dementia in a population sample. J Affect Disord. 1999;52(1):169–76. doi: 10.1016/s0165-0327(98)00070-6. [DOI] [PubMed] [Google Scholar]
- 58.Kessing LV. Depression and the risk for dementia. Curr Opin Psychiatry. 2012;25(6):457–61. doi: 10.1097/YCO.0b013e328356c368. [DOI] [PubMed] [Google Scholar]
- 59.Gao Y, Huang C, Zhao K, et al. Depression as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Int J Geriatr Psychiatry. 2013;28(5):441–9. doi: 10.1002/gps.3845. [DOI] [PubMed] [Google Scholar]
- 60.Ownby RL, Crocco E, Acevedo A, et al. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006;63(5):530. doi: 10.1001/archpsyc.63.5.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Spira AP, Rebok GW, Stone KL, et al. Depressive symptoms in oldest-old women: risk of mild cognitive impairment and dementia. Am J Geriatr Psychiatry. 2012;20(12):1006–15. doi: 10.1097/JGP.0b013e318235b611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kessing LV, Andersen PK. Does the risk of developing dementia increase with the number of episodes in patients with depressive disorder and in patients with bipolar disorder? J Neurol Neurosurg Psychiatry. 2004;75(12):1662–6. doi: 10.1136/jnnp.2003.031773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sapolsky RM, Krey LC, McEwen BS. The neuroendocrinology of stress and aging: the glucocorticoid cascade hypothesis. Sci Aging Knowledge Environ. 2002;2002(38):21. doi: 10.1210/edrv-7-3-284. [DOI] [PubMed] [Google Scholar]
- 64.Seab JP, Jagust WJ, Wong ST, et al. Quantitative NMR measurements of hippocampal atrophy in Alzheimer's disease. Magn Reson Med. 2005;8(2):200–8. doi: 10.1002/mrm.1910080210. [DOI] [PubMed] [Google Scholar]
- 65.Jorm AF, Van Duijn CM, Chandra V, et al. Psychiatric history and related exposures as risk factors for Alzheimer's disease: a collaborative re-analysis of casecontrol studies. Int J Epidemiol. 1991;20(Suppl 2):S43–7. doi: 10.1093/ije/20.supplement_2.s43. [DOI] [PubMed] [Google Scholar]
- 66.Fuhrer R, Dufouil C, Dartigues JF. Exploring sex differences in the relationship between depressive symptoms and dementia incidence: prospective results from the PAQUID Study. J Am Geriatr Soc. 2003;51(8):1055–63. doi: 10.1046/j.1532-5415.2003.51352.x. [DOI] [PubMed] [Google Scholar]
- 67.Bateman RJ, Xiong C, Benzinger TL, et al. Clinical and biomarker changes in dominantly inherited Alzheimer's disease. N Engl J Med. 2012;367(9):795–804. doi: 10.1056/NEJMoa1202753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alexopoulos GS. Vascular disease, depression, and dementia. J Am Geriatr Soc. 2003;51(8):1178–80. doi: 10.1046/j.1532-5415.2003.51373.x. [DOI] [PubMed] [Google Scholar]
- 69.Steffens DC, Taylor WD, Krishnan KR. Progression of subcortical ischemic disease from vascular depression to vascular dementia. Am J Psychiatry. 2003;160(10):1751–6. doi: 10.1176/appi.ajp.160.10.1751. [DOI] [PubMed] [Google Scholar]
- 70.Barnes DE, Yaffe K, Byers AL, et al. Midlife vs late-life depressive symptoms and risk of dementia: differential effects for Alzheimer disease and vascular dementia. Arch Gen Psychiatry. 2012;69(5):493–8. doi: 10.1001/archgenpsychiatry.2011.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alexopoulos GS, Buckwalter K, Olin J, et al. Comorbidity of late life depression: an opportunity for research on mechanisms and treatment. Biol Psychiatry. 2002;52(6):543–58. doi: 10.1016/s0006-3223(02)01468-3. [DOI] [PubMed] [Google Scholar]
- 72.Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry. 2003;54(3):241–7. doi: 10.1016/s0006-3223(03)00111-2. [DOI] [PubMed] [Google Scholar]
- 73.Blazer DG, Moody-Ayers S, Craft-Morgan J, et al. Depression in diabetes and obesity- racial: ethnic: gender issues in older adults. J Psychosom Res. 2002;53(4):913–6. doi: 10.1016/s0022-3999(02)00314-8. [DOI] [PubMed] [Google Scholar]
- 74.Sachs-Ericsson N, Burns AB, Gordon KH, et al. Body mass index and depressive symptoms in older adults- the moderating roles of race, sex, and socioeconomic status. Am J Geriatr Psychiatry. 2007;15(9):815–25. doi: 10.1097/JGP.0b013e3180a725d6. [DOI] [PubMed] [Google Scholar]
- 75.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961–70. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 76.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160(6):1147–56. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 77.Ehrt U, Brønnick K, Leentjens AF, et al. Depressive symptom profile in Parkinson's disease: a comparison with depression in elderly patients without Parkinson's disease. Int J Geriatr Psychiatry. 2006;21(3):252–8. doi: 10.1002/gps.1456. [DOI] [PubMed] [Google Scholar]
- 78.McDonald WM, Richard IH, DeLong MR. Prevalence, etiology, and treatment of depression in Parkinson's disease. Biol Psychiatry. 2003;54(3):363. doi: 10.1016/s0006-3223(03)00530-4. [DOI] [PubMed] [Google Scholar]
- 79.Marsh L, McDonald WM, Cummings J, et al. Provisional diagnostic criteria for depression in Parkinson's disease: report of an NINDS/NIMH Work Group. Mov Disord. 2005;21(2):148–58. doi: 10.1002/mds.20723. [DOI] [PubMed] [Google Scholar]
- 80.Davison TE, McCabe MP, Knight T, et al. Biopsychosocial factors related to depression in aged care residents. J Affect Disord. 2012;142(1–3):290–6. doi: 10.1016/j.jad.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 81.Lahey BB. Public health significance of neuroticism. Am Psychol. 2009;64(4):241. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Steunenberg B, Beekman AT, Deeg DJ, et al. Personality and the onset of depression in late life. J Affect Disord. 2006;92(2–3):243–51. doi: 10.1016/j.jad.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 83.Steunenberg B, Beekman AT, Deeg DJ, et al. Personality predicts recurrence of late-life depression. J Affect Disord. 2010;123(1–3):164–72. doi: 10.1016/j.jad.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 84.Abrams RC, Bromberg CE. Personality disorders in the elderly: a flagging field of inquiry. Int J Geriatr Psychiatry. 2006;21(11):1013–7. doi: 10.1002/gps.1614. [DOI] [PubMed] [Google Scholar]
- 85.Morse JQ, Lynch TR. A preliminary investigation of self-reported personality disorders in late life: prevalence, predictors of depressive severity, and clinical correlates. Aging Ment Health. 2004;8(4):307–15. doi: 10.1080/13607860410001709674. [DOI] [PubMed] [Google Scholar]
- 86.Paradiso S, Naridze R, Holm-Brown E. Lifetime romantic attachment style and social adaptation in late-onset depression. Int J Geriatr Psychiatry. 2012;27(10):1008–16. doi: 10.1002/gps.2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373(9672):1372–81. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 88.Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: critique and reformulation. J Abnorm Psychol. 1978;87(1):49. [PubMed] [Google Scholar]
- 89.Bruce ML. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry. 2001;9(2):102–12. [PubMed] [Google Scholar]
- 90.Kraaij V, Arensman E, Spinhoven P. Negative life events and depression in elderly persons a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2002;57(1):P87–94. doi: 10.1093/geronb/57.1.p87. [DOI] [PubMed] [Google Scholar]
- 91.Bruce ML. Psychosocial risk factors for depressive disorders in late life. Biol Psychiatry. 2002;52(3):175–84. doi: 10.1016/s0006-3223(02)01410-5. [DOI] [PubMed] [Google Scholar]
- 92.Wright JH. Cognitive behavior therapy: basic principles and recent advances. Focus. 2006;4(2):173. [Google Scholar]
- 93.Beck AT, Rush AJ, Shaw BF, et al. Cognitive therapy of depression. United States of America: The Guilford Press; 1987. [Google Scholar]
- 94.Sudak DM. Cognitive behavioral therapy for depression. Psychiatr Clin North Am. 2012;35(1):99–110. doi: 10.1016/j.psc.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 95.Kraaij V, Pruymboom E, Garnefski N. Cognitive coping and depressive symptoms in the elderly: a longitudinal study. Aging Ment Health. 2002;6(3):275–81. doi: 10.1080/13607860220142387. [DOI] [PubMed] [Google Scholar]
- 96.von Gunten A, Herrmann FR, Elliott R, et al. Abnormal sensitivity to negative feedback in late-life depression. Psychiatry Clin Neurosci. 2011;65(4):333–40. doi: 10.1111/j.1440-1819.2011.02215.x. [DOI] [PubMed] [Google Scholar]
- 97.McWilliams N. Psychoanalytic diagnosis: understanding personality structure in the clinical process. United States of America: Guilford Press; 2011. [Google Scholar]
- 98.Freud S. Mourning and melancholia. London: The Hogarth Press; 1917. [Google Scholar]
- 99.Areán PA, Reynolds CF., III The impact of psychosocial factors on late-life depression. Biol Psychiatry. 2005;58(4):277–82. doi: 10.1016/j.biopsych.2005.03.037. [DOI] [PubMed] [Google Scholar]
- 100.Bruce ML, Kim K, Leaf PJ, et al. Depressive episodes and dysphoria resulting from conjugal bereavement in a prospective community sample. Am J Psychiatry. 1990;147(5):608–11. doi: 10.1176/ajp.147.5.608. [DOI] [PubMed] [Google Scholar]
- 101.De Beurs E, Beekman A, Geerlings S, et al. On becoming depressed or anxious in late life: similar vulnerability factors but different effects of stressful life events. Br J Psychiatry. 2001;179(5):426–31. doi: 10.1192/bjp.179.5.426. [DOI] [PubMed] [Google Scholar]
- 102.Blazer DG. Depression and social support in late life: a clear but not obvious relationship. Aging Ment Health. 2005;9(6):497–9. doi: 10.1080/13607860500294266. [DOI] [PubMed] [Google Scholar]
- 103.Chi I, Chou KL. Social support and depression among elderly Chinese people in Hong Kong. Int J Aging Hum Dev. 2001;52(3):231–52. doi: 10.2190/V5K8-CNMG-G2UP-37QV. [DOI] [PubMed] [Google Scholar]
- 104.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10(4):398–406. [PubMed] [Google Scholar]
- 105.Tiikkainen P, Heikkinen RL. Associations between loneliness, depressive symptoms and perceived togetherness in older people. Aging Ment Health. 2005;9(6):526–34. doi: 10.1080/13607860500193138. [DOI] [PubMed] [Google Scholar]
- 106.Prince MJ, Harwood RH, Thomas A, et al. A prospective population-based cohort study of the effects of disablement and social milieu on the onset and maintenance of late-life depression. The Gospel Oak Project VII Psychol Med. 1998;28(2):337–50. doi: 10.1017/s0033291797006478. [DOI] [PubMed] [Google Scholar]
- 107.Chang-Quan H, Zheng-Rong W, Yong-Hong L, et al. Education and risk for late life depression: a meta-analysis of published literature. Int J Psychiatry Med. 2010;40(1):109–24. doi: 10.2190/PM.40.1.i. [DOI] [PubMed] [Google Scholar]
- 108.Sexton CE, Mackay CE, Ebmeier KP. A systematic review and meta-analysis of magnetic resonance imaging studies in late-life depression. Am J Geriatr Psychiatry. 2013;21(2):184–95. doi: 10.1016/j.jagp.2012.10.019. [DOI] [PubMed] [Google Scholar]


