Abstract
The aggressive and rapidly lethal brain tumor glioblastoma (GBM) is associated with profound tissue stiffening and genomic lesions in key members of the epidermal growth factor receptor (EGFR) pathway. Previous studies from our laboratory have shown that increasing microenvironmental stiffness in culture can strongly enhance glioma cell behaviors relevant to tumor progression, including proliferation, yet it has remained unclear whether stiffness and EGFR regulate proliferation through common or independent signaling mechanisms. Here we test the hypothesis that microenvironmental stiffness regulates cell cycle progression and proliferation in GBM tumor cells by altering EGFR-dependent signaling. We began by performing an unbiased reverse phase protein array screen, which revealed that stiffness modulates expression and phosphorylation of a broad range of signals relevant to proliferation, including members of the EGFR pathway. We subsequently found that culturing human GBM tumor cells on progressively stiffer culture substrates both dramatically increases proliferation and facilitates passage through the G1/S checkpoint of the cell cycle, consistent with an EGFR-dependent process. Western Blots showed that increasing microenvironmental stiffness enhances the expression and phosphorylation of EGFR and its downstream effector Akt. Pharmacological loss-of-function studies revealed that the stiffness-sensitivity of proliferation is strongly blunted by inhibition of EGFR, Akt, or PI3 kinase. Finally, we observed that stiffness strongly regulates EGFR clustering, with phosphorylated EGFR condensing into vinculin-positive focal adhesions on stiff substrates and dispersing as microenvironmental stiffness falls to physiological levels. Our findings collectively support a model in which tissue stiffening promotes GBM proliferation by spatially and biochemically amplifying EGFR signaling.
Introduction
Glioblastoma (GBM) is the most commonly diagnosed primary astrocytoma in the United States and is also the most deadly primary brain tumor, with a median survival time of only 15 months [1]. Even with extensive resection, chemotherapy, and radiotherapy, recurrence occurs rapidly and almost universally but rarely involves extracranial metastasis. This suggests that signals encoded within the brain microenvironment may interact with cell-intrinsic factors to promote tumor progression, invasion, and recurrence, and that these cell-extrinsic signals may be investigated to achieve a more complete understanding of GBM and potentially uncover new therapeutic avenues [2], [3].
Of all of the microenvironmental parameters that may modulate GBM progression, mechanical signals remain among the most poorly understood. While it has long been understood that many tumors, including GBM, are mechanically stiffer than the surrounding stroma [4], [5], it has only recently become appreciated that these mechanical aberrations may actively instruct malignant progression rather than simply being a passive manifestation of tumor growth [6]–[8]. For example, we previously demonstrated that GBM cells show higher proliferation and migration rates when cultured on stiff two-dimensional substrates [9], [10]. Consistent with this idea, GBM tumors and culture models often display altered expression of molecules known to play key roles in sensing and/or responding to mechanical signals encoded in the tissue microenvironment (i.e., mechanosensing). This list includes integrins, which physically engage the extracellular matrix (ECM) and process mechanical inputs [11]–[13]; specific integrin subtypes have been implicated in GBM tumor initiation, with expression directly correlating with tumorigenicity [13]–[16]. Other members of the mechanosensing machinery have been similarly implicated in GBM growth and progression, including focal adhesion kinase (FAK) [17], [18], the Rho family GTPases [19], and nonmuscle myosin II [20], [21]. These findings are consistent with the broader recognition that aberrant mechanosensing may drive the progression of many solid tumors, including breast epithelial tumors [6].
At the same time, GBM is also closely associated with dysfunction in canonical mitogenic signaling, which in turn impacts proliferation, apoptosis resistance, and invasion. Most notably, amplifications and mutations in epidermal growth factor receptor (EGFR) represent one of the most common sets of genetic lesions in GBM, with EGFR amplifications present in up to perhaps 50% of GBM tumors [22], [23]. EGFR, also referred to as ErbB1 or HER1, is a member of the HER family of receptor tyrosine kinases [24]. Phosphorylation of downstream signaling molecules phosphoinositide 3-kinase (PI3K) and protein kinase B (PKB or Akt) by activated EGFR promotes cell proliferation [24], [25]. Importantly, amplification of the EGFR gene and expression of the EGFRvIII mutation are associated with significantly decreased overall survival [26], [27]. Due to the prominent role of EGFR in controlling the cell cycle and its correlation with poor prognosis, EGFR and EGFRvIII have recently emerged as promising therapeutic targets for the treatment of GBM [24], [28], as has PI3K [29]–[31].
Despite the established centrality of EGFR signaling to GBM progression and the recognition that GBM tumors are accompanied by profound changes in tissue stiffness, it is unknown what, if any, connections exist between these two classes of lesions. Specifically, does tissue stiffening modulate, potentiate, or otherwise interact with EGFR-based signaling to drive tumor cell proliferation? Evidence for such connections exists in breast tumors, with ErbB2 inhibition blunting ECM stiffness-induced promotion of malignancy in a mammary epithelial tumor culture model [6]. Conversely, integrin clustering induced by enhanced matrix cross-linking has been observed to amplify ErbB2-mediated Akt phosphorylation [32]. Together, these findings led us to hypothesize that microenvironmental stiffness cues can regulate GBM proliferation by modulating EGFR-based signaling [33], which we tested using a combination of defined-stiffness culture substrates, proteomic screens, proliferation and cell cycle analysis, and pharmacological loss-of-function studies. We find that microenvironmental stiffness amplifies proliferation, is associated with enhanced progression through the G1/S cell cycle checkpoint, and is accompanied by increased expression and/or activity of EGFR, Akt, and PI3K. We also find that EGFR and focal adhesion markers co-localize on stiff but not soft substrates, implying that stiffness may amplify these signals by physical clustering of EGFR. Our work offers direct evidence that mechanical signals are transduced through the EGFR pathway in GBM and support the emerging concept of synergy between mitogenic and mechanosensory signaling systems.
Materials and Methods
Cell Culture
U373-MG and U87-MG human glioma cells were cultured as previously described [9]. To clarify nomenclature, we obtained U373-MG cells from the University of California, Berkeley Tissue Culture Facility, which obtained these lines from the American Type Culture Collection (ATCC). Genomic analysis has revealed that ATCC U373-MG cells likely share origins with U251-MG glioma cells, [34] although meta-analyses indicate that these two lines have evolved into distinct entities with different karyotypes and drug sensitivities. [35] Briefly, cells were cultured in DMEM high glucose (1X) with L-glutamine without sodium pyruvate (Invitrogen) and supplemented with 10% Calf Serum Advantage (JR Scientific, Inc.), 1% penicillin/streptomycin, 1% MEM nonessential amino acids (Invitrogen), 1% sodium pyruvate (Invitrogen). Cells were maintained in a humidified incubator at 37°C and 5% CO2.
Synthesis of ECM substrates
Polyacrylamide substrates ranging from 0.08 kPa–119 kPa were fabricated as described previously [9]. Briefly, acrylamide solution (Bio-Rad) ranging from 3%–15% was mixed with N-N'- methylene-bis-acrylamide solutions (Bio-Rad) ranging from 0.05%–1.2% and then polymerized between a glutaraldehyde-activated glass surface and hydrophobic coverslip using 10% ammonium persulfate (Bio-Rad) and 1/2000 TEMED (Sigma-Aldrich). Polymerized substrates were then activated for protein conjugation with the water-soluble, heterobifunctional crosslinker Sulfo-SANPAH at 0.5 mg/mL (Pierce Chemical Co.) under UV exposure followed by functionalization with human plasma fibronectin (Millipore Corp.) at a nominal surface density of 2.6 µg/cm2.
Flow cytometric studies
Glioma cells were plated on fibronectin-coated polyacrylamide substrates at a density of 10000 cells/cm2 (on 119 kPa substrates) and 20000 cells/cm2 (on 19 kPa, 0.8 kPa, and 0.08 kPa substrates). After ∼24 hours of incubation, cell proliferation was then measured according to the FITC-bromodeoxyuridine (BrdU) flow kit protocol (BD Biosciences) with a 90-minute exposure to 5-BrdU. Samples were then analyzed on a flow cytometer FC500 (Beckman-Coulter). An aggregate distribution of cells were gated on an FL4 (7-AAD) channel vs. FL1 (FitC-BrdU) channel plot and BrdU intensity was quantified relative to a non-BrdU treated (negative) control for each condition. The percent of BrdU positive cells was reported as the percent of proliferating cells in a given sample.
Cell cycle analysis
Glioma cells were cultured on the surface of fibronectin-coated polyacrylamide gels for 48 hours prior to trypsinization, fixation, and staining with propidium iodide to quantify DNA content. Cells were then analyzed on a flow cytometer FC500 (Beckman-Coulter). An aggregate distribution of cells was visualized using a histogram of PI intensities and gated to exclude unviable cells and doublets. The gated population was visualized as a histogram and fit to the Watson model to quantify the percent of cells in the G0/G1, S and G2 phases of the cell cycle.
Western blot
U373-MG and U87-MG cells were cultured on fibronectin-coated polyacrylamide substrates of defined stiffness for 48 hours. Cells on each substrate were washed twice in PBS, collected, and lysed using 50 µL RIPA lysis buffer with protease inhibitor (1∶100, Sigma-Aldrich) and phosphatase inhibitor (1∶100, Calbiochem) for 5 minutes. Proteins from cell lysates were separated using standard sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE) and electrophoretically transferred to polyvinylidene fluoride (PVDF) membranes. Immunoblots were performed according to manufacturer specifications (Invitrogen Western Blot kit) as described in a previously established protocol (34). Following blocking, sections of the membrane containing the protein of interest were blotted with the appropriate primary antibody (overnight, 4°C) followed by a horseradish peroxidase-conjugated secondary antibody (1 hour at room temperature) prior to detection by chemiluminescence (West Dura). After development and scanning, band intensities were quantified by ImageJ (NIH). Primary antibodies included: EGFR (1∶500, Santa Cruz Biotechnology Inc.), P-EGFR (1∶1000, Cell Signaling) Akt (1∶40,000, Cell Signaling), P-Akt (1∶20,000, Cell Signaling) PI3K (1∶40,000, Cell Signaling), GAPDH (1∶5,000,000, Sigma-Aldrich).
Immunostaining
U373-MG human GBM cells were seeded on polyacrylamide substrates of varying stiffnesses and allowed to equilibrate overnight before fixation. Cells were fixed with 4% paraformaldehyde in PBS, permeabilized using 0.1% Triton-X100 in PBS, and blocked using 5% goat serum in PBS prior to staining with the appropriate antibodies: P-EGFR (1∶250, Cell Signaling), Vinculin (1∶250, Sigma), DAPI (1∶200, Invitrogen). All fluorescence imaging were performed on a Prairie SFC confocal microscope
Pharmacologic inhibitor studies
U373-MG cells were cultured on fibronectin-coated polyacrylamide substrates of varying stiffness for at least 24 hours prior to treatment with a single pharmacologic inhibitor. Cell proliferation was measured 24 hours post treatment with the drug of interest according to the FitC-BrdU flow kit protocol as described above. Pharmacologic inhibitors included: Tyrphostin AG1478 (20 uM, Calbiochem), Triciribine (20 uM, Enzo Diagnostics), Wortmannin (20 uM, Sigma-Aldrich).
Reverse phase proteomic analysis (RPPA)
U373-MG and U87-MG cells were seeded on fibronectin-coated polyacrylamide substrates of varying stiffnesses. Total cellular protein was isolated using lysis buffer provided by the MD Anderson RPPA Core Facility and then sent to that facility for completion of RPPA following standard protocols (http://www.mdanderson.org/education-and-research/resources-for-professionals/scientific-resources/core-facilities-and-services/functional-proteomics-rppa-core/education-and-references/index.html).
Results
Microenvironmental stiffness influences proliferative signaling in glioma cells
To broadly explore whether stiffness-induced signals may influence the activity of proteins relevant to mitogenic signaling and proliferation, we harvested lysates from human GBM cells cultured on ECM protein-coated substrates of defined stiffness (from 0.08 kPa to 119 kPa) and used reverse phase protein array (RPPA) analysis to comparatively measure levels of a variety of proteins and phosphoproteins. In this technology, cell lysates are immobilized as spots onto a solid support, and each spot is probed with a distinct primary antibody directed against a known molecular target. Each spot is then incubated with a single biotin-tagged secondary antibody, which is then fluorescently labeled for quantification of target abundance. This approach therefore enables the parallel quantification of a large number of protein and phosphoprotein targets from the same lysate. We cultured U373-MG and U87-MG human glioma cells on substrates ranging from brain-like (0.08 kPa) to supraphysiological stiffness values (119 kPa) for 2 days in growth medium, harvested lysates, subjected the lysates to RPPA measurement, and analyzed the resulting data to identify proteins and phosphoproteins whose levels correlated significantly with stiffness (Spearman correlation coefficient R>0.5). Out of the 200 antibody targets that were probed by RPPA, the abundance of 48 correlated positively with stiffness for both U373-MG and U87-MG cells (Figure S1). Interestingly, more than one-quarter (∼27%) of these positive targets fell within pathways canonically associated with proliferation, including MAPK, RAF1, and Src (Figure S1; highlighted). Notably, EGFR levels were found to be significantly correlated with stiffness in U373-MG cells (r = 0.8205), as were the levels of two EGFR phosphoisoforms associated with EGFR auto-phosphorylation (Figure S1; r = 0.5830 and r = 0.5614 for pY106 and pY117, respectively). Finally, phosphorylation levels of the downstream EGFR signaling targets Akt and PI3K were strongly correlated with stiffness in both U373-MG (r = 0.8421 and 0.8205) and U87-MG cells (r = 0.5398 and 0.8205).
Microenvironmental stiffness regulates human glioma cell proliferation
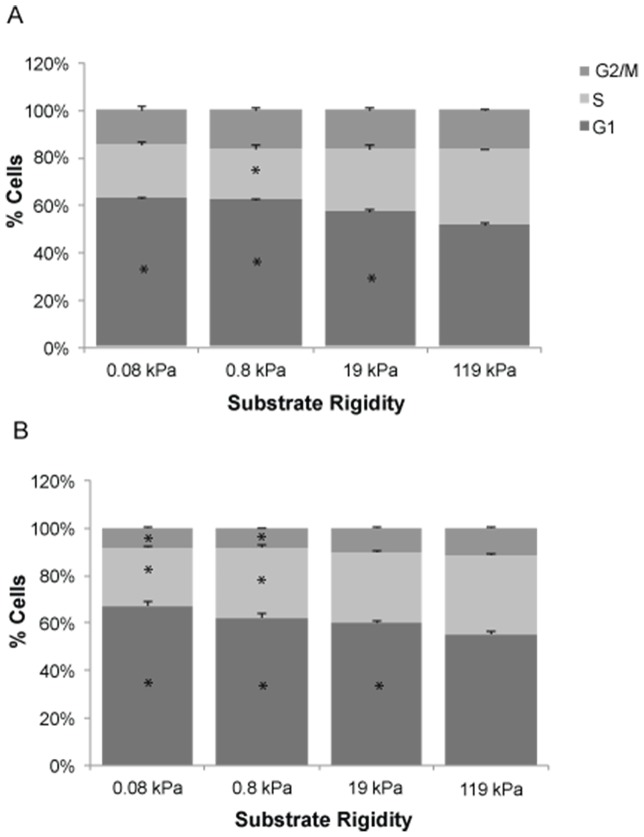
Given the broad correlations between substrate stiffness and the abundance of proteins and phosphoproteins associated with proliferation-related signaling, we next decided to directly quantify the extent to which substrate stiffness regulates proliferation. In a previous study [9] we showed that human GBM cells cultured on stiff substrates proliferated much more avidly than cells on highly compliant substrates of elasticity comparable to normal brain tissue. Because of the limited throughput and precision of the immunofluorescence-based bromodeoxyuridine (BrdU) incorporation method used in this earlier study, we first confirmed this result using a flow cytometry-based BrdU incorporation assay, which enables rapid analysis of tens of thousands of cells (Figure 1). We cultured cells on fibronectin-conjugated polyacrylamide hydrogels, transiently pulsed them with BrdU, harvested them from the substrate, and then measured the fraction of BrdU-positive cells by flow cytometry. Gradually increasing ECM stiffness from 0.08 kPa to 119 kPa dramatically enhanced proliferation in both U373-MG (Figure 1A) and U87-MG (Figure 1B) cells, with the stiffest ECM producing 2-3-fold more BrdU-positive cells than the softest ECM.
Figure 1. Microenvironmental stiffness regulates glioma cell proliferation.
Effect of ECM rigidity on proliferation of U373-MG (A) and U87-MG (B) cells. Results represent quantification of n>10,000 cells for at least three substrates per condition by flow cytometry, where the percentage of dividing cells was determined as the average percentage of cells staining positive for BrdU incorporation. *, P<0.05 with respect to 119 kPa.
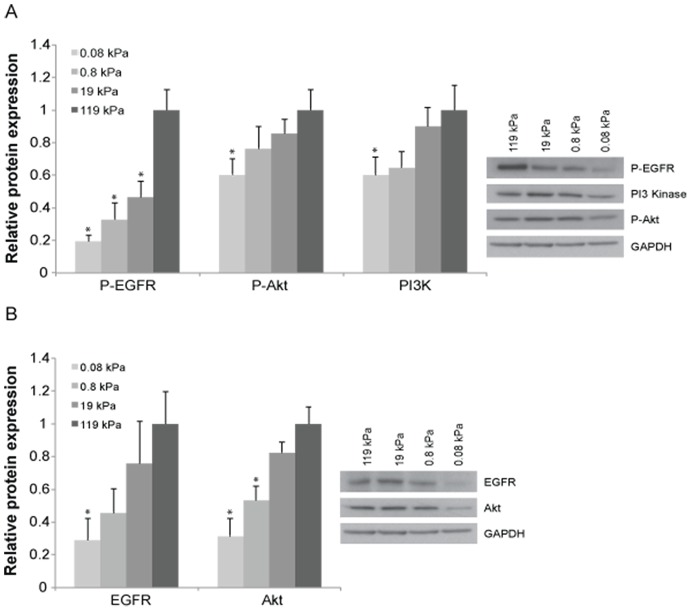
Stiff microenvironments enhance progression through the G1/S checkpoint of the cell cycle
To gain additional mechanistic insight into the dramatic increase in cell proliferation induced by microenvironmental stiffness, we asked whether this effect might be accompanied by changes in cell cycle distribution. We therefore performed additional flow cytometric studies in which we cultured GBM tumor cells on a range of defined-stiffness substrates, treated the cells with propidium iodide to mark DNA content, and performed flow cytometry to measure distribution across the G1, S, and G2/M phases of the cell cycle (Figure 2). For both U373-MG (Figure 2A) and U-87 MG (Figure 2B) cells, the majority of cells were in G1 phase across all stiffness values (Figure 2; dark gray). Interestingly, however, we noted that increasing ECM stiffness increased the percentage of cells in S phase (Figure 2; light gray), with concomitant reductions in the number of cells in G1. For U87-MG cells on the two softest ECMs considered, there was also a corresponding depletion of cells in G2/M phase. Taken together with our proliferation data (Figure 1), these results are consistent with a mechanism in which increasing microenvironmental stiffness accelerates proliferation by facilitating passage through the G1/S checkpoint.
Figure 2. ECM rigidity regulates glioma cell cycle distribution.
Effect of ECM rigidity on cell cycle distribution of U373-MG (A) and U87-MG (B) cells. Results represent quantification of n>10,000 cells for at least three substrates per condition by flow cytometry, where the percentage of cells in each phase of the cell cycle was determined as the average percentage of cells staining positive for propidium iodide incorporation. *, P<0.05 with respect to 119 kPa.
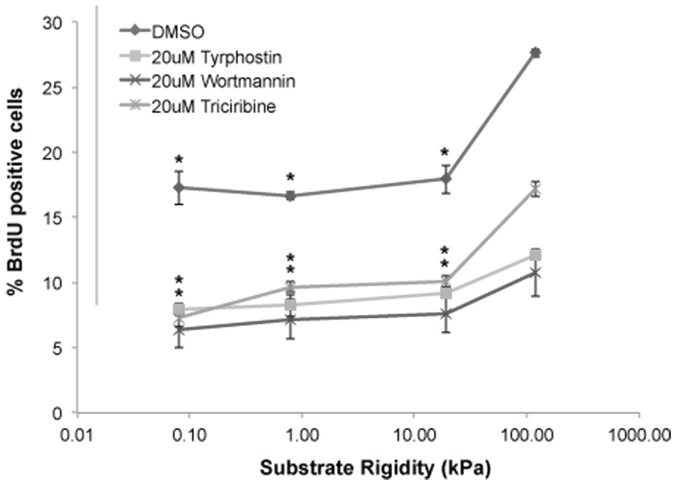
Increasing microenvironmental stiffness promotes expression and phosphorylation of EGFR-induced signals
Our flow cytometry results motivated us to consider potential molecular mechanisms through which increasing ECM stiffness might speed passage through the G1/S checkpoint. EGFR activation is known to promote proliferation in part by accelerating G1/S passage [36]–[39] and is among the most commonly aberrant genes in GBM. Given this and our RPPA finding that substrate stiffness is correlated with expression and phosphorylation of EGFR signaling proteins in both U373-MG cells (EGFR, pEGFR, Akt, pAkt, pPI3K) and U87-MG cells (Akt, pAkt, pPI3K), it occurred to us that ECM stiffness might act through EGFR signaling to promote cell cycle progression and proliferation [22]. However, an important caveat of RPPA is its comparatively limited dynamic range and sensitivity [40], which suits RPPA well for detecting broad correlations among experimental parameters but much less so for quantification of protein levels. To more precisely and quantitatively measure these potential stiffness-dependent proteomic changes, we used Western blots to determine if microenvironmental stiffness could alter expression or phosphorylation of EGFR or its downstream effectors Akt and PI3K (Figure 3A). Remarkably, increasing matrix stiffness from 0.08 kPa to 119 kPa produced a five-fold increase in phosphorylated EGFR (pEGFR) and nearly two-fold increases in phosphorylated Akt (pAkt) and total PI3K. Increasing matrix stiffness over this same range also strongly increased overall levels of EGFR and Akt (Figure 3B), suggesting that the enhancement of phosphorylation may result in part from greater overall levels of each protein. Importantly, these studies were conducted in the absence of exogenous EGF beyond levels already present in serum or secreted by cells. Thus, increasing microenvironmental stiffness broadly activates EGFR signaling in GBM tumor cells.
Figure 3. Microenvironmental stiffness regulates expression and phosphorylation of EGFR pathway components.
The expression of activated EGFR, activated Akt and PI3K in U373-MG cells rises with increasing substrate stiffness (A). Similarly, the expression levels of EGFR and Akt in U373-MG cells rise with increasing substrate stiffness (B). Results represent quantification of at least three biological replicates on three separate Western blots, where the relative protein expression levels have been first normalized to the expression of GAPDH and then normalized to the expression level on the stiffest substrate of 119 kPa. Representative blots for each protein are on the right. *, P<0.05 with respect to 119 kPa.
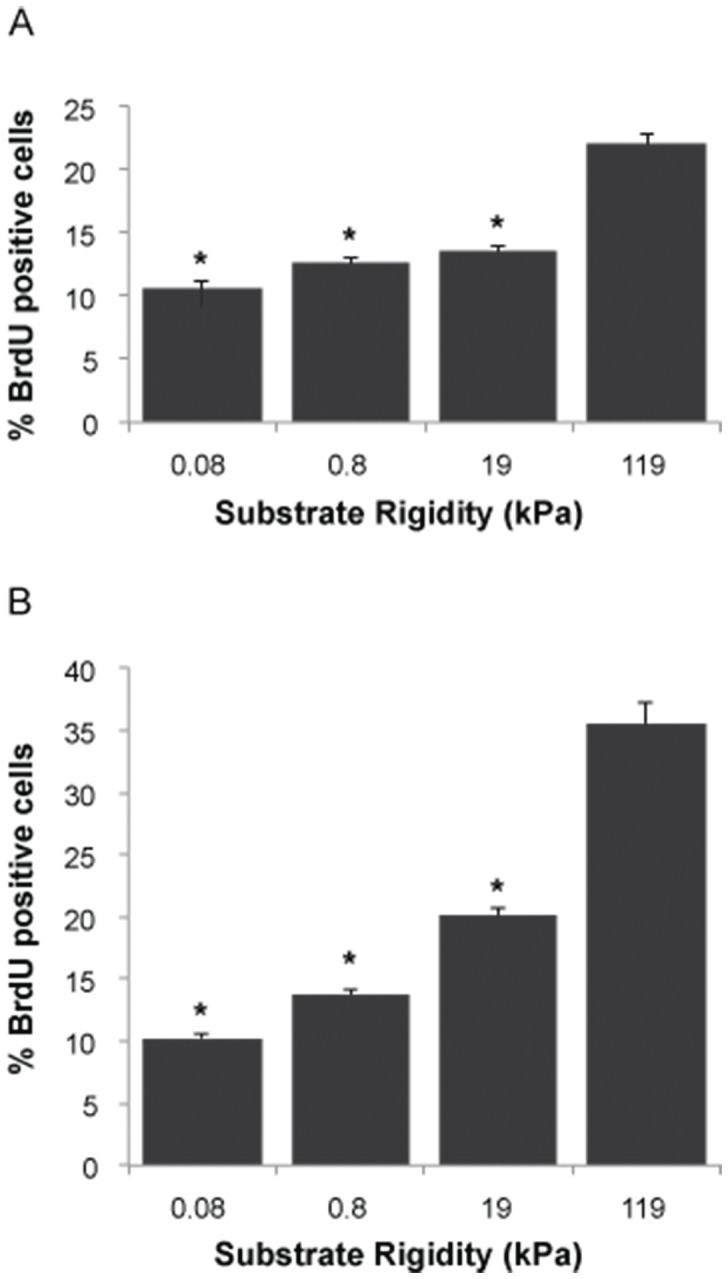
EGFR pathway inhibition renders proliferation significantly less sensitive to substrate stiffness
The above results indicate that increasing matrix stiffness enhances cell proliferation (Figure 1), facilitates passage through the G1/S checkpoint (Figure 2), and potentiates EGFR pathway activation (Figure 3A). To determine whether EGFR pathway activation is necessary for stiffness-induced proliferation, we performed studies in which we cultured cells on defined-stiffness substrates, treated them with pharmacologic inhibitors of EGFR kinase (Tyrphostin), Akt kinase (Triciribine), PI3K (Wortmannin), or, due to the known effects of DMSO on proliferation [41], [42], a DMSO-only control. The specificity and efficacy of these drugs have been extensively characterized in previous studies [43]–[45]. We then repeated BrdU flow cytometric analysis to determine EGFR pathway-dependent effects on cell proliferation. As expected, DMSO-treated U373-MG controls strongly exhibited stiffness-dependent proliferation as observed earlier (Fig. 1). However, treatment with any of the three inhibitors both reduced overall levels of proliferation and desensitized proliferation to stiffness, with the strongest effect observed for EGFR and PI3K inhibition (Figure 4). Thus, GBM tumor cell proliferation is substantially less sensitive to ECM stiffness when EGFR signaling is reduced, implying that matrix stiffness acts in part through EGFR-mediated signaling pathways to promote proliferation.
Figure 4. Stifffness-dependent glioma cell proliferation is dampened upon treatment with 20 uM EGFR inhibitor - Tyrphostin, 20 uM Akt inhibitor - Triciribine, and 20 uM PI3 Kinase inhibitor - Wortmannin for 24 hours as compared with the DMSO negative control.
Results represent quantification of n>10,000 cells for at least three substrates per condition by flow cytometry, where the percentage of dividing cells was determined as the average percentage of cells staining positive for BrdU incorporation *, P<0.05 with respect to 119 kPa for DMSO control, 20 uM Tyrphostin and 20 uM Triciribine.
Changes in microenvironmental stiffness alter EGFR organization and co-localization with focal adhesions
Modulation of tissue stiffness is widely understood to control cell physiology through a number of proximal signals, perhaps the most well-studied of which is assembly of integrin-based adhesion complexes. These adhesions can influence growth factor signaling in a number of important ways, including locally concentrating growth factor receptors and recruiting key mitogenic signaling intermediates such as focal adhesion kinase (FAK) and PI3K. This is important in that EGFR activation is strongly amplified by spatial clustering of the receptor and its downstream effectors [46]. To determine whether matrix stiffness might influence the assembly of EGFR, we cultured U373-MG cells on defined-stiffness matrices and used immunofluorescence to examine colocalization of EGFR and focal adhesion proteins (Figure 5). As expected from our and others' previous studies [9], [47], soft ECMs gave rise to immature, punctate vinculin-positive focal complexes, with stiffer ECMs yielding larger and more elongated focal adhesions. Strikingly, these changes in substrate stiffness also concomitantly enhanced pEGFR clustering, with pEGFR strongly co-localizing with vinculin-positive focal adhesions and forming large structures on stiff matrices. Thus, increasing microenvironmental stiffness promotes the clustering and colocalization of both integrin-based focal adhesion complexes and pEGFR.
Figure 5. Colocalization of focal adhesion of phospho-EGFR.
U373-MG cells were cultured on soft (A, C, E) or stiff (B, D, F) polyacrylamide hydrogels and immunofluorescently stained for vinculin (A, B) and phospo-EGFR (C, D). There are no punctate vinculin-positive focal adhesions on soft substrates (A), while there are large focal adhesions on stiff substrates (C). On stiff substrates, there are distinct, punctate pEGFR structures (D; arrows) that colocalize with vinculin positive adhesions (F; arrows). The colocalization is more clearly evident in the high-magnification insets (B, D). Scale bar is 50 microns.
Discussion
Our study shows that microenvironmental stiffness increases the expression and/or phosphorylation of EGFR and its downstream effectors, and that stiffness-dependent signals stimulate proliferation by acting in part through EGFR-based mitogenic signaling. While the precise mechanism of this interaction remains to be fully elucidated, the strong, stiffness-dependent colocalization of pEGFR with focal adhesion components is consistent with a model in which tissue stiffening promotes GBM proliferation by spatially and biochemically amplifying EGFR signaling. If this is the case, then mechanotransductive and EGFR-based signals may act synergistically to regulate cell proliferation in GBM.
Previous research has suggested the possibility of cooperativity between mechanical inputs and growth factor signaling. Many growth factor receptors including EGFR can interact both directly and indirectly with a variety of integrin subtypes and colocalize within integrin-based adhesions [48]–[51]. Moreover, studies using both in vitro and mouse models of various tumors have suggested that integrin clustering and matrix stiffness may be at least partially responsible for enhanced PI3K signaling. For example, inhibition of PI3K signaling was found to neutralize the tumor-promoting effects of matrix stiffness in a mouse model of breast cancer [32]. Furthermore, reducing substrate stiffness normalized invasive, disorganized colonies formed by EGFR-transformed mammary epithelial cells cultured in reconstituted basement membrane matrices [6]. Moreover, changes in matrix stiffness have previously been shown to alter cell cycle progression in mammary epithelial cells, smooth muscle cells, fibroblasts, and other non-neuroglial cell types [33], [52]. While this body of work implies fundamental connections between growth factor receptors, their canonical downstream targets, and mechanotransductive signaling systems in regulating tumor propagation and invasion, relatively little is known regarding the underlying phenotypic mechanisms or if these findings extend to other tumors. Our results begin to fill this gap by supporting the notion that EGFR- and mechanotransductive signaling act in tandem to promote proliferation in GBM cells, although further investigations are necessary to determine if this is a general phenomenon of mechanosensing or is specific to GBM and perhaps other tumor types. A key limitation of our studies is the use of highly reductionist culture models, which was necessary to cleanly isolate stiffness as an experimental variable. However, future studies in which EGFR and mechanotransductive signals are simultaneously manipulated in vivo (e.g. in orthotopic xenograft paradigms) should help clarify the physiological role of this phenomenon and the relative influence of other inputs that may modulate PI3K/Akt signaling in vivo. These studies would also serve as an important check against our pharmacological inhibition studies, where legitimate concerns may exist about target specificity.
We show that focal adhesions and EGFR co-localize on stiff but not soft substrates, suggesting that enhanced EGFR clustering on stiff substrates may be driven in part by interactions between focal adhesion proteins and EGFR. Importantly, forced clustering of EGFR mutants enhanced tumorgenicity and decreased survival time in a mouse xenograft model of GBM [53]. Much previous work supports the existence of interactions between focal adhesion proteins and EGFR, with many of these efforts focusing specifically on the interaction between focal adhesion kinase (FAK) and EGFR. FAK is a ubiquitously expressed tyrosine kinase that contains an N-terminal FERM domain and a C-terminal focal-adhesion targeting domain (FAT) [54]. The FERM domain has been shown to bind to certain growth factor receptors, including EGFR, while the FAT domain causes FAK to localize to focal adhesions. Focal adhesion-localized EGFR then signals directly through the Band-4.1 domain on FAK, thereby providing a direct link between known mechanosensory machinery and the EGFR pathway [49]. The importance of this connection is highlighted by experiments in mouse models of breast cancer, where FAK is required for ErbB2/3 mediated oncogenic transformation and lung metastases of MDA-231-M2 cell injected into the mammary fat pad [55]. This FAK-based connection may have clinical significance given that FAK inhibition was recently shown to sensitize GBM cells to PD153035-induced EGFR inhibition [56]. Thus, in the future it should be valuable to more precisely dissect the role of FAK in coupling mechanotransductive and EGFR-dependent control of GBM proliferation.
One somewhat unexpected finding from our study is that increases in microenvironmental stiffness increase total levels of EGFR and its downstream effectors, in addition to levels of the corresponding phosphoproteins. This implies that substrate stiffness may influence the transcription, translation, and/or degradation of these proteins. While surprising, similar effects have been observed in breast tumor cells grown in three-dimensional reconstituted basement membrane, where EGFR overexpression has been found to trigger compensatory α1 integrin upregulation [48]. Similarly, total and phospho-EGFR levels are reduced when cytoskeletal tension is relaxed in mammary epithelial cells [6]. Numerous other studies have established a link between mechanotransductive signaling and transcriptional regulation [57]–[59], in which activation of mechanotransductive signals at the plasma membrane may influence transcription through traditional signal transduction events or more hypothetically through direct mechanical deformation of the nucleus [60], [61].
In conclusion, we have investigated interactions between microenvironemental stiffness and EGFR-dependent signaling in controlling cell cycle and proliferation. Our data are broadly consistent with a model in which stiffness enhances EGFR-dependent signaling to regulate proliferation. As GBM tumors are known to be stiffer than normal brain tissue, these stiffness changes may modulate cell proliferation in vivo. An important limitation in making this connection in a more literal way is the relative absence of quantitative measurements of tumor stiffness, which remains technically challenging. As these values become available, it will be informative to revisit these studies with materials designed to tightly bracket that range. Finally, while it may be premature to speculate on the clinical implications of this finding, our results raise the interesting possibility that modulation of microenvironmental mechanics and/or mechanotransductive signaling systems may be used to potentiate the effects of EGFR and PI3K inhibitors. While these small-molecule inhibitors have shown great promise in preclinical studies and early clinical trials, much room certainly remains for improvement [62]–[64]. Analogously, integrins are under evaluation as therapeutic targets in GBM, with an RGD peptide inhibitor showing modest increases in progression-free survival in phase II clinical trials and failed to do so in phase III trials [65], [66]. Co-administration of EGFR pathway inhibitors and agents that modulate the mechanotransduction machinery may thus enhance the activity of both agents. There is ample precedent for such co-administration strategies; for example, in vivo mouse studies have suggested that using Y15, a FAK autophosphorylation inhibitor, synergistically with temozolomide is a more effective at preventing tumor growth than either drug alone [17]. It will be important to carefully and systematically evaluate these concepts in both primary human GBM xenografts and other preclinical models.
Supporting Information
Microenvironmental stiffness-dependent regulation of proteins in U373-MG and U87-MG cells. U373-MG and U87-MG human glioma cells were cultured on one of four defined-stiffness substrates and then subjected to reverse phase protein array (RPPA) analysis. Correlations between substrate stiffness and protein expression were quantified by Spearman correlation analysis for each cell type. A significant correlation is defined as a correlation coefficient (R) of absolute value greater than 0.5. The table includes only proteins whose levels correlate significantly with stiffness in both U373-MG and U87-87 cells, U373-MG only, or U87-MG only. For proteins that correlate significantly with both cell lines, R values are the reported as the average of the absolute values of the R values for the individual cell lines. All other R values are reported as the absolute vale of the R score. Proteins known to be related to proliferation are highlighted in yellow.
(DOCX)
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All data are included within the paper.
Funding Statement
A.R. gratefully acknowledges the support of a National Institutes of Health NRSA postdoctoral fellowship (1F32CA174361). S.K. gratefully acknowledges support from the National Institutes of Health (1DP2OD004213 and 1U54CA143836) and National Science Foundation (CMMI PESO 1105539). The MD Anderson RPPA Core facility is funded by a grant through the National Cancer Institute (2P30CA016672). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Agnihotri S, Burrell KE, Wolf A, Jalali S, Hawkins C, et al. (2013) Glioblastoma, a brief review of history, molecular genetics, animal models and novel therapeutic strategies. Arch Immunol Ther Exp (Warsz) 61: 25–41 10.1007/s00005-012-0203-0 [DOI] [PubMed] [Google Scholar]
- 2. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, et al. (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352: 987–996 10.1056/NEJMoa043330 [DOI] [PubMed] [Google Scholar]
- 3. Berens ME, Giese A (1999) “…those left behind.” Biology and Oncology of Invasive Glioma Cells. Neoplasia N Y N 1: 208–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Unsgaard G, Rygh OM, Selbekk T, Müller TB, Kolstad F, et al. (2006) Intra-operative 3D ultrasound in neurosurgery. Acta Neurochir (Wien) 148: 235–253 discussion 253 10.1007/s00701-005-0688-y [DOI] [PubMed] [Google Scholar]
- 5. Lopez JI, Kang I, You W-K, McDonald DM, Weaver VM (2011) In situ force mapping of mammary gland transformation. Integr Biol Quant Biosci Nano Macro 3: 910–921 10.1039/c1ib00043h [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paszek MJ, Zahir N, Johnson KR, Lakins JN, Rozenberg GI, et al. (2005) Tensional homeostasis and the malignant phenotype. Cancer Cell 8: 241–254 10.1016/j.ccr.2005.08.010 [DOI] [PubMed] [Google Scholar]
- 7. Elkin BS, Azeloglu EU, Costa KD, Morrison B 3rd (2007) Mechanical heterogeneity of the rat hippocampus measured by atomic force microscope indentation. J Neurotrauma 24: 812–822 10.1089/neu.2006.0169 [DOI] [PubMed] [Google Scholar]
- 8. Lefranc F, Brotchi J, Kiss R (2005) Possible future issues in the treatment of glioblastomas: special emphasis on cell migration and the resistance of migrating glioblastoma cells to apoptosis. J Clin Oncol Off J Am Soc Clin Oncol 23: 2411–2422 10.1200/JCO.2005.03.089 [DOI] [PubMed] [Google Scholar]
- 9. Ulrich TA, de Juan Pardo EM, Kumar S (2009) The mechanical rigidity of the extracellular matrix regulates the structure, motility, and proliferation of glioma cells. Cancer Res 69: 4167–4174 10.1158/0008-5472.CAN-08-4859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ananthanarayanan B, Kim Y, Kumar S (2011) Elucidating the mechanobiology of malignant brain tumors using a brain matrix-mimetic hyaluronic acid hydrogel platform. Biomaterials 32: 7913–7923 10.1016/j.biomaterials.2011.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Belot N, Rorive S, Doyen I, Lefranc F, Bruyneel E, et al. (2001) Molecular characterization of cell substratum attachments in human glial tumors relates to prognostic features. Glia 36: 375–390. [DOI] [PubMed] [Google Scholar]
- 12. Friedlander DR, Zagzag D, Shiff B, Cohen H, Allen JC, et al. (1996) Migration of brain tumor cells on extracellular matrix proteins in vitro correlates with tumor type and grade and involves alphaV and beta1 integrins. Cancer Res 56: 1939–1947. [PubMed] [Google Scholar]
- 13. Paulus W, Baur I, Schuppan D, Roggendorf W (1993) Characterization of integrin receptors in normal and neoplastic human brain. Am J Pathol 143: 154–163. [PMC free article] [PubMed] [Google Scholar]
- 14. Lathia JD, Gallagher J, Heddleston JM, Wang J, Eyler CE, et al. (2010) Integrin alpha 6 regulates glioblastoma stem cells. Cell Stem Cell 6: 421–432 10.1016/j.stem.2010.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gingras MC, Roussel E, Bruner JM, Branch CD, Moser RP (1995) Comparison of cell adhesion molecule expression between glioblastoma multiforme and autologous normal brain tissue. J Neuroimmunol 57: 143–153. [DOI] [PubMed] [Google Scholar]
- 16. Lathia JD, Li M, Hall PE, Gallagher J, Hale JS, et al. (2012) Laminin alpha 2 enables glioblastoma stem cell growth. Ann Neurol 72: 766–778 10.1002/ana.23674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Golubovskaya VM, Huang G, Ho B, Yemma M, Morrison CD, et al. (2013) Pharmacologic blockade of FAK autophosphorylation decreases human glioblastoma tumor growth and synergizes with temozolomide. Mol Cancer Ther 12: 162–172 10.1158/1535-7163.MCT-12-0701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Natarajan M, Hecker TP, Gladson CL (2003) FAK signaling in anaplastic astrocytoma and glioblastoma tumors. Cancer J Sudbury Mass 9: 126–133. [DOI] [PubMed] [Google Scholar]
- 19. Hirata E, Yukinaga H, Kamioka Y, Arakawa Y, Miyamoto S, et al. (2012) In vivo fluorescence resonance energy transfer imaging reveals differential activation of Rho-family GTPases in glioblastoma cell invasion. J Cell Sci 125: 858–868 10.1242/jcs.089995 [DOI] [PubMed] [Google Scholar]
- 20. Ivkovic S, Beadle C, Noticewala S, Massey SC, Swanson KR, et al. (2012) Direct inhibition of myosin II effectively blocks glioma invasion in the presence of multiple motogens. Mol Biol Cell 23: 533–542 10.1091/mbc.E11-01-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Beadle C, Assanah MC, Monzo P, Vallee R, Rosenfeld SS, et al. (2008) The Role of Myosin II in Glioma Invasion of the Brain. Mol Biol Cell 19: 3357–3368 10.1091/mbc.E08-03-0319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Verhaak RGW, Hoadley KA, Purdom E, Wang V, Qi Y, et al. (2010) An integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR and NF1. Cancer Cell 17: 98 10.1016/j.ccr.2009.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Furnari FB, Fenton T, Bachoo RM, Mukasa A, Stommel JM, et al. (2007) Malignant astrocytic glioma: genetics, biology, and paths to treatment. Genes Dev 21: 2683–2710 10.1101/gad.1596707 [DOI] [PubMed] [Google Scholar]
- 24. Taylor TE, Furnari FB, Cavenee WK (2012) Targeting EGFR for Treatment of Glioblastoma: Molecular Basis to Overcome Resistance. Curr Cancer Drug Targets 12: 197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lui VWY, Grandis JR (2002) EGFR-mediated cell cycle regulation. Anticancer Res 22: 1–11. [PubMed] [Google Scholar]
- 26. Jones TS, Holland EC (2011) Molecular pathogenesis of malignant glial tumors. Toxicol Pathol 39: 158–166 10.1177/0192623310387617 [DOI] [PubMed] [Google Scholar]
- 27. Shinojima N, Tada K, Shiraishi S, Kamiryo T, Kochi M, et al. (2003) Prognostic value of epidermal growth factor receptor in patients with glioblastoma multiforme. Cancer Res 63: 6962–6970. [PubMed] [Google Scholar]
- 28. Mishima K, Johns TG, Luwor RB, Scott AM, Stockert E, et al. (2001) Growth suppression of intracranial xenografted glioblastomas overexpressing mutant epidermal growth factor receptors by systemic administration of monoclonal antibody (mAb) 806, a novel monoclonal antibody directed to the receptor. Cancer Res 61: 5349–5354. [PubMed] [Google Scholar]
- 29. Fan Q-W, Knight ZA, Goldenberg DD, Yu W, Mostov KE, et al. (2006) A dual PI3 kinase/mTOR inhibitor reveals emergent efficacy in glioma. Cancer Cell 9: 341–349 10.1016/j.ccr.2006.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Raynaud FI, Eccles SA, Patel S, Alix S, Box G, et al. (2009) Biological properties of potent inhibitors of class I phosphatidylinositide 3-kinases: from PI-103 through PI-540, PI-620 to the oral agent GDC-0941. Mol Cancer Ther 8: 1725–1738 10.1158/1535-7163.MCT-08-1200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Joy AM, Beaudry CE, Tran NL, Ponce FA, Holz DR, et al. (2003) Migrating glioma cells activate the PI3-K pathway and display decreased susceptibility to apoptosis. J Cell Sci 116: 4409–4417 10.1242/jcs.00712 [DOI] [PubMed] [Google Scholar]
- 32. Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, et al. (2009) Matrix Crosslinking Forces Tumor Progression by Enhancing Integrin signaling. Cell 139: 891–906 10.1016/j.cell.2009.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Klein EA, Yin L, Kothapalli D, Castagnino P, Byfield FJ, et al. (2009) Cell-cycle control by physiological matrix elasticity and in vivo tissue stiffening. Curr Biol CB 19: 1511–1518 10.1016/j.cub.2009.07.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Torsvik A, Røsland GV, Svendsen A, Molven A, Immervoll H, et al. (2010) Spontaneous malignant transformation of human mesenchymal stem cells reflects cross-contamination: putting the research field on track - letter. Cancer Res 70: 6393–6396 10.1158/0008-5472.CAN-10-1305 [DOI] [PubMed] [Google Scholar]
- 35. Stepanenko AA, Kavsan VM (2014) Karyotypically distinct U251, U373, and SNB19 glioma cell lines are of the same origin but have different drug treatment sensitivities. Gene 540: 263–265 10.1016/j.gene.2014.02.053 [DOI] [PubMed] [Google Scholar]
- 36. Owa T, Yoshino H, Yoshimatsu K, Nagasu T (2001) Cell cycle regulation in the G1 phase: a promising target for the development of new chemotherapeutic anticancer agents. Curr Med Chem 8: 1487–1503. [DOI] [PubMed] [Google Scholar]
- 37.Collin de l'Hortet A, Gilgenkrantz H, Guidotti J-E (2012) EGFR: A Master Piece in G1/S Phase Transition of Liver Regeneration. Int J Hepatol 2012. Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3461622/. Accessed 3 February 2014. [DOI] [PMC free article] [PubMed]
- 38. Collins NL, Reginato MJ, Paulus JK, Sgroi DC, Labaer J, et al. (2005) G1/S cell cycle arrest provides anoikis resistance through Erk-mediated Bim suppression. Mol Cell Biol 25: 5282–5291 10.1128/MCB.25.12.5282-5291.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sahin Ö, Fröhlich H, Löbke C, Korf U, Burmester S, et al. (2009) Modeling ERBB receptor-regulated G1/S transition to find novel targets for de novo trastuzumab resistance. BMC Syst Biol 3: 1 10.1186/1752-0509-3-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Brennan DJ, O'Connor DP, Rexhepaj E, Ponten F, Gallagher WM (2010) Antibody-based proteomics: fast-tracking molecular diagnostics in oncology. Nat Rev Cancer 10: 605–617 10.1038/nrc2902 [DOI] [PubMed] [Google Scholar]
- 41. Kaneski CR, Constantopoulos G, Brady RO (1991) Effect of dimethylsulfoxide on the proliferation and glycosaminoglycan synthesis of rat prostate adenocarcinoma cells (PAIII) in vitro: isolation and characterization of DMSO-resistant cells. The Prostate 18: 47–58. [DOI] [PubMed] [Google Scholar]
- 42. Grunt TW, Somay C, Pavelka M, Ellinger A, Dittrich E, et al. (1991) The effects of dimethyl sulfoxide and retinoic acid on the cell growth and the phenotype of ovarian cancer cells. J Cell Sci 100 (Pt 3): 657–666. [DOI] [PubMed] [Google Scholar]
- 43. Wymann MP, Bulgarelli-Leva G, Zvelebil MJ, Pirola L, Vanhaesebroeck B, et al. (1996) Wortmannin inactivates phosphoinositide 3-kinase by covalent modification of Lys-802, a residue involved in the phosphate transfer reaction. Mol Cell Biol 16: 1722–1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yaish P, Gazit A, Gilon C, Levitzki A (1988) Blocking of EGF-dependent cell proliferation by EGF receptor kinase inhibitors. Science 242: 933–935. [DOI] [PubMed] [Google Scholar]
- 45. Yang L, Dan HC, Sun M, Liu Q, Sun X, et al. (2004) Akt/Protein Kinase B Signaling Inhibitor-2, a Selective Small Molecule Inhibitor of Akt Signaling with Antitumor Activity in Cancer Cells Overexpressing Akt. Cancer Res 64: 4394–4399 10.1158/0008-5472.CAN-04-0343 [DOI] [PubMed] [Google Scholar]
- 46. Stabley D, Retterer S, Marshall S, Salaita K (2013) Manipulating the lateral diffusion of surface-anchored EGF demonstrates that receptor clustering modulates phosphorylation levels. Integr Biol 5: 659–668 10.1039/C3IB20239A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pelham RJ, Wang Y (1997) Cell locomotion and focal adhesions are regulated by substrate flexibility. Proc Natl Acad Sci U S A 94: 13661–13665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang F, Weaver VM, Petersen OW, Larabell CA, Dedhar S, et al. (1998) Reciprocal interactions between β1-integrin and epidermal growth factor receptor in three-dimensional basement membrane breast cultures: A different perspective in epithelial biology. Proc Natl Acad Sci 95: 14821–14826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sieg DJ, Hauck CR, Ilic D, Klingbeil CK, Schaefer E, et al. (2000) FAK integrates growth-factor and integrin signals to promote cell migration. Nat Cell Biol 2: 249–256 10.1038/35010517 [DOI] [PubMed] [Google Scholar]
- 50. Lu Z, Jiang G, Blume-Jensen P, Hunter T (2001) Epidermal growth factor-induced tumor cell invasion and metastasis initiated by dephosphorylation and downregulation of focal adhesion kinase. Mol Cell Biol 21: 4016–4031 10.1128/MCB.21.12.4016-4031.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cabodi S, Moro L, Bergatto E, Boeri Erba E, Di Stefano P, et al. (2004) Integrin regulation of epidermal growth factor (EGF) receptor and of EGF-dependent responses. Biochem Soc Trans 32: 438–442 10.1042/BST0320438 [DOI] [PubMed] [Google Scholar]
- 52. Mih JD, Marinkovic A, Liu F, Sharif AS, Tschumperlin DJ (2012) Matrix stiffness reverses the effect of actomyosin tension on cell proliferation. J Cell Sci 125: 5974–5983 10.1242/jcs.108886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hwang Y, Chumbalkar V, Latha K, Bogler O (2011) Forced Dimerization Increases the Activity of ΔEGFR/EGFRvIII and Enhances Its Oncogenicity. Mol Cancer Res MCR 9: 1199–1208 10.1158/1541-7786.MCR-11-0229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mitra SK, Hanson DA, Schlaepfer DD (2005) Focal adhesion kinase: in command and control of cell motility. Nat Rev Mol Cell Biol 6: 56–68 10.1038/nrm1549 [DOI] [PubMed] [Google Scholar]
- 55. Benlimame N, He Q, Jie S, Xiao D, Xu YJ, et al. (2005) FAK signaling is critical for ErbB-2/ErbB-3 receptor cooperation for oncogenic transformation and invasion. J Cell Biol 171: 505–516 10.1083/jcb.200504124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Srikanth M, Das S, Berns EJ, Kim J, Stupp SI, et al. (2013) Nanofiber-mediated inhibition of focal adhesion kinase sensitizes glioma stemlike cells to epidermal growth factor receptor inhibition. Neuro-Oncol 15: 319–329 10.1093/neuonc/nos316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Engler AJ, Sen S, Sweeney HL, Discher DE (2006) Matrix elasticity directs stem cell lineage specification. Cell 126: 677–689 10.1016/j.cell.2006.06.044 [DOI] [PubMed] [Google Scholar]
- 58. Shih Y-RV, Tseng K-F, Lai H-Y, Lin C-H, Lee OK (2011) Matrix stiffness regulation of integrin-mediated mechanotransduction during osteogenic differentiation of human mesenchymal stem cells. J Bone Miner Res Off J Am Soc Bone Miner Res 26: 730–738 10.1002/jbmr.278 [DOI] [PubMed] [Google Scholar]
- 59. Dupont S, Morsut L, Aragona M, Enzo E, Giulitti S, et al. (2011) Role of YAP/TAZ in mechanotransduction. Nature 474: 179–183 10.1038/nature10137 [DOI] [PubMed] [Google Scholar]
- 60. Kook S-H, Jang Y-S, Lee J-C (2011) Involvement of JNK-AP-1 and ERK-NF-κB signaling in tension-stimulated expression of Type I collagen and MMP-1 in human periodontal ligament fibroblasts. J Appl Physiol 111: 1575–1583 10.1152/japplphysiol.00348.2011 [DOI] [PubMed] [Google Scholar]
- 61. Wang N, Tytell JD, Ingber DE (2009) Mechanotransduction at a distance: mechanically coupling the extracellular matrix with the nucleus. Nat Rev Mol Cell Biol 10: 75–82 10.1038/nrm2594 [DOI] [PubMed] [Google Scholar]
- 62. Gan HK, Kaye AH, Luwor RB (2009) The EGFRvIII variant in glioblastoma multiforme. J Clin Neurosci Off J Neurosurg Soc Australas 16: 748–754 10.1016/j.jocn.2008.12.005 [DOI] [PubMed] [Google Scholar]
- 63. Raizer JJ, Abrey LE, Lassman AB, Chang SM, Lamborn KR, et al. (2010) A phase II trial of erlotinib in patients with recurrent malignant gliomas and nonprogressive glioblastoma multiforme postradiation therapy. Neuro-Oncol 12: 95–103 10.1093/neuonc/nop015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Halatsch M-E, Gehrke EE, Vougioukas VI, Bötefür IC, A-Borhani F, et al. (2004) Inverse correlation of epidermal growth factor receptor messenger RNA induction and suppression of anchorage-independent growth by OSI-774, an epidermal growth factor receptor tyrosine kinase inhibitor, in glioblastoma multiforme cell lines. J Neurosurg 100: 523–533 10.3171/jns.2004.100.3.0523 [DOI] [PubMed] [Google Scholar]
- 65. Reardon DA, Fink KL, Mikkelsen T, Cloughesy TF, O'Neill A, et al. (2008) Randomized Phase II Study of Cilengitide, an Integrin-Targeting Arginine-Glycine-Aspartic Acid Peptide, in Recurrent Glioblastoma Multiforme. J Clin Oncol 26: 5610–5617 10.1200/JCO.2008.16.7510 [DOI] [PubMed] [Google Scholar]
- 66.Stupp R, Hegi ME, Gorlia T, Erridge S, Grujicic D, et al. (2013) Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma and methylated O6-methylguanine-DNA methyltransferase (MGMT) gene promoter: Key results of the multicenter, randomized, open-label, controlled, phase III CENTRIC study. J Clin Oncol 31 . Available: http://meetinglibrary.asco.org/content/112780-132. Accessed 8 May 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Microenvironmental stiffness-dependent regulation of proteins in U373-MG and U87-MG cells. U373-MG and U87-MG human glioma cells were cultured on one of four defined-stiffness substrates and then subjected to reverse phase protein array (RPPA) analysis. Correlations between substrate stiffness and protein expression were quantified by Spearman correlation analysis for each cell type. A significant correlation is defined as a correlation coefficient (R) of absolute value greater than 0.5. The table includes only proteins whose levels correlate significantly with stiffness in both U373-MG and U87-87 cells, U373-MG only, or U87-MG only. For proteins that correlate significantly with both cell lines, R values are the reported as the average of the absolute values of the R values for the individual cell lines. All other R values are reported as the absolute vale of the R score. Proteins known to be related to proliferation are highlighted in yellow.
(DOCX)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All data are included within the paper.