Abstract
The degeneration of nigral dopaminergic neurons in Parkinson disease is believed to be associated with oxidative stress. Since iron levels are increased in the substantia nigra of parkinsonian patients and this metal catalyzes the formation of free radicals, it may be involved in the mechanisms of nerve cell death. The cause of nigral iron increase is not understood. Iron acquisition by neurons may occur from iron-transferrin complexes with a direct interaction with specific membrane receptors, but recent results have shown a low density of transferrin receptors in the substantia nigra. To investigate whether neuronal death in Parkinson disease may be associated with changes in a pathway supplementary to that of transferrin, lactoferrin (lactotransferrin) receptor expression was studied in the mesencephalon. In this report we present evidence from immunohistochemical staining of postmortem human brain tissue that lactoferrin receptors are localized on neurons (perikarya, dendrites, axons), cerebral microvasculature, and, in some cases, glial cells. In parkinsonian patients, lactoferrin receptor immunoreactivity on neurons and microvessels was increased and more pronounced in those regions of the mesencephalon where the loss of dopaminergic neurons is severe. Moreover, in the substantia nigra, the intensity of immunoreactivity on neurons and microvessels was higher for patients with higher nigral dopaminergic loss. These data suggest that lactoferrin receptors on vulnerable neurons may increase intraneuronal iron levels and contribute to the degeneration of nigral dopaminergic neurons in Parkinson disease.
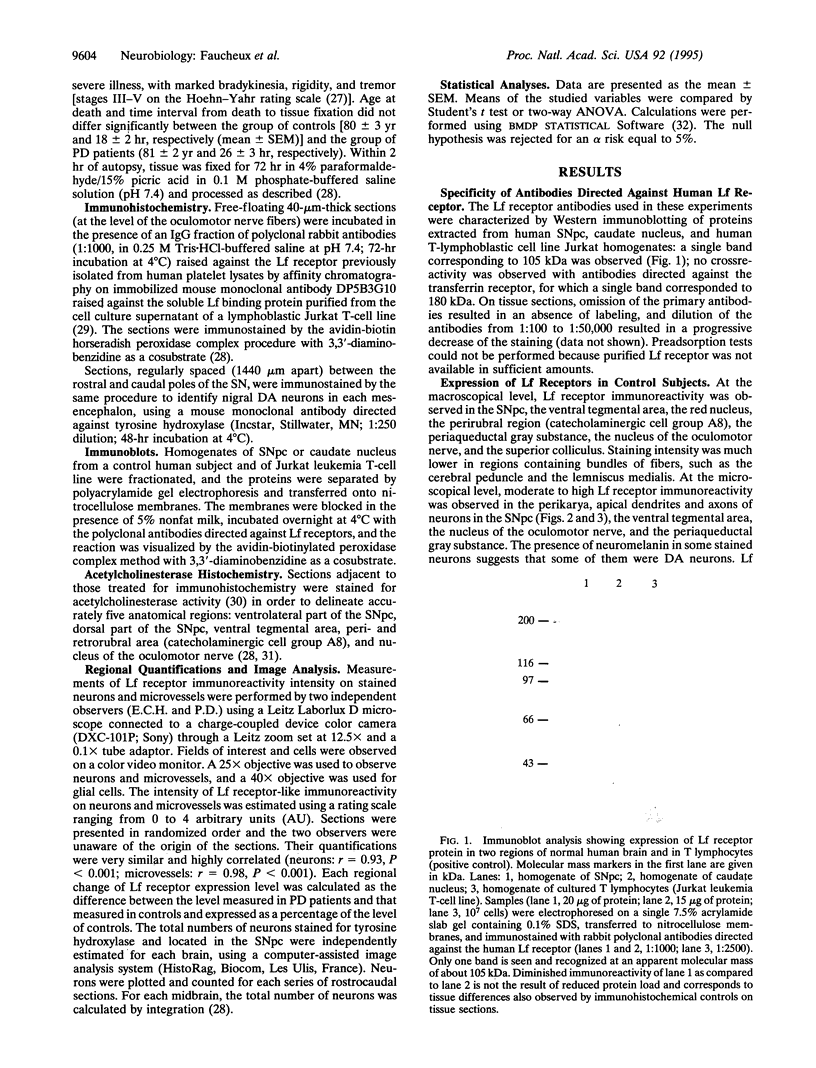
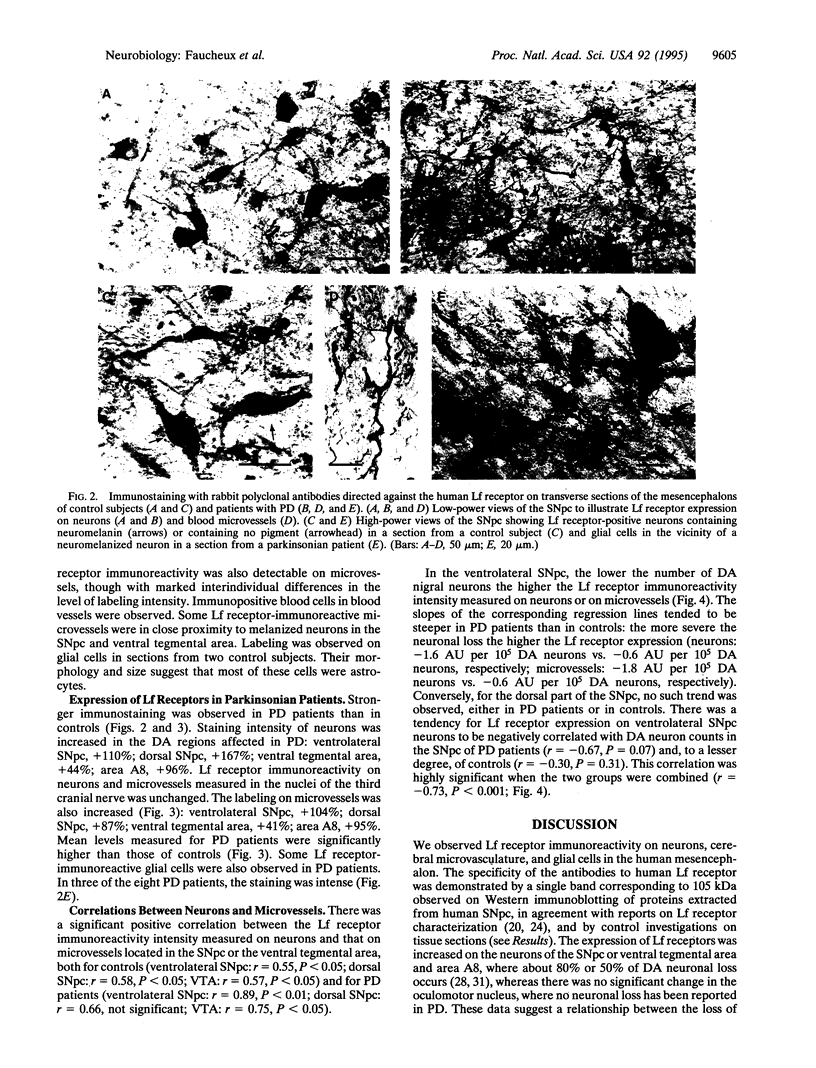
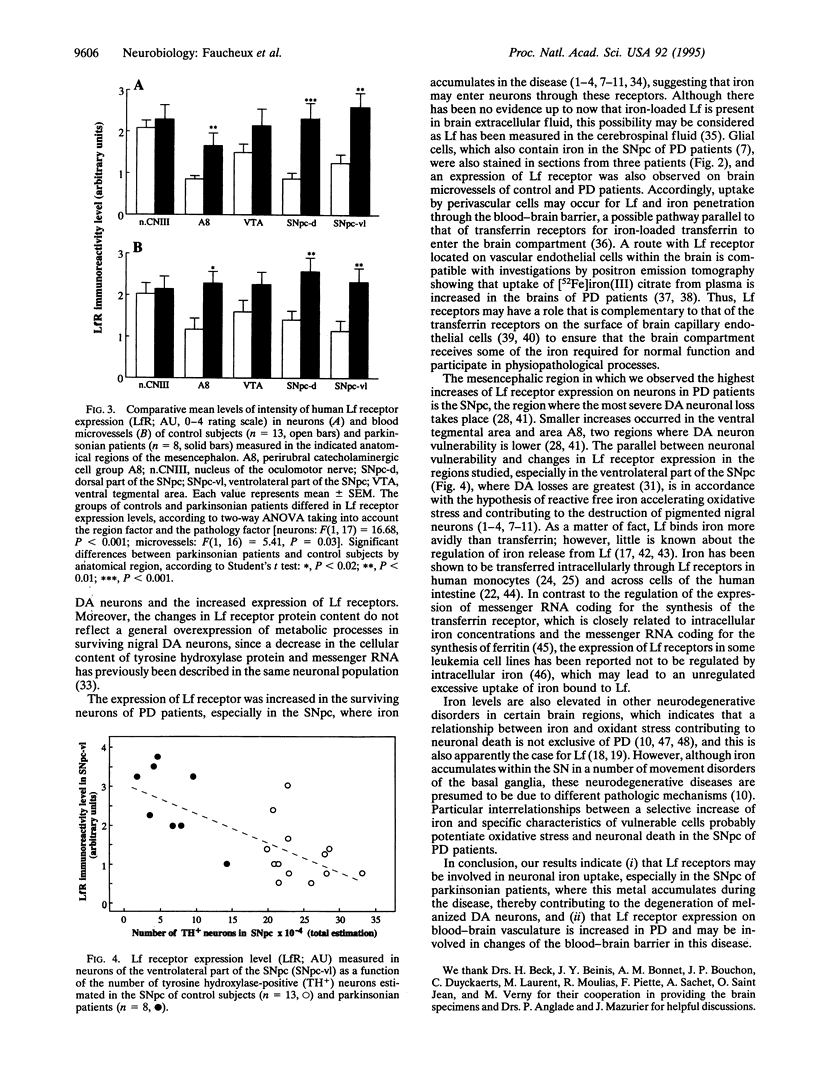
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agid Y., Ruberg M., Javoy-Agid F., Hirsch E., Raisman-Vozari R., Vyas S., Faucheux B., Michel P., Kastner A., Blanchard V. Are dopaminergic neurons selectively vulnerable to Parkinson's disease? Adv Neurol. 1993;60:148–164. [PubMed] [Google Scholar]
- Aisen P. Entry of iron into cells: a new role for the transferrin receptor in modulating iron release from transferrin. Ann Neurol. 1992;32 (Suppl):S62–S68. doi: 10.1002/ana.410320711. [DOI] [PubMed] [Google Scholar]
- Aisen P., Leibman A. Lactoferrin and transferrin: a comparative study. Biochim Biophys Acta. 1972 Feb 29;257(2):314–323. doi: 10.1016/0005-2795(72)90283-8. [DOI] [PubMed] [Google Scholar]
- Beard J. L., Connor J. R., Jones B. C. Iron in the brain. Nutr Rev. 1993 Jun;51(6):157–170. doi: 10.1111/j.1753-4887.1993.tb03096.x. [DOI] [PubMed] [Google Scholar]
- Bi B. Y., Leveugle B., Liu J. L., Collard A., Coppe P., Roche A. C., Nillesse N., Capron M., Spik G., Mazurier J. Immunolocalization of the lactotransferrin receptor on the human T lymphoblastic cell line Jurkat. Eur J Cell Biol. 1994 Oct;65(1):164–171. [PubMed] [Google Scholar]
- Birgens H. S., Kristensen L. O., Borregaard N., Karle H., Hansen N. E. Lactoferrin-mediated transfer of iron to intracellular ferritin in human monocytes. Eur J Haematol. 1988 Jul;41(1):52–57. doi: 10.1111/j.1600-0609.1988.tb00868.x. [DOI] [PubMed] [Google Scholar]
- Crowe A., Morgan E. H. Iron and transferrin uptake by brain and cerebrospinal fluid in the rat. Brain Res. 1992 Oct 2;592(1-2):8–16. doi: 10.1016/0006-8993(92)91652-u. [DOI] [PubMed] [Google Scholar]
- Dexter D. T., Carayon A., Javoy-Agid F., Agid Y., Wells F. R., Daniel S. E., Lees A. J., Jenner P., Marsden C. D. Alterations in the levels of iron, ferritin and other trace metals in Parkinson's disease and other neurodegenerative diseases affecting the basal ganglia. Brain. 1991 Aug;114(Pt 4):1953–1975. doi: 10.1093/brain/114.4.1953. [DOI] [PubMed] [Google Scholar]
- Fahn S., Cohen G. The oxidant stress hypothesis in Parkinson's disease: evidence supporting it. Ann Neurol. 1992 Dec;32(6):804–812. doi: 10.1002/ana.410320616. [DOI] [PubMed] [Google Scholar]
- Faucheux B. A., Herrero M. T., Villares J., Levy R., Javoy-Agid F., Obeso J. A., Hauw J. J., Agid Y., Hirsch E. C. Autoradiographic localization and density of [125I]ferrotransferrin binding sites in the basal ganglia of control subjects, patients with Parkinson's disease and MPTP-lesioned monkeys. Brain Res. 1995 Sep 11;691(1-2):115–124. doi: 10.1016/0006-8993(95)00629-5. [DOI] [PubMed] [Google Scholar]
- Faucheux B. A., Hirsch E. C., Villares J., Selimi F., Mouatt-Prigent A., Javoy-Agid F., Hauw J. J., Agid Y. Distribution of 125I-ferrotransferrin binding sites in the mesencephalon of control subjects and patients with Parkinson's disease. J Neurochem. 1993 Jun;60(6):2338–2341. doi: 10.1111/j.1471-4159.1993.tb03527.x. [DOI] [PubMed] [Google Scholar]
- Fearnley J. M., Lees A. J. Ageing and Parkinson's disease: substantia nigra regional selectivity. Brain. 1991 Oct;114(Pt 5):2283–2301. doi: 10.1093/brain/114.5.2283. [DOI] [PubMed] [Google Scholar]
- Gerlach M., Ben-Shachar D., Riederer P., Youdim M. B. Altered brain metabolism of iron as a cause of neurodegenerative diseases? J Neurochem. 1994 Sep;63(3):793–807. doi: 10.1046/j.1471-4159.1994.63030793.x. [DOI] [PubMed] [Google Scholar]
- Good P. F., Olanow C. W., Perl D. P. Neuromelanin-containing neurons of the substantia nigra accumulate iron and aluminum in Parkinson's disease: a LAMMA study. Brain Res. 1992 Oct 16;593(2):343–346. doi: 10.1016/0006-8993(92)91334-b. [DOI] [PubMed] [Google Scholar]
- HALLGREN B., SOURANDER P. The effect of age on the non-haemin iron in the human brain. J Neurochem. 1958 Oct;3(1):41–51. doi: 10.1111/j.1471-4159.1958.tb12607.x. [DOI] [PubMed] [Google Scholar]
- Halliwell B. Reactive oxygen species and the central nervous system. J Neurochem. 1992 Nov;59(5):1609–1623. doi: 10.1111/j.1471-4159.1992.tb10990.x. [DOI] [PubMed] [Google Scholar]
- Hill J. M., Switzer R. C., 3rd The regional distribution and cellular localization of iron in the rat brain. Neuroscience. 1984 Mar;11(3):595–603. doi: 10.1016/0306-4522(84)90046-0. [DOI] [PubMed] [Google Scholar]
- Hirsch E. C., Brandel J. P., Galle P., Javoy-Agid F., Agid Y. Iron and aluminum increase in the substantia nigra of patients with Parkinson's disease: an X-ray microanalysis. J Neurochem. 1991 Feb;56(2):446–451. doi: 10.1111/j.1471-4159.1991.tb08170.x. [DOI] [PubMed] [Google Scholar]
- Hirsch E., Graybiel A. M., Agid Y. A. Melanized dopaminergic neurons are differentially susceptible to degeneration in Parkinson's disease. Nature. 1988 Jul 28;334(6180):345–348. doi: 10.1038/334345a0. [DOI] [PubMed] [Google Scholar]
- Hoehn M. M., Yahr M. D. Parkinsonism: onset, progression and mortality. Neurology. 1967 May;17(5):427–442. doi: 10.1212/wnl.17.5.427. [DOI] [PubMed] [Google Scholar]
- Hu W. L., Mazurier J., Montreuil J., Spik G. Isolation and partial characterization of a lactotransferrin receptor from mouse intestinal brush border. Biochemistry. 1990 Jan 16;29(2):535–541. doi: 10.1021/bi00454a030. [DOI] [PubMed] [Google Scholar]
- Huebers H. A., Finch C. A. The physiology of transferrin and transferrin receptors. Physiol Rev. 1987 Apr;67(2):520–582. doi: 10.1152/physrev.1987.67.2.520. [DOI] [PubMed] [Google Scholar]
- Jefferies W. A., Brandon M. R., Hunt S. V., Williams A. F., Gatter K. C., Mason D. Y. Transferrin receptor on endothelium of brain capillaries. Nature. 1984 Nov 8;312(5990):162–163. doi: 10.1038/312162a0. [DOI] [PubMed] [Google Scholar]
- Jellinger K., Kienzl E., Rumpelmair G., Riederer P., Stachelberger H., Ben-Shachar D., Youdim M. B. Iron-melanin complex in substantia nigra of parkinsonian brains: an x-ray microanalysis. J Neurochem. 1992 Sep;59(3):1168–1171. doi: 10.1111/j.1471-4159.1992.tb08362.x. [DOI] [PubMed] [Google Scholar]
- Jellinger K., Paulus W., Grundke-Iqbal I., Riederer P., Youdim M. B. Brain iron and ferritin in Parkinson's and Alzheimer's diseases. J Neural Transm Park Dis Dement Sect. 1990;2(4):327–340. doi: 10.1007/BF02252926. [DOI] [PubMed] [Google Scholar]
- Jenner P. Oxidative damage in neurodegenerative disease. Lancet. 1994 Sep 17;344(8925):796–798. doi: 10.1016/s0140-6736(94)92347-7. [DOI] [PubMed] [Google Scholar]
- Kalaria R. N., Sromek S. M., Grahovac I., Harik S. I. Transferrin receptors of rat and human brain and cerebral microvessels and their status in Alzheimer's disease. Brain Res. 1992 Jul 10;585(1-2):87–93. doi: 10.1016/0006-8993(92)91193-i. [DOI] [PubMed] [Google Scholar]
- Kastner A., Hirsch E. C., Agid Y., Javoy-Agid F. Tyrosine hydroxylase protein and messenger RNA in the dopaminergic nigral neurons of patients with Parkinson's disease. Brain Res. 1993 Mar 26;606(2):341–345. doi: 10.1016/0006-8993(93)91005-d. [DOI] [PubMed] [Google Scholar]
- Kawamata T., Tooyama I., Yamada T., Walker D. G., McGeer P. L. Lactotransferrin immunocytochemistry in Alzheimer and normal human brain. Am J Pathol. 1993 May;142(5):1574–1585. [PMC free article] [PubMed] [Google Scholar]
- Klausner R. D., Rouault T. A., Harford J. B. Regulating the fate of mRNA: the control of cellular iron metabolism. Cell. 1993 Jan 15;72(1):19–28. doi: 10.1016/0092-8674(93)90046-s. [DOI] [PubMed] [Google Scholar]
- Leenders K. L., Antonini A., Schwarzbach R., Smith-Jones P., Reist H., Ben-Shachar D., Youdim M., Henn V. Blood to brain iron uptake in one rhesus monkey using [Fe-52]-citrate and positron emission tomography (PET): influence of haloperidol. J Neural Transm Suppl. 1994;43:123–132. [PubMed] [Google Scholar]
- Leveugle B., Mazurier J., Legrand D., Mazurier C., Montreuil J., Spik G. Lactotransferrin binding to its platelet receptor inhibits platelet aggregation. Eur J Biochem. 1993 May 1;213(3):1205–1211. doi: 10.1111/j.1432-1033.1993.tb17871.x. [DOI] [PubMed] [Google Scholar]
- Leveugle B., Spik G., Perl D. P., Bouras C., Fillit H. M., Hof P. R. The iron-binding protein lactotransferrin is present in pathologic lesions in a variety of neurodegenerative disorders: a comparative immunohistochemical analysis. Brain Res. 1994 Jul 4;650(1):20–31. doi: 10.1016/0006-8993(94)90202-x. [DOI] [PubMed] [Google Scholar]
- MONTREUIL J., TONNELAT J., MULLET S. [Preparation and properties of lactosiderophilin (lactotransferrin) of human milk]. Biochim Biophys Acta. 1960 Dec 18;45:413–421. doi: 10.1016/0006-3002(60)91478-5. [DOI] [PubMed] [Google Scholar]
- Mash D. C., Pablo J., Buck B. E., Sanchez-Ramos J., Weiner W. J. Distribution and number of transferrin receptors in Parkinson's disease and in MPTP-treated mice. Exp Neurol. 1991 Oct;114(1):73–81. doi: 10.1016/0014-4886(91)90086-r. [DOI] [PubMed] [Google Scholar]
- Mazurier J., Legrand D., Hu W. L., Montreuil J., Spik G. Expression of human lactotransferrin receptors in phytohemagglutinin-stimulated human peripheral blood lymphocytes. Isolation of the receptors by antiligand-affinity chromatography. Eur J Biochem. 1989 Feb 1;179(2):481–487. doi: 10.1111/j.1432-1033.1989.tb14578.x. [DOI] [PubMed] [Google Scholar]
- Mikogami T., Heyman M., Spik G., Desjeux J. F. Apical-to-basolateral transepithelial transport of human lactoferrin in the intestinal cell line HT-29cl.19A. Am J Physiol. 1994 Aug;267(2 Pt 1):G308–G315. doi: 10.1152/ajpgi.1994.267.2.G308. [DOI] [PubMed] [Google Scholar]
- Mikogami T., Marianne T., Spik G. Effect of intracellular iron depletion by picolinic acid on expression of the lactoferrin receptor in the human colon carcinoma cell subclone HT29-18-C1. Biochem J. 1995 Jun 1;308(Pt 2):391–397. doi: 10.1042/bj3080391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris C. M., Candy J. M., Omar S., Bloxham C. A., Edwardson J. A. Transferrin receptors in the parkinsonian midbrain. Neuropathol Appl Neurobiol. 1994 Oct;20(5):468–472. doi: 10.1111/j.1365-2990.1994.tb00997.x. [DOI] [PubMed] [Google Scholar]
- Riederer P., Dirr A., Goetz M., Sofic E., Jellinger K., Youdim M. B. Distribution of iron in different brain regions and subcellular compartments in Parkinson's disease. Ann Neurol. 1992;32 (Suppl):S101–S104. doi: 10.1002/ana.410320717. [DOI] [PubMed] [Google Scholar]
- Rochard E., Legrand D., Lecocq M., Hamelin R., Crepin M., Montreuil J., Spik G. Characterization of lactotransferrin receptor in epithelial cell lines from non-malignant human breast, benign mastopathies and breast carcinomas. Anticancer Res. 1992 Nov-Dec;12(6B):2047–2051. [PubMed] [Google Scholar]
- Sofic E., Paulus W., Jellinger K., Riederer P., Youdim M. B. Selective increase of iron in substantia nigra zona compacta of parkinsonian brains. J Neurochem. 1991 Mar;56(3):978–982. doi: 10.1111/j.1471-4159.1991.tb02017.x. [DOI] [PubMed] [Google Scholar]
- Terent A., Hällgren R., Venge P., Bergström K. Lactoferrin, lysozyme, and beta 2-microglobulin in cerebrospinal fluid. Elevated levels in patients with acute cerebrovascular lesions as indices of inflammation. Stroke. 1981 Jan-Feb;12(1):40–46. doi: 10.1161/01.str.12.1.40. [DOI] [PubMed] [Google Scholar]
- Yamada Y., Amagasaki T., Jacobsen D. W., Green R. Lactoferrin binding by leukemia cell lines. Blood. 1987 Jul;70(1):264–270. [PubMed] [Google Scholar]