Abstract
Importance
The Centers for Medicare and Medicaid Services (CMS) recently identified 30-day readmission after discharge from inpatient rehabilitation facilities as a national quality indicator. Research is needed to determine the rates and factors related to readmission in this patient population.
Objective
Determine 30-day readmission rates and factors related to readmission for patients receiving post-acute inpatient rehabilitation.
Design
Retrospective cohort study.
Setting
1,365 post-acute inpatient rehabilitation facilities providing services to Medicare fee-for service beneficiaries.
Participants
Records for 736,536 post-acute patients discharged from inpatient rehabilitation facilities to the community in 2006 through 2011. Mean age 78.0 (SD = 7.3) years. Sixty-three percent of patients were female and 85.1% were non-Hispanic white.
Main Outcome and Measures
30-day readmission rates for the six largest diagnostic impairment categories receiving inpatient rehabilitation. These included stroke, lower extremity fracture, lower extremity joint replacement, debility, neurological disorders and brain dysfunction.
Results
Mean rehabilitation length of stay was 12.4 (SD = 5.3) days. The overall 30-day readmission rate was 11.8% (95%CI, 11.7%, 11.8%). Rates ranged from 5.8% (95%CI, 5.8%, 5.9%) for patients with lower extremity joint replacement to 18.8% (95%CI, 18.8%, 18.9%). for patients with debility. Rates were highest in men (13.0%; 95%CI, 12.8%, 13.1%), non-Hispanic blacks, (13.8%; 95%CI, 13.5%, 14.1%), dual eligible beneficiaries (15.1%; 95%CI, 14.9%, 15.4%), and in patients with tier 1 comorbidities (25.6%; 95%CI, 24.9%, 26.3%). Higher motor and cognitive functional status were associated with lower hospital readmission rates across the six impairment categories. Variability in adjusted readmission rates by state ranged from 9.2% to 13.6%. Approximately 50% of patients who were rehospitalized within the 30-day period were readmitted within 11 days of discharge. MS-DRG codes for heart failure, urinary tract infection, pneumonia, septicemia, nutritional and metabolic disorders, esophagitis, gastroenteritis and digestive disorders were common reasons for readmission.
Conclusion and Relevance
Among post-acute rehabilitation facilities providing services to Medicare fee-for-service beneficiaries, 30-day readmission rates ranged from 5.8% to 18.8% for selected impairment groups. Further research is needed to understand the reasons for readmission.
INTRODUCTION
The Patient Protection and Affordable Care Act 1 created the hospital readmission reduction program to reduce readmissions and improve patient transitions from acute care. Research examining 30-day readmission has focused on patients discharged from acute care hospitals.2, 3 Patients discharged to post-acute care institutional settings have been excluded from previous research on hospital readmission.3, 4–6 Little research on hospital readmission has been reported for patients receiving post-acute services.
The Medicare Payment Advisory Commission (MedPAC)7 recently began tracking hospital readmission for post-acute care settings. In 2010, 12% of patients discharged from inpatient rehabilitation facilities to the community were readmitted to acute care hospitals within 30 days.7 The MedPAC report did not stratify these cases by impairment categories.7
It is important to study readmission after discharge from post-acute rehabilitation for three reasons. First, patients referred to post-acute rehabilitation are at high risk for readmission (e.g., stroke and hip fracture).4, 6 Second, the Centers for Medicare and Medicaid Services (CMS) recently identified 30-day readmission as a national quality indicator for inpatient rehabilitation facilities.8, 9 Reporting will be required in 2014 by CMS and is consistent with the Affordable Care Act.1, 8 Third, CMS has proposed bundled payment models (acute and post-acute care) to align performance incentives and contain costs.10, 11 Understanding the influence of bundling requires accurate information regarding readmission rates for patients receiving post-acute services.
We examined patients from the six largest impairment categories receiving post-acute inpatient rehabilitation. These include patients with stroke, lower extremity fracture, lower extremity joint replacement, debility, neurological disorders and brain dysfunction.4 We were interested in answering the following questions: What is the 30-day readmission rate following discharge from inpatient rehabilitation? Are there differences in readmission rates across impairment categories? Are readmissions associated with patient socio-demographics, clinical characteristics, functional status or facility factors?
METHODS
Source of Data
Data analyzed were from CMS files: 1) Medicare Provider Analysis and Review (MedPAR); 2) Inpatient Rehabilitation Facility–Patient Assessment Instrument (IRF-PAI); 3) Beneficiary Summary file; and 4) Inpatient Rehabilitation Facility Rate Settings.
Obtaining CMS Files
Stay-level Medicare data in the Research Identifiable Format were acquired for 2006 through 2011. The study was approved by the University of Texas Medical Branch Institutional Review Board. Use of Medicare data files was reviewed by CMS and met all federal privacy and confidentiality requirements. A Data Use Agreement was completed following CMS guidelines.
Facilities
Rehabilitation facilities are divided into hospital-based units or freestanding centers.12 Sixty-two percent of inpatient rehabilitation beds in 2010 were in hospital-based units.7
Study Population
Our population was Medicare fee-for-service patients discharged directly from short-term acute care hospitals to inpatient rehabilitation facilities. The patients’ rehabilitation admission diagnosis placed them in one of the six rehabilitation impairment categories described previously. Ninety-five percent of all patients admitted to inpatient rehabilitation facilities during the study period were from acute care hospitals.7 We selected the six impairment categories based on the 2013 MedPAC report4 indicating that approximately 75% of Medicare fee-for-service patients receiving in inpatient rehabilitation were included in these impairment groups.
Variables
Hospital Readmission
We examined readmission to an acute care hospital that occurred within 30-days following discharge from the rehabilitation facility to the community. In the Medicare rehabilitation inpatient data, community includes home, board and care, transitional living, and assisted living residence.13 Descriptions of the rehabilitation impairment categories, number of patients in each category, and the ICD-9-CM diagnostic codes associated with the categories are included on-line in Appendix 1.
Socio-demographics
Age at rehabilitation admission (continuous and categories: ≤74; 75–84; ≥85 years), gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic and other), married (yes/no), pre-hospital living status (living alone vs. with family/relatives, friends, attendant, or others), disability (receiving disability benefits yes/no), and Medicaid dual eligibility (yes/no). These variables were extracted from the rehabilitation assessment data (IRF-PAI) and Beneficiary Summary files.
Case-Mix Group (CMG)
Case-mix groups are used to determine Medicare fee-for-service payment for individual patient stays.12 Rehabilitation patients are classified into a case-mix group at the time of admission based on impairment category, motor and cognitive functional status (see below) and age. Each impairment category has a set number of case-mix groups (e.g., stroke has 10). Each case-mix group and comorbidity tier (described below) is associated with a projected length of stay and base-level reimbursement provided to the facility.14 Medicare reimbursement rates are also adjusted by several factors (e.g., rural versus urban location).
Comorbidity Tier
CMS developed three tiers for inpatient rehabilitation reimbursement - Tier 1 (high reimbursement) to tier 3 (low reimbursement).15 In 2012, there were eight comorbid conditions in Tier 1, 11 in Tier 2, and 924 in Tier 3. An example of a Tier 1 comorbidity is renal dialysis.4 Some forms of diabetes are classified as Tier 3 comorbidities. Each case mix-group is paired with the patient’s comorbidity tier status (Tier 1, 2, 3 or no tier level comorbidity) and assigned a weight that reflects the resources required to provide treatment to the average patient with that clinical presentation. Patients are assigned to the tier with the highest level of reimbursement.
Functional Status
Functional status items are included in the Medicare rehabilitation assessment data (IRF-PAI). The 18 items cover six domains; self-care, sphincter control, transfers, locomotion, communication, and social cognition.16 Items are assigned to one of seven levels of function ranging from complete dependence (level 1) to independence (level 7). A rating of zero is recorded if an activity does not occur and is used only at admission. Functional status ratings can be divided into motor and cognitive subscales. The functional status items are administered to the patient upon admission and within 36 hours of discharge. Motor function ratings range from 13 to 91. Cognitive function ratings range from 5 to 35. The reliability and validity of the ratings have been widely studied and found to be psychometrically adequate.17, 18 The admission motor and cognitive ratings are used to determine patient CMG assignment.12, 19
Clinical Variable
Length of stay (LOS) in days (continuous)
Facility Factors
Type of facility (hospital-based unit vs. free-standing); location (urban or rural); teaching facility (yes/no); ownership (government, not-for-profit, and for profit); and location by state.
Reason for Readmission
Readmissions were categorized using Medicare Severity Diagnostic Related Groups (MS-DRGs). MS-DRGs classify the reason for a hospitalization based on a series of principal and secondary diagnoses as well as procedure codes.20 MS-DRGs incorporate the severity of the patient’s condition with codes that mark the presence of complications and comorbidities.20 We identified the top 25 MS-DRG Codes at readmission for each of the impairment categories using the acute care claims associated with readmit status.
Data Analysis
Summary statistics (means and standard deviations and/or column percentages) of patient characteristics were calculated for each rehabilitation impairment category and for the combined sample. Thirty-day readmission rates and 95% confidence intervals were computed for each category of the patient- and facility-level variables. We used the normal approximation method for binomial confidence intervals.21
The top 25 reasons for readmission, based on Medicare Severity - Diagnosis Related Groups (MS-DRGs), were identified within each rehabilitation impairment category by frequency analyses.
State-specific risk-standardized readmission rates were calculated using hierarchical generalized linear mixed models to account for clustering of patients within states. The models adjusted for eight patient demographic and clinical variables: age, sex, race/ethnicity, living situation, rehabilitation impairment category, tier comorbidities, and admission motor and cognitive functioning. The final rates were obtained by taking the ratio of predicted to expected readmissions for each state and multiplying by the global unadjusted rate.22 Data were analyzed using SPSS 21 and SAS 9.3.
RESULTS
Patients receiving rehabilitation from January 2006 through November 2011 in one of the six impairment categories with complete Medicare records for 30-days after discharge were the eligible sample (N = 1,705,109). We excluded patients with an atypical rehabilitation stay (length of stay >30 days) (n = 26,750), patients admitted to inpatient rehabilitation facilities from settings other than acute hospitals (n = 68,319), patients living in non-community settings prior to their admission (n = 22,559), and those who died during the rehabilitation stay (n = 3,005). Also excluded were patients with rehabilitation stay other than ‘initial rehabilitation’ (n = 46,058) and those with rehabilitation program interruptions (n = 14,471). Our sample included beneficiaries in Medicare’s traditional fee-for-service plan age 65 and above, including those eligible for disability and those who had dual (Medicare and Medicaid) eligibility. We selected only those patients discharged to community settings after rehabilitation stay and excluded persons transferred on the day of discharge to acute care, long-term care hospitals, or nursing homes (n = 293,211). After compiling data for six years, we considered only the first rehabilitation stay and those who survived 30 days after rehabilitation stay. The final cohort included 736,536 patients from 1,365 rehabilitation facilities, with ICD-9 CM codes that placed them in one of the six rehabilitation impairment categories.
The mean age was 78.0 (SD = 7.3) years. The majority of patients were female (62.5%), with 85.1% non-Hispanic white. Forty-eight percent were married and 65.7% were living with someone prior to their acute care hospitalization. Sixty-four percent received rehabilitation services in hospital based rehabilitation units and 27.9% had at least one CMS rehabilitation tier comorbidity. The mean rehabilitation length of stay was 12.4 (SD = 5.3) days.
Lower extremity joint replacement was the largest rehabilitation impairment category of patients discharged to the community, representing 25% of our cohort. They were followed by patients with lower extremity fracture (23%), stroke (21%), debility (12%), neurological conditions (10%) and brain dysfunction (9%) (Table 1).
Table 1.
Sample characteristics for each rehabilitation impairment category - values as mean (sd) or column %.
| Stroke | Brain dysfunction | Neurologic conditions | Fracture | Joint replace | Debility | Total | |
|---|---|---|---|---|---|---|---|
| Total | 155,476 | 62,974 | 73,740 | 169,426 | 184,282 | 90,638 | 736,536 |
| Readmitted | 12.7% | 16.4% | 17.4% | 9.4% | 5.8% | 18.8% | 11.8% |
| 1–10 days | 5.4% | 7.4% | 7.9% | 4.1% | 2.8% | 8.7% | 5.3% |
| 11–20 days | 4.1% | 5.2% | 5.5% | 3.0% | 1.8% | 5.9% | 3.7% |
| 21–30 days | 3.2% | 3.9% | 4.0% | 2.3% | 1.3% | 4.2% | 2.8% |
| Year | |||||||
| 2006 | 19.1% | 16.0% | 15.5% | 19.4% | 25.6% | 13.3% | 19.5% |
| 2007 | 17.6% | 16.0% | 15.3% | 18.0% | 19.2% | 15.0% | 17.4% |
| 2008 | 16.2% | 16.1% | 15.0% | 16.8% | 16.0% | 17.0% | 16.3% |
| 2009 | 16.4% | 17.2% | 16.8% | 16.1% | 14.1% | 17.3% | 16.0% |
| 2010 | 16.0% | 17.3% | 18.3% | 15.4% | 13.4% | 18.6% | 15.9% |
| 2011 | 14.7% | 17.3% | 19.1% | 14.3% | 11.7% | 18.8% | 15.0% |
| Age | 77.7 (7.4) | 77.8 (7.3) | 77.7 (7.1) | 80.2 (7.3) | 75.8 (6.5) | 79.6 (7.3) | 78.0 (7.3) |
| < 75 yrs | 36.4% | 35.6% | 35.4% | 23.9% | 45.6% | 26.7% | 34.4% |
| 75–84 yrs | 43.6% | 44.8% | 45.9% | 45.8% | 42.8% | 45.8% | 44.5% |
| 85+ yrs | 20.0% | 19.6% | 18.7% | 30.3% | 11.6% | 27.6% | 21.1% |
| Female | 54.7% | 49.6% | 53.2% | 73.6% | 68.8% | 58.4% | 62.5% |
| Race/ethnicity | |||||||
| White | 78.1% | 84.0% | 85.4% | 89.5% | 86.9% | 85.6% | 85.1% |
| Black | 12.8% | 7.2% | 7.8% | 3.6% | 6.9% | 8.7% | 7.7% |
| Hispanic | 5.7% | 5.2% | 4.7% | 4.6% | 4.2% | 3.8% | 4.7% |
| Other/unknown | 3.5% | 3.6% | 2.1% | 2.4% | 2.0% | 2.0% | 2.5% |
| Married | 50.1% | 54.5% | 50.1% | 43.2% | 51.6% | 43.0% | 48.4% |
| Prior living situation* | |||||||
| With others | 69.7% | 70.9% | 67.8% | 62.6% | 64.5% | 62.3% | 65.7% |
| Alone | 27.6% | 25.7% | 28.4% | 33.7% | 34.5% | 33.5% | 31.3% |
| Unspecified | 2.7% | 3.5% | 3.9% | 3.8% | 1.1% | 4.2% | 2.9% |
| Disability+ | 10.9% | 10.2% | 14.3% | 8.3% | 9.2% | 12.0% | 10.3% |
| Dual eligibility◃ | 18.7% | 14.0% | 15.8% | 13.9% | 10.3% | 15.7% | 14.4% |
| Tier comorbidity□ | |||||||
| No tier | 79.4% | 56.5% | 57.8% | 79.4% | 79.1% | 54.1% | 72.1% |
| Tier 3 | 18.0% | 25.9% | 26.2% | 15.0% | 18.9% | 31.4% | 20.7% |
| Tier 2 | 1.2% | 14.9% | 12.3% | 4.2% | 1.7% | 10.0% | 5.4% |
| Tier 1 | 1.4% | 2.7% | 3.7% | 1.4% | .3% | 4.5% | 1.8% |
| Rehabilitation length of stay | 14.6 (6.4) | 13.2 (5.5) | 12.8 (4.9) | 13.3 (4.5) | 9.4 (3.6) | 11.8 (4.7) | 12.4 (5.3) |
| <10 | 24.7% | 28.3% | 27.1% | 21.6% | 56.3% | 34.4% | 33.6% |
| 10–14 | 29.8% | 35.6% | 39.6% | 39.8% | 36.0% | 40.4% | 36.4% |
| 15+ | 45.5% | 36.0% | 33.4% | 38.6% | 7.8% | 25.2% | 30.0% |
| Cognitive function: admit⋄ | 21.5 (7.1) | 20.3 (7.0) | 24.0 (6.5) | 25.7 (6.5) | 29.0 (5.2) | 24.9 (6.4) | 24.9 (7.0) |
| <23 | 51.6% | 59.3% | 36.6% | 27.1% | 10.9% | 31.5% | 32.5% |
| 23–28 | 30.9% | 28.1% | 36.4% | 34.1% | 27.6% | 36.6% | 31.8% |
| 29+ | 17.5% | 12.6% | 27.1% | 38.8% | 61.4% | 31.9% | 35.7% |
| Motor function: admit⋄ | 39.7 (12.5) | 39.6 (12.1) | 38.7 (11.2) | 37.4 (9.7) | 44.1 (9.0) | 40.9 (10.8) | 40.3 (11.0) |
| <36 | 36.8% | 36.8% | 38.8% | 42.2% | 17.6% | 31.2% | 32.7% |
| 36–45 | 27.5% | 28.9% | 31.5% | 36.2% | 36.0% | 32.8% | 32.8% |
| 46+ | 35.6% | 34.3% | 29.7% | 21.6% | 46.4% | 36.1% | 34.5% |
| Cognitive function: discharge | 26.1 (6.2) | 25.4 (6.0) | 28.2 (5.4) | 29.3 (5.2) | 32.0 (3.4) | 28.6 (5.2) | 28.8 (5.6) |
| <29 | 58.8% | 65.3% | 44.1% | 34.1% | 12.8% | 40.2% | 38.4% |
| 29–32 | 27.1% | 24.2% | 32.9% | 34.6% | 32.3% | 34.9% | 31.4% |
| 33+ | 14.2% | 10.6% | 23.0% | 31.4% | 54.9% | 24.9% | 30.2% |
| Motor function: discharge | 63.1 (13.8) | 63.6 (12.8) | 63.5 (12.9) | 63.9 (11.3) | 71.1 (8.2) | 64.9 (12.2) | 65.6 (12.1) |
| <63 | 41.8% | 40.7% | 40.9% | 39.0% | 14.1% | 36.8% | 33.4% |
| 63–72 | 31.6% | 33.9% | 31.8% | 36.5% | 34.0% | 33.1% | 33.7% |
| 73+ | 26.6% | 25.4% | 27.3% | 24.5% | 51.8% | 30.2% | 32.9% |
| Cognitive function: gain | 4.6 (4.4) | 5.1 (5.0) | 4.2 (4.6) | 3.6 (4.4) | 3.0 (4.0) | 3.8 (4.4) | 3.9 (4.4) |
| <2 | 26.4% | 25.3% | 32.7% | 38.5% | 46.0% | 36.7% | 35.9% |
| 2–5 | 37.4% | 34.3% | 34.7% | 34.4% | 33.5% | 34.6% | 34.8% |
| 6+ | 36.3% | 40.4% | 32.5% | 27.1% | 20.5% | 28.7% | 29.3% |
| Motor function: gain | 23.4 (10.6) | 24.0 (11.3) | 24.7 (11.0) | 26.4 (10.0) | 27.0 (9.3) | 24.0 (10.6) | 25.3 (10.4) |
| <21 | 39.9% | 39.1% | 35.4% | 27.3% | 23.9% | 37.4% | 32.1% |
| 21–29 | 33.2% | 31.1% | 32.5% | 35.1% | 37.8% | 33.6% | 34.6% |
| 30+ | 26.9% | 29.8% | 32.2% | 37.6% | 38.4% | 29.0% | 33.3% |
| Freestanding‡ | 27.1% | 33.4% | 45.1% | 33.6% | 38.3% | 43.2% | 35.7% |
| Ownership | |||||||
| Non-profit | 63.3% | 59.8% | 52.2% | 55.3% | 58.3% | 52.2% | 57.4% |
| For profit | 30.2% | 34.8% | 44.0% | 37.5% | 36.2% | 42.2% | 36.6% |
| Government | 5.5% | 4.5% | 3.0% | 6.1% | 4.7% | 4.7% | 5.0% |
| Rural△ | 10.2% | 5.8% | 8.0% | 12.3% | 10.8% | 9.4% | 10.1% |
Prior living setting categories are defined and recorded in the Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI).14
Disability based on persons meeting Social Security Disability criteria and receiving benefits for two years.
Dual eligibility refers to Medicare beneficiaries who qualify for both Medicare and Medicaid.
Tier comorbidity = Medicare tier level comorbidities developed for post-acute inpatient medical rehabilitation and recorded in the IRF-PAI.14
Cognitive and motor function are based on items from the IRF-PAI. The range of scores for motor items is 13–91; the range of scores for cognitive items is 5–35. Higher scores indicate better performance. 17 Admission includes rating within 36 hours of admission. Discharge includes ratings within 36 hours of discharge. Gain is the difference between admission and discharge ratings.14, 17
Freestanding refers to facilities that are independent rehabilitation hospitals rather than units located within acute care hospitals. This information is defined and recorded in the IRF-PAI.14
Rural (versus urban) is designated for reimbursement purposes under the IRF prospective payment system.
Note: missing values ranged from 1.1–1.5% for marital status, 0.0–4.4% for dual eligibility, 0.5–0.9% for facility type (freestanding/unit), 0.8–1.0% for ownership, and 0.5–0.9% for facility location (rural/urban).
The gradual increase in percent of patients readmitted over time in the total sample (Table 2, last column) is a consequence of changes in the relative contributions of certain rehabilitation impairment groups to the combined sample. Joint replacement, which has the lowest readmission rates, showed the largest decrease in sample size over the six-year study period from approximately 33% of the total sample in 2006 to 20% in 2011. Conversely, debility, which has the highest readmission rate, demonstrated the largest increase in sample size from 8% of the total sample in 2006 to 15% in 2011. Examination of the readmission rates by individual impairment categories indicates they have remained relatively stable during the six-year study period. Based on these stable rates within impairment categories, the analyses reported below are aggregated across the six-year period.
Table 2.
Percentages (95% confidence intervals) of patients rehospitalized within 30 days of discharge by sample characteristics for each rehabilitation impairment.
| Stroke | Brain dysfunction | Neurologic conditions | Fracture | Joint replace | Debility | Total | |
|---|---|---|---|---|---|---|---|
| Overall | 12.7 (12.6, 12.8) | 16.4 (16.3, 16.5) | 17.4 (17.3, 17.5) | 9.4 (9.4, 9.5) | 5.8 (5.8, 5.9) | 18.8 (18.8, 18.9) | 11.8 (11.7, 11.8) |
| Year | |||||||
| 2006 | 12.7 (12.5, 12.9) | 16.9 (16.7, 17.0) | 17.5 (17.3, 17.7) | 9.6 (9.5, 9.8) | 5.8 (5.7, 5.9) | 19.3 (19.1, 19.5) | 10.9 (10.8, 11.1) |
| 2007 | 13.1 (12.9, 13.3) | 16.7 (16.5, 16.9) | 16.7 (16.5, 16.9) | 9.3 (9.2, 9.5) | 5.7 (5.6, 5.9) | 18.8 (18.6, 19.1) | 11.4 (11.2, 11.6) |
| 2008 | 12.8 (12.6, 13.0) | 16.4 (16.2, 16.6) | 17.3 (17.1, 17.5) | 9.6 (9.4, 9.7) | 5.9 (5.8, 6.0) | 19.1 (18.9, 19.3) | 11.9 (11.7, 12.1) |
| 2009 | 12.5 (12.3, 12.6) | 16.9 (16.7, 17.1) | 17.7 (17.5, 17.9) | 9.6 (9.4, 9.8) | 5.8 (5.6, 5.9) | 18.7 (18.4, 18.9) | 12.1 (11.9, 12.3) |
| 2010 | 12.6 (12.4, 12.8) | 16.1 (15.9, 16.3) | 17.5 (17.3, 17.7) | 9.2 (9.0, 9.4) | 6.2 (6.0, 6.3) | 18.8 (18.6, 19.0) | 12.3 (12.1, 12.5) |
| 2011 | 12.3 (12.1, 12.5) | 15.8 (15.6, 16.0) | 17.5 (17.3, 17.7) | 9.1 (8.9, 9.3) | 5.7 (5.6, 5.8) | 18.5 (18.3, 18.7) | 12.3 (12.1, 12.5) |
| Age | |||||||
| < 75 yrs | 12.0 (11.9, 12.1) | 16.9 (16.8, 17.0) | 16.8 (16.7, 16.9) | 8.7 (8.6, 8.8) | 5.1 (5.1, 5.2) | 20.6 (20.4, 20.8) | 11.0 (10.8, 11.1) |
| 75–84 yrs | 12.8 (12.7, 12.9) | 16.3 (16.2, 16.4) | 17.5 (17.4, 17.7) | 9.2 (9.1, 9.3) | 6.2 (6.1, 6.3) | 18.7 (18.6, 18.9) | 11.9 (11.8, 12.0) |
| 85+ yrs | 13.7 (13.5, 13.9) | 15.9 (15.7, 16.0) | 18.1 (17.9, 18.3) | 10.3 (10.1, 10.4) | 7.2 (7.1, 7.3) | 17.3 (17.2, 17.5) | 12.8 (12.7, 13.0) |
| Sex | |||||||
| Male | 12.2 (12.1, 12.4) | 17.1 (17.0, 17.2) | 17.5 (17.3, 17.6) | 10.7 (10.6, 10.8) | 6.2 (6.1, 6.3) | 19.7 (19.5, 19.8) | 13.0 (12.8, 13.1) |
| Female | 13.1 (13.0, 13.2) | 15.8 (15.6, 15.9) | 17.3 (17.2, 17.4) | 9.0 (8.9, 9.1) | 5.6 (5.6, 5.7) | 18.2 (18.1, 18.3) | 11.0 (11.0, 11.1) |
| Race/ethnicity | |||||||
| White | 12.3 (12.3, 12.4) | 16.1 (16.0, 16.2) | 17.2 (17.1, 17.3) | 9.4 (9.3, 9.4) | 5.9 (5.8, 5.9) | 18.6 (18.5, 18.7) | 11.5 (11.5, 11.6) |
| Black | 14.4 (14.1, 14.7) | 19.1 (18.8, 19.5) | 19.7 (19.4, 20.0) | 10.2 (10.0, 10.4) | 6.0 (5.8, 6.2) | 20.4 (20.0, 20.7) | 13.8 (13.5, 14.1) |
| Hispanic | 13.8 (13.5, 14.2) | 17.3 (16.9, 17.7) | 17.3 (16.9, 17.7) | 10.2 (9.9, 10.5) | 5.6 (5.4, 5.9) | 20.0 (19.6, 20.5) | 12.5 (12.1, 12.8) |
| Other/unknown | 12.4 (11.9, 12.8) | 16.9 (16.4, 17.5) | 17.3 (16.7, 17.8) | 9.2 (8.8, 9.6) | 4.9 (4.6, 5.2) | 19.9 (19.4, 20.5) | 11.9 (11.4, 12.4) |
| Marital status | |||||||
| Not married | 13.4 (13.2, 13.6) | 16.4 (15.9, 16.8) | 18.1 (17.7, 18.5) | 9.8 (9.6, 10.0) | 6.0 (5.9, 6.2) | 18.4 (18.0, 18.7) | 12.1 (12.0, 12.2) |
| Married | 12.0 (11.7, 12.2) | 16.5 (16.1, 16.9) | 16.8 (16.4, 17.1) | 9.0 (8.8, 9.2) | 5.6 (5.5, 5.8) | 19.5 (19.1, 19.9) | 11.4 (11.3, 11.5) |
| Missing | 13.8 (12.4, 15.2) | 17.3 (14.7, 19.8) | 15.3 (13.0, 17.7) | 9.0 (7.8, 10.3) | 5.6 (4.7, 6.6) | 18.6 (16.3, 20.9) | 11.9 (11.3, 12.6) |
| Prior living situation* | |||||||
| With others | 12.7 (12.6, 12.8) | 16.9 (16.8, 17.0) | 17.6 (17.5, 17.7) | 9.6 (9.5, 9.7) | 5.9 (5.8, 6.0) | 19.7 (19.6, 19.8) | 12.1 (12.0, 12.2) |
| Alone | 12.3 (12.2, 12.5) | 15.2 (15.0, 15.3) | 16.5 (16.4, 16.7) | 8.8 (8.7, 8.9) | 5.6 (5.5, 5.7) | 17.2 (17.1, 17.4) | 10.8 (10.7, 11.0) |
| Unspecified | 15.4 (14.9, 15.9) | 16.4 (15.9, 16.9) | 19.4 (18.9, 19.9) | 12.6 (12.1, 13.0) | 8.6 (8.2, 9.0) | 18.7 (18.2, 19.2) | 15.1 (14.7, 15.6) |
| Disability+ | |||||||
| No | 12.4 (12.3, 12.5) | 16.1 (16.1, 16.2) | 17.1 (17.0, 17.1) | 9.2 (9.1, 9.3) | 5.6 (5.6, 5.7) | 18.4 (18.3, 18.5) | 11.4 (11.3, 11.5) |
| Yes | 15.1 (14.8, 15.3) | 19.0 (18.7, 19.3) | 19.2 (19.0, 19.5) | 11.8 (11.6, 12.0) | 7.9 (7.7, 8.1) | 22.1 (21.8, 22.4) | 14.8 (14.5, 15.0) |
| Dual eligibility◃ | |||||||
| No | 12.0 (11.8, 12.2) | 15.9 (15.6, 16.2) | 16.6 (16.3, 16.9) | 9.0 (8.8, 9.1) | 5.6 (5.5, 5.7) | 18.2 (17.9, 18.5) | 11.1 (11.0, 11.2) |
| Yes | 15.8 (15.4, 16.2) | 19.4 (18.6, 20.2) | 21.0 (20.3, 21.8) | 12.0 (11.6, 12.4) | 7.4 (7.0, 7.8) | 21.8 (21.1, 22.5) | 15.1 (14.9, 15.3) |
| Missing | 3.2 (−3.0, 9.4) | 18.4 (16.6, 20.3) | 20.9 (19.0, 22.8) | 11.3 (9.1, 13.5) | 11.6 (9.9, 13.2) | 19.7 (18.4, 20.9) | 17.7 (16.9, 18.4) |
| Tier comorbidity□ | |||||||
| No tier | 11.7 (11.6, 11.7) | 14.5 (14.4, 14.6) | 14.8 (14.7, 14.9) | 8.3 (8.3, 8.4) | 5.2 (5.2, 5.3) | 16.4 (16.3, 16.5) | 9.9 (9.9, 10.0) |
| Tier 3 | 15.7 (15.5, 15.8) | 18.6 (18.4, 18.8) | 20.0 (19.8, 20.2) | 12.7 (12.5, 12.8) | 7.7 (7.5, 7.8) | 20.3 (20.1, 20.5) | 15.1 (14.9, 15.3) |
| Tier 2 | 21.1 (20.7, 21.5) | 18.4 (18.1, 18.8) | 20.5 (20.1, 20.9) | 14.8 (14.5, 15.2) | 11.2 (10.9, 11.5) | 23.2 (22.8, 23.6) | 18.9 (18.5, 19.3) |
| Tier 1 | 25.9 (25.2, 26.6) | 24.6 (23.9, 25.3) | 28.8 (28.1, 29.6) | 20.4 (19.7, 21.0) | 15.2 (14.6, 15.8) | 28.0 (27.3, 28.8) | 25.6 (24.9, 26.3) |
| Length of stay | |||||||
| <10 | 11.1 (10.9, 11.2) | 15.1 (14.9, 15.2) | 15.4 (15.3, 15.6) | 7.1 (7.0, 7.2) | 4.9 (4.8, 5.0) | 16.6 (16.5, 16.8) | 9.2 (9.1, 9.3) |
| 10–14 | 12.5 (12.3, 12.6) | 16.4 (16.2, 16.5) | 17.0 (16.8, 17.1) | 8.7 (8.6, 8.8) | 6.5 (6.4, 6.6) | 18.8 (18.7, 19.0) | 11.7 (11.6, 11.9) |
| 15+ | 13.7 (13.6, 13.9) | 17.6 (17.4, 17.7) | 19.4 (19.3, 19.6) | 11.4 (11.3, 11.6) | 9.8 (9.6, 9.9) | 21.9 (21.7, 22.1) | 14.7 (14.5, 14.8) |
| Cognitive function: adm⋄ | |||||||
| <23 | 14.2 (14.0, 14.3) | 17.0 (16.9, 17.2) | 18.2 (18.0, 18.3) | 11.9 (11.7, 12.0) | 8.0 (7.9, 8.1) | 19.7 (19.5, 19.8) | 14.8 (14.6, 14.9) |
| 23–28 | 11.6 (11.4, 11.7) | 15.4 (15.3, 15.6) | 17.7 (17.6, 17.9) | 9.4 (9.3, 9.6) | 6.5 (6.4, 6.6) | 18.9 (18.7, 19.1) | 12.0 (11.8, 12.1) |
| 29+ | 10.3 (10.2, 10.5) | 15.9 (15.8, 16.1) | 15.8 (15.7, 16.0) | 7.7 (7.6, 7.8) | 5.1 (5.0, 5.2) | 18.0 (17.8, 18.1) | 8.9 (8.7, 9.0) |
| Motor function: admit⋄ | |||||||
| <36 | 15.1 (15.0, 15.2) | 18.4 (18.3, 18.6) | 19.0 (18.8, 19.1) | 11.4 (11.3, 11.5) | 8.0 (7.9, 8.1) | 21.0 (20.9, 21.2) | 14.5 (14.4, 14.7) |
| 36–45 | 12.3 (12.2, 12.4) | 16.6 (16.4, 16.7) | 17.3 (17.2, 17.5) | 8.7 (8.6, 8.8) | 6.1 (6.0, 6.2) | 19.1 (18.9, 19.2) | 11.3 (11.2, 11.5) |
| 46+ | 10.5 (10.4, 10.6) | 14.2 (14.0, 14.3) | 15.3 (15.2, 15.5) | 6.7 (6.6, 6.8) | 4.8 (4.7, 4.9) | 16.7 (16.6, 16.9) | 9.6 (9.4, 9.7) |
| Cognitive function: DC | |||||||
| <29 | 14.4 (14.3, 14.5) | 17.2 (17.1, 17.4) | 18.9 (18.8, 19.1) | 12.1 (12.0, 12.3) | 8.8 (8.7, 8.9) | 20.3 (20.1, 20.4) | 15.2 (15.0, 15.3) |
| 29–32 | 10.6 (10.5, 10.8) | 15.1 (15.0, 15.3) | 17.1 (16.9, 17.2) | 9.0 (8.9, 9.1) | 6.3 (6.2, 6.4) | 18.4 (18.2, 18.5) | 11.1 (11.0, 11.3) |
| 33+ | 9.5 (9.4, 9.7) | 14.4 (14.3, 14.6) | 14.8 (14.7, 15.0) | 6.9 (6.8, 7.0) | 4.9 (4.8, 4.9) | 17.2 (17.0, 17.4) | 8.1 (8.0, 8.2) |
| Motor function: DC | |||||||
| <63 | 16.1 (16.0, 16.3) | 20.7 (20.5, 20.8) | 20.7 (20.6, 20.9) | 12.8 (12.6, 12.9) | 9.8 (9.7, 9.9) | 23.1 (22.9, 23.3) | 16.5 (16.4, 16.7) |
| 63–72 | 11.2 (11.0, 11.3) | 14.5 (14.4, 14.7) | 16.6 (16.5, 16.8) | 8.2 (8.1, 8.3) | 6.3 (6.2, 6.4) | 18.0 (17.8, 18.1) | 10.8 (10.7, 10.9) |
| 73+ | 9.1 (9.0, 9.2) | 12.2 (12.1, 12.4) | 13.2 (13.1, 13.3) | 6.0 (5.9, 6.1) | 4.4 (4.4, 4.5) | 14.6 (14.5, 14.8) | 7.9 (7.8, 8.0) |
| Cognitive function: gain | |||||||
| <2 | 13.6 (13.5, 13.8) | 18.3 (18.2, 18.5) | 17.8 (17.7, 18.0) | 9.5 (9.4, 9.6) | 5.6 (5.5, 5.7) | 19.3 (19.1, 19.4) | 11.4 (11.3, 11.5) |
| 2–5 | 12.5 (12.3, 12.6) | 16.5 (16.4, 16.7) | 17.5 (17.3, 17.6) | 9.2 (9.1, 9.3) | 5.9 (5.8, 6.0) | 19.0 (18.8, 19.1) | 11.8 (11.7, 11.9) |
| 6+ | 12.2 (12.1, 12.4) | 15.2 (15.0, 15.3) | 16.8 (16.6, 16.9) | 9.6 (9.5, 9.8) | 6.3 (6.2, 6.4) | 18.1 (18.0, 18.3) | 12.2 (12.1, 12.3) |
| Motor function: gain | |||||||
| <21 | 14.9 (14.7, 15.0) | 19.1 (18.9, 19.3) | 19.8 (19.7, 20.0) | 11.8 (11.7, 11.9) | 6.8 (6.7, 6.9) | 21.3 (21.2, 21.5) | 14.7 (14.5, 14.8) |
| 21–29 | 11.8 (11.7, 11.9) | 15.5 (15.4, 15.6) | 16.8 (16.7, 17.0) | 9.0 (8.9, 9.1) | 5.5 (5.4, 5.6) | 18.1 (17.9, 18.2) | 10.9 (10.8, 11.1) |
| 30+ | 10.6 (10.5, 10.7) | 13.9 (13.8, 14.0) | 15.2 (15.1, 15.4) | 8.1 (8.0, 8.2) | 5.5 (5.4, 5.6) | 16.5 (16.4, 16.7) | 9.8 (9.7, 9.9) |
| Facility type‡ | |||||||
| Unit | 12.7 (12.5, 12.9) | 16.8 (16.4, 17.1) | 17.2 (16.8, 17.5) | 9.4 (9.2, 9.6) | 6.0 (5.9, 6.1) | 19.1 (18.7, 19.4) | 11.7 (11.6, 11.8) |
| Freestanding | 12.7 (12.3, 13.0) | 15.8 (15.3, 16.3) | 17.7 (17.2, 18.1) | 9.4 (9.2, 9.7) | 5.5 (5.4, 5.7) | 18.5 (18.1, 18.9) | 11.8 (11.7, 11.9) |
| Missing | 13.7 (11.8, 15.6) | 15.6 (12.4, 18.9) | 14.3 (10.9, 17.8) | 9.6 (8.2, 11.1) | 8.2 (6.8, 9.6) | 19.9 (16.8, 22.9) | 12.2 (11.3, 13.0) |
| Ownership | |||||||
| Non-profit | 12.6 (12.5, 12.7) | 16.7 (16.6, 16.8) | 17.1 (17.0, 17.2) | 9.3 (9.2, 9.4) | 5.8 (5.8, 5.9) | 19.1 (18.9, 19.2) | 11.6 (11.5, 11.7) |
| For profit | 12.9 (12.8, 13.1) | 16.1 (15.9, 16.2) | 17.8 (17.6, 17.9) | 9.6 (9.5, 9.7) | 5.8 (5.7, 5.9) | 18.5 (18.4, 18.7) | 12.0 (11.9, 12.1) |
| Government | 12.5 (12.1, 12.8) | 15.3 (15.0, 15.7) | 16.4 (16.0, 16.7) | 9.3 (9.0, 9.6) | 5.7 (5.5, 6.0) | 19.4 (18.9, 19.8) | 11.3 (10.9, 11.6) |
| Missing | 14.2 (13.3, 15.0) | 15.3 (14.5, 16.2) | 14.3 (13.5, 15.1) | 9.4 (8.7, 10.1) | 8.1 (7.4, 8.7) | 18.9 (18.0, 19.9) | 12.2 (11.4, 12.9) |
| Facility location△ | |||||||
| Urban | 12.7 (12.5, 12.8) | 16.5 (16.2, 16.8) | 17.5 (17.2, 17.8) | 9.4 (9.3, 9.6) | 5.8 (5.7, 5.9) | 18.9 (18.7, 19.2) | 11.8 (11.8, 11.9) |
| Rural | 12.8 (12.3, 13.3) | 16.0 (14.8, 17.2) | 16.5 (15.5, 17.4) | 9.5 (9.1, 9.9) | 6.1 (5.7, 6.4) | 17.8 (17.0, 18.6) | 11.1 (10.9, 11.3) |
| Missing | 13.7 (11.8, 15.6) | 15.6 (12.4, 18.9) | 14.3 (10.9, 17.8) | 9.6 (8.2, 11.1) | 8.2 (6.8, 9.6) | 19.9 (16.8, 22.9) | 12.2 (11.3, 13.0) |
Prior living setting categories are defined and recorded in the Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI).14
Disability based on persons meeting Social Security Disability criteria and receiving benefits for two years.
Dual eligibility refers to Medicare beneficiaries who qualify for both Medicare and Medicaid.
Tier comorbidity = Medicare tier level comorbidities developed for post-acute inpatient medical rehabilitation and recorded in the IRF-PAI.14
Cognitive and motor function are based on items from the Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI). The range of scores for motor items is 13–91; the range of scores for cognitive items is 5–35. Higher scores indicate better performance. 17 Admission includes rating within 36 hours of admission. Discharge includes ratings within 36 hours of discharge. Gain is the difference between admission and discharge ratings.14, 17
Facility type: Unit is located in acute care hospital; Freestanding refers to facilities that are independent versus hospital-based. This information is defined and recorded in the Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI).14
Facility location: Urban vs. Rural is defined and recorded in the Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI) file.
Table 2 shows the unadjusted hospital readmission status by percent and confidence interval for the total sample and for each impairment group. The 30-day hospital readmission rate across the six impairment groups was 11.8% (95%CI, 11.7%, 11.8%) and ranged from 5.8% (95%CI, 5.8%, 5.9%) for persons with lower extremity joint replacement to 18.8% (95%CI, 18.8%, 18.9%) for persons with debility. The readmission rate was higher for males (13.0%; 95%CI, 12.8%. 13.1%), non-Hispanic blacks, (13.8%; 95%CI, 13.5%, 14.1%), dual eligible beneficiaries (15.1%; 95%CI, 14.9%, 15.4%), and in patients with tier 1 comorbidities (25.6%; 95%CI, 24.9%, 26.3%). Readmission rate varied by case-mix group for each impairment category (Table 3). For example, the readmission rates for the 10 stroke case-mix groups ranged from 9.0% (95%CI, 8.4%, 9.7%) to 15.3% (95%CI, 14.9%, 15.8%).
Table 3.
Case-Mix Group (CMG)* distributions and 30-day readmission rates for each rehabilitation impairment category.‡
| Population
|
Readmitted
|
||
|---|---|---|---|
| N | Column % | % (95% CI) | |
| Stroke | 155,476 | 100.0 | 12.7 (12.5, 12.9) |
| CMG 0101 | 7,312 | 4.7 | 9.0 (8.4, 9.7) |
| CMG 0102 | 14,626 | 9.4 | 10.1 (9.6, 10.6) |
| CMG 0103 | 2,804 | 1.8 | 11.2 (10.0, 12.3) |
| CMG 0104 | 26,180 | 16.8 | 11.2 (10.8, 11.6) |
| CMG 0105 | 21,932 | 14.1 | 12.1 (11.7, 12.6) |
| CMG 0106 | 19,635 | 12.6 | 12.5 (12.1, 13.0) |
| CMG 0107 | 16,558 | 10.6 | 13.2 (12.7, 13.7) |
| CMG 0108 | 9,990 | 6.4 | 16.7 (15.9, 17.4) |
| CMG 0109 | 11,047 | 7.1 | 13.3 (12.7, 14.0) |
| CMG 0110 | 25,392 | 16.3 | 15.3 (14.9, 15.8) |
| Brain dysfunction | 62,974 | 100.0 | 16.4 (16.1, 16.7) |
| CMG 0201 | 456 | 0.7 | 12.1 (9.1, 15.1) |
| CMG 0202 | 1,858 | 3.0 | 12.3 (10.8, 13.8) |
| CMG 0203 | 1,707 | 2.7 | 11.3 (9.8, 12.8) |
| CMG 0204 | 2,638 | 4.2 | 11.1 (9.9, 12.3) |
| CMG 0205 | 9,477 | 15.0 | 13.2 (12.5, 13.9) |
| CMG 0206 | 4,194 | 6.7 | 14.3 (13.2, 15.3) |
| CMG 0207 | 4,393 | 7.0 | 15.6 (14.5, 16.7) |
| CMG 0301 | 9,348 | 14.8 | 15.3 (14.5, 16.0) |
| CMG 0302 | 7,412 | 11.8 | 18.3 (17.5, 19.2) |
| CMG 0303 | 10,447 | 16.6 | 19.2 (18.4, 19.9) |
| CMG 0304 | 11,044 | 17.5 | 20.4 (19.6, 21.1) |
| Neurologic conditions | 73,740 | 100.0 | 17.4 (17.1, 17.6) |
| CMG 0601 | 3,588 | 4.9 | 13.0 (11.9, 14.1) |
| CMG 0602 | 18,334 | 24.9 | 16.1 (15.5, 16.6) |
| CMG 0603 | 28,422 | 38.5 | 17.7 (17.2, 18.1) |
| CMG 0604 | 22,110 | 30.0 | 19.2 (18.7, 19.8) |
| CMG 1901 | 485 | 0.7 | 12.0 (9.1, 14.8) |
| CMG 1902 | 634 | 0.9 | 7.6 (5.5, 9.6) |
| CMG 1903 | 167 | 0.2 | 9.0 (4.6, 13.3) |
| Lower ext fracture | 169,426 | 100.0 | 9.4 (9.3, 9.6) |
| CMG 0701 | 9,643 | 5.7 | 6.1 (5.7, 6.6) |
| CMG 0702 | 34,377 | 20.3 | 7.4 (7.1, 7.6) |
| CMG 0703 | 40,062 | 23.6 | 9.0 (8.7, 9.2) |
| CMG 0704 | 76,958 | 45.4 | 11.1 (10.9, 11.3) |
| CMG 1701 | 723 | 0.4 | 6.5 (4.7, 8.3) |
| CMG 1702 | 1,748 | 1.0 | 7.6 (6.4, 8.9) |
| CMG 1703 | 1,793 | 1.1 | 8.4 (7.1, 9.6) |
| CMG 1704 | 4,122 | 2.4 | 9.1 (8.2, 10.0) |
| Joint replace | 184,282 | 100.0 | 5.8 (5.7, 5.9) |
| CMG 0801 | 6,905 | 3.7 | 4.3 (3.9, 4.8) |
| CMG 0802 | 68,103 | 37.0 | 4.7 (4.5, 4.8) |
| CMG 0803 | 10,125 | 5.5 | 6.7 (6.2, 7.2) |
| CMG 0804 | 56,107 | 30.4 | 5.8 (5.6, 6.0) |
| CMG 0805 | 29,144 | 15.8 | 7.2 (6.9, 7.5) |
| CMG 0806 | 13,898 | 7.5 | 9.0 (8.5, 9.4) |
| Debility | 90,638 | 100.0 | 18.8 (18.6, 19.1) |
| CMG 2001 | 4,649 | 5.1 | 14.1 (13.1, 15.1) |
| CMG 2002 | 24,328 | 26.8 | 16.9 (16.4, 17.4) |
| CMG 2003 | 35,740 | 39.4 | 19.3 (18.8, 19.7) |
| CMG 2004 | 25,921 | 28.6 | 20.9 (20.4, 21.4) |
Case-Mix Group (CMG): Patients are classified into a case-mix group at the time of admission based on impairment category, motor and cognitive functional status and age. Case-mix groups are used to determine Medicare fee for service payment for individual patient stays.
Rehabilitation Impairment Categories: Developed by CMS to classify patients receiving inpatient medical rehabilitation based on selected ICD-9-CM codes. See details in Appendix 1.
Several MS-DRGs were associated with readmission across all impairment categories. MS-DRG 689/690 (Kidney and Urinary Tract Infection), MS-DRG 193/194 (Simple Pneumonia and Pleurisy); MS-DRG 291/292 (Heart Failure and Shock), MS-DRG 391/392 (Esophagitis, Gastroenteritis and Miscellaneous Digestive Disorders), and MS-DRG 640/641 (Nutritional and Miscellaneous Metabolic Disorder) all occurred in the top 20 MS-DRGs for all rehabilitation impairment categories. MS-DRG 871/872 (Septicemia without MV96+ Hours) occurred in the top 10 MS-DRGs for all impairment categories except lower extremity joint replacement. The distribution of the top 25 MS-DRGs by impairment category is included in Appendix 2 on-line.
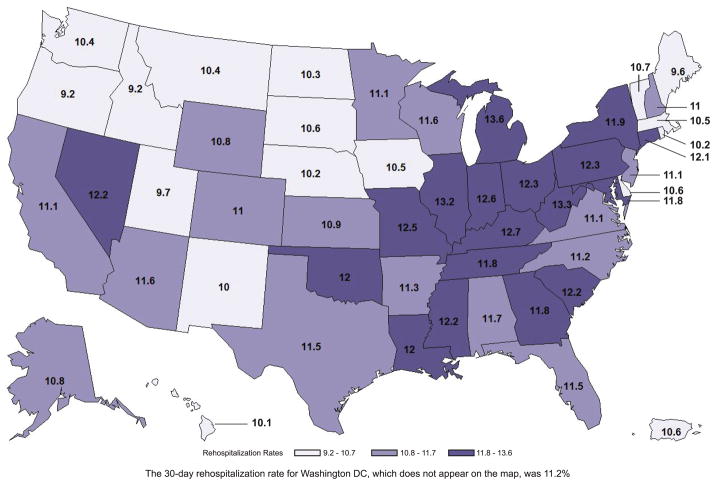
Figure 1 displays state readmission rates across the United States and Puerto Rico adjusted for age, sex, race/ethnicity, living situation, rehabilitation impairment category, tier comorbidities, and admission motor and cognitive functioning. The rates ranged from 9.2% (Idaho and Oregon) to 13.6% (Michigan) with a pattern of lower readmission rates in states in the mid-north and northwest.
Figure 1.
Rate (%) of hospital readmission within 30-days of discharge from rehabilitation.
DISCUSSION
Our results can be summarized as follows. The 30-day readmission rate among patients discharged to the community for the six impairment categories was 11.8%. Readmission varied from 5.8% for patients with lower extremity joint replacement to 18.8% for patients with debility. In 2011, MedPAC reported an all cause readmission rate across all conditions of 15.3% for acute care hospitals.4 An all cause readmission rate of 19.2% was reported for heart failure, respiratory infection, urinary tract infection, septicemia, and electrolyte imbalance in Medicare skilled nursing patients in 2010.7 The American Hospital Association reported an all cause readmission rate of 13.7% for long-term care hospitals based on 2007–2009 Medicare data.23 The above readmission rates are not directly comparable due to differences in adjustment models and patient groups included, but provide a context for our overall findings Our value of 11.8% is an under-estimate of the overall readmission rate for inpatient rehabilitation facilities since it is based on patients discharged to the community and includes six selected rehabilitation impairment groups.
Readmission rates for our sample were higher for men and non-Hispanic backs, for dual eligible beneficiaries, for persons with longer lengths of stay, and for individuals with rehabilitation tier level comorbidities. Readmission rates were similar for rural versus urban facilities, freestanding versus hospital-based, and ownership status. Patients with debility had the highest readmission rate. The number of cases in this impairment group has been increasing and the reason is not known.24 Research to better understand and manage persons in this impairment category represents an opportunity to reduce readmissions.
Higher motor and cognitive ratings, indicating better patient function, were consistently related to lower readmission rates across all impairment categories. Motor and cognitive status information is not available in Medicare data files for patients in short-term acute care hospitals. Analyses by MedPAC suggest that functional status measures, such as those used in the Medicare rehabilitation assessment data (IRF-PAI), improve the ability to predict resources use in post-acute settings.25, 26 This is an important area for future research related to readmission in acute and post-acute care.16, 27
We examined potential reasons for readmission for each impairment category following the approach used by Jencks et al.3 We found that the 25 most frequent MS-DRGs were associated with approximately 40–50% of the readmissions across the impairment categories. Several MS-DRGs were consistently related to readmission. Of particular interest are MS-DRGs representing potential targets for intervention to reduce readmission. For example, kidney and urinary tract infections (MS-DRG 689/690), pneumonia (MS-DRG 193/194), and nutritional and miscellaneous metabolic disorders (MS-DRG 640/641) were in the top 20 MS-DRGs associated with readmission for all six impairment categories. Septicemia (MS-DRG 871/872) was not in the top 20 MS-DRGs for lower extremity joint replacement, but was in the top 10 MS-DRGs for the five remaining rehabilitation impairment categories.
Approximately half of the rehospitalized patients were readmitted within 11 days after discharge. A number of investigators have argued that the 30-day readmission window is arbitrary.28, 29 Joynt and colleagues29 suggested that Medicare weight the Hospital Readmission Reduction Program penalties for acute care according to the timing of readmission because earlier readmissions may reflect poor care coordination or inadequate recognition of post-discharge needs.29, p. 1177 Care transition research suggests that programs involving early follow-up have reduced readmission for some patients.2, 30 Weighting the Medicare penalties based on earlier readmissions would provide incentive to develop innovative programs including patient/family education, home visits, partnerships with community primary care providers, and the use of technology to monitor compliance and medication use.
We found geographic variation in readmission with rates ranging from 9.2% to 13.6%. The variation is similar to that reported for patients discharged from acute care hospitals3, 4 with lower rates in the mid-northern and northwestern states and higher rates in southern and some mid-western states. The analysis was conducted at the state level and adjusted for rehabilitation impairment categories and sociodemographic factors. These findings need to be confirmed with more refined geographic analyses.
Consistent with research on acute care rehospitalizations, we found slightly higher readmission rates for males than females and for non-Hispanic blacks.3, 5, 31 Gender and racial disparities in healthcare are complex issues and much has been written regarding the need to reduce disparities.5, 31–33 This need extends to the emerging research literature on hospital readmissions in both acute and post-acute settings.
Medicare is currently examining bundled payment models designed to improve quality and contain costs.10, 11, 34 The payment options cover different time periods and include multiple healthcare providers and settings.26 In the context of bundled payment, what happens to patients during post-acute care becomes important in the management of resources, quality, cost, and readmissions.35 Recent research has demonstrated that most of the variation in Medicare spending across geographic areas is attributable to post-acute care.36 Readmission will likely add to the cost variation. For example, the median cost for a 30-day fixed length episode for a patient with major joint replacement of the lower extremity is $18,128 without readmission and $29,803 with readmission.23 In describing the role of readmission in bundled payment models, O’Malley states that, “Hospitals are not going to achieve meaningful reductions in readmission unless they are partnered with post-acute care.”37, p.12
Despite the establishment of readmission in acute care, and its introduction into post-acute care as an indicator of quality, questions remain regarding its validity.38 The evidence linking readmission to improvement in the care transition process and quality outcomes is inconsistent.39 Questions regarding the validity of readmission as a quality indicator are likely to increase as the accountability for readmission expands to include post-acute care settings.11 While readmission is an imperfect quality indicator, it has the potential to serve as a platform for efforts to improve patient transitions and care continuity associated with bundling and other initiatives proposed by the Affordable Care Act to reduce cost and improve health outcomes.2
Our study has several limitations. These include the reliability, accuracy and completeness of data collected for billing and administrative functions.40 The majority of our analyses are descriptive and included the ‘population’ of individuals meeting our inclusion criteria. We did not include adjustments for potential mediating factors except for the geographic variation analysis by state. Nor did we examine interactions across rehabilitation impairment categories or other subgroups.
The lack of variables directly measuring socioeconomic status and education in the Medicare claims files limits our ability to document the role of these factors in readmission. We did not attempt to differentiate between planned and unplanned readmissions. It is also important to understand that our decision to include only patients discharged to the community influenced the case-mix of the impairment groups analyzed. If all patients receiving inpatient rehabilitation were included in our analyses regardless of discharge destination the different case-mix would influence the results.
CONCLUSIONS
Among post-acute rehabilitation facilities providing services to Medicare fee-for-service beneficiaries, 30-day readmission rates ranged from 5.8% to 18.8% for selected impairment groups. Further research is needed to understand the reasons for readmission.
Supplementary Material
Acknowledgments
Funding. Supported by the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Center for Medical Rehabilitation Research (R24-HD065702, R01-HD069443 and K01-HD068513) and National Center for Advancing Translational Sciences, Clinical and Translational Science Award (UL1RR029876). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data, and preparation, review or approval of the manuscript.
Footnotes
Kenneth J. Ottenbacher and Amol Karmarkar had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Amol Karmarkar conducted and is responsible for all data analysis. Yong-Fang Kuo contributed to data analysis.
Anne Deutsch works at an inpatient rehabilitation facility – Rehabilitation Institute of Chicago. Carl Granger is employed by the Uniform Data System for Medical Rehabilitation. The remaining authors report no conflicts of interest, including financial interests, activities, relationships, and affiliations.
Author Contributions: K.J. Ottenbacher - conceptual development, first draft of all sections except methods and results, PI for primary funding sources; A. Karmarkar – analyze data, management of data files, draft of results, review and revision of manuscript; J. E. Graham – draft of methods, assist with data management, development of tables and figures, review and revision of manuscript; Y-F Kuo – contribute to analyses of data, provide interpretation of data, contribute to results and review and revision of entire manuscript; A. Deutsch – revision of methods, interpretation of data, contribute to and revise information on legislation and interpretation of CMS files, review and revision of manuscript; T Reistetter - contribute development of tables, figures and appendix material, provide interpretation for geographic data, review and revision of manuscript; S. Al Snih – analysis and interpretation of clinical data, provide interpretation for MS-DRG data including appendix, contribute to writing discussion and review and revision of entire manuscript; C.V. Granger – provide conceptual integration, interpretation of functional assessment and clinical variables, interpretation of functional status measures, assist in writing discussion and review and revision of manuscript.
References
- 1.111th Congress. Patient Protection and Affordable Care Act PL 111–148. 2010 http://www.healthcare.gov/law/index.html.
- 2.Goodman D, Fisher E, Chang C. The Revolving Door: A Report on US Hospital Readmissions. Princeton, NJ: Robert Wood Johnson Foundation; 2013. [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.MedPAC. Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 2013. [Google Scholar]
- 5.Joynt KE, Orav E, Jha AK. Thirty-day readmission rates for medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lichtman JH, Leifheit-Limson EC, Jones SB, et al. Predictors of Hospital Readmission After Stroke. A Systematic Review. Stroke. 2010;41:2525–2533. doi: 10.1161/STROKEAHA.110.599159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MedPAC. Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 2012. [Google Scholar]
- 8.CMS. Specificatins for the All-Cause Unplanned Readmission Measure for 30 Days Post Discharge from Inpatient Rehabilitation Faculities. Washington, DC: Centers for Medciare and Medicaid Services; 2013. [Google Scholar]
- 9.Federal Register. Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2014; Proposed Rule. Washington, DC: U.S. Government Printing Office; FR Doc No: 2013–10755; 2013. Report No.: Federal Register. 42 CFR Part 412, Volume 78, Number 89 (August 8, 2013) [Google Scholar]
- 10.DeJong G. Bundling acute and postacute payment: From a culture of compliance to a culture of innovation and best practice. Phys Ther. 2010;90(5):658–662. doi: 10.2522/ptj.2010.90.5.658. [DOI] [PubMed] [Google Scholar]
- 11.Hussey P, Mulcahy A, Schnyer C, Schneider E. Evidence Report/Technology Assessment No. 208. Rockville, MD: Agency for Healthcare Research and Quality; 2012. Bundled Payment Effects on Health Care Spending and Quality. Closing the Quality Gap: Revisting the State of the Science. (Prepared by RAND Evidence-based Practice Center) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan L, Koepsell TD, Deyo RA, et al. The effect of Medicare’s payment system for rehabilitation hospitals on length of stay, charges, and total payments. N Engl J Med. 2009;337(14):978–985. doi: 10.1056/NEJM199710023371406. [DOI] [PubMed] [Google Scholar]
- 13.Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI) Training Manual. Buffalo, NY: Uniform Data System for Medical Rehabilitation; 2001. [Google Scholar]
- 14.Federal Register. Federal Register: Quality Report Program for IRFs. Washington, DC: Department of Health and Human Services; 2011. Report No.: 76. [Google Scholar]
- 15.Carter G, Totten M. TR-201-CMS, editor. Preliminary Analyses for Refinement of the Tier Comorbidities in the Inpatient Rehabilitation Facility Prospective Payment System. Santa Monica, CA: Rand Corporation; 2005. [Google Scholar]
- 16.Granger CV, Deutsch A, Russell C, Black T, Ottenbacher KJ. Modifications of the FIM instrument under the inpatient rehabilitation facility prospective payment system. Am J Phys Med Rehabil. 2007;86(11):883–892. doi: 10.1097/PHM.0b013e318152058a. [DOI] [PubMed] [Google Scholar]
- 17.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: A quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 18.Stineman MG, Shea JA, Jette A, et al. The Functional Independence Measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. 1996;77(11):1101–1108. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- 19.Carter GM, Relles DA, Ridgeway GK, Rimes CM. Measuring function for Medicare inpatient rehabilitation payment. Health Care Financ Rev. 2003;24(3):25–44. [PMC free article] [PubMed] [Google Scholar]
- 20.McNutt R, Johnson TJ, Odwazny R, et al. Change in MS-DRG Assignment and Hospital Reimbursement as a Result of Centers for Medicare & Medicaid Changes in Payment for Hospital-Acquired Conditions: Is It Coding or Quality? Quality Management in Healthcare. 2010;19(1) doi: 10.1097/QMH.0b013e3181ccbd07. [DOI] [PubMed] [Google Scholar]
- 21.Blyth C, Still H. Binomial confidence intervals. J Am Statist Assoc. 1983;78:108–116. [Google Scholar]
- 22.Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circul Cardiovas Qual & Outcomes. 2009;2(5):407–413. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 23.American Hospital Association. Issue Brief: Moving Towards Bundled Payment. Washington, DC: American Hospital Association; 2013. [Google Scholar]
- 24.Galloway RV, Granger CV, Karmarkar AM, et al. The Uniform Data System for Medical Rehabilitation: Report of Patients with Debility Discharged from Inpatient Rehabilitation Programs in 2000–2010. Am J Phys Med Rehabil. 2013;92(1):14–27. doi: 10.1097/PHM.0b013e31827441bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.3M Health Information Systems. The impact of disability measures on expected Medicare payments and expected provider charges for event-based episodes that include post-acute care. Salt Lake Cite, UT: 3M Health Information Systems; 2013. [Google Scholar]
- 26.MedPAC. Report to the Congress: Medicare and the Health Care Delivery System. Washington, DC: Medicare Payment Advisory Commission; 2013. [Google Scholar]
- 27.Deutsch A, Mallinson T, Gage B. Analysis of crosscutting Medicare functional status quality metrics using Continuity and Assessment Record and Evaluation (CARE) item set. Washington, DC: RTI International; 2012. Report No.: 0212050. [Google Scholar]
- 28.Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: Penny wise and pound foolish? Arch Intern Med. 2010;170(4):340–346. doi: 10.1001/archinternmed.2009.511. [DOI] [PubMed] [Google Scholar]
- 29.Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368(13):1175–1177. doi: 10.1056/NEJMp1300122. [DOI] [PubMed] [Google Scholar]
- 30.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: A systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 31.Li Y, Glance L, Yin J, Mukamel D. Racial disparities in rehospitalization among Medicare patients in skilled nursing facilities. Am J Public Health. 2011;101(5):875–882. doi: 10.2105/AJPH.2010.300055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 33.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (Institute of Medicine) Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 34.Mechanic R, Tompkins C. Lessons learned preparing for medicare bundled payments. N Engl J Med. 2012;367(20):1873–1875. doi: 10.1056/NEJMp1210823. [DOI] [PubMed] [Google Scholar]
- 35.Chandra A, Dalton MA, Holmes J. Large increases In spending on postacute care In Medicare point to the potential for cost savings in these settings. Health Aff. 2013;32(5):864–872. doi: 10.1377/hlthaff.2012.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368(16):1465–1468. doi: 10.1056/NEJMp1302981. [DOI] [PubMed] [Google Scholar]
- 37.American Hospital Association. Trendwatch: Maximizing the Value of Post-acute Care. Washington, DC: American Hosptial Association; 2010. [Google Scholar]
- 38.Axon R, Williams M. Hospital readmission as an accountability measure. JAMA. 2013;305(5):504–505. doi: 10.1001/jama.2011.72. [DOI] [PubMed] [Google Scholar]
- 39.Brock J, Mitchell J, Irby K. Association between quality improvement for care transitions in communities and rehospitalizations among medicare beneficiaries. JAMA. 2013;309(4):381–391. doi: 10.1001/jama.2012.216607. [DOI] [PubMed] [Google Scholar]
- 40.van Walraven C, Austin P. Administrative database research has unique characteristics that can risk biased results. J Clin Epidemiol. 2012;65:126–131. doi: 10.1016/j.jclinepi.2011.08.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.