Abstract
Background
Dengue is a major contributor to morbidity in children aged twelve and below throughout Cambodia; the 2012 epidemic season was the most severe in the country since 2007, with more than 42,000 reported (suspect or confirmed) cases.
Methods
We report basic epidemiological characteristics in a series of 701 patients at the National Paediatric Hospital in Cambodia, recruited during a prospective clinical study (2011–2012). To more fully explore this cohort, we examined climatic factors using multivariate negative binomial models and spatial clustering of cases using spatial scan statistics to place the clinical study within a larger epidemiological framework.
Results
We identify statistically significant spatial clusters at the urban village scale, and find that the key climatic predictors of increasing cases are weekly minimum temperature, median relative humidity, but find a negative association with rainfall maximum, all at lag times of 1–6 weeks, with significant effects extending to 10 weeks.
Conclusions
Our results identify clustering of infections at the neighbourhood scale, suggesting points for targeted interventions, and we find that the complex interactions of vectors and climatic conditions in this setting may be best captured by rising minimum temperature, and median (as opposed to mean) relative humidity, with complex and limited effects from rainfall. These results suggest that real-time cluster detection during epidemics should be considered in Cambodia, and that improvements in weather data reporting could benefit national control programs by allow greater prioritization of limited health resources to both vulnerable populations and time periods of greatest risk. Finally, these results add to the increasing body of knowledge suggesting complex interactions between climate and dengue cases that require further targeted research.
Background
Globally, dengue is the most widespread arbovirus, causing an estimated 390 million [95% Bayesian uncertainty interval 284–528] infections a year, of which only 96 million [67–136] are captured via surveillance systems [1]. Dengue is endemic throughout Cambodia, one of the poorest countries in Asia, which currently faces numerous health challenges with limited health infrastructure and poor economic indicators [2]. Morbidity from dengue is extensive due to a range of interconnected factors, including delays in care seeking, limited impacts of vector control, and limitations within the health sector [3,4].
Historically, large epidemics have occurred on a 3–4 year cycle, and generally all four dengue virus serotypes circulate annually; DENV-2 and DENV-3 predominated until recently, but have been largely displaced by DENV-1 since 2009 [5]. Dengue cases are reported throughout the year, but with a sharp increase during the rainy season (May to November).
A national syndromic surveillance program was established in 1980, which includes passive reporting of clinically diagnosed cases by public sector hospitals. Dengue is included in the list of the 12 priority diseases that are reported weekly to the Communicable Disease Control Department of the Ministry of Health (MOH); this reporting system contains only aggregated data on new cases and deaths for the diseases under syndromic surveillance. To supplement this system, in 2001 the National Dengue Control Program (NDCP) of the MOH implemented a hospital-based surveillance in seven paediatric hospitals or paediatric wards within referral hospitals. Weekly case reporting from these sentinel hospitals includes basic demographic indicators (age, gender, place of residence) clinical findings on admission, and status at discharge. Subsequently, this program was enhanced by the inclusion of virological and serological surveillance at five sentinel hospital sites. During the period 2002–2008, the National Dengue Control Program (NDCP) has reported on average 103 cases per 100,000 with an annual case fatality rate (CFR) ranging from 0.7 to 1.7% [3]. However, these sentinel sites are not able to capture detailed epidemiological, clinical or laboratory data, and reporting is generally incomplete; a capture-recapture study in Cambodia indicated a 4- to 29-fold underreporting rate [6]. The 2012 epidemic season was the most severe in the country since 2007, with more than 42,000 suspect or confirmed cases reported, and serves to highlight the serious epidemic potential within Cambodia.
To help address these limitations, our clinical study was designed to capture comprehensive data for a prospective series of paediatric dengue cases. The global objectives were to fully explore the epidemiology and clinical spectrum of clinical paediatric dengue in Cambodia; this portion of the study examines the captured clinical cases within the larger epidemiological context of spatial and climatic trends.
As a vector-borne disease, dengue transmission is inherently tied to weather patterns and climatic cycles, and epidemics generally peak during the wet season, beginning in the ‘hot wet’ season from May-August, and then tapering off through the ‘cold wet’ season in September. However, the fine-scale interactions of these climatic conditions on Aedes vector populations are poorly understood. Recent years have seen progressively larger epidemics throughout Cambodia and SE Asia; detailed spatial and epidemiological data are therefore increasingly critical to maximize the effectiveness of control programs within inherently limited budgets [7].
Methods
Sampling plan
Enrolment was organized weekly from September 20, 2011 to January 15, 2013 during specific surveillance days in both the internal medicine and emergency wards of the National Paediatric Hospital, Phnom Penh. All children aged 1–15 years and presenting with fever, or history of fever within seven days, on admission were screened for eligibility criteria using the 1997 and the 2009 WHO dengue case definitions [8,9]. Informed consent was obtained from parents or legal guardians for all eligible children. Demographics and clinical data on admission and during hospitalization were reported on a study-designed Case Report Form (CRF). Paired sera were collected on admission and at discharge and shipped via courier the same day for serologic (IgM Capture ELISA and haemagglutination inhibition assays) and virological (virus isolation on 2 cell lines, real time RT-PCR, and NS1 antigen detection by commercial ELISA (BioRad®)) tests for dengue and other arboviral infections (i.e., Japanese encephalitis and chikungunya) as reported previously [10]. Anonymized data were entered into an electronic password-protected database by a trained data manager, using Epi-Data 3.1 (Odense, Denmark) with range-checks; data monitoring was performed by a clinician who checked the concordance between the clinical notes, the study CRF and the electronic files; discrepancies were then corrected in both the CRF and the dataset.
Data sources
All clinical data in this study were collected by National Paediatric Hospital staff (Phnom Penh) and all serolological and virological testing were performed at the virology department of Institut Pasteur, Phnom Penh. Temperature and humidity data were obtained for the weather station in Phnom Penh [11], and precipitation was obtained from satellite estimations [12]. Population data and population density were obtained from published reports from the Ministry of Statistics (2008) [13]. Approximately 60% of the 558 dengue-positive patients resided in the greater Phnom Penh area; 216 patients were geocoded to the sangkat (commune/urban village) level. National-level reporting data was provided by the National Dengue Control Program at the Ministry of Health, Phnom Penh; open source base map layers were obtained from Open Development Cambodia (March 2013), see http://www.opendevelopmentcambodia.net/maps/downloads/.
Data analysis- regressions
Analysis of the relationship between weather events and national reported disease counts utilized Poisson regression for over-dispersed data (negative binomial), and examined the time period January 2011 to January 2013. All time-series models utilized Newey-West error corrections for autocorrelated and heteroskedastic data [14]. Explanatory factors examined were the weekly mean, median, minimum, and maximum of available weather data, including temperature, relative humidity and rainfall, plus the rainfall index defined as [(cumulative rainfall X days with rainfall)/days in reporting period] [15]. Lag periods of 1–15 weeks were examined for all variables. Optimal models were identified by Akaike information (AIC) and Bayesian information (BIC) criteria; model fit was assessed using standardized deviance residuals [16]. Stata 13.1 (College Station, Texas) was used for all analyses and all tests were two-tailed, with α = 0.05.
Data analysis- spatial
Visualization of captured cases data utilized ArcGIS 10.1 and QGIS 1.8 ‘Lisboa.’ Detailed mapping and analysis included only patients residing within greater Phnom Penh; cases were geo-referenced to the centroid of the respective sangkat (commune). ‘Hot-spot’ detection used SaTScan version 9.1 [17]; spatial and spatio-temporal clusters were examined with Poisson models including the underlying population density by commune. Bernoulli models were not utilized due to the limited number of dengue-negative patients. Clusters were limited to 25% of the total population, and estimations used 999 replications for Monte Carlo inference.
Ethics review
The study was conducted according to the ethical principles of the Declaration of Helsinki of October 2002. The Cambodian National Ethics Committee for Health Research approved the overall study protocol after institutional review (approval number 123-NECHR, 22 August 2011).
Results
From September 20, 2011 to January 15, 2013 a total of 1,228 febrile cases were admitted to the two participating wards. An eligibility form was completed for more than 96% of these admissions (1,185/1,228); the proportion of eligible patients was 59% (703/1,185) and the study refusal rate was less than 1% (2/703). A total of 701 suspected dengue patients were enrolled during the study period, and of these 80% (558/701) had a laboratory confirmation of dengue (Figure 1).
Figure 1.
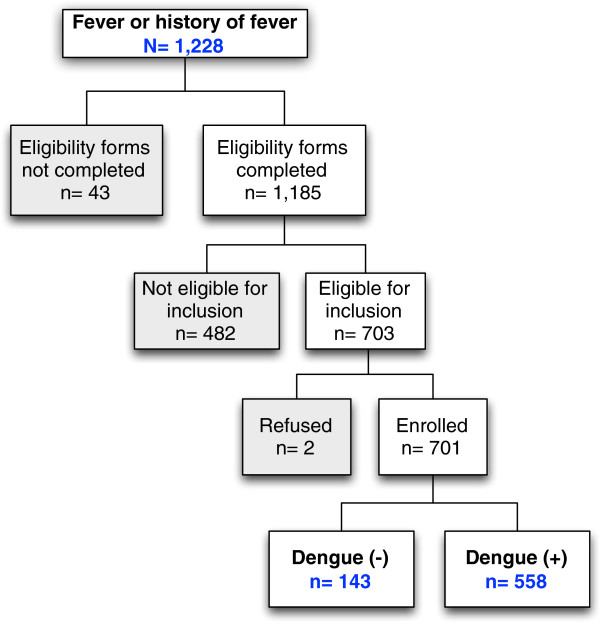
Patient inclusion flow, National Paediatric Hospital, Phnom Penh, January 2011- January 2013.
All four serotypes were identified during the study, but DENV-1 predominated (520/558; 93%) (Table 1). Our sentinel surveillance also detected a noteworthy chikungunya outbreak reported in Cambodia in 2012: 7 patients had test results which were suggestive of recent chikungunya infection [18,19]. However, no pathogens were identified in the remaining patients.
Table 1.
Results of the dengue serological and virological testing (N = 701), National Paediatric Hospital, Phnom Penh, September 2011 - January 2013
|
Diagnosis |
n |
% of total |
% of all dengue positive or negative |
|
|---|---|---|---|---|
| (95% CI) | (95% CI) | |||
|
Positive dengue |
558 |
79.6 |
- |
|
| |
(76.4 - 82.5) |
|
||
| |
Dengue 1 |
520 |
- |
93.2 |
| |
|
(90.8 – 95.1) |
||
| |
Dengue 2 |
8 |
- |
1.4 |
| |
|
(0.6 – 2.8) |
||
| |
Dengue 3 |
1 |
- |
0.2 |
| |
|
(0.005 – 1.0) |
||
| |
Dengue 4 |
2 |
- |
0.4 |
| |
|
(0.04 – 1.3) |
||
| |
Serotype unspecified |
27 |
- |
4.8 |
| |
|
(3.2 – 7.0) |
||
|
Negative dengue |
143 |
20.4 |
- |
|
| |
(17.5 – 23.6) |
|
||
| |
Chikungunya |
7 |
- |
4.9 |
| (2.0 – 9.8) | ||||
Overall the proportion of under-5 children was 18% (128/558) with an equal number of boys and girls. The onset of fever prior admission was less or equal to three days for 18% of subjects (126/558), and the median duration of hospital stay was 3 days. Overall, there were 5 deaths in the study population, indicating a case-fatality rate of 0.7% (95% CI, 0.2–1.7%).
To assess the representativeness of our hospital cohort relative to the national epidemic, we compared the weekly caseload of admissions at the National Paediatric Hospital with the figures reported nationally (Figure 2). While this represents a crude proxy, the relationship is statistically significant across the study period when compared by simple correlation (R2 = 0.67; p < 0.001) and by time-series regression (p < 0.001). These results indicate that the temporal trends within the hospital and across Cambodia are highly correlated and suggest that the admission trends in cases captured in our study are indeed representative of the national-scale dengue epidemic.Two purely spatial clusters were identified (Figure 3). In the first cluster, 46 cases were aggregated within the southwest of the Phnom Penh suburban area over the entire reporting period (RR = 2.12, no CI; p = 0.004). The second cluster includes 43 cases aggregated in central Phnom Penh (RR = 1.93, no CI; p = 0.031). These p-values of less than 0.05 suggest these specific case aggregations are unlikely to be due to chance. In spatio-temporal analysis, only a single large cluster (radius > 9 km) was found to be marginally significant (p = 0.04) during October 2011 (data not shown). The standardized annual rates (per 100,000 population) within the city are shown as a choropleth map in Figure 4; highest rates are evident in the southwest and central regions, and these regions of highest risk coincide with the clusters identified in the spatial analysis. To assess any biases in capture of patients with geocoded addresses, the baseline demographics of patients were compared to the overall study population, and no significant differences were found (gender by rank-sum test, p = 0.302; age by Kruskal-Wallis test, p = 0.063).
Figure 2.
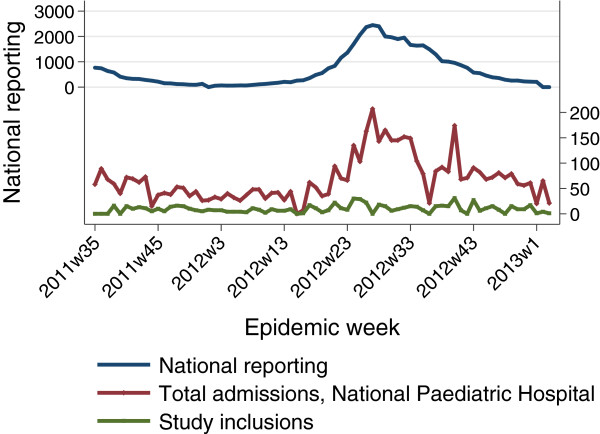
Comparison of national reporting data versus hospital inpatient cases, National Paediatric Hospital, Phnom Penh September. 2011- January 2013. Note: (p < 0.001, time-series regression of total hospital admissions and national cases).
Figure 3.
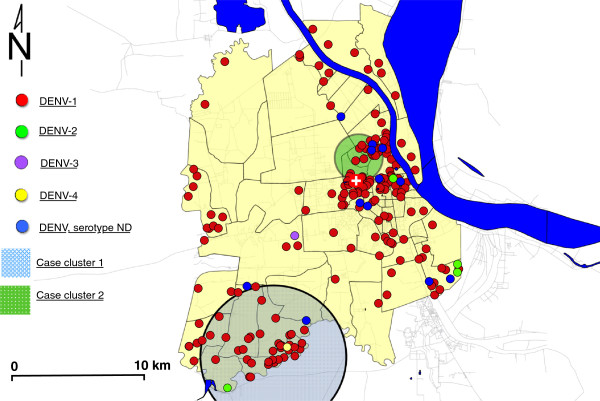
Mapping of cases by serotype showing significant spatial clusters within greater Phnom Penh, by smallest administrative district (sangkat) (n = 216). Note: Cluster 1 (radius- 5.2 km): 46 cases; relative Risk = 2.1 (p = 0.004); Cluster 2 (1.7 km): 43 cases; relative Risk = 1.9 (p = 0.031).
Figure 4.
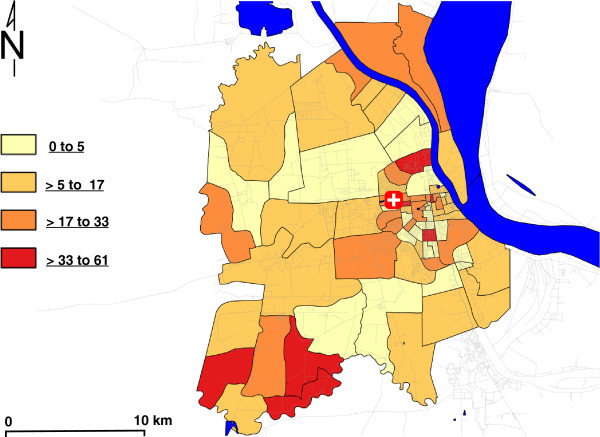
Mapping of cases as annual population standardized rates per 100,000 total population (2008 population estimates) by smallest administrative district ( sangkat ) (n = 216).
In the analysis of climatic impact on national dengue reports, three examined variables had greatest explanatory power in bivariate analysis: minimum weekly temperature; median weekly relative humidity; and weekly maximum rainfall (see Additional file 1: Table S1). The minimum temperature was positively correlated with the number of cases nationwide, with significant effects at lagged intervals of 1–3, 6, and 9–11 weeks. The corresponding incidence rate ratios (IRRs), ranging from 1.12 to 1.22, indicate a 12-22% increase in cases per degree Celsius increase in the weekly minimum temperature. The median relative humidity was also positively correlated with dengue cases in multivariate models, having significant effects at 1–3 weeks, with an IRR ranging from 1.036-1.042, indicating a 4% increase in cases for each unit increase in the weekly median relative humidity. Figure 5 illustrates the general relationships between national reported cases and significant climatic variables from multivariate analysis.
Figure 5.
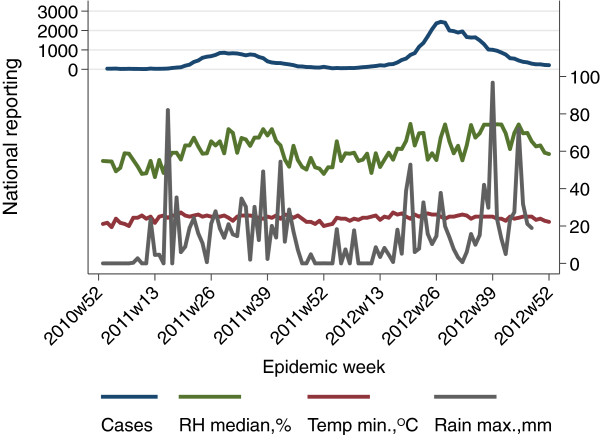
Comparison of national reporting data and significant climatic variables, Cambodia national data, December 2010- December 2012. Note: RH = relative humidity.
Among the examined rainfall variables, the maximum weekly rainfall showed the strongest association with reported dengue cases, with a positive correlation in bivariate analysis. However, in multivariate analysis the coefficients became negative, indicating an inverse relationship with dengue cases after adjusting for covariates. Lag periods of 1–5, and 10–12 weeks were all significant, with IRRs ranging from 0.991–0.987, indicting a 0.9–1.3% decrease in cases per mm of rain per week. Analysis of data from the other weather station in Cambodia (Siem Reap; not shown) indicates the same general multivariate trends, however these data are limited by extensive missing values.
Discussion
We present the results of a large prospective descriptive study of paediatric dengue infection conducted in a single referral centre in Phnom Penh, Cambodia. All 701 children enrolled in the study were initially suspected as having dengue, and nearly 80% included had a positive confirmatory test. The inclusion period was from September 2011 to January 2013, which covered two dengue epidemic seasons. Although all four serotypes were found in circulation during the period, DENV-1 predominated in 2012–2013; these trends are consistent with data from the National Surveillance system [5].
Spatial epidemiology has been specifically highlighted as a key component to guide dengue control efforts, especially in resource-limited settings. A recent analysis of large-scale transmission patterns of dengue in Cambodia identified ‘hotspots’ - zones of high transmission that may serve as reservoirs of virus for subnational scale epidemiology [20]. Extensive fever cohorts have found large differences in transmission within and between urban and rural regions [21]; however, these studies did not address neighbourhood-scale effects, which are dominated by human movements between neighbourhoods. The results from this study show substantial heterogeneity of transmission within Phnom Penh, mirroring larger scale infection dynamics within Cambodia. Our results suggest that rapid identification and targeting of these areas could have important impacts on transmission, especially in areas of high population density.
When examined as total cases per population for the study period, we identified several areas of elevated risk in the southwest and central areas of Phnom Penh aggregated over the course of this study. Such clusters could be high-risk areas for dengue epidemics due to larval sites or other modifiable characteristics and should be prioritized for vector control activities including community health promotion & education, elimination of breeding sites, water treatment using larvicides, and isolation of fever cases. Recent large-scale studies conducted in Bangkok found long-term modulation of transmission based on population-level (‘herd’) immunity at the neighbourhood scale [22]; our study findings are consistent with these results. The overwhelming predominance of a single serotype, however, hindered investigation of serotype-specific clusters and any potential interactions on population immunity.
The time lags identified within this study are broadly consistent with those found in other locations within SE Asia: in Thailand lag times of 6 months for temperature maxima and 3 months for rainfall events were identified; in Singapore, lag times of 1–5 months for mean temperature and rainfall events were identified [23,24]. In common with studies in Sri Lanka and New Caledonia, we find very limited and complex impact of rainfall on dengue incidence [25,26]. A main limitation is that the rainfall data are derived from satellite imagery, and may have limited spatial and temporal accuracy. However, satellite imagery in general has been shown to be most accurate for low latitudes during the warm season [27], suggesting that these estimates are likely reasonable. Additional support for this interpretation is the finding of an inverse relationship between rainfall and Aedes larval densities in Malaysia, suggesting a ‘flooding-out’ of larval habitats during periods of extreme rainfall [28]. These results concur with recent studies that found complex non-linear interactions between climatic variables and dengue incidence [29].
Limitations of this study
These data have been collected in a single referral paediatric hospital in Phnom Penh during a limited period of time, and therefore our findings may not be representative of other areas with different dengue transmission patterns, populations or population density characteristics. Cases from the spatiotemporal analyses were limited to those cases with an address that could be geo-referenced; some patients provided the name of an older administrative system that could not be readily mapped; however, this bias would have led to omission of cases This would not impact cluster detection with underlying population values as any impacts would be expected to dilute the observed effect sizes. There were no significant differences in age or gender between captured patients and those without addresses, suggesting there was no differential loss to follow-up.
There is also the potential for bias in our results due to differences in care-seeking behaviour. Patients are likely to seek care at the closest referral centre, which may partially explain the clustering of the cases in this study within Phnom Penh. However, as the hospital serves as the main paediatric referral centre within the public sector, this bias is likely minor.
We have also used a single set of weather data to predict the national scale epidemic. The local-scale interactions between climate, vectors and people - that is, the micro-epidemiology and heterogeneous exposures - cannot be captured at this scale [30].
Bearing these limitations in mind, our analysis shows a very strong correlation between observed trends and national dengue data trends as well as a strong correlation between local rainfall and temperature data and satellite estimates at the national level.
Conclusions
From an operational standpoint, the monitoring of peak temperatures, extreme humidity and rainfall indexes could help prioritize resources to be mobilized to address any emerging transmission cycles; however, the lead times identified in these data of 1–6 and 9–10 weeks might not provide sufficient time to implement aggressive campaigns in a resource-limited setting like Cambodia. Our results also suggest that a wider range of weather summary indexes should be incorporated into models to improve model fit and prediction. Recent work in malaria also suggests that predictions may be improved by using high-resolution data instead of traditional regional and weekly summaries [31], and surveillance in Cambodia could benefit from improved weather reporting systems.
While the routine use of environmental variables for real-time dengue surveillance can be complex in real-world settings [32], the wide availability of open-source tools (QGIS, R software and SaTScan) [17,33,34] make this increasingly feasible even in resource-limited settings. These results can serve as a foundation for the implementation of robust real-time surveillance within Cambodia.
Finally, the ability to pre-plan and stockpile needed resources (control staff, Bti, etc.) should be considered [35], and the identification of multiple hotspots of higher risk relative to the remainder of Phnom Penh suggests areas that should targeted for enhanced surveillance and vector control efforts during future transmission seasons.
Competing interests
JLB is a paid employee of Sanofi Pasteur; YSL was a medical advisor for Sanofi Pasteur; all other authors declare that they have no conflicts of interest.
Authors’ contributions
JB assisted in the design of the overall clinical study; all other authors participated in conceptualizing the design and coordination/data collection of the overall clinical study. AAL and PC conceived, planned, and analysed the data for this analysis and wrote the first draft; all authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Time series negative binomial regression for reported national dengue cases, Cambodia, Dec. 2010- Dec. 2012.
Contributor Information
Andrew A Lover, Email: andrew.a.lover@gmail.com.
Philippe Buchy, Email: pbuchy@pasteur-kh.org.
Anne Rachline, Email: arachline@yahoo.fr.
Duch Moniboth, Email: moniboth@yahoo.com.
Rekol Huy, Email: rekolh@cnm.gov.kh.
Chour Y Meng, Email: Chchouchnn@yahoo.com.
Yee Sin Leo, Email: yee_sin_leo@ttsh.com.sg.
Kdan Yuvatha, Email: kyuvatha.nph@online.com.kh.
Ung Sophal, Email: Chchouchnn@yahoo.com.
Ngan Chantha, Email: chanthan@cnm.gov.kh.
Bunthin Y, Email: ybunthin@pasteur-kh.org.
Veasna Duong, Email: dveasna@pasteur-kh.org.
Sophie Goyet, Email: sophiegoyet@gmail.com.
Jeremy L Brett, Email: Jeremy.Brett@sanofipasteur.com.
Arnaud Tarantola, Email: atarantola@pasteur-kh.org.
Philippe Cavailler, Email: Philippe.CAVAILLER@geneva.msf.org.
Acknowledgements and funding
We are grateful for both the patients and their families for agreeing to take part in this study, and for the critical contributions of the staff and nurses at the National Paediatric Hospital, without which this study would not have been possible. We are also grateful for the assistance of Julien Cappelle (Institut Pasteur, Cambodia) for his assistance in bulk downloading of weather data. The rainfall data used in this study were acquired using the GES-DISC Interactive Online Visualization ANd aNalysis Infrastructure (Giovanni) as part of the NASA’s Goddard Earth Sciences (GES) Data and Information Services Center (DISC).
Funding for this study was provided by Sanofi-Pasteur. The sponsors of the study were involved in study design and review of the manuscript; the sponsors had no role in the data collection/analysis and the decision to publish was made jointly by all authors.
References
- Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, Drake JM, Brownstein JS, Hoen AG, Sankoh O, Myers MF, George DB, Jaenisch T, Wint GRW, Simmons CP, Scott TW, Farrar JJ, Hay SI. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Development Programme. Human Development Report. New York; London: United Nations; Eurospan; 2013. [Google Scholar]
- Huy R, Buchy P, Conan A, Ngan C, Ong S, Ali R, Duong V, Yit S, Ung S, Te V, Chroeung N, Pheaktra NC, Uok V, Vong S. National dengue surveillance in Cambodia 1980–2008: epidemiological and virological trends and the impact of vector control. Bull World Health Organ. 2010;88:650–657. doi: 10.2471/BLT.09.073908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauté J, Vong S. Cost and disease burden of dengue in Cambodia. BMC Public Health. 2010;10:521. doi: 10.1186/1471-2458-10-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dengue situation in Cambodia, 2012 update (National Dengue Control Programme) http://www.cnm.gov.kh/userfiles/file/Annual%20Report%202012/19_Dengue_CNM_%20Situation_2012.pdf.
- Vong S, Goyet S, Ly S, Ngan C, Huy R, Duong V, Wichmann O, Letson GW, Margolis HS, Buchy P. Under-recognition and reporting of dengue in Cambodia: a capture–recapture analysis of the National Dengue Surveillance System. Epidemiol Infect. 2012;140:491–499. doi: 10.1017/S0950268811001191. [DOI] [PubMed] [Google Scholar]
- Eisen L, Lozano-Fuentes S. Use of mapping and spatial and space-time modeling approaches in operational control of Aedes aegypti and dengue. PLoS Negl Trop Dis. 2009;3:e411. doi: 10.1371/journal.pntd.0000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Guidelines for Treatment of Dengue Fever / Dengue Haemorrhagic Fever in Small Hospitals. New Delhi: WHO Regional Office for South-East Asia; 1999. [Google Scholar]
- World Health Organization. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control. Geneva: World Health Organization; 2010. New edition. [PubMed] [Google Scholar]
- Andries A-C, Duong V, Ngan C, Ong S, Huy R, Sroin KK, Te V, Y B, Try PL, Buchy P. Field evaluation and impact on clinical management of a rapid diagnostic kit that detects dengue NS1, IgM and IgG. PLoS Negl Trop Dis. 2012;6:e1993. doi: 10.1371/journal.pntd.0001993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Integrated Surface Database (ISD) | National Climatic Data Center (NCDC) http://www.ncdc.noaa.gov/land-based-station-data/integrated-surface-database-isd.
- TRMM Multi-Satellite Precipitation Data. http://disc2.nascom.nasa.gov/Giovanni/tovas/TRMM_V7.3B42_daily.2.shtml.
- General Population Census 2008. http://celade.cepal.org/khmnis/census/khm2008/
- Newey WK, West KD. A simple, positive semi-definite, heteroskedasticity and autocorrelation consistent covariance matrix. Econometrica. 1987;55:703–708. doi: 10.2307/1913610. [DOI] [Google Scholar]
- Russell PF, West LS, Manwell RD. Practical Malariology. Philadelphia: W. B. Saunders; 1946. [Google Scholar]
- Dupont WD. Statistical Modeling for Biomedical Researchers. 2. Cambridge, New York: Cambridge University Press; 2009. [Google Scholar]
- Kulldorff M, Information Management Services, Inc. SaTScan. 2011. Software for the Spatial and Space-Time Scan Statistics, http://www.satscan.org/
- Duong V, Andries A-C, Ngan C, Sok T, Richner B, Asgari-Jirhandeh N, Bjorge S, Huy R, Ly S, Laurent D, Hok B, Roces MC, Ong S, Char MC, Deubel V, Tarantola A, Buchy P. Reemergence of chikungunya virus in Cambodia. Emerg Infect Dis. 2012;18:2066–2069. doi: 10.3201/eid1812.120471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Chikungunya outbreak--Cambodia, February-March 2012. MMWR Morb Mortal Wkly Rep. 2012;61:737–740. [PubMed] [Google Scholar]
- Teurlai M, Huy R, Cazelles B, Duboz R, Baehr C, Vong S. Can human movements explain heterogeneous propagation of dengue fever in Cambodia? PLoS Negl Trop Dis. 2012;6:e1957. doi: 10.1371/journal.pntd.0001957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vong S, Khieu V, Glass O, Ly S, Duong V, Huy R, Ngan C, Wichmann O, Letson GW, Margolis HS, Buchy P. Dengue incidence in urban and rural Cambodia: results from population-based active fever surveillance, 2006–2008. PLoS Negl Trop Dis. 2010;4:e903. doi: 10.1371/journal.pntd.0000903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salje H, Lessler J, Endy TP, Curriero FC, Gibbons RV, Nisalak A, Nimmannitya S, Kalayanarooj S, Jarman RG, Thomas SJ, Burke DS, Cummings DAT. Revealing the microscale spatial signature of dengue transmission and immunity in an urban population. PNAS. 2012;109:9535–9538. doi: 10.1073/pnas.1120621109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hii YL, Rocklöv J, Wall S, Ng LC, Tang CS, Ng N. Optimal lead time for dengue forecast. PLoS Negl Trop Dis. 2012;6:e1848. doi: 10.1371/journal.pntd.0001848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Focks DA, Barrera R. WHO Report of the Scientific Working Group meeting on Dengue, Geneva. Geneva: Working paper for the Scientific Working Group on Dengue Research, convened by the Special Programme for Research and Training in Tropical Diseases; 2006. Dengue Transmission Dynamics: Assessment and Implications for Control. http://www.who.int/tdr/publications/publications/swg_dengue_2.htm. [Google Scholar]
- Goto K, Kumarendran B, Mettananda S, Gunasekara D, Fujii Y, Kaneko S. Analysis of effects of meteorological factors on dengue incidence in Sri Lanka using time series data. PLoS One. 2013;8:e63717. doi: 10.1371/journal.pone.0063717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Descloux E, Mangeas M, Menkes CE, Lengaigne M, Leroy A, Tehei T, Guillaumot L, Teurlai M, Gourinat A-C, Benzler J, Pfannstiel A, Grangeon J-P, Degallier N, De Lamballerie X. Climate-based models for understanding and forecasting dengue epidemics. PLoS Negl Trop Dis. 2012;6:e1470. doi: 10.1371/journal.pntd.0001470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert EE, Janowiak JE, Kidd C. Comparison of near-real-time precipitation estimates from satellite observations and numerical models. Bull Am Meteorol Soc. 2007;88:47–64. doi: 10.1175/BAMS-88-1-47. [DOI] [Google Scholar]
- Wee LK, Weng SN, Raduan N, Wah SK, Ming WH, Shi CH, Rambli F, Ahok CJ, Marlina S, Ahmad NW, Mckemy A, Vasan SS, Lim LH. Relationship between rainfall and Aedes larval population at two insular sites in Pulau Ketam, Selangor, Malaysia. Southeast Asian J Trop Med Public Health. 2013;44:157–166. [PubMed] [Google Scholar]
- Hii YL, Zhu H, Ng N, Ng LC, Rocklöv J. Forecast of dengue incidence using temperature and rainfall. PLoS Negl Trop Dis. 2012;6:e1908. doi: 10.1371/journal.pntd.0001908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DL, Dushoff J, McKenzie FE. The risk of a mosquito-borne infection in a heterogeneous environment. PLoS Biol. 2004;2:e368. doi: 10.1371/journal.pbio.0020368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss DJ, Bhatt S, Mappin B, Boeckel TPV, Smith DL, Hay SI, Gething PW. Air temperature suitability for Plasmodium falciparum malaria transmission in Africa 2000–2012: a high-resolution spatiotemporal prediction. Malar J. 2014;13:171. doi: 10.1186/1475-2875-13-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racloz V, Ramsey R, Tong S, Hu W. Surveillance of dengue fever virus: a review of epidemiological models and early warning systems. PLoS Negl Trop Dis. 2012;6:e1648. doi: 10.1371/journal.pntd.0001648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- QGIS Development Team. QGIS Geographic Information System. Open Source Geospatial Foundation Project. 2013. http://qgis.osgeo.org.
- R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: Foundation for Statistical Computing; 2013. [Google Scholar]
- Conolly MA. World Health Organization: Communicable Disease Control in Emergencies: A Field Manual. Geneva: World Health Organization; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Time series negative binomial regression for reported national dengue cases, Cambodia, Dec. 2010- Dec. 2012.


