Abstract
PURPOSE
To evaluate the effects of different abutment geometries in combination with varying luting agents and the effectiveness of different cleaning methods (prior to re-cementation) regarding the retentiveness of zirconia copings on implants.
MATERIALS AND METHODS
Implants were embedded in resin blocks. Three groups of titanium abutments (pre-fabricated, height: 7.5 mm, taper: 5.7°; customized-long, height: 6.79 mm, taper: 4.8°; customized-short, height: 4.31 mm, taper: 4.8°) were used for luting of CAD/CAM-fabricated zirconia copings with a semi-permanent (Telio CS) and a provisional cement (TempBond NE). Retention forces were evaluated using a universal testing machine. Furthermore, the influence of cleaning methods (manually, manually in combination with ultrasonic bath or sandblasting) prior to re-cementation with a provisional cement (TempBond NE) was investigated with the pre-fabricated titanium abutments (height: 7.5 mm, taper: 5.7°) and SEM-analysis of inner surfaces of the copings was performed. Significant differences were determined via two-way ANOVA.
RESULTS
Significant interactions between abutment geometry and luting agent were observed. TempBond NE showed the highest level of retentiveness on customized-long abutments, but was negatively affected by other abutment geometries. In contrast, luting with Telio CS demonstrated consistent results irrespective of the varying abutment geometries. Manual cleaning in combination with an ultrasonic bath was the only cleaning method tested prior to re-cementation that revealed retentiveness levels not inferior to primary cementation.
CONCLUSION
No superiority for one of the two cements could be demonstrated because their influences on retentive strength are also depending on abutment geometry. Only manual cleaning in combination with an ultrasonic bath offers retentiveness levels after re-cementation comparable to those of primary luting.
Keywords: Implant abutments, Zirconia copings, CAD/CAM, Temporary cementation, Semi-permanent cementation, Cleaning method
INTRODUCTION
Titanium has been used as standard material in dental implantology for implants and abutments due to its excellent mechanical and biological properties. Nevertheless, there are some esthetical limitations for metal-based implant supported reconstructions because of its lacking translucency and dark grey margins.1,2 Therefore, Yttria-stabilized zirconia has been established as a suitable material for the basis of prosthetic superstructures on dental implants.3,4 This polycrystalline ceramic offers best mechanical resistance, biological advantages like reduced plaque-accumulation combined with a satisfying esthetical performance.5 The fabrication of such restorations via computer-aided design and computer-aided manufacturing (CAD/CAM) bears some advantages like an economic processing and advanced marginal precision6 where quality is affected by processing routes like centralized or in-lab production7 and different milling strategies.8 Implant-supported superstructures could be subdivided into screw-retained or cement-retained restorations. In literature, there is actually no consent which of these fixing techniques provides better mechanical or biological clinical performances and some advantages and disadvantages were still controversial. Cement-retained reconstructions provide better esthetics, functional occlusions, clinical operability and lower costs.9,10 Advantages of screw-retained superstructures are better reparability (for instance in case of loosening of the abutment-screw or chippings of the veneering ceramic) and cleanability due to their retrievability.11 Furthermore, there are possibly lower peri-implantitis rates because there is no cement-induced irritation of peri-implant tissues.12 However, during a 5-year observation period the survival rates of screw-retained and cement-retained implant crowns were similar.13 To maintain the advantages of retrievability also for cement-retained superstructures provisional or semi-permanent luting agents can be used.14 Otherwise the opacity of provisional luting agents may lead to a reduced esthetical performance and cement washout can induce debonding of the restoration.9 Modern semi-permanent cements from different companies developed for the luting especially on implant abutments provide higher levels of translucency and transparency. However, data regarding the retentiveness levels of semi-permanent luting agents are actually rare. Customized abutments offer some advantages towards the pre-fabricated ones. There is the possibility of individual angulation and resulting higher fracture resistances,15 advanced esthetics of the surrounding soft tissues due to a better support via a correct emergence profile,16 a better removability of remnants of cements17 and the reduction of technical complications like retention-loss or screw loosening.18,19 Furthermore, there is the opportunity for enhancing retentiveness of cement-retained copings due to optimized geometries20,21 where retention is more affected by taper and height than by width or total surface of the abutment.22,23
Cementation type implant restorations sometimes need recementationand to clean the remaining cements in an ultrasonic bath containing alcohol and sandblasting with aluminium oxide for zirconia copings prior to cementation on implant abutments were performed.24,25 Etching, burnout or manual cleaning (we think clinically the most common technique) with curettes or similar instruments are other known methods for removing provisional cement before re-cementing of the copings. But to the author's knowledge, there is only one study available that evaluates the effect of different cleaning methods on retentiveness of temporarily cemented casted (no zirconia) copings after re-cementation but for cleaning of the abutments, not the inner surface of the copings; and in that study, airborne particle abrasion was the most effective technique.26 Furthermore, sandblasting of zirconia copings is seen critically regarding the influence of the mechanical integrity of the copings by some authors,27,28 so that it is still unclear what cleaning method could be truly recommended for debonded temporarily cemented zirconia copings.
The aim of this study was to evaluate the retentiveness levels of single zirconia copings on titanium abutments cemented with a provisional (TempBond NE, Kerr, Hamm, Germany) and a semi-permanent (Telio CS Cem Implant, Ivoclar Vivadent, Ellwangen, Germany) luting agent in dependence on three different abutment geometries (prefabricated, customized-long and customized-short). Furthermore, the resulting retentive force of temporarily cemented zirconia copings on titanium abutments depending on three different cleaning methods (manual, manual in combination with ultrasonic bath and sandblasting) prior to re-cementation was investigated. Finally, a scanning electron microscopy (SEM) analysis of the inner surface of the zirconia copings after the different cleaning techniques was performed.
MATERIALS AND METHODS
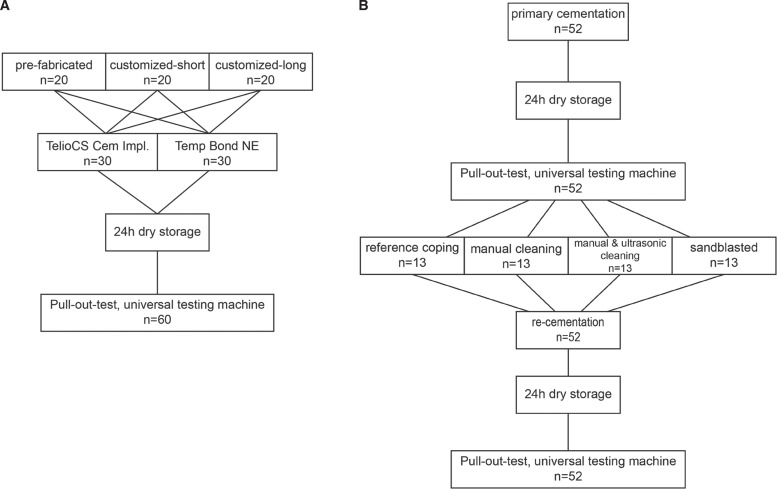
For evaluation of the retentiveness of zirconia copings two series of uni-axially pull-out tests were performed: a) regarding the influence of three different geometries in combination with two different luting agents (n = 60)(Fig. 1 show all conducted investigations) and b) regarding the influence of three different cleaning techniques (n = 52) after debonding prior to re-cementation of the copings.
Fig. 1.
Scheme of pull-out tests with zirconia copings. (A) varying abutment geometries and luting agents, (B) varying cleaning methods.
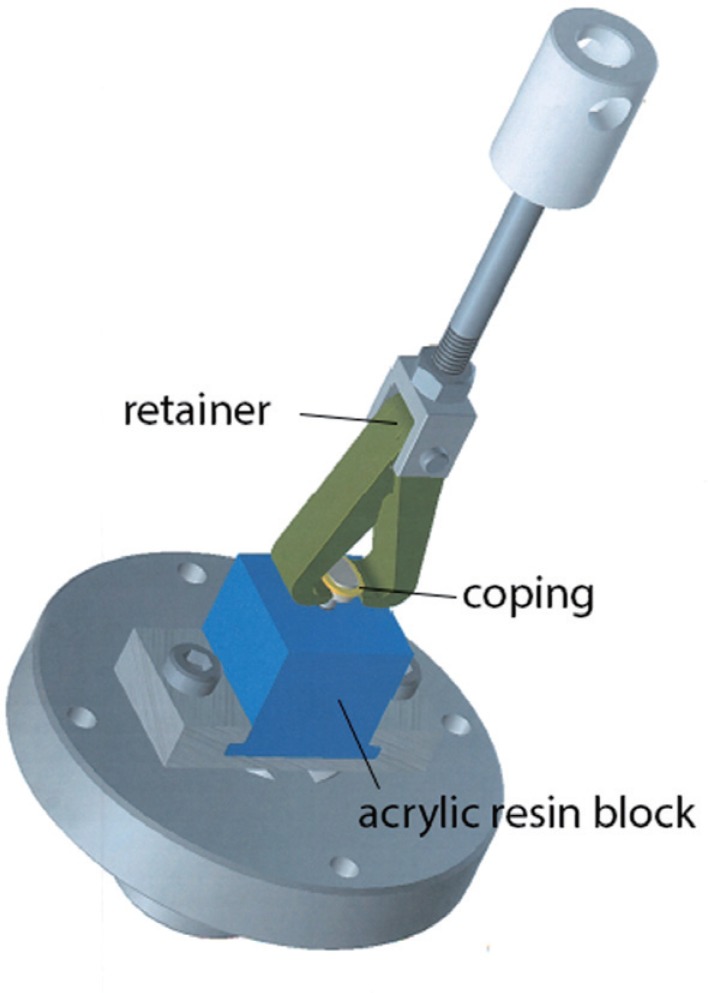
Titanium Ankylos implants (Dentsply Implants Manufacturing GmbH, Mannheim, Germany) with a diameter of 3.5 mm and a length of 11 mm were embedded strictly vertical with the help of a parallelometer in a block of autopolymerizing acrylic resin (Palavit G, Heraeus Kulzer, Hanau, Germany). An individually designed retainer made of stainless steel was used to fix the acrylic resin block (Fig. 2) into a universal testing machine.
Fig. 2.
Scheme of the individually designed metal retraction device to fix the specimens for pull-out tests into a universal testing machine.
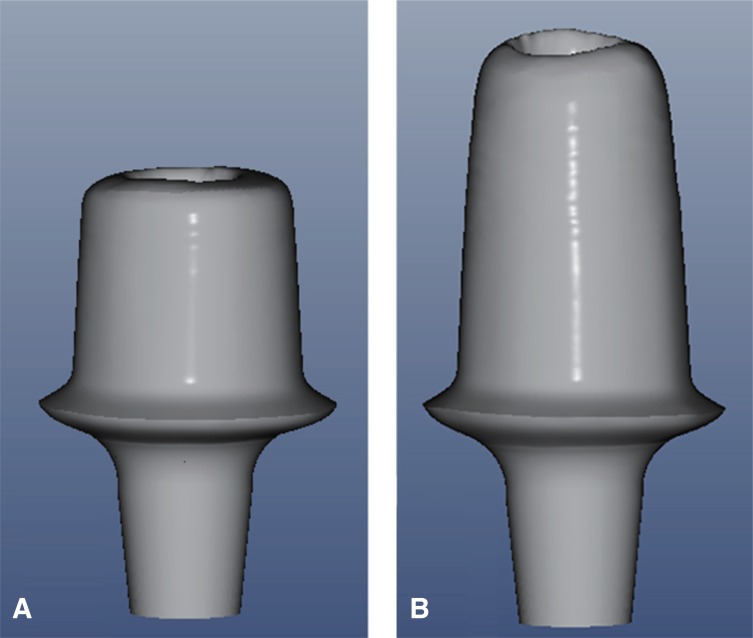
Three different types of titanium abutments were used. In the first series pre-fabricated abutments with a height of 7.5 mm and a taper of 5.7° (Ankylos Regular C, Dentsply Implants Manufacturing GmbH, Mannheim, Germany) were used. The customized abutments and all fabricated zirconia copings were designed using the CAD system Cercon art 3.2.2 (DeguDent GmbH, Hanau, Germany) and fabricated by Compartis (DeguDent). Customized abutment designs are shown in Fig. 3A and Fig. 3B. All of the abutments were fixed on the implants with a torque of 15 Ncm-1.
Fig. 3.
Virtually designed customized abutments (Software Cercon art, DeguDent GmbH, Hanau Germany). (A) "short" with a height of 4.31 mm and a taper 4.8° (B) "long" with a height of 6.79 mm and a taper of 4.8°.
The design of the zirconia copings included special hooks on the top of the copings to allow the application of a pull-out force later on. The copings were randomly assigned to subgroups for the various luting agents and cleaning methods.
Evaluated luting agents for the retentive forces of zirconia copings were a provisional (TempBond NE, Kerr, Hamm, Germany) and a semi-permanent (Telio CS Cem Implant, Ivoclar Vivadent, Ellwangen, Germany) cement in combination with three different abutment designs. For the evaluation of the influence of the cleaning method (manually using a curette and gauze, manually in combination with ultrasonic bath (isopropyl alcohol, 30℃, 15 min) and sandblasting with 110 µm aluminium oxide particles (2 bar, 15 s, held at distance of 10 mm) only the provisional cement (TempBond NE, Kerr, Hamm, Germany) on prefabricated titanium abutments (Dentsply Implants Manufacturing GmbH, Mannheim, Germany) was used for both, primary cementation and re-cementation after dislodgement. The provisional luting agent TempBond NE is a non-eugenol zinc-oxide cement. The semi-permanent Telio CS Cem Implant is a dual curing composite cement. Both agents were mixed according to the manufacturer's instructions at room temperature (23℃). Telio CS was delivered in self-mixing cartridges, for TempBond NE the mixture ratio of 1:1 for base and catalyst paste was weighted with a tolerance limit of ±0.1 mg. After seating of the copings onto the abutments a weight of 2.0 kg was applied to the copings for 5 min. When using the composite for luting additionally UV light was applied for 40 s. Before performing the pull-out test each specimen of all series was letting rest for 24 h.
Each coping was pulled off from the abutment in axial direction using a specially fabricated device (Fig. 2) with a universal testing machine (Zwick Z007, Zwick GmbH & Co, Ulm, Germany) at a crosshead speed of 5 mm/min and the dislodgement strength was recorded in Newton using the testing software (TestXpert2, Zwick GmbH & Co, Ulm, Germany).
All specimens were dried for at least 24 h prior to a SEM analysis. The inner surface of one specimen per cleaning technique and one untreated coping as reference was evaluated with a SEM (Quanta 200, FEI, Hillsboro, Or, USA) at a working distance of 10 mm.
Means and 95% confidence intervals were calculated. Statistically significant differences were determined via two-way ANOVA for the test variables "abutment geometry" and "luting agent" and via one-way ANOVA for "cleaning technique". Post hoc tests were performed and adjusted by Dunnett's procedure. The level of significance was set at P=.05. All tests were accomplished using the software SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Significant interactions between abutment geometries and luting agents could be demonstrated (P<.002).
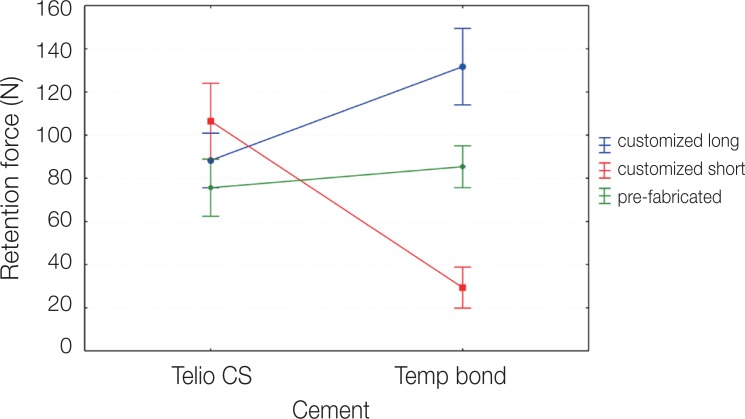
For the pre-fabricated abutments the evaluated retentiveness levels of the luting agents showed no significant difference (P=.2495). Values for Telio CS differed from 44.92 to 104.91 N and for TempBond NE from 62.83 to 111.93 N. Means with standard deviations and the corresponding 95% confidence intervals are demonstrated in Table 1 and Fig. 4.
Table 1.
Means, standard deviations and 95% confidence intervals of retention forces (N) depending on different abutment geometries and luting agents
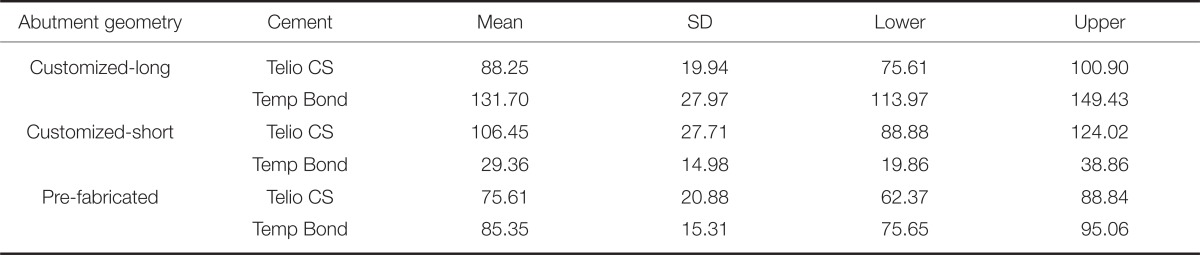
Fig. 4.
Means of retention forces (N) with 95% confidence intervals.
The removal forces of customized-short abutments ranged for Telio CS from 71.87 to 141.00 N. The respective values for the provisional cement TempBond NE were significantly inferior to those of the semi-permanent luting agent (11.20 to 60.45 N, P<.0001). Means with standard deviations and corresponding 95% confidence intervals are also demonstrated in Table 1 and Fig. 4.
In the series of customized-long abutments the effect of the luting agent was inverted relatively to the values of the customized-short series. The retentive strength of TempBond NE ranged from 100.5 to 174.26 N and was significantly superior (P<.0008) to the retentiveness of Telio CS (52.90 to 117.64 N). Means with standard deviations and 95% confidence intervals are shown in Table 1 and Fig. 4. So it can be stated that the effect of the luting agent is not consistent through the series of different abutment geometries.
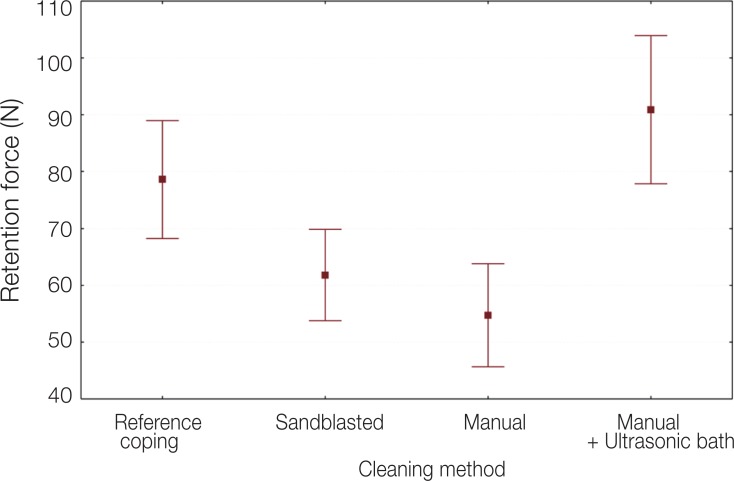
A significant impact of the cleaning technique on the required dislodgement forces could be shown (P<.001).
All specimens within these series were cemented with TempBond NE. The reference series (primary cementation) showed values of retentive forces from 50.36 to 111.93 N. After manual cleaning the retentive strength ranged from 33.66 to 79.29 N. When manual and ultrasonic cleaning was combined increased values of 57.72 to 129.28 N were necessary for dislodgement. After sandblasting of the copings removing forces of 44.49 to 90.82 N have to be applied. Only the combination of manual and ultrasonic cleaning enables retentive forces of TembBond NE after re-cementation comparable to primary cementation (no significant difference, P=.3224). Both, cleaning with hand instruments (P=.003) and sandblasting (P=.0348) showed significantly lower retention forces after re-cementation than the reference group. All means, standard deviations and 95% confidence intervals are shown in Table 2 and Fig. 5.
Table 2.
Means, standard deviations and 95% confidence intervals of retention forces (N) depending on different cleaning methods
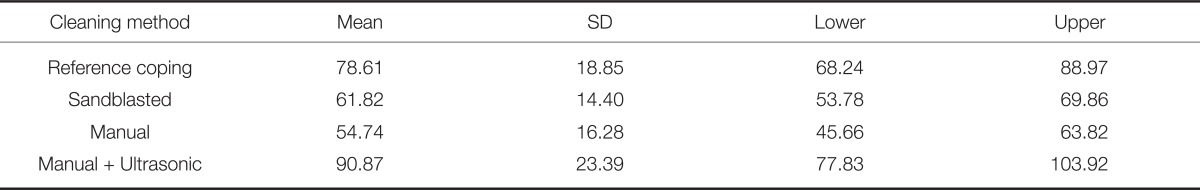
Fig. 5.
Means of retention forces (N) with 95% confidence intervals.
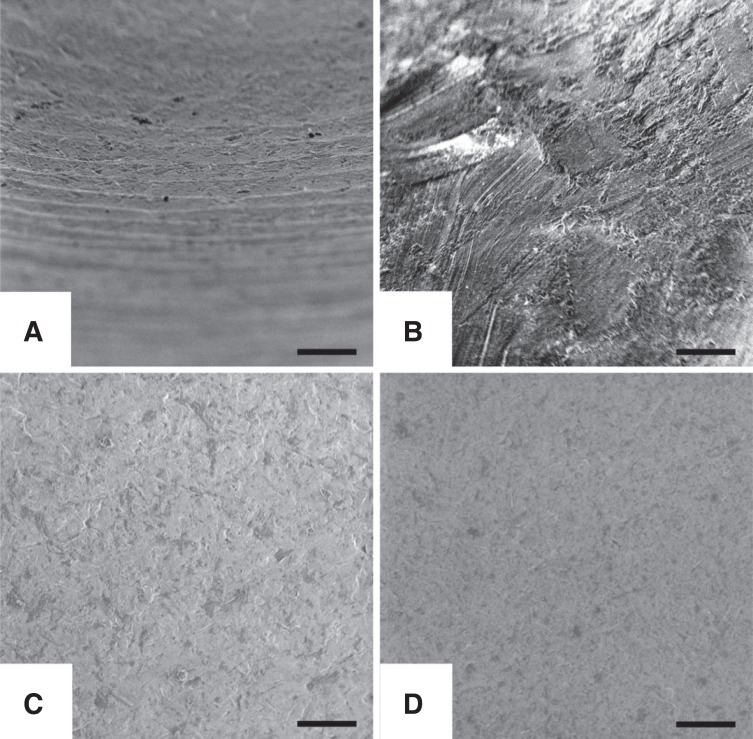
The scanning electron micrograph of the untreated coping (before cementation) shows distinct grinding marks (Fig. 6A). After manual treating with a curette and gauze the specimens show remnants of the cement and scratch marks of the used hand instruments (Fig. 6B). When additionally an ultrasonic bath was used, the surface quality seemed to be more homogenous and cement particles were nearly eliminated (Fig. 6C). After sandblasting all cement particles were completely removed, surface quality could be rated as very homogenous with a slightly increased surface roughness (Fig. 6D).
Fig. 6.
Scanning electron micrographs of the inner surface of zirconia copings. Magnification 400x.
(A) Untreated, (B) After manual treatment using a curette and gauze, (C) After manual treatment and an ultrasonic bath, (D) After sandblasting; Bars: 100 µm.
DISCUSSION
In this study, uni-axial pull-out tests were performed to evaluate retention forces of zirconia copings cemented with a provisional (TempBond NE) and a semi-permanent (Telio CS) luting agent on implant abutments with varying geometries (pre-fabricated, customized-long, customized-short) and different cleaning techniques (manually, manually and ultrasonic bath, sandblasted) prior to re-cementation.
In this study, values for provisionally or semi-permanently cemented zirconia copings on implant abutments between 29.36 N (customized-short abutment, TempBond NE) and 131.70 N (customized-long abutment, TempBond NE) were revealed. These values were consistent to another study investigating retentiveness levels of cobalt-chromium and zirconia copings on implant abutments with varying tapers and surface roughness cemented with definitive and provisional luting agents.21 Another study investigating the retention of zirconia copings on zirconia abutments revealed also comparable values for TempBond NE (around 100 N).25
For customized-long abutments TempBond NE offered the highest retention strength (131.70 N; Telio CS: 88.25 N). But attachment surface and taper seemed to be crucial for the mechanic retention of the provisional luting agent. Another study revealed that retention forces for implant-retained single crowns cemented with TempBond NE was significantly increased by additionally prepared circumferential grooves, supporting the hypothesis that provisional luting is critically effected by abutment geometries.29 However, retention forces when the semi-permanent luting with Telio CS was performed were consistent through all series between 75.61 and 106.45 N, also when height of the abutments was significantly reduced (customized-short). But it has been shown that height of the abutment could significantly influence the retention for of single crowns.30 For customized-short series retentiveness levels of Temp Bond NE were dramatically reduced (29.36 N). Maybe a certain adhesive effect of the resin-based semi-permanent Telio CS compensates unfavorable abutment geometries. However, some specimens of Telio CS were found not adequately hardened after dislodgement although a 24 h phase of drying before the pull-out tests were strictly applied. This could be a possible explanation for the wide range of values and its respective standard deviations (Table 1). But all processes within this study were performed strictly according to the manufacturer's instructions (calibration of the investigators was done during some pilot experiments). Especially variations of the manual mixing processes had to be avoided as far as possible.31 It is known, that besides internal and marginal accuracy of the restorations also the cement space is a determining factor for retentive strength.32 Some studies postulate an insufficient polymerization of resin-based cements when film thickness amounts below 20 µm.33 However, manufacturers of modern luting agents predict film thicknesses around 10 µm due to a good flowability, for example for Telio CS. A recent study demonstrated that retention of implant-supported crowns was significantly increased for a film thickness of 15 µm relatively to 50 µm, especially for resin-based cements.34 In our study, customized-long abutments showed better retentiveness levels than the pre-fabricated ones despite of lower heights (6.79 mm vs. 7.5 mm). Recently, it has been demonstrated that retentiveness levels were significantly affected by abutment heights only when the difference exceeded a moderate amount.35 Maybe the better retention of the customized abutments was caused by the smaller taper degree (4.8° vs. 5.7°) as it was demonstrated in other studies evaluating the retention forces of implant-retained crowns in dependence of different abutment geometries.21,36 But an increased degree of taper seemed to be more effective for solid cements than for provisional luting agents. However accordingly to our previous study it was demonstrated that the provisional luting agent (TempBond NE) was more sensitive regarding retentive strength for varying taper degrees than the semi-permanent cement (Implantlink, Detax, Ettlingen, Germany).21 Another co-factor for better retention forces on customized abutments might be a better precision of fit than for pre-fabricated ones. Customized abutments showed less degree of rotation (<3°)18 between abutment and implant interface than prefabricated ones (>5°)37 but a precise congruence is a crucial factor for the integrity of the whole construction and respective retentiveness levels of the copings.36,38 Due to possible misfit of zirconia-based abutments caused by shrinking processes during sintering, titanium abutments were used in this study. Furthermore, a metal-to-metal interface seemed to be preferable because the increased hardness of zirconia abutments can lead to abrasion of the metal surface of the implant due to micro movements at the interface.39
For evaluation of the efficacy of the cleaning methods only the series of TempBond NE was chosen because remnants of Telio CS were not residual on the copings and could be easily removed in toto from the abutment, which can be seen as clinical advantage because easy and complete removability is useful to prevent peri-implantitis. The investigated cleaning methods were chosen after some pilot-series that formerly included the burnout and edging method. The reference series (dislodgement after primary cementation) revealed values of retentive strength around 78.61 N. After manual cleaning with hand instruments lowest levels of retention (54.74 N) were measured after re-cementation. As seen on SEM (Fig. 6B) there are a lot of cement remnants that possibly inhibited mechanic friction. This is consistent to the results of a study investigating the influence of implant abutment cleaning techniques on retentive strength of zirconia copings.26 The sandblasted copings showed the most homogenous surfaces free of cement's remnants (Fig. 6D), as it was also demonstrated for the cleaning of implant abutments.26 However, sandblasting prior to re-cementation (retentive strength: 61.82 N) leads to values that were better than after manual cleaning but also significantly inferior to those of the reference series. Maybe there was a relevant air abrasion, causing a reduced precision of fit that lead to a less retentive force due to a thicker cement film. Another possible explanation regarding this phenomenon could be that an equalization of the inner surface due to air abrasion reduced the stiction of the cement particles. Results of previous studies regarding the impact of sandblasting on retention forces are inconsistent: it has been demonstrated that there was no significant effect for improving the retentive strength of provisional luting agents25 but otherwise sandblasting has significantly improved retention strength of implant retained single crowns cemented with various provisional and permanent luting agents.35 In addition, the influence of sandblasting on the mechanical integrity of zirconia copings is still unclear and is discussed critically by some authors.27,28 To the author's knowledge comparable investigations are rare. In one study, sandblasting was combined with ultrasonic cleaning for 3 min.40 In our study manual cleaning was combined with an ultrasonic bath for 15 min. The crown retention after combined manual and ultrasonic cleaning was slightly but not significantly increased relatively to dislodgement forces after primary cementation. On the respective SEM (Fig. 6C) a well-cleaned surface of the coping can be clearly identified. Furthermore, it seemed that some zirconia crystallites were separated from the surface, possibly leading to an enlargement of the contact area and better retention.
The uni-axial pull-out test allows functional evaluation of various impact factors on retention forces of dental restorations. In this study, no thermocycling or water storage was performed. This must be seen critically regarding the transferability of our in vitro results directly to clinical situations. It has been shown that thermocycling could be a crucial factor for determining the retentive strength of TempBond NE.21,25,30 The uni-axial test is also limited in representing adequate clinical situations because naturally multidirectional forces were applied on restorations and implants during mastication or bruxism. Therefore, conclusions regarding clinical implementation have to be drawn carefully.
CONCLUSION
Considering the conditions and limitations of this in vitro study, the following conclusions can be drawn:
The provisional luting agent (TempBond NE) was more affected by different heights and tapers of the abutment. Therefore, semi-permanent luting agents should be used when adequate geometries of the abutments cannot be realized.
The combination of manual and ultrasonic cleaning for temporarily cemented, debonded zirconia copings seemed to be an adequate and clinically feasible procedure to obtain retention forces for re-cementation comparable to primary luting.
Footnotes
The authors would like to thank DeguDent GmbH, Hanau, Germany for supporting this study.
References
- 1.Heydecke G, Kohal R, Gläser R. Optimal esthetics in single-tooth replacement with the Re-Implant system: a case report. Int J Prosthodont. 1999;12:184–189. [PubMed] [Google Scholar]
- 2.Sailer I, Zembic A, Jung RE, Hämmerle CH, Mattiola A. Single-tooth implant reconstructions: esthetic factors influencing the decision between titanium and zirconia abutments in anterior regions. Eur J Esthet Dent. 2007;2:296–310. [PubMed] [Google Scholar]
- 3.Fischer H, Karaca F, Marx R. Detection of microscopic cracks in dental ceramic materials by fluorescent penetrant method. J Biomed Mater Res. 2002;61:153–158. doi: 10.1002/jbm.10148. [DOI] [PubMed] [Google Scholar]
- 4.Guess PC, Att W, Strub JR. Zirconia in fixed implant prosthodontics. Clin Implant Dent Relat Res. 2012;14:633–645. doi: 10.1111/j.1708-8208.2010.00317.x. [DOI] [PubMed] [Google Scholar]
- 5.Rekow ED, Silva NR, Coelho PG, Zhang Y, Guess P, Thompson VP. Performance of dental ceramics: challenges for improvements. J Dent Res. 2011;90:937–952. doi: 10.1177/0022034510391795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larsson C, Wennerberg A. The clinical success of zirconia-based crowns: a systematic review. Int J Prosthodont. 2014;27:33–43. doi: 10.11607/ijp.3647. [DOI] [PubMed] [Google Scholar]
- 7.Kohorst P, Junghanns J, Dittmer MP, Borchers L, Stiesch M. Different CAD/CAM-processing routes for zirconia restorations: influence on fitting accuracy. Clin Oral Investig. 2011;15:527–536. doi: 10.1007/s00784-010-0415-9. [DOI] [PubMed] [Google Scholar]
- 8.Beuer F, Naumann M, Gernet W, Sorensen JA. Precision of fit: zirconia three-unit fixed dental prostheses. Clin Oral Investig. 2009;13:343–349. doi: 10.1007/s00784-008-0224-6. [DOI] [PubMed] [Google Scholar]
- 9.Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77:28–35. doi: 10.1016/s0022-3913(97)70203-8. [DOI] [PubMed] [Google Scholar]
- 10.Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants. 2003;18:719–728. [PubMed] [Google Scholar]
- 11.Torrado E, Ercoli C, Al Mardini M, Graser GN, Tallents RH, Cordaro L. A comparison of the porcelain fracture resistance of screw-retained and cement-retained implant-supported metal-ceramic crowns. J Prosthet Dent. 2004;91:532–537. doi: 10.1016/j.prosdent.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Brägger U, Karoussis I, Persson R, Pjetursson B, Salvi G, Lang N. Technical and biological complications/failures with single crowns and fixed partial dentures on implants: a 10-year prospective cohort study. Clin Oral Implants Res. 2005;16:326–334. doi: 10.1111/j.1600-0501.2005.01105.x. [DOI] [PubMed] [Google Scholar]
- 13.Sherif S, Susarla SM, Hwang JW, Weber HP, Wright RF. Clinician- and patient-reported long-term evaluation of screw- and cement-retained implant restorations: a 5-year prospective study. Clin Oral Investig. 2011;15:993–999. doi: 10.1007/s00784-010-0460-4. [DOI] [PubMed] [Google Scholar]
- 14.Breeding LC, Dixon DL, Bogacki MT, Tietge JD. Use of luting agents with an implant system: Part I. J Prosthet Dent. 1992;68:737–741. doi: 10.1016/0022-3913(92)90194-f. [DOI] [PubMed] [Google Scholar]
- 15.Park JI, Lee Y, Lee JH, Kim YL, Bae JM, Cho HW. Comparison of fracture resistance and fit accuracy of customized zirconia abutments with prefabricated zirconia abutments in internal hexagonal implants. Clin Implant Dent Relat Res. 2013;15:769–778. doi: 10.1111/j.1708-8208.2011.00426.x. [DOI] [PubMed] [Google Scholar]
- 16.Jung RE, Holderegger C, Sailer I, Khraisat A, Suter A, Hämmerle CH. The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: a randomized controlled clinical trial. Int J Periodontics Restorative Dent. 2008;28:357–365. [PubMed] [Google Scholar]
- 17.Blatz MB, Bergler M, Holst S, Block MS. Zirconia abutments for single-tooth implants-rationale and clinical guidelines. J Oral Maxillofac Surg. 2009;67:74–81. doi: 10.1016/j.joms.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 18.Vigolo P, Fonzi F, Majzoub Z, Cordioli G. An in vitro evaluation of titanium, zirconia, and alumina procera abutments with hexagonal connection. Int J Oral Maxillofac Implants. 2006;21:575–580. [PubMed] [Google Scholar]
- 19.Zembic A, Sailer I, Jung RE, Hämmerle CH. Randomized-controlled clinical trial of customized zirconia and titanium implant abutments for single-tooth implants in canine and posterior regions: 3-year results. Clin Oral Implants Res. 2009;20:802–808. doi: 10.1111/j.1600-0501.2009.01717.x. [DOI] [PubMed] [Google Scholar]
- 20.Bresciano M, Schierano G, Manzella C, Screti A, Bignardi C, Preti G. Retention of luting agents on implant abutments of different height and taper. Clin Oral Implants Res. 2005;16:594–598. doi: 10.1111/j.1600-0501.2005.01159.x. [DOI] [PubMed] [Google Scholar]
- 21.Schiessl C, Schaefer L, Winter C, Fuerst J, Rosentritt M, Zeman F, Behr M. Factors determining the retentiveness of luting agents used with metal- and ceramic-based implant components. Clin Oral Investig. 2013;17:1179–1190. doi: 10.1007/s00784-012-0798-x. [DOI] [PubMed] [Google Scholar]
- 22.Bernal G, Okamura M, Muñoz CA. The effects of abutment taper, length and cement type on resistance to dislodgement of cement-retained, implant-supported restorations. J Prosthodont. 2003;12:111–115. doi: 10.1016/S1059-941X(03)00006-8. [DOI] [PubMed] [Google Scholar]
- 23.Zidan O, Ferguson GC. The retention of complete crowns prepared with three different tapers and luted with four different cements. J Prosthet Dent. 2003;89:565–571. doi: 10.1016/s0022-3913(03)00182-3. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y, Yamashita J, Shotwell JL, Chong KH, Wang HL. The comparison of provisional luting agents and abutment surface roughness on the retention of provisional implant-supported crowns. J Prosthet Dent. 2006;95:450–455. doi: 10.1016/j.prosdent.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Kokubo Y, Kano T, Tsumita M, Sakurai S, Itayama A, Fukushima S. Retention of zirconia copings on zirconia implant abutments cemented with provisional luting agents. J Oral Rehabil. 2010;37:48–53. doi: 10.1111/j.1365-2842.2009.02013.x. [DOI] [PubMed] [Google Scholar]
- 26.Keum EC, Shin SY. A comparison of retentive strength of implant cement depending on various methods of removing provisional cement from implant abutment. J Adv Prosthodont. 2013;5:234–240. doi: 10.4047/jap.2013.5.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frankenberger R, Krämer N, Sindel J. Repair strength of etched vs silica-coated metal-ceramic and all-ceramic restorations. Oper Dent. 2000;25:209–215. [PubMed] [Google Scholar]
- 28.Chintapalli RK, Mestra Rodriguez A, Garcia Marro F, Anglada M. Effect of sandblasting and residual stress on strength of zirconia for restorative dentistry applications. J Mech Behav Biomed Mater. 2014;29:126–137. doi: 10.1016/j.jmbbm.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Lewinstein I, Block L, Lehr Z, Ormianer Z, Matalon S. An in vitro assessment of circumferential grooves on the retention of cement-retained implant-supported crowns. J Prosthet Dent. 2011;106:367–372. doi: 10.1016/S0022-3913(11)60149-2. [DOI] [PubMed] [Google Scholar]
- 30.Mehl C, Harder S, Shahriari A, Steiner M, Kern M. Influence of abutment height and thermocycling on retrievability of cemented implant-supported crowns. Int J Oral Maxillofac Implants. 2012;27:1106–1115. [PubMed] [Google Scholar]
- 31.Caughman WF, Chan DC, Rueggeberg FA. Curing potential of dual-polymerizable resin cements in simulated clinical situations. J Prosthet Dent. 2001;85:479–484. doi: 10.1067/mpr.2001.114842. [DOI] [PubMed] [Google Scholar]
- 32.Son YH, Han CH, Kim S. Influence of internal-gap width and cement type on the retentive force of zirconia copings in pullout testing. J Dent. 2012;40:866–872. doi: 10.1016/j.jdent.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Ernst CP, Wenzl N, Stender E, Willershausen B. Retentive strengths of cast gold crowns using glass ionomer, compomer, or resin cement. J Prosthet Dent. 1998;79:472–476. doi: 10.1016/s0022-3913(98)70164-7. [DOI] [PubMed] [Google Scholar]
- 34.Mehl C, Harder S, Steiner M, Vollrath O, Kern M. Influence of cement film thickness on the retention of implant-retained crowns. J Prosthodont. 2013;22:618–625. doi: 10.1111/jopr.12058. [DOI] [PubMed] [Google Scholar]
- 35.Cano-Batalla J, Soliva-Garriga J, Campillo-Funollet M, Munoz-Viveros CA, Giner-Tarrida L. Influence of abutment height and surface roughness on in vitro retention of three luting agents. Int J Oral Maxillofac Implants. 2012;27:36–41. [PubMed] [Google Scholar]
- 36.Enkling N, Ueda T, Gholami H, Bayer S, Katsoulis J, Mericske-Stern R. Precision of fit and retention force of cast non-precious-crowns on standard titanium implant-abutment with different design and height. Clin Oral Implants Res. 2014;25:451–457. doi: 10.1111/clr.12167. [DOI] [PubMed] [Google Scholar]
- 37.Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont. 1996;9:149–160. [PubMed] [Google Scholar]
- 38.Cibirka RM, Nelson SK, Lang BR, Rueggeberg FA. Examination of the implant-abutment interface after fatigue testing. J Prosthet Dent. 2001;85:268–275. doi: 10.1067/mpr.2001.114266. [DOI] [PubMed] [Google Scholar]
- 39.Binon PP. Implants and components: entering the new millennium. Int J Oral Maxillofac Implants. 2000;15:76–94. [PubMed] [Google Scholar]
- 40.Attia A, Lehmann F, Kern M. Influence of surface conditioning and cleaning methods on resin bonding to zirconia ceramic. Dent Mater. 2011;27:207–213. doi: 10.1016/j.dental.2010.10.004. [DOI] [PubMed] [Google Scholar]