Abstract
Visceral Leishmaniasis has been showing remarkable epidemiological changes in recent decades, with marked expansion and an emergence of cases in urban areas of the North, Southeast and Midwest regions of Brazil. The Kala-azar cases reported here, despite being very characteristic, presented a great difficulty of diagnosis, because the disease is not endemic in Volta Redonda. The child underwent two hospitalizations in different hospitals, but got the correct diagnosis only after 11 months of symptom onset. In this report we discuss the main differential diagnoses and call attention to the suspected symptoms of visceral leishmaniasis in patients with prolonged fever, hepatosplenomegaly and pancytopenia, even in areas not traditionally endemic for the disease.
Keywords: Visceral Leishmaniasis, Kala-azar, Epidemiology, Rio de Janeiro
Abstract
A leishmaniose visceral vem apresentando mudanças epidemiológicas marcantes nas últimas décadas, com acentuada expansão e surgimento de casos em áreas urbanas do Norte, Sudeste e Centro-Oeste do Brasil. O caso de Calazar aqui relatado, apesar de ser muito característico, apresentou grande dificuldade de diagnóstico, por se tratar de doença não-endêmica em Volta Redonda. A criança passou por duas internações em hospitais diferentes, porém, só obteve o diagnóstico correto após 11 meses do início dos sintomas. Neste relato são discutidos os principais diagnósticos diferenciais e chama-se a atenção de sempre considerar a hipótese de leishmaniose visceral em todo paciente com febre prolongada, hepatoesplenomegalia e pancitopenia, mesmo em áreas tradicionalmente não endêmicas.
INTRODUCTION
Visceral Leishmaniasis (VL) remains an important public health problem worldwide with an estimated annual incidence of 500,000 cases and 50,000 deaths16. In Brazil, a marked expansion of the disease in the last decades has been observed, particularly in the North, Southeast and Midwest country regions4,5,7. In the state of Rio de Janeiro (RJ), the occurrence of human cases is sporadic, with most reports concentrated in the city of Rio de Janeiro, relating to conditions of poverty and deforestation of protected areas7. The city of Volta Redonda is located in the Médio Paraíba area, South Fluminense region and 120 km from the capital. It has 260,000 inhabitants. The steel industry and the service sector are the most important economic activities, creating migration flows that contribute to uncontrolled growth and occupation of previous rural areas around the urban center13.
The objective of this report is to draw the attention of clinicians and pediatricians and ensure they always include the diagnosis of VL in every patient with prolonged fever and hepatosplenomegaly.
CASE REPORT
LGD, 5 years old, white, male, born in Volta Redonda, resident in Jardim Belmonte. In September 2011 he was admitted to the pediatric ward of the Municipal Hospital São João Batista (MHSJB) with a reported fever and enlarged abdomen that he had had for 15 days, associated with cough, weight loss and poor general condition. His previous medical records showed earlier hospitalization, from November 2010 to January 2011 at another hospital in the municipality with the same symptoms. At his first hospital admission, the patient developed neutropenia and sepsis and was transferred to the intensive care unit (ICU). Initially, the following possible diagnoses were investigated: leukemia, lymphoma, AIDS, tuberculosis, hepatitis, toxoplasmosis, cytomegalovirus infection, infectious mononucleosis, typhoid fever and the juvenile form of paracoccidioidomycosis. Various antimicrobial agents were used, including amphotericin B deoxycholate for 15 days. According to the medical records, the final hypothesis at the patient's discharge was cat-scratch disease. All tests were initially negative (specific serology, tuberculin test, microscopy of gastric contents for AFB, fecal culture, bone marrow microscopy, cervical lymph node biopsy). The hypothesis of VL came to be considered, although no confirmatory test was requested at the time. In epidemiological history, the child's mother denied a history of travel outside the RJ.
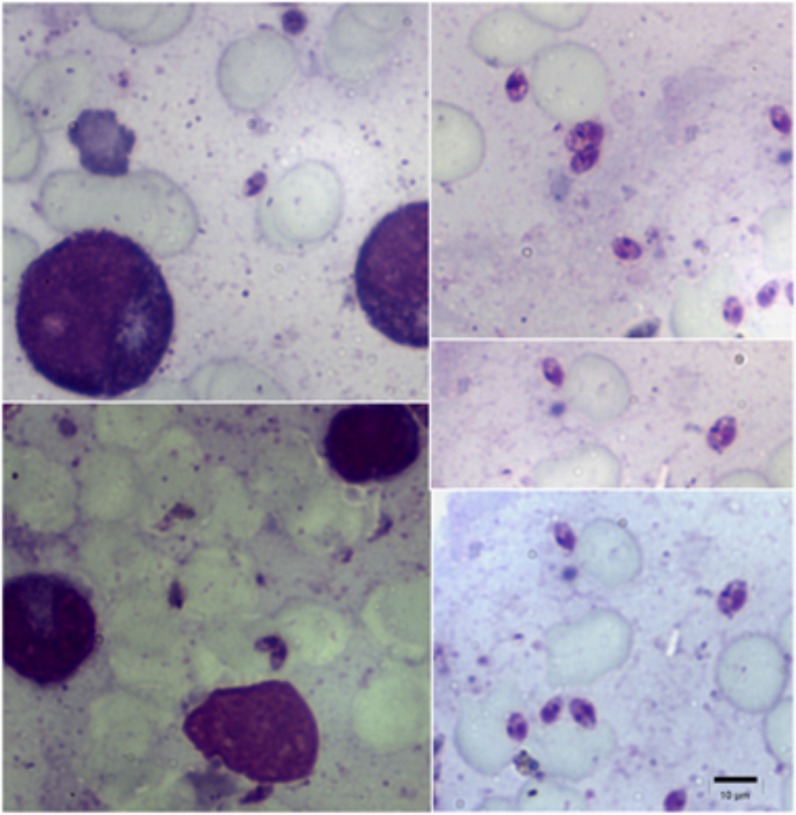
The physical examination at admission in the pediatric ward of MHSJB showed that patient had lost 14 kg weight, had pallor, dehydration, presence of lymphadenopathy in small chains of cervical area and massive hepatosplenomegaly (Fig. 1). The diagnosis of leukemia and sepsis were initially suspected and intravenous hydration and cefepime was started, new laboratory tests and the hematology department were called. The initial blood count showed 3.64 million erythrocytes, hemoglobin 7.3 g%, hematocrit 25.5%, total leukocyte count 3,800, with 14% neutrophils and platelets 93,000. Total protein 6.7g/dL, 2.2g and 4.5g albumin and globulin levels respectively. Serology for HIV, syphilis, hepatitis, toxoplasmosis and cytomegalovirus were negative. The chest radiography was normal. The myelogram showed normal cellularity and relationship in the series myeloid/erythroid and lymphocytic/megakaryocytic but no search of parasites in bone marrow was conducted in the first instance. After seven days of hospitalization, the child had two daily peaks of fever, his general condition had worsened and a WBC with 836 granulocytes. It was then decided to associate vancomycin to the initial antimicrobial therapy. Finally the infectious diseases were called and visceral leishmaniasis was suspected, with the recommendation to repeat bone marrow aspirate to search for Leishmania spp. Blood cultures were negative for bacteria. On the 15th day of hospitalization, we performed computed tomography of the abdomen which revealed that the liver was 13 cm of the diaphragm and the spleen measured 17 cm in length. A new bone marrow aspirate was performed and the new material sent to the Laboratory for Leishmaniasis Surveillance Evandro Chagas Clinical Research Institute, Oswaldo Cruz Foundation in Rio de Janeiro. After Giemsa staining of the material, the presence of numerous amastigotes of Leishmania spp. was proven (Fig. 2).
Fig. 1. LGD, 5 years, with massive hepatosplenomegaly.

Fig. 2. Photomicrographs of bone marrow aspirate stained with Giemsa showing numerous amastigote forms of Leishmania spp. (1000x).
The patient was treated initially with pentavalent antimony (antimony N-methyl glucamine) at a dose of 20 mg/kg/day intravenously. After 10 days of use of antimony, as the daily fever remained, it was replaced by amphotericin B deoxycholate. The patient evolved with remission of fever and general improvement; however, he began to show severe hypokalemia, despite intravenous potassium replacement and full-dose regimen of amphotericin B on alternate days. We chose to replace the amphotericin B deoxycholate for liposomal formulation, which was used for more seven days at a dose of 3 mg/kg/day. A blood work done 46 days after admission depicted an improvement towards normal with hematocrit 31%, hemoglobin 10.4 g/%, total leukocyte count 4,400 (64% neutrophils and 43% lymphocytes), platelets 224,000, albumin 3.7g and globulin 2.6 g. The patient was then discharged for outpatient monitoring.
DISCUSSION
The VL has undergone marked epidemiological changes in recent decades. Initially characterized as an anthropozoonosis typical disease from rural areas of the Northeast, since the 1980s, an expansion to the urban areas of large and medium cities in the Midwest, Southeast and North Brazil4,5,7 has been recorded. The disease is mainly prevalent in male children and in children under 10 years old4,6,12. The city of Volta Redonda has never registered cases of VL, which probably hindered the initial clinical diagnosis on admission. The child was left for 11 months without the correct diagnosis. In non-endemic areas, it is recommended to include the diagnosis of VL in all cases of patients with fever and splenomegaly right after other possibilities, more prevalent in the region, are elucidated4. Since the beginning it was observed that the child had, in addition to clinical signs, laboratory abnormalities characteristic of the disease, such as pancytopenia, hypoalbuminemia and hyperglobulinemia4,6,12. In his initial hospitalization, we cannot rule out the possibility of bacterial sepsis co-existence, since he improved after ICU admission and use of broad-spectrum antimicrobial. It should be noted that the child made use of amphotericin B deoxycholate for 15 days in its passage through the ICU, which may have contributed to the initial improvement. However, the cumulative dose was lower than recommended to treat the VL, causing the worsening of the disease few months later4.
In the acute phase of VL the main differential diagnoses are infectious mononucleosis, toxoplasmosis and cytomegalovirus infection6. All these possibilities were investigated and had negative tests. In the classic presentation with massive hepatosplenomegaly, the VL can be confused with malaria, typhoid, schistosomiasis, prolonged course of enteric bacterial infection and myeloproliferative disorders6,9. Although it presents with fever, cat-scratch disease has, in most cases, a benign course, with involvement of the skin and local lymph nodes, not being included in the differential diagnosis of VL2,3,6,9. The involvement of the liver and spleen is rare and, if affected, they can show abscesses and have considerably less growth2,3. Different from kala-azar, cat-scratch disease shows no increase in the total number of leukocytes and neutrofilia2.
Other possible diagnosis for this case was acute lymphocytic leukemia, the most common type in childhood, lymphoblasts can be seen in peripheral blood and bone marrow examination, but this was not observed in this case1. Lymphomas are rare in childhood and typically include more prominent lymph node enlargement, sometimes with mediastinal involvement1. The severe form of lymphoma shows atypical lymphocytes in the lymph nodes and bone marrow, which was not seen in the tests of the patient described here1. It is very unlikely that the possibility of the prolonged course of enteric bacterial infection, since schistosomiasis is not endemic in Volta Redonda10. The child underwent several courses of antibiotics and reported no travel outside the state. The splenomegaly and anemia in typhoid fever are usually less intense and there was no elevation of serum globulins6. Malaria is not considered endemic in Volta Redonda and the few reports by the municipality health team are imported8. Although rare in this age group, we must consider the possibility of the juvenile form of paracoccidioidomycosis, often evidenced in the Médio Paraíba, South Fluminense14. However, lymph node enlargement in the acute phase is usually bulkier and often drains spontaneously through cutaneous fistula. The enlargement in the liver and spleen is less pronounced in the paracoccidioidomycosis. Furthermore we do not observe pancytopenia and neutrophils count tends to be high. The mycological exam of the cervical lymph node biopsy in first hospitalization would have confirmed the diagnosis15.
Hypokalemia is a frequent adverse effect of the prolonged use of amphotericin B, which was observed in this case11. The resistance to pentavalent antimony in the treatment of VL has been documented in India and Africa, a phenomenon that has also been observed in Brazil6. In the latest report of leishmaniasis control from the World Health Organization, liposomal amphotericin B is indicated as an initial drug for the treatment of VL in South America, this opposes the recommendations adopted by the Ministry of Health of Brazil, that indicates antimony as the initial drug of choice4,5,16. New research is needed to better assess this issue.
According to information from the environmental surveillance department in the municipality of Volta Redonda, there were recently captured specimens of Lutzomyia longipalpis in the neighborhood of Eucaliptal, next to the Jardim Belmonte, residence address of the patient described. Control measures and identification of infected dogs have been made since then to contain the spread of the disease in the region.
Finally, we emphasize the importance of always investigating VL in patients presenting with clinical signs characteristic of the disease, even in non-endemic areas, thus carrying out an early diagnosis and reducing the lethality of the disease.
ACKNOWLEDGMENTS
We thank Dr. Clarisse Bressan for her collaboration in the translation of the text into the English language.
REFERENCES
- 1.Adamson JW. Harrison's principles of internal medicine. 17th ed. New York: McGraw-Hill Medical; 2008. Malignancies of lymphoid cells; p. chap. 105. [Google Scholar]
- 2.Arisoy ES, Correa AG, Wagner ML, Kaplan SL. Hepatosplenic cat-scratch disease in children: select clinical features and treatment. Clin Infect Dis. 1999;28:778–84. doi: 10.1086/515197. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Ami R, Ephros M, Avidor B, Katchman E, Varon M, Leibowitz C, et al. Cat-scratch disease in elderly patients. Clin Infect Dis. 2005;41:969–74. doi: 10.1086/432934. [DOI] [PubMed] [Google Scholar]
- 4.Brasil . Manual de vigilância e controle da leishmaniose visceral. Brasília: Ministério da Saúde; 2006. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. [Google Scholar]
- 5.Brasil . Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Guia de vigilância epidemiológica: Leishmaniose visceral. 7ª ed. Brasília: Ministério da Saúde; 2009. [Google Scholar]
- 6.Duarte MIS, Badaró RS. Leishmaniose Visceral (Calazar) In: Veronesi R, Focaccia R, editors. Tratado de infectologia. 4ª ed. v. 2. São Paulo: Atheneu; 2010. pp. 1707–36. [Google Scholar]
- 7.Marzochi MC, Fagundes A, Andrade MV, Souza MB, Madeira MF, Mouta-Confort E, et al. Visceral leishmaniasis in Rio de Janeiro, Brazil: eco-epidemiological aspects and control. Rev Soc Bras Med Trop. 2009;42:570–80. doi: 10.1590/s0037-86822009000500017. [DOI] [PubMed] [Google Scholar]
- 8.Miguel RB. Estudo da infecção por Plasmodium spp no município de Guapimirim, estado do Rio de Janeiro. [Dissertação] Rio de Janeiro: Instituto Oswaldo Cruz, Fundação Oswaldo Cruz; 2011. [Google Scholar]
- 9.Nascimento EL, Medeiros IM. Rotinas de diagnóstico e tratamento das doenças infecciosas e parasitárias. 3ª ed. São Paulo: Atheneu; 2012. Leishmaniose visceral (Calazar) pp. 695–701. [Google Scholar]
- 10.Prata A. Esquistossomose mansônica. In: Veronesi R, Focaccia R, editors. Tratado de infectologia. 4ª ed. v. 2. São Paulo: Atheneu; 2010. pp. 1859–82. [Google Scholar]
- 11.Prentice HG, Hann IM, Herbrecht R, Aoun M, Kvaloy S, Catovsky D, et al. A randomized comparison of liposomal versus conventional amphotericin B for the treatment of pyrexia of unknown origin in neutropenic patients. Br J Haematol. 1997;98:711–8. doi: 10.1046/j.1365-2141.1997.2473063.x. [DOI] [PubMed] [Google Scholar]
- 12.Queiroz MJ, Alves JG, Correia JB. Leishmaniose visceral: características clínico-epidemiológicas em crianças de área endêmica. J Pediatr. 2004;80:141–6. [PubMed] [Google Scholar]
- 13.Rio de Janeiro (Estado) Tribunal de Contas. Secretaria-Geral de Planejamento. Estudo Socioeconômico 2007: Volta Redonda: histórico e caracterização do município. Rio de Janeiro: Tribunal de Contas; 2007. [Google Scholar]
- 14.Rios Gonçalves AJ, Londero AT, Terra GM, Rozenbaum R, Abreu TF, Nogueira AS. Paracoccidioidomycosis in children in the state of Rio de Janeiro (Brazil). Geographic distribution and the study of a “reservarea”. Rev Inst Med Trop Sao Paulo. 1998;40:11–4. doi: 10.1590/s0036-46651998000100003. [DOI] [PubMed] [Google Scholar]
- 15.Rios Gonçalves AJ, Terra GM, Passioni LF. Paracoccidioidomicose infanto-juvenil: relato de dez pacientes recentemente observados na cidade do Rio de Janeiro. Revisão da literatura. Rev Med HSE. 2000;34 Available from: http://www.hse.rj.saude.gov.br/profissional/revista/34/parac.asp. [Google Scholar]
- 16.World Health Organization . Control of the leishmaniases. (Technical Report Series; 949) Geneva: WHO; 2010. [PubMed] [Google Scholar]