Abstract
Study Design and Objective:
The author reports experience with treatment of degenerative lumbar canal stenosis that involved fixation-arthrodesis of the affected spinal segment using “double insurance” transarticular screws for each joint. No direct bone, ligament or disc resection is done for decompression of the spinal dural tube or root canal.
Methods and Summary of Background Data:
During the period March 2011-September 2011, seven patients having lumbar canal stenosis were treated with a modification of transarticular method of screw fixation that involved insertion of two or “double insurance” screws at each articular joint. The operation involved section of the spinous process at its base, opening up of the facet joint, denuding of articular cartilage, insertion of intra-articular bone graft and insertion of two transarticular screws at each facet joint. The fixation was done in four levels in two patients, at three levels in four patients and at two levels in one patient. Oswestry disability index and visual analog scale were used to clinically assess the patients before and after the surgery and at follow-up.
Results:
During the average period of follow-up of 26.9 months (range 24-30 months), there was varying degree of recovery of symptoms. The procedure resulted in firm stabilization and fixation of the spinal segment and provided a ground for arthrodesis. During the period of follow-up, one patient underwent re-exploration and decompressive laminectomy as she continued to have significant pain symptom.
Conclusions:
Vertical instability and telescoping, listhesis or overriding of the facets on physical activity seems to be the defining phenomenon in the pathogenesis of lumbar canal stenosis. The clinical outcome in our patients suggest that fixation of the spinal segment can be a rationale form of treatment. “Double insurance” transarticular method of treatment is a simple, safe, and effective method of spinal stabilization.
Keywords: Facet joint, lumbar canal stenosis, transarticular screws
INTRODUCTION
In this report, we present our experience and results of treatment of lumbar canal stenosis that involved only fixation of the involved segments of the lumbar spine using two interarticular screws or “double insurance” screws for each joint. The proposed treatment is based on the hypothesis that “vertical instability” that results in telescoping of the facets on physical activity forms the basis of pathogenesis of lumbar canal stenosis.[1,2,3,4] The operation aims at arthrodesis of the affected spinal segments.[5] Fixation of the segments resulted in immediate postoperative and lasting relief from symptoms. The rationale of treatment is presented and the literature on the subject has been briefly reviewed.
MATERIALS AND METHODS
During the period March 2011-September 2011, we treated seven cases of lumbar degenerative spinal disease using the proposed technique. These patients were analyzed prospectively. There were four males and three female patients and their ages ranged from 50 to 65 years (average 56 years). The clinical symptoms at the time of presentation are elaborated in Table 1. The patients had characteristic lumbar degenerative disease that resulted in manifestations of lumbar canal stenosis. All patients had characteristic claudication pain on walking for a distance. No patient had any focal neurological deficits. The patients had progressive symptoms, and failure of nonoperative management. Patients having an acute disc herniation or an extruded disc fragment were not included. Patients having manifest instability on dynamic imaging that resulted in any degree of spondylolisthesis were excluded. All patients were investigated with dynamic (flexion and extension views) plain radiography, computerized tomography scan and magnetic resonance imaging before and after surgery [Figures 1 and 2]. One patient underwent a two level, four patients underwent three level and two patients underwent a four-level treatment. The presenting clinical symptoms, radiological features and the outcome are enumerated in Tables 1–3. Oswestry disability index (ODI)[6] and visual analog score (VAS)[7] were used to evaluate the patients before and after surgery and at last follow-up. All radiographic measurements were taken with back in a neutral position. The radiographic analyses that were performed included assessment of bone fusion and status of the spinal canal dimensions.
Table 1.
The presenting clinical and radiological features
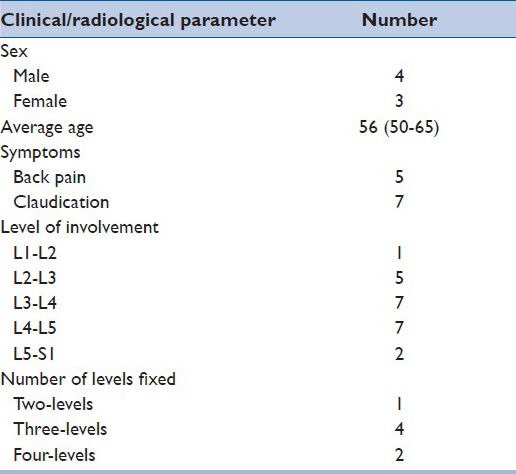
Figure 1.
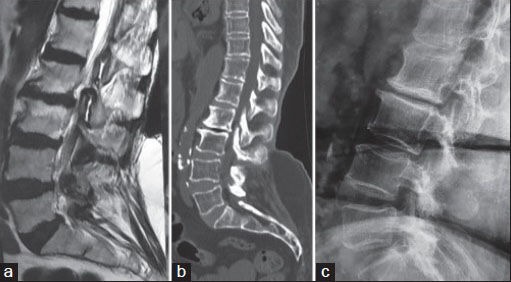
Preoperative images of a 65-year-old female. (a) Sagittal T2 weighted magnetic resonance imaging image showing features of lumbar canal stenosis. (b) Sagittal computerized tomography image showing lumbar canal stenosis. (c) Lateral X-ray
Figure 2.
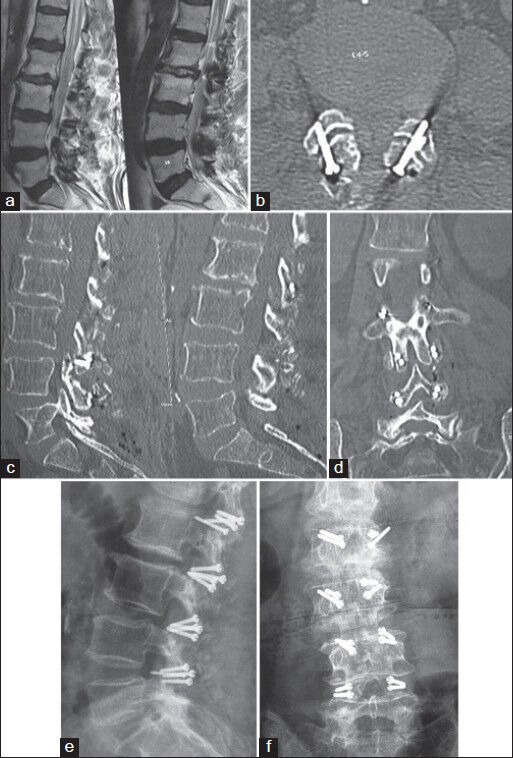
Postoperative images. (a) Sagittal magnetic resonance imaging showing unbuckling of the ligamentum flavum and reduction of the dural compression. (b) Axial computerized tomography image showing the transfacetal screws. (c) Sagittal computerized tomography image showing the screws. (d) Coronal computerized tomography image showing the double insurance screw fixation. (e) Lateral X-ray of the lumbar spine showing the four level fixation. (f) Antero-posterior X-ray of the lumbar spine showing the screws
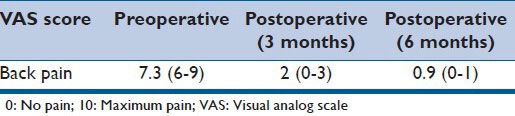
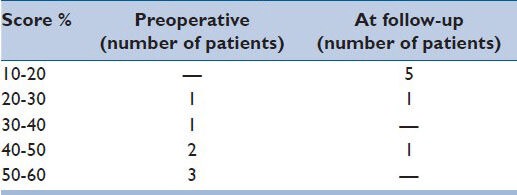
Table 3.
VAS
Operative technique
The patient was placed in the standard prone position that flattened the lumbar lordosis. Midline incision was taken and by employing sub-periosteal dissection the articular joints were exposed widely on both sides. The spinal level of the surgery was confirmed with the help of intra-operative fluoroscopy. Based on our experience in dealing with facets and articular joints, the facets having clear evidence of “instability” and excessive abnormal movements on direct visual and manual inspection were considered suitable for the proposed operation. These findings were valuable and were correlated with clinical symptoms and findings on images, whilst considering the levels and extent of fixation. The interspinous-process ligaments are widely removed. Spinous process is sectioned along its base and was shredded into small pieces. The articular capsule was opened and the facets were distracted using varying sizes of osteotomes that were introduced with their flat-sharp edge and then turned 90° to affect distraction. Essentially, the distraction involved superior elevation of the facet of the rostral vertebra. The articular capsule and end plate cartilage was widely denuded using screwing motion of the osteotome and whenever necessary using micro-drill. Bone graft pieces harvested from the spinous process were jammed into the articular cavity. Transarticular screw insertion was then done under direct vision on the superior and inferior halves of joint. The sectioning of the spinous process provided an inferior and direct angle for insertion of the screws. After the screw insertion, bone graft pieces are placed over the appropriately prepared host bone area of laminae. The patient is then advised bed rest for a period of 8 weeks and only minor activities were permitted during this time with lumbar restraint. After this period, and confirmation of spinal fusion, all routine activities were permitted.
RESULTS
The follow-up period ranged from 24 to 30 months, average being 26.9 months. Neurological and radiographic assessments were performed by observers independent of the principal surgeon. The clinical outcome of surgery is elaborated in Tables 2 and 3. There was no incidence of misplacement or dislodgement of the implant. Six patients improved in symptoms following surgery to varying extent. The degree of improvement was monitored as per the ODI and VAS and is elaborated in Tables 2 and 3. The evaluation included the location and degree of preoperative and postoperative pain using an analog scale. In one patient, significant pain persisted in the low back, but the character was not of claudication type and the degree of pain appeared shade less then preoperative pain. Decompressive laminectomy was done on her 12 months after the first operation. All other patients are satisfied with the surgery and are back into their preoperative profession. In none of the other cases, the operation was repeated or any additional surgical maneuver done on the same surgical level or at any other lumbar spinal level. There was no implant related complication. Fusion of the spinal segment was defined when there was clear radiological evidence of bone fusion across the facets and when there was the absence of all kinds of motion and alterations in the interlaminar and intervertebral body distances on flexion-extension X-ray films done at a follow-up of at-least 6 months. Bone formation was observed within and over the facet joint. As per this criterion, successful fusion was obtained in all the treated spinal levels.
Table 2.
Oswestry disability index
DISCUSSION
Lumbar canal stenosis has been treated by a variety of nonsurgical and surgical methods. Lumbar traction and lumbosacral belts have been employed effectively for a long time. Decompression of lumbar spinal canal by laminectomy has stood the test of time, is still considered to be a Gold standard in treatment and is employed by most surgeons. Bone preserving or saving methods have recently found favor. Spinous process[8,9] and laminar distraction[10] techniques using specially designed implants are currently gaining increasing popularity. We recently described facetal distraction as an option for the treatment of lumbar canal stenosis.[1,2,3,4]
Lumbar spinal degeneration that leads to lumbar canal stenosis is a disabling clinical condition. The pathogenesis has been well-described in the literature.[11,12,13] The most accepted view of pathogenesis is that it is related to a cascade of processes that start with degeneration of the disc due to its dehydration or herniation. It has been generally accepted that following this primary event, there occurs loss of disc space height, bulge of the posterior annulus/posterior longitudinal ligament, overriding of the facets and/or infolding of the ligamentum flavum and similar such events that ultimately lead to stenosis of the spinal canal and intervertebral neural foramina. Although the issue of instability in lumbar canal stenosis has been discussed on several occasions, its role as the primary factor in the pathogenesis of lumbar canal stenosis has not been appropriately addressed.
On the basis of our observations, we identified that instability of the spinal segment, probably related to muscle weakness, had a profound impact on the pathogenesis of the entire spectrum of spondylosis or degeneration of the spine.[1,2,5] The symptoms of lumbar canal stenosis are related to posture and often increase on extension and on prolonged standing or walking. Considering that the symptoms occur only after physical activity, and only rarely at rest, it appears that the canal is not inherently stenosed, but the physical activity or posture initiates a phenomenon that leads to stenosis. After a period of rest or on altering the posture, the canal stenosis is reversed. It is apparent that weakness of the muscles of the back leads to their fatigue on exercise and subsequent incompetence may lead to facetal override or telescoping. The radiological effect on the lumbar canal size on axial loading has been discussed. It appears that the phenomenon of lumbar canal stenosis is “dynamic” in nature and local spinal instability plays a major role in its genesis. Standing human posture, ageing muscles, heavy body weight and sedentary life style may have contributory effects on pathogenesis of lumbar canal stenosis. It does appear that the muscles have a role in keeping the spinal segments apart. Reduction of the articular cavity space and subsequent facetal overriding or telescoping and consequent ligamental laxity and buckling might occur on activity. Physiotherapy and traction over the back have been successfully used for decades in the management of lumbar spinal degeneration. We identified that such a form of treatment that involved facetal distraction resulted in reversal of several pathologic events that are related to spondylosis. In the presented series, we fixed the affected spinal segments using transarticular screws, without physically distracting the facets. However, the fixation of the facets was done in a prone position that obliterated the lumbar lordosis, widened the inter-facet distance and resulted in flexion of the spinal segment. Our successful outcome in the presented group of patients suggests that stabilization of the spinal segment has a role in the treatment of lumbar canal stenosis. Stabilization of the facets might assist in the alleviation of dynamic events that are associated with lumbar canal stenosis. Fixation of the involved motion segment assists in eliminating subtle movements that could probably be the cause of pain in the segment.
Transarticular screws have been described earlier in stabilization of the lumbar spine.[14] A number of biomechanical studies are available that suggest that transarticular screws provide satisfactory stability to the lumbar spinal segment. However, such screws have not become a popular mode of spinal stabilization as lumbar pedicular screw-rod stabilization has become a standard form of fixation and seem clearly stronger. We sectioned the spinous process at its base. This procedure provided a possibility of insertion of transarticular screw with a wider and inferior angle. The screw could now travel in the lamina and subsequently through the facets and ended in the base of the transverse process. Wider exposure of the facets following the spinous process resection and the relatively large size of the facets facilitated insertion of two screws in a transarticular fashion. Insertion of the two screws provided “double-insurance” stabilization. Although navigation provided accuracy to the procedure, even free-hand screw insertion under direct surgical vision seemed to be safe. The remarkable strength of the transarticular screws could be appreciated during the process of screw tightening and was also evident by the fact that not a single screw seemed to malfunction or changed its initial deployment position during the period of follow-up. Mineral density of the bones of the facets is significantly superior to that of any other part of the vertebra, imparting greater strength to the process of fixation. The large spinous process provided ample bone graft material. The spinous process was shredded into small multiple pieces, was placed in the articular cavity after denuding the articular cartilage and was placed over the appropriately prepared host area of laminae. The technique of deployment of screws is simple and significantly quick when compared with most other methods of decompression and fixation. The procedure can be done in isolation or can be employed as a supplement to all other techniques. It can be done when other methods of fixation/decompression have failed. The drawback of this study is that a comparative cohort of patients who had undergone either a traditional decompressive laminectomy or other types of decompressive surgery was not performed. Moreover, the exact inclusion/exclusion criteria for deployment of the technique will need to be assessed, evaluated and determined on the basis of further clinical experience.
CONCLUSION
Fixation of the spinal segment using double insurance screws can be a rational, relatively simple, safe and effective surgical option for lumbar canal stenosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Goel A. Facet distraction spacers for treatment of degenerative disease of the spine: Rationale and an alternative hypothesis of spinal degeneration. J Craniovertebr Junction Spine. 2010;1:65–6. doi: 10.4103/0974-8237.77669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goel A. Facet distraction-arthrodesis technique: Can it revolutionize spinal stabilization methods? J Craniovertebr Junction Spine. 2011;2:1–2. doi: 10.4103/0974-8237.85306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goel A, Shah A. Facetal distraction as treatment for single- and multilevel cervical spondylotic radiculopathy and myelopathy: A preliminary report. J Neurosurg Spine. 2011;14:689–96. doi: 10.3171/2011.2.SPINE10601. [DOI] [PubMed] [Google Scholar]
- 4.Goel A, Shah A, Jadhav M, Nama S. Distraction of facets with intraarticular spacers as treatment for lumbar canal stenosis: Report on a preliminary experience with 21 cases. J Neurosurg Spine. 2013;19:672–7. doi: 10.3171/2011.8.SPINE11249. [DOI] [PubMed] [Google Scholar]
- 5.Goel A. ‘Only fixation’ as rationale treatment for spinal canal stenosis. J Craniovertebr Junction Spine. 2011;2:55–6. doi: 10.4103/0974-8237.100049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairbank JC, Pynsent PB. The oswestry disability index. Spine (Phila Pa 1976) 2000;25:2940–52. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Huskisson EC. Measurement of pain. J Rheumatol. 1982;9:768–9. [PubMed] [Google Scholar]
- 8.Richards JC, Majumdar S, Lindsey DP, Beaupre G, Yerby S. Montreaux: Tran International Meeting on Advanced Spine Techniques; 2002. Quantitative changes in the lumbar spinal canal with an interspinous implant. [Google Scholar]
- 9.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, et al. A prospective randomized multi-center study for the treatment of lumbar spinal stenosis with the X Stop interspinous implant: 1-year results. Eur Spine J. 2004;13:22–31. doi: 10.1007/s00586-003-0581-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lo TP, Jr, Salerno SS, Colohan AR. Interlaminar spacer: A review of its mechanism, application, and efficacy. World Neurosurg. 2010;74:617–26. doi: 10.1016/j.wneu.2010.05.038. [DOI] [PubMed] [Google Scholar]
- 11.Boden SD, Riew KD, Yamaguchi K, Branch TP, Schellinger D, Wiesel SW. Orientation of the lumbar facet joints: Association with degenerative disc disease. J Bone Joint Surg Am. 1996;78:403–11. doi: 10.2106/00004623-199603000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Dunlop RB, Adams MA, Hutton WC. Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br. 1984;66:706–10. doi: 10.1302/0301-620X.66B5.6501365. [DOI] [PubMed] [Google Scholar]
- 13.Kirkaldy-Willis WH, Paine KW, Cauchoix J, McIvor G. Lumbar spinal stenosis. Clin Orthop Relat Res. 1974;99:30–50. doi: 10.1097/00003086-197403000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Rajasekaran S, Naresh-Babu J. Translaminar facetal screw (Magerl's) fixation. Neurol India. 2005;53:520–4. doi: 10.4103/0028-3886.22624. [DOI] [PubMed] [Google Scholar]


