Abstract
Aim:
Quantitative anatomy of the facets of the sub-axial cervical spine was performed. The purpose of the evaluation was to determine the feasibility of insertion of Goel inter-facetal articular spacers in the sub-axial cervical spine. Only few studies detailing the morphometry of the facets are available in the literature.
Materials and Methods:
Ten cervical vertebrae from C3 to C7 with a total of 20 facets were evaluated by the author. The anatomic parameters studied were the height, width, thickness, shape, orientation, and inclination of each of the superior and inferior facets. The alterations in a number of intervertebral segmental distances were measured before and after spacer insertion. The distance of the inferior facet from the foramen tranversarium, spinal canal, and neural foramina was measured to assess safety of spacer insertion with respect to the vertebral artery and neural structures.
Results:
The height, width and thickness of the superior facets from C3 to C7 ranged from 6 to 12 mm, 8 to 12 mm, and 2.5 to 6 mm, respectively. The inferior facets had an average height of 10.5 mm, average width of 11.2 mm and average thickness of 3.5 mm. The inclination of the superior facets with respect to the transverse plane ranged from 22° to 45° and that of the inferior facets ranged from 29° to 53°. The distance of the anterior margin of the inferior facet from the posterior border of the foramen transversium ranged from 5 to 7 mm. This distance was maximum at C3 level, then decreased at C4 and remained constant from C5 to C7.
Conclusion:
This anatomic evaluation aided in understanding the morphology of the cervical facets and the suitability of the cervical facetal articular cavity for insertion of spacers.
Keywords: Goel inter-facet spacer, spondylosis, sub-axial cervical facets
INTRODUCTION
Various methods are available for treatment of cervical spondylosis. These include anterior and posterior approaches with or without fixation of the affected segments. A number of techniques have been used for spinal fixation. We have recently described a novel method of cervical spinal fixation using facetal spacers.[1,2,3,4] The technique involves facetal distraction and indirect decompression of the spinal cord and the roots without removal of any bone, disc or ligaments. To use this technique effectively knowledge of the anatomy of the cervical facets is essential. The quantitative anatomy, orientation of the facet joints and the movements occurring at these joints has been discussed on occasions. The mechanical strength and the thick quality of the bone of the facets have been therapeutically exploited only infrequently due to its close proximity to the vertebral artery and the nerve roots. Moreover, the anatomy of facets was poorly delineated on the relatively inferior quality radiological images that were available earlier. There are only a few studies in literature discussing the orientation and morphometry of the cervical facets.[5,6,7] In the present analysis, the physical characters of the cervical sub-axial facets has been evaluated and their suitability for insertion of Goel facetal spacers has been discussed. The effects and safety of technique are elaborated on the basis of this anatomic review.
MATERIALS AND METHODS
Ten dried cadaveric C3 to C7 vertebrae were procured from the Anatomy Department of our Institution [Figures 1–5]. A total of 20 facets of each vertebra were evaluated. Morphometric evaluation of the superior and inferior facets was conducted. The shape, orientation, dimensions, inclination, and relationship of the facets with the adjoining spinal and intervertebral root canal and vertebral artery foramina were studied. The various parameters used for measurement are shown in Tables 1 and 2. A micro caliper was used for linear measurements and a goniometer was used for angular measurements. The heights of the facets were measured from superior to inferior, the width was measured in a lateral to medial direction and the thickness of the facets was measured in an anteroposterior direction. The maximum diameters were considered for each parameter [Figure 1a]. The inclination of the facets was measured in the transverse plane with the vertebra held in the position that it lies in the body. The inclination of the facet in the transverse plane was measured as the angle between a line drawn along the length of the facet and a line drawn through the inferior edge of the facet parallel to the transverse plane [Figure 1c]. The distance between the anterior margins of the inferior facet to the posterior margin of the foramen transversarium was also measured. After these preliminary measurements, the facetal height and inter spinous distances were measured before and after insertion of facetal spacers. Spacers used were Goel inter-facetal titanium spacers and ranged from 2 to 4 mm in height and 8 mm in diameter. The facetal height was measured from the anterior lip of the inferior facet of the rostral vertebra to the anterior lip of the superior facet of the caudal vertebra. The interspinous distance was measured as the distance between the tips of the spinous processes. Each vertebra was measured twice at varied times to decrease interobserver variability. The safety of facetal spacer insertion with respect to the vertebral artery and exiting nerve roots was evaluated.
Figure 1a.
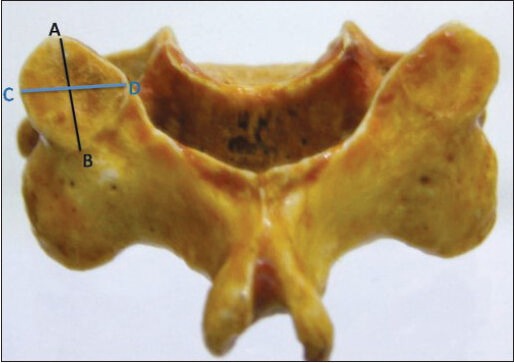
Posterior view of the C3 vertebra showing the superior articular facets. The lines AB and CD show the measured height and width respectively of the superior articular facet
Figure 5a.
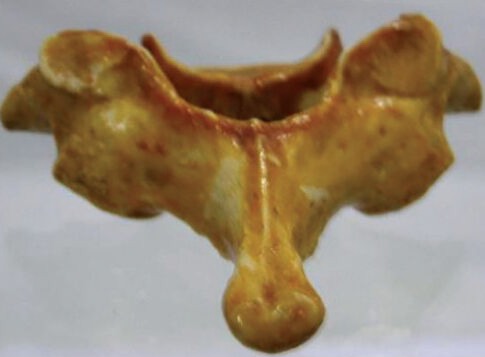
Posterior view of the C7 vertebra showing the superior articular facets
Table 1.
The measured parameters of the superior facet of the sub-axial vertebrae
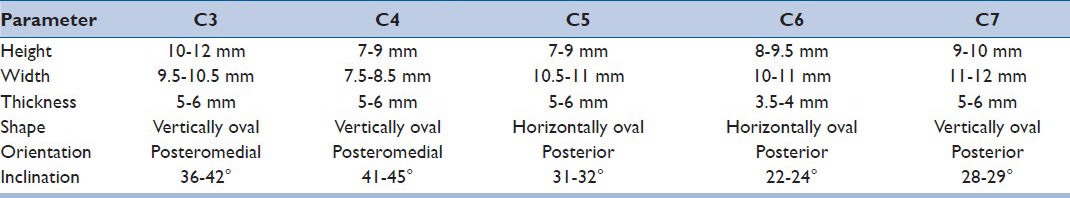
Table 2.
The measured parameters of the inferior facet of the sub-axial vertebrae
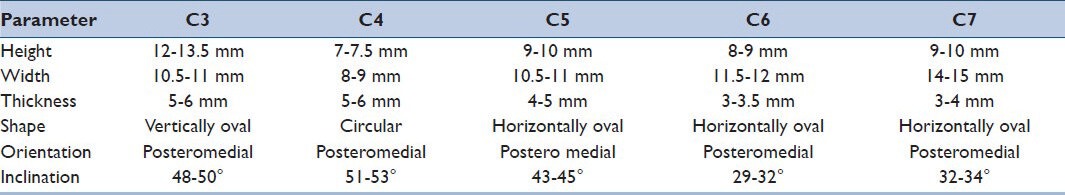
Figure 1c.
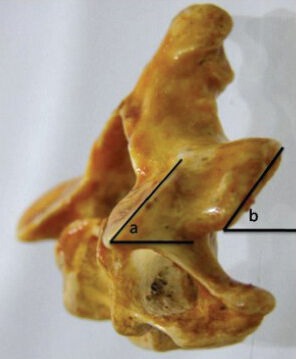
View of the C3 vertebra as it lies in the prone position in the human body. The angles a and b denote the angle of the superior and inferior respectively facets with the transverse plane
RESULTS
The results of measurements of various parameters from C3 to C7 are shown in Tables 1 and 2. There was no significant difference observed between the two sides in the parameters measured. The difference between males and females was not evaluated.
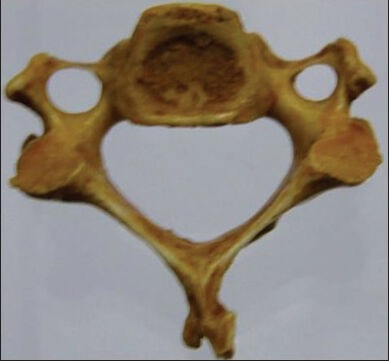
Superior facet [Figures 1a, 2a, 3a, 4a and 5a]
Figure 2a.
Posterior view of the C4 vertebra showing the superior articular facets. Note that the facets are smaller in size as compared to C3 and the other lower cervical vertebra
Figure 3a.

Posterior view of the C5 vertebra showing the superior articular facets
Figure 4a.
Posterior view of the C6 vertebra showing the superior articular facets
The heights of the superior facets ranged from 7 to 12 mm. The largest height of the superior facet was found at C3 level. The height decreased from C4 to C5 and then again increased from C6 to C7. The width of the facets ranged from 7.5 to 12 mm. The superior facet was widest at C7 level. The width decreased from C3 to C4 and again increased from C5 to C7. The thickness of the superior facets ranged from 3.5 to 6 mm. The inclination with the transverse plane ranged from 22° to 45°. The largest transition of the angle was seen at the C6 vertebra where the angle became more acute. The shape of the superior facet was vertically oval at C3 and C4 level and horizontally oval at C5 and C6 levels and again becoming more toward the vertical at C7 level. The superior facets of C3 and C4 had a posteromedial orientation, whilst those of C5 to C7 faced posteriorly.
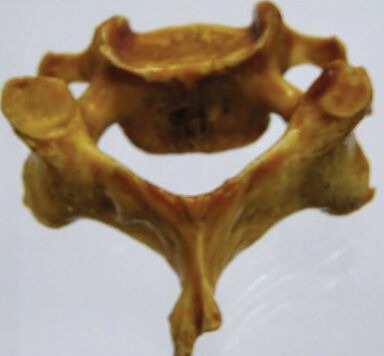
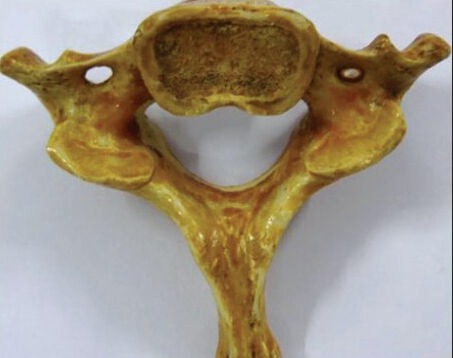
Inferior facet [Figures 1b, 2b, 3b, 4b and 5b]
Figure 1b.

Inferior view of the C3 vertebra showing the inferior articular facets
Figure 2b.
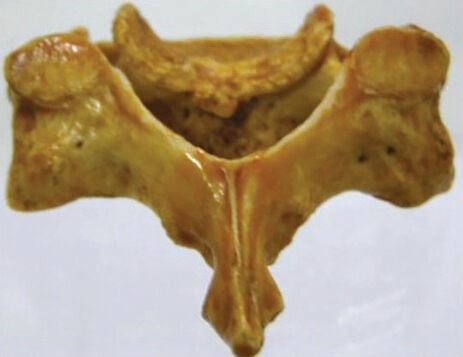
Inferior view of the C4 vertebral body showing the inferior articular facets
Figure 3b.

Inferior view of the C5 vertebral body showing the inferior articular facets
Figure 4b.

Inferior view of the C6 vertebral body showing the inferior articular facets
Figure 5b.
Inferior view of the C7 vertebral body showing the inferior articular facets
The heights of the inferior facets ranged from 7 to 13.5 mm. The height of the inferior facet was maximum at C3 level then decreased at C4 level and then again increased at C5 and was nearly the same at C6 and C7 levels. The widths of the inferior facets ranged from 8 to 15 mm. The width of the inferior facet was maximum at C7 level and least at C4 level. The thickness of the inferior facets ranged from 3 to 6 mm. The thickness of the inferior facet decreased from C3 to C7. The facet angle was wider at C3 and became narrower at C6 and C7. The shape of the inferior facet was vertically oval at C3, circular at C4 level and horizontally oval at C5 to C7 levels. The inclination of the facet with the transverse plane ranged from 29° to 53°. The most acute angle was seen at C6 level.
Thus, the facets had the greatest height at C3 level and the greatest width at C7 level. C4 facets were the smallest in size. The C6 superior and inferior facet showed the most sudden transition in angles with respect to the transverse plane.
The inter-facetal height was maximum at C3 level then decreased from C4 to C6 and then again increased at C7 level. The thickness at the inter-facetal region was maximum at C3 level and then decreased from C3 to C7. The distance of the anterior margin of the inferior facet from the posterior margin of the foramen transversarium ranged from 5 to 7 mm and was maximum at C3 level, then decreased at C4 and remained constant from C5 to C7.
In the normal position, the superior and inferior facets lie close to each other with just a thin articular cartilage lining between them. The facetal height (distance between the superior and inferior facets before and after insertion of spacers) ranged from 5 to 8 mm prior to insertion of facetal spacers, after insertion the height ranged from 7.5 to 12 mm. The interspinous height ranged from 1.8 to 2.1 cm prior to spacer insertion and increased to 2.1–3 cm after spacer insertion. Insertion of the spacers distracted the cervical vertebrae and led to an increase in the intervertebral neural foramen height and in the inter spinous distances. This in turn indirectly decompresses the exiting nerve root and also causes the buckled ligamentum flavum to become tauter. The increase in the intervertebral height was difficult to measure on the dried bones, but this has already been shown by us radiologically in our prior publication where there was an average of 2.2 mm increase in foraminal height [Figures 6a and b].[1]
Figure 6a.

Pre-operative 3D CT scan showing the facets and the alignment
Figure 6b.

Post-operative CT scan showing Goel intrafacetal spacers
DISCUSSION
Anatomy of the cervical vertebrae has been described on occasions, but most of these studies are focused on the dimensions of the pedicle for transpedicular fixation. Very few studies are available on the quantitative anatomy of the sub-axial cervical facets.[5,6,7] Orientation of the cervical facets and its significance to spinal movements also has been studied. Pal et al. in their study noted the orientation of the facet joints at the cervical and upper thoracic region.[5] Panjabi et al. studied the linear and angular measurements of the cervical facets.[6] In this study, the sub-axial cervical facet joints were studied and their suitability was assessed for Goel facet distraction arthrodesis technique using facetal spacers.
The superior facet lies rostrally with its articular facet facing dorsally and the inferior facet lies caudally with its articular facet facing ventrally. The articular processes of the cervical spine are inclined approximately 45° from the horizontal plane with steeper inclinations in the lower segments. They are oriented 0° in the coronal plane. These are the most horizontally oriented regional facet joints in the spinal column. The orientation of these facets allows flexion and extension, lateral bending and rotation of the lower cervical spine.
Panjabi et al.[6] have reported posteromedial orientation of all the superior facets from C3 to C7, whereas there was posterolateral orientation from C5 in the studies by Ebraheim et al.[7] and Pal et al.[5] In this study, the facets of C3 and C4 were found to be posteromedially oriented and those of C5, C6 and C7 were posteriorly oriented. This orientation of the facetal joints in the cervical region is such that their distraction leads to an increase in not only the inter-facetal height, but also the interspinous height and the intervertebral body height. This distraction leads to a decrease in the ligamentous buckling in the region, thus decompressing the cord. The intervertebral foraminal height also increases thus decompressing the root.
The height of the superior facet ranged from 7 to 12 mm and that of the inferior facet ranged from 7 to 13.5 mm. The width of the superior facet ranged from 7.5 to 12 mm and that of the inferior facet ranged from 8 to 15 mm. The width and height of the facets were almost the same at C3 and C4 level. From C5 to C7, the width was more than the height.
In a study performed by Francis, the mean facet joint widths for males ranged from 10.1 to 12.3 mm and from 9.9 to 11.7 mm for females.[8] In 1991, Milne disarticulated human cadaver vertebrae and determined facet joint widths from C3 to T1 levels.[9] Data from this study ranged from 8.5 to 10.4 mm. In 1993, Panjabi et al. reported a higher range (10.2-13.9 mm) in the C3 to T1 facet joint widths.[10] In contrast, in 1997 Ebraheim et al. found the widths to range from 8.6 to 9.6 mm for C3 to C7 levels of the spine.[10] Our findings were consistent with these studies.
In this study, the angle of inclination of the superior and inferior facets was measured with the vertebra kept in the position as it lies in the human prone position. This angle gave the angle of insertion of the spacers between the superior and inferior facets. The angle varied from approximately 30° to 50° at the various levels.
The mechanical strength, oblique profile, shape, and relatively large size of the facets can be used quite safely and effectively for facetal spacer insertion. The sizes of the spacers used varied from 2 to 4 mm in height and 8 mm in diameter. Spacers of larger diameter can be used for the C3 and C7 vertebrae. The distance of the inferior articular facet from the foramen tranversarium was more than 5 mm at all levels, thus keeping the vertebral artery at a safe distance from facetal spacers. The diameter of the spacers used never exceeded the facetal area available. Thus there is no risk of injury to the root or the vertebral artery.
Measuring the facetal and interspinous height before and after spacer insertion demonstrated a mean increase of 3 mm in the facetal height and a mean increase of 4 mm in the interspinous distance. This increase gives credence to the philosophy of decompression of the root and spinal cord using the technique of facetal distraction. Tan et al. in a recent publication studied the effects of machined allograft spacers on the cervical foraminal height and area.[11] The use of the spacers increased the cervical foraminal height and area and caused indirect decompression of the exiting nerve root.
It is generally believed that spinal degenerative disease initiates in the disc and osteophyte formation and retrolisthesis of the facets are secondary phenomenon. It has been proposed by us that the spondylotic disease may actually commence in the facet joints leading to subtle facetal instability and retrolisthesis, secondarily involving the intervertebral discs. This retrolisthesis is a result of subtle or manifest instability of the segment. This retrolisthesis can lead to a decrease in the inter-facet height and a reduction in the foraminal and intervertebral canal height causing radiculopathy and myelopathy. Impaction of the spacers within the intra-articular space causes several structural changes, which can result in reversal of the pathological effects of cervical spondylosis. The impacted spacer also provided firm stability to the region and is safe with respect to the vertebral artery and the exiting nerve root.
CONCLUSION
Goel intra-articular spacers can be effectively used in the cervical facets for treatment of cervical spondylotic disease. They can be used as a stand-alone method of treatment or in combination with other methods of fixation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Goel A, Shah A. Facetal distraction as treatment for single- and multilevel cervical spondylotic radiculopathy and myelopathy: a preliminary report. J Neurosurg Spine. 2011;14:689–96. doi: 10.3171/2011.2.SPINE10601. [DOI] [PubMed] [Google Scholar]
- 2.Goel A. Facet distraction spacers for treatment of degenerative disease of the spine: Rationale and an alternative hypothesis of spinal degeneration. J Craniovertebr Junction Spine. 2010;1:65–6. doi: 10.4103/0974-8237.77669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goel A. Facet distraction-arthrodesis technique: Can it revolutionize spinal stabilization methods? J Craniovertebr Junction Spine. 2011;2:1–2. doi: 10.4103/0974-8237.85306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goel A. Relevance of Goel's hypothesis regarding pathogenesis of degenerative spondylosis and its implications on facet distraction surgery. J Craniovertebr Junction Spine. 2012;3:39–41. doi: 10.4103/0974-8237.116531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pal GP, Routal RV, Saggu SK. The orientation of the articular facets of the zygapophyseal joints at the cervical and upper thoracic region. J Anat. 2001;198:431–41. doi: 10.1046/j.1469-7580.2001.19840431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panjabi MM, Oxland T, Takata K, Goel V, Duranceau J, Krag M. Articular facets of the human spine. Quantitative three-dimensional anatomy. Spine (Phila Pa 1976) 1993;18:1298–310. doi: 10.1097/00007632-199308000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Ebraheim NA, Patil V, Liu J, Haman SP, Yeasting RA. Morphometric analyses of the cervical superior facets and implications for facet dislocation. Int Orthop. 2008;32:97–101. doi: 10.1007/s00264-006-0286-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Francis CC. Variations in the articular facets of the cervical vertebrae. Anat Rec. 1955;122:589–602. doi: 10.1002/ar.1091220408. [DOI] [PubMed] [Google Scholar]
- 9.Milne N. The role of zygapophysial joint orientation and uncinate processes in controlling motion in the cervical spine. J Anat. 1991;178:189–201. [PMC free article] [PubMed] [Google Scholar]
- 10.Ebraheim NA, Xu R, Challgren E, Yeasting RA. Quantitative anatomy of the cervical facet and the posterior projection of its inferior facet. J Spinal Disord. 1997;10:308–16. [PubMed] [Google Scholar]
- 11.Tan LA, Gerard CS, Anderson PA, Traynelis VC. Effect of machined interfacet allograft spacers on cervical foraminal height and area. J Neurosurg Spine. 2014;20:178–82. doi: 10.3171/2013.11.SPINE131. [DOI] [PubMed] [Google Scholar]


