Abstract
Background:
During recent years, there have been many advances in different types of pharmacological and non-pharmacological tobacco control treatments. In this study, we aimed to identify the most effective smoking cessation methods used in quit based upon a review of the literature.
Methods:
We did a search of PubMed, limited to English publications from 2000 to 2012. Two trained reviewers independently assessed titles, abstracts and full texts of articles after a pilot inter-rater reliability assessment which was conducted by the author (GH). The total number of papers and their conclusions including recommendation of that method (positive) or not supporting (negative) was computed for each method. The number of negative papers was subtracted from the number of positive ones for each method. In cases of inconsistency between the two reviewers, these were adjudicated by author.
Results:
Of the 932 articles that were critically assessed, 780 studies supported quit smoking methods. In 90 studies, the methods were not supported or rejected and in 62 cases the methods were not supported. Nicotine replacement therapy (NRT), Champix and Zyban with 352, 117 and 71 studies respectively were the most supported methods and e-cigarettes and non-Nicotine medications with one case were the least supported methods. Finally, NRT with 39 and Champix and education with 36 scores were the most supported methods.
Conclusions:
Results of this review indicate that the scientific papers in the most recent decade recommend the use of NRT and Champix in combination with educational interventions. Additional research is needed to compare qualitative and quantitative studies for smoking cessation.
Keywords: Methods, systematic review, tobacco cessation, tobacco control
INTRODUCTION
Among smokers who are aware of the ill effects of smoking, 3 out of 4 individuals are interested in quitting.[1] One of the most important responsibilities of a countries’ health care system is to treat nicotine dependence. This effort consists of different methods such as simple clinical counseling, medications and quit lines. The cost of these methods differs, however and these methods are not equally effective. It also is important to match the treatment method to the local and cultural context as well as to clients’ current needs.[2]
Repeated consultation is important in reinforcing the necessity of quitting smoking at every clinical visit.[3] Furthermore, counseling by health workers increases quit rates.[4] This intervention is relatively cost-effective, because it is part of the existing health care services which are used by the majority of smokers. These interventions are effective because they are offered by health care providers, who are respected by the public and smokers also have a good relationship with them.[5,6] Moreover, it is important to provide the quit lines services free- of- charge from any telephone. Even old telephone line systems that responded only to incoming calls showed very significant results.[7]
In addition to clinical counseling and quit lines for consultation, an effective treatment can include medication. Medication includes nicotine replacement therapy (NRT) (patches, gum, sublingual tablets, lozenges, inhalers and nasal spray) and prescribed drugs such as Bupropion and Varenicline.[8] In general, medication is more expensive than medical counseling and quit lines. However, the evidence showed that it can double or triple quit rates.[9]
Now after 9 years from the first educational interventions for quitting smoking and one of two complementary integrated programs in the primary health care network, the situation for counseling, human resources and medication is not suitable at the country level and there is insufficient documentation and studies in this regard.[10,11,12,13] Thus, it was considered beneficial to identify the best current evidence and incorporate the latest outcomes. This would allow for development of an appropriate framework necessary to assess different methods in order to select the best approaches for essential interventions at the country level. This study specifically targeted decision makers in Iran to enable a quantitative systematic review based on the two following two main questions:
Which smoking cessation methods are most published?
Which one is the most effective method?
METHODS
Based on a cross-sectional study, English publications from 2000 to 2012 in PubMed were selected.
To find articles related to quitting smoking, we considered one of the following keywords from a title: Quit or cessation, NRT, Champix or Varenicline or Chantix, Zyban or Bupropion sustained-release, Combination Therapy, Training, Self-learning material, Behavior Therapy, Quit and Win, Hypnosis, Telephone consulting, Acupuncture, Interactive Voice Response (IVR), E-Cigarettes, pharmacological treatments, Non-pharmacological treatments, Personal Methods, Non-nicotine medications.
In an expert panel meeting it was proposed to include relevant articles (at a minimum, these must include the abstracts). Unpublished and duplicated articles and opinion based papers were excluded as they were not classified as relevant. Articles were reviewed separately by two qualified assistants, who were trained and calibrated to achieve desirable agreement in the selecting of articles. In order to reach check reliability, a pilot inter-rater reliability assessment was conducted by the author (GH). Each reviewer assessed three randomly selected articles. The inter-rater reliability was 67% before discussion; any discrepancies in answers were discussed and a consensus was achieved on review.
After the training and pilot assessment, the author (GH) determined that the assistants were ready to do the search. The reports of the assistants were observed again by the author (GH), who determined when the assistants were ready to work alone.
Finally, the assistants selected and categorized the articles according to the following criteria for each method: Total number of articles, the number of articles that supported quit smoking efforts, the number of articles that did not support quit smoking efforts and the number of articles without any firm conclusions.
Again in order to assess the reliability of each assistant, one method was selected randomly and the recorded results were compared by the author (GH). If there were discrepancies in the figures, these were corrected by author (GH).
Different methods were used for rating articles and the strengths and weakness of each were discussed through an expert panel meeting. Finally, the best scoring model was accepted for each stop-smoking method, which included a maximum of 40 scores of which 20 scores were for articles that supported methods (positive articles minus negative articles) and 20 points for the highest proportion of supported to the total number of articles.
For scoring of each article, one point was possible, since we did not consider differences between articles which were published in PubMed. However, a point was not given for articles that did not have a clear result.
Because newer treatment methods had less chance for having more published articles; an index of positive articles to total articles was calculated and awarded half of the total index of 20. The papers were prioritized according to their scores.
RESULTS
This search resulted in a folder with 3081 titles of articles; of which 1436 were inaccessible (at a minimum an abstract). Out of 1645 remaining articles, 713 were not about treatment and its effect on quitting smoking (they were about history, smoking cessation programs in countries, relevant policies, rules and regulations for stopping smoking, Article 14 of World Health Organization [WHO] Framework Convention on Tobacco Control, etc.)
Of the 932 remaining articles, 62 articles did not support quit smoking methods (with no good results or side-effects). Of 870 remaining manuscript, 90 cases did not demonstrate a clear result (even whether the method is usable) [Figure 1].
Figure 1.
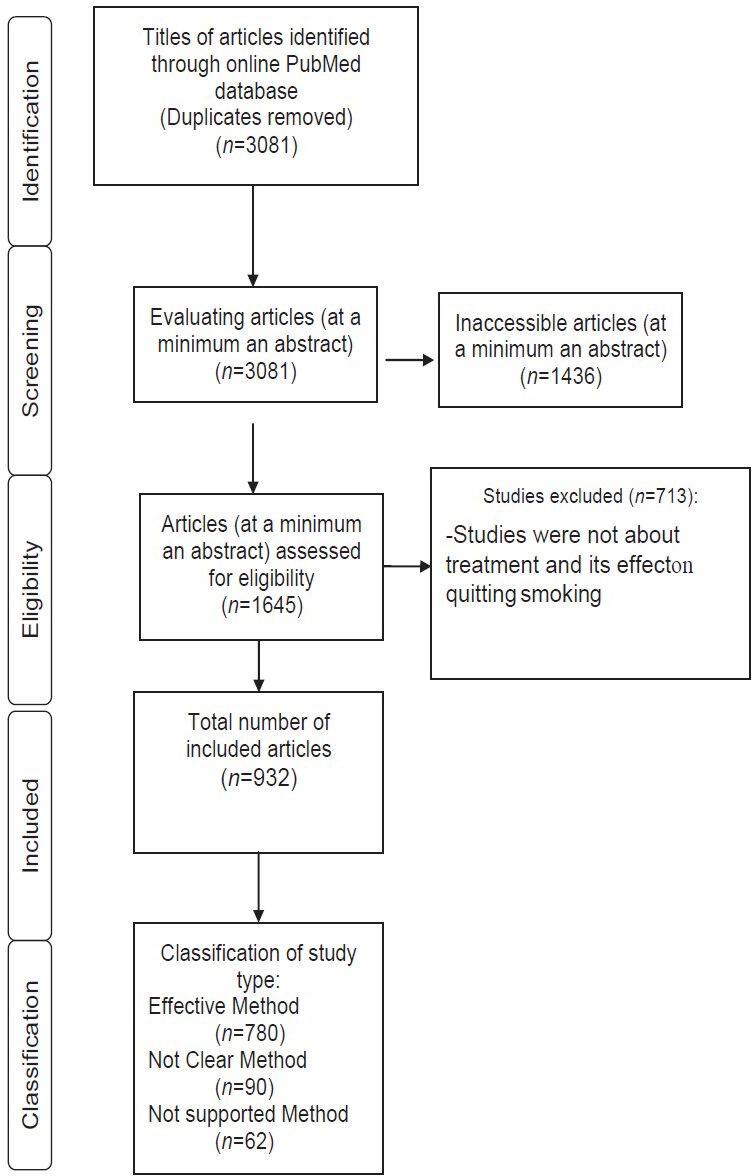
Study selection flow diagram
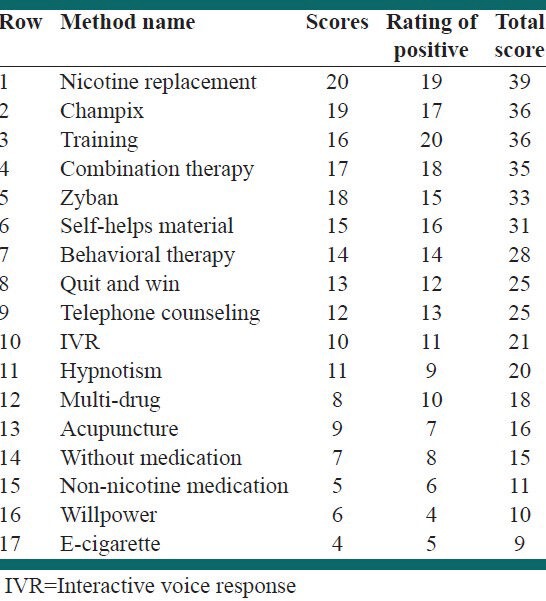
NRT, Champix and Zyban respectively with 352, 117 and 71 cases were the most advised method and E-cigarette and non-nicotine medication with one case were the least advised methods. For each method the number of advising articles to the total was 31 out of 32 and for NRT was 376 of 407 (which was considered the maximum score). Willpower with two out of 9 was the lowest score and finally NRT with a score of 39 and Champix and training with a score of 36 were the best methods. The number of selected articles and the results are shown in Tables 1 and 2.
Table 1.
Prevalence of smoking cessation methods in included articles (n=932) and the results obtained by number of articles and based on classification of the studies
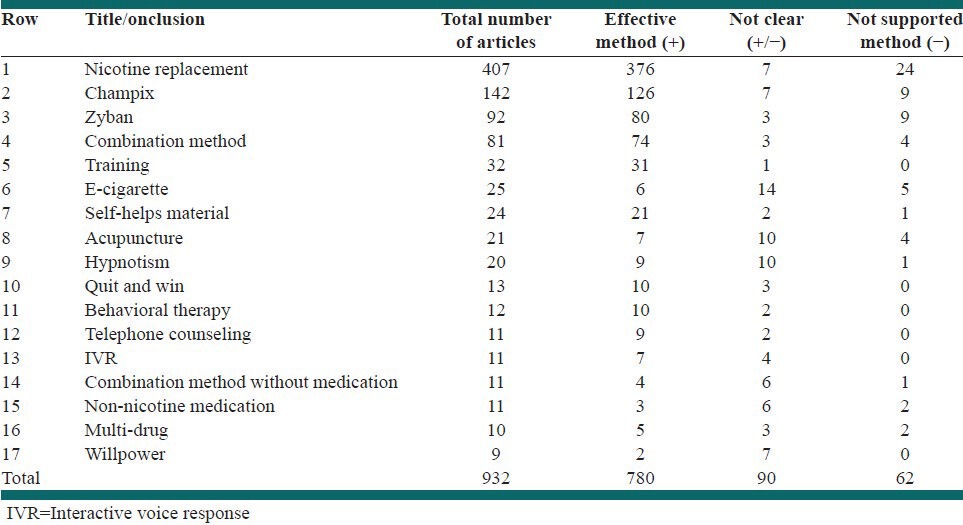
Table 2.
Prevalence of quit smoking methods in the included articles (n=932 and their scores)
DISCUSSION
Unfortunately, after a decade of offering quit smoking services, the situation is not so positive in Iran and is still based on older methods such as 15 mg nicotine patches and group therapy. These services have not been updated on the basis of more recent evidence. For determining which quit smoking methods are maximally effective, a comprehensive review of all recent articles was a necessity in order to obtain suitable qualitative indicators for selecting effective quit smoking methods.
In this study, it was found that three methods – NRT, Champix and education for quitting smoking – are advised most frequently based on the articles referenced in PubMed between the years 2000 and 2012. These findings are informative in updating the health care services at the country level and a combination of these methods might be provided. Many countries that offer cessation services follow better methods through evaluation and incorporating necessary modifications to these methods.[14]
As displayed in the results, NRT, Champix, Training, Combination treatment, Zyban and self-help materials received the highest scores with over 30 points; multi-drug treatment, acupuncture, some methods without medication such as nurse counseling, Non-nicotine drugs, will power and E-cigarettes had the lowest scores with less than 20 and the remaining methods including behavioral methods, Quit and Win, telephone counseling and IVR and Hypnotism were in the middle. The results of this study are consistent with the findings of high impact articles in WHO, Centers for Disease Control and Prevention and Cochrane,[15,16,17,18] and these results also were consistent with the writers’ experience. However, it was necessary to prioritize quitting methods based on a new quantitative analysis and simple qualitative methods in order to gain the support of decision makers for further necessary interventions. That is because the systematic reviews, such as Cochrane, do not provide guidance on which of the effective methods are best for a particular environment.
In the systematic reviews articles were weighted based on a qualitative approach. The results from articles reporting similar methods were added. Finding the relevant articles was challenging in the current study because we selected a huge number of articles for a particular selected method (based on the accessibility of the full text or abstract). However, subsequently calculating the results was straightforward.
Boyle et al.[19] and Linder et al.[20] in their studies have reported that use of electronic medical registration and continuous use of nicotine patches can increase success of smoking cessation attempts. Furthermore, new methods in Thailand have reached more tobacco users.[21]
This study was the first quantitative study, which provided us with a wide perspective about all tobacco cessation methods.
There were several limitations including the fact that not all studies were equal. We considered all indexed journals independently of impact factors. Scores were based in part on number of publications, thereby creating a bias in favor of older methods with more opportunity for publication. Some of the newer methods are quite recent and therefore not surprisingly have few published assessments. This study could be a useful indicator of effective quit smoking methods based on updated scientific documents. The results of this study could be used as a reference for decision makers who are charged with selecting cessation methods at the country level that will produce good outcomes.
CONCLUSIONS
The articles reviewed produced significant results across a wide range of included studies. Methods that obtained the higher scores have been applied most frequently in interventions that have had positive effects on quit rates. According to the updated scientific and updated evidence based on a simple and quantitative approach, quit smoking methods with high and better scores including NRT, Champix and training have been recognized as effective and the other methods have received lower scores. Further studies are needed to implement a comparative study on qualitative and quantitative smoking cessation methods that could lead to increased quit rates at the country level.
ACKNOWLEDGMENTS
I would like to express my gratitude to all those who helped us to complete this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jones JM. Smoking habits stable; most would like to quit. [Last cited on 2007 Dec 6; Last updated on 2006 Jul 18]. Available from: http://www.gallup.com/poll/23791/Smoking-Habits-Stable-Most-Would-Like-Quit.aspx .
- 2.Solberg LI, Maciosek MV, Edwards NM, Khanchandani HS, Goodman MJ. Repeated tobacco-use screening and intervention in clinical practice: Health impact and cost effectiveness. Am J Prev Med. 2006;31:62–71. doi: 10.1016/j.amepre.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 3.West R, Sohal T. “Catastrophic” pathways to smoking cessation: Findings from national survey. BMJ. 2006;332:458–60. doi: 10.1136/bmj.38723.573866.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fiore MC. Rockville, MD: U.S. Department of Health and Human Services, Press Briefing; [Last cited on 2007 Dec 16; Last updated on 2000 Jun 27]. Treating Tobacco Use and Dependence: A Public Health Service Clinical Practice Guideline. Available from: http://www.surgeongeneral.gov/tobacco/mf062700.htm . [Google Scholar]
- 5.Feenstra TL, Hamberg-van Reenen HH, Hoogenveen RT, Rutten-van Mölken MP. Cost-effectiveness of face-to-face smoking cessation interventions: A dynamic modeling study. Value Health. 2005;8:178–90. doi: 10.1111/j.1524-4733.2005.04008.x. [DOI] [PubMed] [Google Scholar]
- 6.Bao Y, Duan N, Fox SA. Is some provider advice on smoking cessation better than no advice? An instrumental variable analysis of the 2001 National Health Interview Survey. Health Serv Res. 2006;41:2114–35. doi: 10.1111/j.1475-6773.2006.00592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Owen L. Impact of a telephone helpline for smokers who called during a mass media campaign. Tob Control. 2000;9:148–54. doi: 10.1136/tc.9.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pfizer for Professionals. Mechanism of action of CHANTIX™ (varenicline) [Last cited on 2007 Dec; Last updated on 2007]. Available from: https://www.pfizerpro.com/product_info/chantix_dual_action.jsp .
- 9.London: Royal College of Physicians of London; [Last cited on 2007 Dec 6; Last updated on 2000]. Tobacco Advisory Group of the Royal College of Physicians. Nicotine addiction in Britain; a report of the Tobacco Advisory Group of the Royal College of Physicians. Available from: http://www.rcplondon.ac.uk/pubs/books/nicotine . [Google Scholar]
- 10.Masjedi MR, Azaripour MH, Hosseini M, Heydari G. Effective factors on smoking cessation among the smokers in the first “smoking cessation clinic” in Iran. Tanaffos J Respir Dis. 2002;1:61–7. [Google Scholar]
- 11.Heydari G, Sharifi MH, Hosseini M, Masjedi MR. The effect of training and behavioral therapy recommendations on smoking cessation. Tanaffos J Respir Dis. 2003;2:39–44. [Google Scholar]
- 12.Heydari G, Marashian M, Ebn Ahmady A, Masjedi M, Lando HA. Which form of nicotine replacement therapy is more effective for quitting smoking? A study in Tehran, Islamic Republic of Iran. East Mediterr Health J. 2012;18:1005–10. doi: 10.26719/2012.18.10.1005. [DOI] [PubMed] [Google Scholar]
- 13.Heydari G, Talischi F, Tafti SF, Masjedi MR. Quitting smoking with varenicline: Parallel, randomised efficacy trial in Iran. Int J Tuberc Lung Dis. 2012;16:268–72. doi: 10.5588/ijtld.11.0183. [DOI] [PubMed] [Google Scholar]
- 14.Gaus RC, Satcher D. Rockville: US Department of Health and Human Services; 1996. Health Care Policy and Research. AHCPR Publication No. 96-0692. [Google Scholar]
- 15.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2004;3:CD000146. doi: 10.1002/14651858.CD000146.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Hughes J, Stead L, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2004;4:CD000031. doi: 10.1002/14651858.CD000031.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Geneva: WHO; 2001. World Health Organization. European partnership to reduce tobacco dependence: WHO evidence based recommendations on the treatment of tobacco dependence. [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC). Quitting smoking among adults – United States, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60:1513–9. [PubMed] [Google Scholar]
- 19.Boyle RG, Solberg LI, Fiore MC. Electronic medical records to increase the clinical treatment of tobacco dependence: A systematic review. Am J Prev Med. 2010;39:S77–82. doi: 10.1016/j.amepre.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 20.Linder JA, Rigotti NA, Schneider LI, Kelley JH, Brawarsky P, Haas JS. An electronic health record-based intervention to improve tobacco treatment in primary care: A cluster-randomized controlled trial. Arch Intern Med. 2009;169:781–7. doi: 10.1001/archinternmed.2009.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yunibhand J. Goyang: Republic of Korea; 2011. Thailand Report on Quit line Activities. Paper presented at: 2011 Asian Pacific Quit line Workshop; 7-8 Jun. [Google Scholar]


