Abstract
Background:
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in reproductive women. Nearly 10% of young women in this period involved. Although factors such as Insulin Resistance, hyper insulinemia, obesity and dietary are suggested to be associated with PCOS, cause of PCOS is not completely understood. Dairy products (a key component of the usual diet) of participants can also affect the factors of this disease and may have beneficial effects on treatment of PCOS. However, research in this area is scarce. The purpose of this study was to evaluate the relationship between dairy products consumption and PCOS.
Methods:
This descriptive cross-sectional study of 400 women was conducted in Shahid Beheshti Hospital of Isfahan University of Medical Science, Iran. Dietary intake was evaluated by validated food frequency questionnaire. Other variables such as ovarian disease, inherited predisposition, age at menarche, physical activity and history of other diseases were evaluated using questionnaire. Data analysis was performed by a logistic regression test using SPSS software version 15 Predictive analytics software and solutions.
Results:
There were a significant association between PCOS and ovarian disease (P < 0.001), age (P < 0.001) and using medication (P = 0.001). Body mass index (BMI) was inversely associated with PCOS, but it was not significant (P = 0.068). There was a significant direct relationship between milk consumption and risk of PCOS after adjusting for confounding factors (P = 0.028).
Conclusions:
The findings of this study indicated that ovarian disease and medication use is directly linked to PCOS. Dairy consumption was not significantly correlated with PCOS. However, after adjustment for confounders, there was an direct relationship between milk consumption and risk of PCOS.
Keywords: Dairy products, polycystic ovary syndrome, Infertility
INTRODUCTION
Polycystic ovary syndrome (PCOS) which was first reported in 1935 is known as one of the most common endocrine hormones disorders in the women of the reproductive age[1,2,3] afflicting as many as %10 of them.[4,5] The name of this syndrome has been derived from the appearance of the ovaries of the afflicted women (an ovary of enlarged size and full of cysts). These cysts are in the form of follicles filled with liquid sacs full of developed ovum.[6] Due to the lack of a set of standard and unified diagnostic criteria, the rate of prevalence of this syndrome reported in the different studies is varied. Some studies which used sonography as their diagnostic criteria found that the prevalence of PCOS ranged between 21% and 22% respectively.[7] On the contrary, in some other studies using oligomenerrhea and hyperandrogenemia manifestations as the PCOS's diagnostic criteria, the prevalence rate was reported to be 9%.[8]
The clinical symptoms of PCOS include amenorrhea, infertility, hirsutism and obesity.[9] This syndrome accounts for 30-40% of the common causes of infertility resulting from ovary dysfunctions. In addition, PCOS is considered as the most leading cause of ovary disorders.[9] As recent studies indicate, a person may have PCOS without showing one or some of the above-mentioned symptoms,[2,10] Some other symptoms and signs which can be enumerated for PCOS are as follows: Increased androgenic hormones, metabolic syndrome (insulin resistance), fat-related disorders, type 2 diabetes, cardiovascular disease, endometrial cancer and blood pressure.[11,12] The patients with PCOS also suffer from anxiety and depression some symptoms which are believed to be mostly a result of disorders occurred in the reproduction cycle which is naturally completed by releasing an ovum every month.[8] The exact cause of PCOS is not yet completely known, however, some factors such as insulin resistance/hyperinsulinaemeia, obesity, heredity and genetics factors, environmental factors such as exposure to high levels of masculinizing hormones, embryonic life cycle-related factors, hyperandrogenemia, gonadotropins secreting and functioning, hyperprolactinemia, hypothyroidism or thyroid-related dysfunctions, diet all may play a part in developing PCOS.[13,14,15] According to previous studies, the eating habits are not different between patients with PCOS and healthy persons but some foods seem to affect hormone parameters.[9] In the year 2008, one case-control study was carried out in Al-Zahra hospital of the city of Tabriz, Iran in which 60 women were studied, the results showed that the intake amounts of Ca, Mg, D vitamin, dairy, fruits and nuts and seeds were remarkably low among the women with PCOS. The frequency of their milk and dairy intakes products was also lower compared with the healthy women (P < 0.05).[9] Another study by Billaudel et al.[16] revealed that D vitamin and calcium play a critical role in insulin secretion and insulin-resistance in human and animal models. Another research on 103 women with PCOS and 103 healthy women provided some evidence on the decreased amount of adiponectine, calcium, D vitamin in the patients suffering from PCOS with having a higher thyroglobulin. There was also a significant correlation between adioponectrine and calcium concentrations (OH-D 25).[17] In one prospective study on 3157 young women aged 18-30, Pereira et al.[17] have reported in 2002 that the amount of dairy intake and insulin-resistance were indirectly related. A study by Pereira et al.[18] found an inverse relationship between consuming more than 4 units of dairy products per day and metabolic syndrome in the females. However, this relationship was not significant between males.[18]
As indicated in previous research, diet and dairy intake which itself is a source of calcium not only can trigger PCOS condition, but also may directly affect obesity and insulin-resistance, two factors which themselves act as the causes of PCOS. Numerous studies have demonstrated the association between the diet and its components and risk factors developing various diseases.[9] However, previous studies did not address the relationship between nutrition choices and type of diet chosen by the patients.[9]
The adverse health effects of PCOS such as infertility, diabetes, cardiovascular diseases and the growth in its prevalence, can impose huge financial and health costs on the society and can affect affecting many families. Therefore, taking preventive measures would have remarkable desirable outcomes. However, the number of studies which have addressed the relationship between dairy intake and PCOS is limited. Hence, the present study intends to explore the relationship between the amount of dairy intake and PCOS.
METHODS
Study design and participants
As a descriptive cross-sectional study, the present research tried to find the relationship between the amount of dairy consumption and PCOS condition in 400 women who referred to Shahid Beheshti hospital clinic in 2013. As far as exclusion and inclusion criteria of the study is concerned, it is noteworthy that the criteria for the inclusion in the study were willingness to participation, lack of precocious puberty, not having uterus cancer and not being pregnant. On the contrary, the subjects were excluded from the study if they were unwilling to participation, did not respond to more than 30 food items included in the food frequency questionnaire (FFQ), diagnosed with typical (chronic) diseases having to follow a specific diet.
Study instrument and variables assessment
At the start of the study, a written information-consent form was signed by the participants. The data related to the food intakes were checked by the researcher using FFQ, (In the FFQs the person were asked how often they consumed certain foods from a given lst of foods) the validity and reliability of which were previously confirmed.[19] The validity of the questionnaire was checked against daily food records. The data on the history of developing ovary dysfunctions (any endocrine disorders related to reproductive system), genetics background (having first related family members with ovarian disease), the age of the first menstruation, the history of thyroid diseases, the patients’ medication history (any kind of medicine used or any surgery), the period of developing PCOS and physical activity were collected by a nutritious expert using a self-developed questionnaire. The weight and height of the participants were also measured. To do so, the weight (kg) of the participants was measured with clothes but without shoes. The height of the participants was measured in a normal condition without wearing shoes using a strip tape. The body mass index (BMI) was calculated by dividing the weight (kg) value by the square root of height (m) value. The PCOS condition was identified through sonography diagnostic assessment with checking patients’ clinical manifestations performed by a trained authority.
Statistical analysis
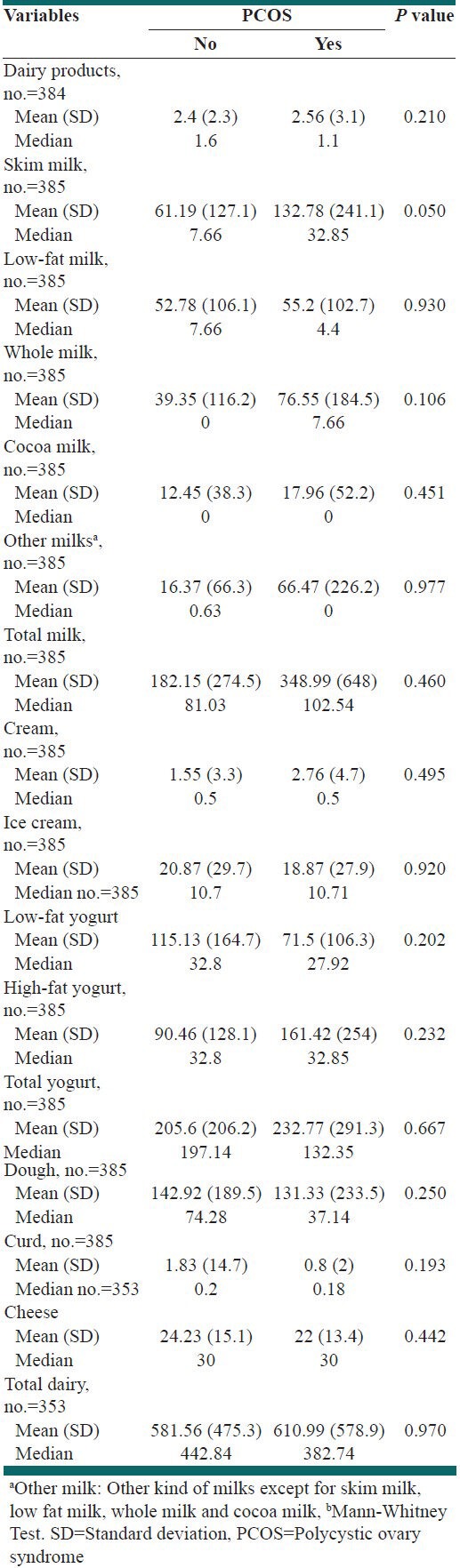
Data analysis was performed by descriptive analysis and logistic regression tests using SPSS software version 15. For age, age at menarch and BMI t-test was applied. Mann-Whitney t-test was applied for kcal while for other variables Chi-square test was applied [Table 1]. As shown in Table 2 for all variables Mann-Whitney test were used. The samples were selected by random sampling. The size of the sample was decided as many as 400. The study's confidence coefficient was considered at 95% and the level of strength of the study at 80%. Furthermore, the ratio of PCOS-afflicted patients and the sampling error were assumed to be 50% and 0.07%, respectively.
Table 1.
Frequency (%) and central tendency (spread) of some health condition characteristics of participants
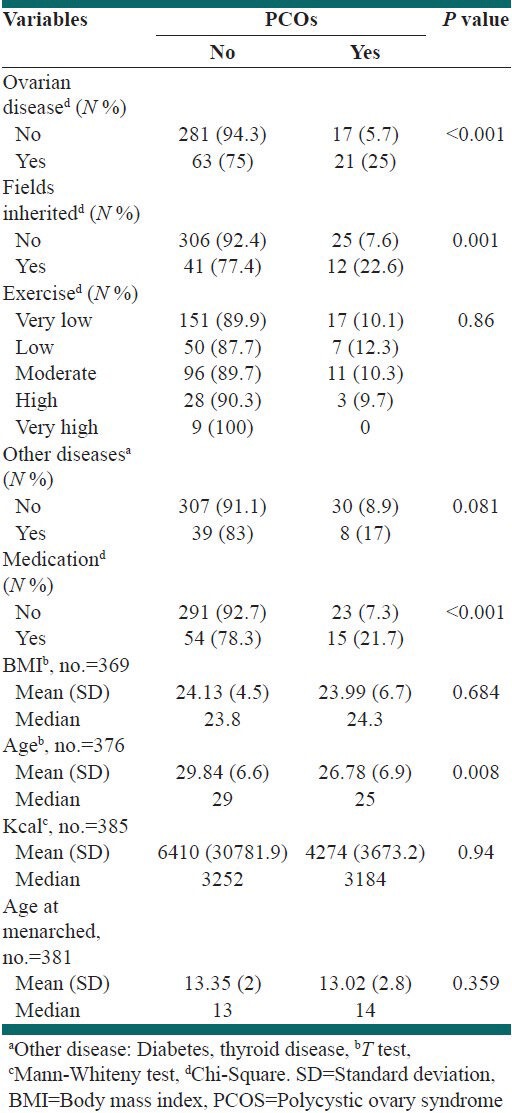
Table 2.
Frequency (%) and central tendency (spread) of food intake characteristics of sample population study
RESULTS
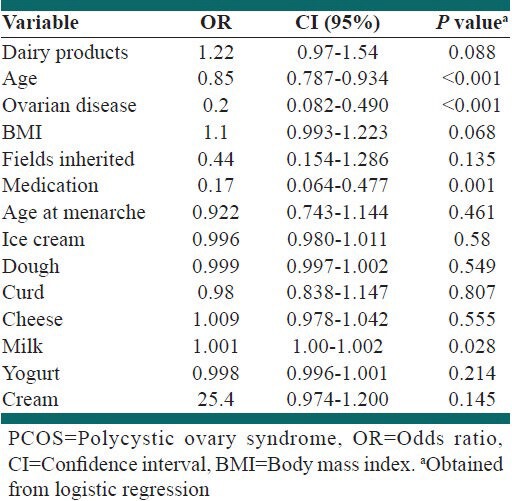
This study was carried out on 400 women of an mean ± standard deviation (SD) age of 29.5 ± 4.8 years old and an mean ± SD BMI of 24.1 ± 4.8 admitted to the Shahid Beheshti hospital. The prevalence of PCOS in the persons in the study was found to be 9.9%. Based on the primary analyses on the data (descriptive analysis), there was relationship between the history of ovarian diseases, genetics and the use of medications and PCOS. No relationship was observed between PCOS and other variables [Table 1]. As for the history of ovarian diseases, there was statistically significant difference between the patients with PCOS and healthy people (P < 0.001). As for the family history, a similar result was obtained so that 22.6% of the patients with PCOS were revealed having a family history of PCOS. On the contrary, there was no significant relationship between physical activity and PCOS (P = 0.86). A significant relationship was also observed between the use of medications and PCOS (P ≤ 0.001). The PCOS-afflicted patients and healthy persons did not show any difference in terms of weight and BMI. The average age of the patients with PCOS was 26.7 compared to 29.8 as the average age of the healthy persons. The two groups also differed in terms of the amount of calorie intake with 4247 kcal for the subjects with PCOS and 6410 kcal for the healthy subjects. The average age of the first menstrual period was found to be 13.35 years among the healthy individuals and 13.02 years among the individuals afflicted with PCOS [Table 1]. The average sum of dairy intake was 581.5 and 611 g for the healthy persons and patients with PCOS, respectively [Table 2]. The results from using logistic regression revealed that there was no association between genetics and PCOS (P = 0.13) [Table 3]. On the contrary, a negative relationship was observed between the history of ovary diseases. (P < 0.001 odds ratio [OR] =0.2 confidence interval [CI] (95%) =0.082-0.490), age (P < 0.001, OR = 0.85 CI (95%) =0.787-0.934) and the use of medication as three confounding variables (P = 0.001 OR = 0.17 CI (95%) =0.064-0.477) and PCOS [Table 3]. Based on the results, BMI and PCOS were not significantly related but their relationship may be remarkable (P = 0.068). Every one-unit increase in the BMI was accompanied by an increase in the risk of affliction with PCOS. There was a direct relationship between the exchange portion of dairy and PCOS. Although like BMI, this relationship was not significant but remarkable (P = 0.088). After modifying the effects of confounding variables, a direct significant relationship was found between the intake of milk and PCOS (P = 0.028) so that every 1-unit increase in the milk intake led to a %1-increase in the risk factors [Table 3].
Table 3.
Summary of PCOSs risk factors
DISCUSSION
In the present study we evaluated the effects of dairy product on PCOS. According to the results of this study, no significant relationship was observed between each component of dairy foods group and other variables with PCOS. However, after modifying the effects of confounding variables, it was found that the milk intake and PCOS were directly related.
Very few studies have been conducted on exploring the direct effect which dairy foods may have on PCOS. The results of empirical research on the effect of dairy foods on the weight which itself is believed to be one of the effective factors of infliction with PCOS are inconsistent without producing a rigid and strong outcome.[20] The results of available clinical evaluations especially those who address the effects of a diet rich in dairy foods on the weight do not yield a fixed outcome.
The results of some previous studies are in line with our results. According to Adebamowo et al., there is a relationship between slim/low-fat or free-fat milk and increased frequency of acne, a component of the PCOS.[21] two intervention studies (Thompson et al. and Harvey-Berino, et al.) provided no evidence on an additional weight loss when choosing a diet rich in dairy foods compared with a low-dairy diet.[22,23] These studies both used obese subjects as their samples. The results of these studies were similar to those of one earlier research by Zemel et al. (2004) with a study period of 12 weeks. However, the periods of these two recent studies in which no association was observed between the variables in question was 48 weeks and 52 weeks, respectively. The findings of a 3-year prospective study on a large number of children and young adults revealed that the subjects with a higher intake of milk had a higher BMI. Although this reported increase was very trivial per year, adjusting for a number of body weight factors, it was statistically significant.[24]
Chavarro et al. in their prospective cohort study found that high intake of low-fat dairy products may lead to an increase in the women's risk of ovulation-related infertility, while incorporating more high-fat dairy foods may decrease its risk.[25] Cramer et al. (1994) reported a positive association between intakes of milk and age-related decreased fertility rates in 31 nations. To put it differently, consuming milk accounted for 36% of the variation in the age-related infertility.[26] Gunther et al.[27] in their study divided 155 women of normal weight into three sub-categories as per their amount of dairy foods intake within 1 year, while their diets during intervention were the same in terms of caloric value. Although the results of the study did not support the hypothesis related to the dairy foods intake and weight loss, following 51 of the healthy women participating in the study for a 6-month period after the study revealed that compared to those with a low intake of dairy foods, those who had a diet of high dairy intake had a lower fat accumulation.[27] Results of some previous studies are not in line with our findings. In two studies by Zemel et al.[28,29] a considerable decrease was reported for BMI and waist circumference with a notable decrease in the plasma insulin. In one case-control study, Dixon, et al. argued that there is an intricate association between obesity and dairy products intake concluding that for the children of higher age,[7,8,9,10] there was an inverse association between the intake of dairy foods and obesity.[30] By analyzing a number of databases, a group of cross-sectional studies on the adults and children almost demonstrated the inverse relationship between the intake of dairy foods and initial obesity. The samples used in these studies were mostly selected from among post-menopausal middle-aged women.[20] Carruth and Skinner in their research on a group of preschool children concluded that the number of servings estimated per day is obviously inversely related to the fat accumulation and positively related to the individuals’ slimness. In particular, each serving resulted in an additional weight loss up to 0.9-1.1 kg.[27]
As for consuming dairy foods and insulin resistance relationship, a cross-sectional study conducted on 496 samples of participants aged 20-68 aged in 2009 can be enumerated. This study tried to assess the amounts of consumed dairy foods using a food history questionnaire the validity of which had been checked. Based on the results, compared with other groups, the samples situated on the top quarter of the intake of dairy products had the lowest mean scores for insulin resistance markers. Although the observed differences were not statistically significant, eating whole-fat dairy products was inversely associated with HOMA-IR. In contrast, there was no relationship between low-fat dairy products and insulin resistance markers.[31] A case-control study by Keshavarzi demonstrated that the risk of infertility among the women who ate 3 or more glasses of milk per day was lower than those with no intake of milk as much as 70%.[32] Most of these studies were done on obese subjects, children or on adolescents. On the whole, the findings of this study indicated that there was no statistically significant relationship between consuming milk, yogurt, sherbet/frozen yogurt, cheese and cream and PCOS. Conversely, it became evident that PCOS and the history of ovarian diseases (P < 0.001), age (P < 0.001) and the use of medication (P = 0.001) as three confounding variables were inversely related. Furthermore, although no statistically significant relationship was obtained between BMI and PCOS, it was at the threshold of being significant (P = 0.068). Every one-unit increase in BMI is associated with a 10% increase in the risk of PCOS. Of course, this relationship was no significant. There was also a positive relationship between the dairy substitutes’ units and PCOS. Similar to BMI, this relationship was insignificant (being at the threshold of significance, P = 0.0880. After modifying the effects of confounding variables, a statistically significant relationship was observed between milk intake and risk of PCOS (P = 0.028) Hence that every 1-unit increase in the amount of milk consumed caused a 1%-increase in the risk of PCOS. There is no study addressing the relationship between the history of ovarian diseases and PCOS. As for the relationship between the use of medication and PCOS, the research suggest that since the medications used by the majority of the participants were metformin, anti-fertility as well as thyroid medications, they helped prevent developing PCOS due to their effect on androgen secretion and luteinizing hormone/follicle-stimulating hormone ratio. Based on past research, the higher the age, makes the lower the possibility of PCOS.[15]
Affecting ovulation, dairy foods may lead to infertility. However, it is noteworthy that yielding inconsistent results, few studies have addressed this issue. If the women with PCOS or those who are suspicious of having it make some changes in their diets, for instance choosing low-fat dairy foods instead of high-fat ones, a positive relationship between these changes and anovulatory infertility would be expected. Foods factors relevant to the augmentation of the phenotype attributes of PCOS may increase infertility risk due to disturbed ovulation.[25]
The current study revealed that the average intake of milk and PCOS had significant relationship. To explain more, on the average the total intake of low- and free-fat milk was estimated to be 52 ± 61 (gr) and 55 ± 132 (gr) for the healthy and patient individuals, respectively. The average amount of low- and free-fat milk consumption was found to be 12.4 ± 39.35 (gr) for the healthy persons and 76.55 (gr) for the PCOS patients. Furthermore, the individuals with PCOS condition, revealed to have a higher consumption of low- and free-fat milk. As per the results of the past studies, there is a positive relationship between low-fat milk and PCOS. Low-fat dairy products may increase the level of insulin like growth factor I (IGF-I). As some researchers have controversies, IGF-I may have a role in the pathogenesis of PCOS. The IGF-I existing in the human ovarian cells may stimulate the cell activity-related changes observed in the PCOS. It is not yet known whether the change in the level of IGF-I caused by diet may contribute to the PCOS's clinical manifestations or not.[32] As the research suggest, the fatty acids of dairy products may have potential positive effects on the ovary function. In more details, the substance soluble in the fat available in the dairy products plays the essential role in creating such effects. Compared with low-fat dairy products, whole milk and fat-rich dairy products have a higher estrogen concentration. Since estrogen can decrease the level of IGF-I,[30] their existence in high-fat dairy foods may explain the observed association.[30] The frequent increased insulin sensitivity in the high-fat dairy consumers may improve their ovulation performance. Eating low-fat dairy foods has also been accompanied by an excess of androgens secretion known as one of components of PCOS.[9] One of the weak points of this study is its cross-sectional design which fails to identify the cause-effect relationships. In addition, hormone tests such as thyroid, prolactine and HOMA-IR tests were not taken from the subjects. In contrast, some strength points that can be mentioned for this study include: The large number of the samples, lack of similar study in Iran directly addressing the relationship between dairy products intake and PCOS, evaluating the foods intakes using a validated FFQ, using sonography test known as the most reliable method for PCOS diagnose.
CONCLUSIONS
Based on the findings of the study, milk intake and prevalence of PCOS may be related in some way. Due to the adverse health effects of this condition, its high prevalence in the society as well as the shortage of research on the effectiveness of diets on preventing and treating it, the need to more research is felt. In the future research, it is better to address laboratory practices such as thyroid, prolactine and sexual hormones, as well.
ACKNOWLEDGMENTS
I express my sincere and utmost gratitude to the manager of Shahid Beheshti hospital for his help and cooperation during different stages of conducting the present research and all the participants for their assistance and support. This study was extracted from Msc dissertation which was approved by School of Nutrition & Food Sciences, Isfahan University of Medical Sciences (code 392169) in acknowledgement section.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fumeron F, Lamri A, Abi Khalil C, Jaziri R, Porchay-Baldérelli I, Lantieri O, et al. Dairy consumption and the incidence of hyperglycemia and the metabolic syndrome: Results from a French prospective study, Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR) Diabetes Care. 2011;34:813–7. doi: 10.2337/dc10-1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moran LJ, Noakes M, Clifton PM, Tomlinson L, Galletly C, Norman RJ. Dietary composition in restoring reproductive and metabolic physiology in overweight women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2003;88:812–9. doi: 10.1210/jc.2002-020815. [DOI] [PubMed] [Google Scholar]
- 3.Gambineri A, Patton L, Vaccina A, Cacciari M, Morselli-Labate AM, Cavazza C, et al. Treatment with flutamide, metformin, and their combination added to a hypocaloric diet in overweight-obese women with polycystic ovary syndrome: A randomized, 12-month, placebo-controlled study. J Clin Endocrinol Metab. 2006;91:3970–80. doi: 10.1210/jc.2005-2250. [DOI] [PubMed] [Google Scholar]
- 4.Le Donne M, Alibrandi A, Giarrusso R, Lo Monaco I, Muraca U. Diet, metformin and inositol in overweight and obese women with polycystic ovary syndrome: Effects on body composition. Minerva Ginecol. 2012;64:23–9. [PubMed] [Google Scholar]
- 5.Pasquali R, Gambineri A, Cavazza C, Ibarra Gasparini D, Ciampaglia W, Cognigni GE, et al. Heterogeneity in the responsiveness to long-term lifestyle intervention and predictability in obese women with polycystic ovary syndrome. Eur J Endocrinol. 2011;164:53–60. doi: 10.1530/EJE-10-0692. [DOI] [PubMed] [Google Scholar]
- 6.Lyon F, Aspyraf L. 8th ed. Golban Nashr; 2011. Translation of Women of Clinical Endocrinology and Infertility Aspyraf. [Google Scholar]
- 7.Pirak A, Kashani ZA, Azarkish F, Salehian T, Hagani H, Parsania Z, et al. A study on correlation between gestational diabetes and history polycystic ovary syndrome in women referred to Akbar Abady Hospital in Tehran 1998-2005. Sci J Ilam Univ Med Sci. 2009;17:17–25. [Google Scholar]
- 8.Motta AB. The role of obesity in the development of polycystic ovary syndrome. Curr Pharm Des. 2012;18:2482–91. doi: 10.2174/13816128112092482. [DOI] [PubMed] [Google Scholar]
- 9.Gargari BP, Hojaghani SH, Mahbum SH, Farzdi L, Safaeian A. The comparison of food pattern in women with polycystic ovary syndrome with healthy women. J Obstet Gynaecol Infertil. 1390;14:1–8. [Google Scholar]
- 10.Zhai HL, Wu H, Xu H, Weng P, Xia FZ, Chen Y, et al. Trace glucose and lipid metabolism in high androgen and high-fat diet induced polycystic ovary syndrome rats. Reprod Biol Endocrinol. 2012;10:5. doi: 10.1186/1477-7827-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson AL, Harris TB, Tylavsky FA, Perry SE, Houston DK, Lee JS, et al. Dietary patterns, insulin sensitivity and inflammation in older adults. Eur J Clin Nutr. 2012;66:18–24. doi: 10.1038/ejcn.2011.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kasim-Karakas SE, Cunningham WM, Tsodikov A. Relation of nutrients and hormones in polycystic ovary syndrome. Am J Clin Nutr. 2007;85:688–94. doi: 10.1093/ajcn/85.3.688. [DOI] [PubMed] [Google Scholar]
- 13.Kachoie A, Jahanipoor A, Ghahiri A. Evaluation of serum prolactin levels in patients with polycystic ovary syndrome. J Isfahan Med Sch. 2012;30:353–8. [Google Scholar]
- 14.Barba G, Russo P. Dairy foods, dietary calcium and obesity: A short review of the evidence. Nutr Metab Cardiovasc Dis. 2006;16:445–51. doi: 10.1016/j.numecd.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Hajishafieha M. Causes and Treatment of Chronic Anovulation. Institute Publications Shahed and Isargaran Uromieh Medical University. 1993:258. [Google Scholar]
- 16.Billaudel BJ, Bourlon PM, Sutter BC, Faure-Dussert AG. Regulatory effect of 1,25-dihydroxyvitamin D3 on insulin release and calcium handling via the phospholipid pathway in islets from vitamin D-deficient rats. J Endocrinol Invest. 1995;18:673–82. doi: 10.1007/BF03349788. [DOI] [PubMed] [Google Scholar]
- 17.Spence LA, Cifelli CJ, Miller GD. The role of dairy products in healthy weight and body composition in children and adolescents. Curr Nutr Food Sci. 2011;7:40–9. doi: 10.2174/157340111794941111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pereira MA, Jacobs DR, Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: The CARDIA Study. JAMA. 2002;287:2081–9. doi: 10.1001/jama.287.16.2081. [DOI] [PubMed] [Google Scholar]
- 19.Hosseini-Esfahani F, Asghari G, Mirmiran P, Farahani PJ, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the theran lipid and glucose study. Razi J Med Sci. 2010;17:41–55. doi: 10.2188/jea.JE20090083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Warensjo E, Nolan D, Tapsell L. Dairy food consumption and obesity-related chronic disease. Adv Food Nutr Res. 2010;59:1–41. doi: 10.1016/S1043-4526(10)59001-6. [DOI] [PubMed] [Google Scholar]
- 21.Adebamowo CA, Spiegelman D, Danby FW, Frazier AL, Willett WC, Holmes MD. High school dietary dairy intake and teenage acne. J Am Acad Dermatol. 2005;52:207–14. doi: 10.1016/j.jaad.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Thompson WG, Rostad Holdman N, Janzow DJ, Slezak JM, Morris KL, Zemel MB. Effect of energy-reduced diets high in dairy products and fiber on weight loss in obese adults. Obes Res. 2005;13:1344–53. doi: 10.1038/oby.2005.163. [DOI] [PubMed] [Google Scholar]
- 23.Harvey-Berino J, Gold BC, Lauber R, Starinski A. The impact of calcium and dairy product consumption on weight loss. Obes Res. 2005;13:1720–6. doi: 10.1038/oby.2005.210. [DOI] [PubMed] [Google Scholar]
- 24.Zemel MB. Role of calcium and dairy products in energy partitioning and weight management. Am J Clin Nutr. 2004;79:907S–12. doi: 10.1093/ajcn/79.5.907S. [DOI] [PubMed] [Google Scholar]
- 25.Chavarro JE, Rich-Edwards JW, Rosner B, Willett WC. A prospective study of dairy foods intake and anovulatory infertility. Hum Reprod. 2007;22:1340–7. doi: 10.1093/humrep/dem019. [DOI] [PubMed] [Google Scholar]
- 26.Cramer DW, Xu H, Sahi T. Adult hypolactasia, milk consumption and age-specific fertility. Am J Epidemiol. 1994;139:282–9. doi: 10.1093/oxfordjournals.aje.a116995. [DOI] [PubMed] [Google Scholar]
- 27.Gunther CW, Legowski PA, Lyle RM, McCabe GP, Eagan MS, Peacock M, et al. Dairy 15 products do not lead to alterations in body weight or fat mass in young women in a 1-y intervention. Am J Clin Nutr. 2005;81:751–6. doi: 10.1093/ajcn/81.4.754. [DOI] [PubMed] [Google Scholar]
- 28.Zemel MB, Richards J, Mathis S, Milstead A, Gebhardt L, Silva E. Dairy augmentation of total and central fat loss in obese subjects. Int J Obes. 2005;29:391–7. doi: 10.1038/sj.ijo.0802880. [DOI] [PubMed] [Google Scholar]
- 29.Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res. 2004;12:582–90. doi: 10.1038/oby.2004.67. [DOI] [PubMed] [Google Scholar]
- 30.Dixon LB, Pellizzon MA, Jawad AF, Tershakovec AM. Calcium and dairy intake and measures of obesity in hyperand normocholesterolemic children. Obes Res. 2005;13:1727–38. doi: 10.1038/oby.2005.211. [DOI] [PubMed] [Google Scholar]
- 31.Akter S, Kurotani K, Nanri A, Pham NM, Sato M, Hayabuchi H, Mizoue T. Dairy consumption is associated with decreased insulin resistance among the Japanese. Nutr Res. 2013;33:286–92. doi: 10.1016/j.nutres.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 32.Greenlee AR, Arbuckle TE, Chyou PH. Risk factors for female infertility in an agricultural region. Epidemiology. 2003;14:429–36. doi: 10.1097/01.EDE.0000071407.15670.aa. [DOI] [PubMed] [Google Scholar]


