Abstract
Background:
The aim of the current study was twofold: To investigate the effect of veteran status on risk of developing heart disease over a period of 20 years in the United States and to test if socio-economic characteristics, chronic conditions, health behaviors, body mass index (BMI) and depressive symptoms explain the association between veteran status and risk of heart disease.
Methods:
Data came from the Health and Retirement Study, a 20 year national cohort from 1992 to 2012. The study enrolled a representative sample of Americans over the age of 50. We included 8,375 individuals who were older than 50 years at entry, did not have heart disease at baseline and provided data on heart disease over the next 20 years. Veteran status was considered to be the independent variable. Self-reported data on physician diagnosis of heart disease, which was measured on a biannual basis, was the outcome. Baseline socio-economic data (i.e. age, gender, race, marital status and education), chronic conditions (diabetes and hypertension), health behaviors (i.e. drinking, smoking, and exercise), BMI and depressive symptoms (modified Center for Epidemiologic Studies Depression Scale) were entered into logistic regressions. Logistic regression was used for data analysis.
Results:
Veterans were at higher risk of having a new onset of heart disease (unadjusted relative risk [RR] = 1.996, 95% confidence interval [CI] =1.694-2.351), compared with non-veterans. Logistic regression confirmed the association between veteran status and heart disease (adjusted RR = 1.483, 95% CI = 1.176-1.871) after controlling for all covariates.
Conclusions:
Veterans may be at higher risk for heart disease over time and this link may be independent of baseline socio-economic characteristics, chronic medical conditions, health behaviors, BMI and depressive symptoms. Veterans may require more rigorous cardiovascular prevention programs.
Keywords: Cohort, depression, drinking, exercise, heart disease, smoking, veterans
INTRODUCTION
About 65% of American men over the age of 55 have served in World War II or other wars.[1,2] Veterans are at higher risk of poor physical health[3,4] and mental health.[5] They also more frequently report health compromising behaviors such as smoking.[6] The long-term health outcomes among veterans, however, have been less frequently studied. As a result, veteran status is being called a “hidden variable” in the aging of older Americans.[1,7]
Although there is some evidence suggesting that veterans may be at higher risk for cardiovascular disease (CVD),[1,2,7,8,9,10,11,12] studies on long-term cardiovascular health of veterans are inconclusive.[1,13] Veterans have higher rates of mental illnesses such as depression[2] and post-traumatic stress disorder (PTSD).[1,7,8,9,10] Both depression and PTSD are associated with increased CVD risk.[14,15] High prevalence of mental health problems may partially mediate the higher rate of CVD among veterans.
Controlling for depression has been shown to weaken the association between veteran status and heart disease.[2] Race and gender may also influence pattern of CVD risk factors among veterans.[16] Although literature has consistently suggested that veterans with mental disorders such as PTSD are at higher risk of cardiovascular morbidity and mortality,[1,2,7,8,9,10] evidence is lacking about the link between veteran status – per se – and CVD.
The aim of this study was twofold: (1) To test if veterans are at a higher risk of new onset heart disease over 20 years in the United States and (2) to test if the above association is independent of socio-economics,[16] physical health,[3,4] mental health,[5] and health compromising behaviors.[6] Information on the links between veteran status, traditional CVD risk factors and CVD risk is hoped to inform efforts to ultimately prevent CVD among veterans.[17]
METHODS
Study design and participants
This study used the Health and Retirement Study (HRS) data to study the effect of veteran status at year 1992 on the development of heart disease in the United States from 1992 to 2012. The HRS is a longitudinal cohort that has enrolled a representative sample of Americans over the age of 50. Since its launch in 1992, the study has followed the participants for 20 years, and has interviewed them every 2 years.
The HRS has collected data about socio-economic status, physical health, functioning, mental health and health care utilization. The University of Michigan Institutional Review Board approved the study. The study design and sampling have been described in detail elsewhere.[18,19]
The HRS has been designed to collect information on persons from pre-retirement into retirement. The study was intended to provide scientists with data to generate more accurate models of the health causes and consequences associated with aging and retirement, and also to provide policy-makers with up-to-date information on disability patterns associated with retirement. Thus, the HRS explored the health transitions that individuals undergo toward the end of their work lives and in the years that follow.
Participants of the HRS cohort were comprised of people who were born between 1931 and 1941 and were 51-61 years of age. The first interview took place in 1992. We only included 8,375 individuals who did not have heart disease at baseline and had data on all waves during the next 20 years.
Interview and measures
Data was collected using face-to-face interviews. Interviews were conducted within participants’ homes. Participants received compensation for participating in this study.
Socio-economic data
We used data on race, ethnicity, age, gender, education and marital status. The respondent was asked if they consider their race to be White or Caucasian, Black or African American, American Indian, Asian, or something else. Ethnicity included Hispanic or Latino.
Depressive symptomatology
A modified nine-item version of the Center for Epidemiologic Studies Depression Scale was used to measure depressive symptoms.[20] Participants reported whether during the past week they had felt (a) depressed, (b) everything was an effort, (c) sleep was restless, (d) happy, (e) lonely, (f) that he or she enjoyed life, (g) sad, (h) that he or she could not get going and (i) that he or she had a lot of energy. Factor analytic studies have identified the following three subscales for this measure: Somatic (items 2, 3, 8 and 9), lack of positive affect (items 4 and 6) and dysphoria (items 1, 5 and 7).[21] A higher score reflects negative affect. The measure displays acceptable internal consistency (a = 0.80 - 0.83).[22]
Smoking
Two items were used to measure smoking behavior at baseline. In the first item, the participant was asked if they have ever smoked and in the second item, they were asked if they currently smoked. Using both items, we categorized individuals into never smokers, previous smokers and current smokers.
Exercise
Three items were used to measure physical activity and exercise. Cronbach's alpha of the measure was 0.792.
Heart disease
Participants reported if a doctor had ever told them that they had any heart conditions including heart attacks, angina, congestive heart failure, or coronary heart disease (CHD). If respondents reported “yes” in the previous wave of data and “no” in the current wave, their response was coded as “no.”[23]
Statistical analysis
Data were downloaded from the HRS website, Institute for Social Research, University of Michigan (http://hrsonline.isr.umich.edu/). Due to the complex sample design used in the HRS, Stata 13.0 (Stata Corp., College Station, TX) was used for data analysis. Taylor series linearization was used for estimation of standard errors. Thus, the stratified and clustered nature of data, in addition to the non-response pattern, were considered for data analysis. Using weights enabled us to provide rates which are generalizable to the US population.
We used six logistic regressions to test the association between veteran status at baseline and risk of heart disease over 20 years among the participants. Veteran status and covariates including baseline socio-economic characteristics (i.e. age, gender, race, marital status and education), chronic conditions (diabetes and hypertension), health behaviors (i.e. drinking, smoking and exercise), body mass index (BMI) and depressive symptoms were gradually added to Models I to VI. Relative risk (RR) with 95% confidence intervals (CI) were reported. RR greater than 1 shows higher chance of heart disease over 20 years.
Before our modeling, we ruled out possible multi-collinearity between our covariates. Based on tolerance value or variance inflation factor, we did not find any sign of multi-collinearity between the predictors.[24] We did not impute missing data for this study. P < 0.05 were considered to be statistically significant.
RESULTS
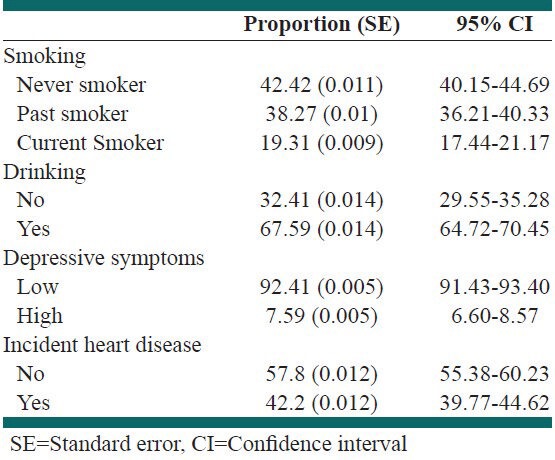
As shown in Table 1, most participants were women (54%) and Whites and non-Hispanics (95%). About 8% had high depressive symptoms. Nearly 42% were never smokers, 38% were past smokers and 19% were current smokers. About 68% reported drinking alcohol. 42% developed new CHD during the 20 years of follow-up [Table 2].
Table 1.
Proportion of socioeconomic status among participants
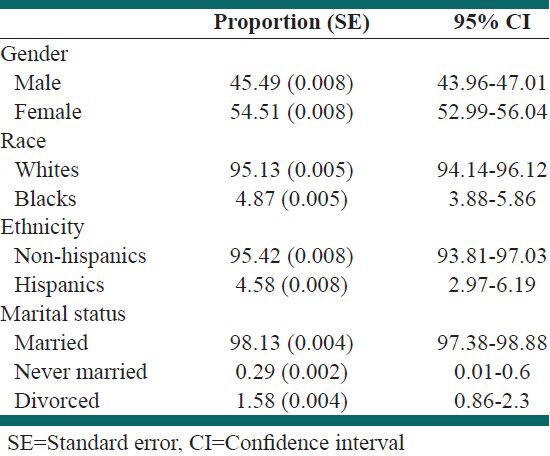
Table 2.
Proportion of behaviors, depression and heart disease among participants
Model I, which did not control for any covariate, suggested that veterans were at higher risk of new CHD during the 20 years of follow-up (RR = 1.691, 95% CI = 1.244-2.298) [Table 3].
Table 3.
Summary of logistic regressions among participants (Model I, II, III, and IV)
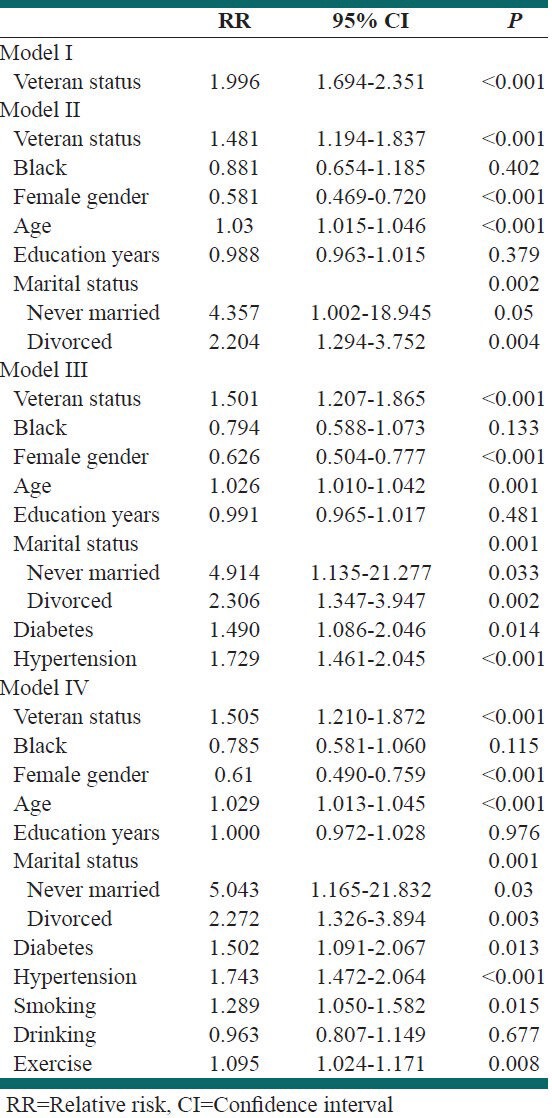
Model II, which controlled for socio-economic characteristics, suggested that veterans had a higher rate of new CHD during the 20 years of follow-up (RR = 1.481, 95% CI = 1.194-1.837) [Table 3].
Model III controlled for socio-demographic data and chronic conditions and suggested that veteran status was linked to higher risk of new CHD during 20 years of follow-up (unadjusted RR = 1.501, 95% CI = 1.207-1.865) [Table 3].
Model IV, which controlled for socio-demographic data, chronic conditions and health behaviors suggested that veterans have higher risk of new CHD during the 20 years of follow-up (RR = 1.505, 95% CI = 1.210-1.872) [Table 3].
Model V which controlled for socio-demographic characteristics, chronic conditions, health behaviors and BMI suggested that veteran status is associated with higher risk of new CHD during the 20 years of follow-up (adjusted RR = 1.504, 95% CI = 1.209-1.871) [Table 4].
Table 4.
Summary of logistic regressions among participants (Model V and Model VI)
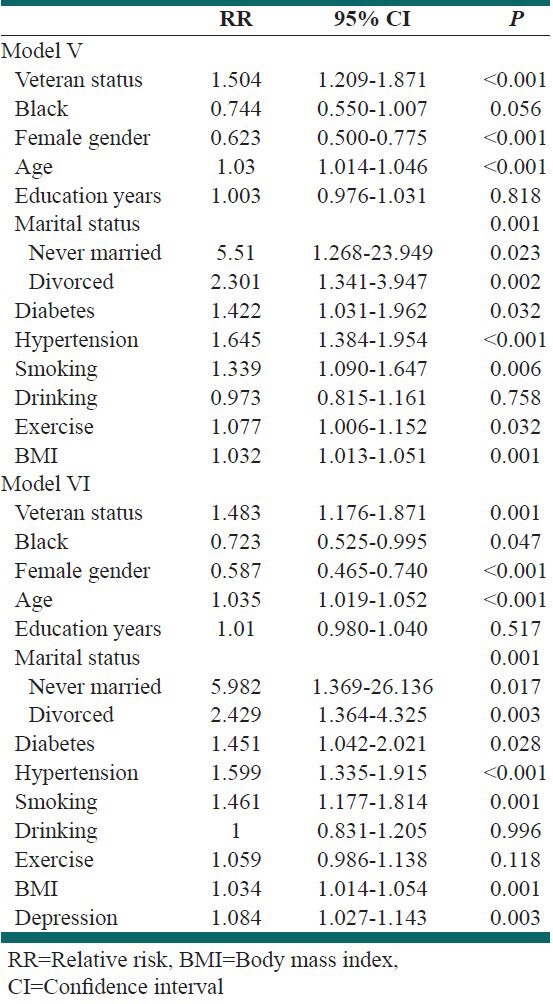
Model VI which controlled for socio-demographics, chronic conditions, health behaviors, BMI and depression, suggested that veteran status is associated with higher risk of new CHD during the 20 years of follow-up (adjusted RR = 1.483, 95% CI = 1.176-1.871) [Table 4].
DISCUSSION
With a longitudinal design, the current study showed that veterans are at higher risk of CVD over a period of 20 years. Our study also suggested that such link is independent of socio-demographic characteristics, comorbid conditions, health behaviors, BMI and depressive symptoms at baseline. Our finding is in line with other studies suggesting that veterans may be at an increased risk of CVD.[1,2,7,8,9,10,11,12]
Our study suggested that the link between veteran status and CVD risk is independent of socio-demographic characteristics, comorbid conditions, health behaviors, BMI and depressive symptoms at baseline. Veterans have higher rates of mental illnesses such as depression and PTSD, which are associated with an increased risk of CVD.[14,15] Depression[2] and PTSD[1,7,8,9,10] have been suggested to be factors that may partially explain the higher rate of CVD among veterans.
The link between veteran status and heart disease was above and beyond depressive symptoms. Vietnam veterans with PTSD have been shown to be more likely to have physician-diagnosed circulatory diseases and abnormal electrocardiograph results nearly 20 years after military service.[7,8] Vietnam veterans with PTSD are also more likely to die from cardiovascular-related diseases 30 years after military service.[1] Studies involving World War II and Korean War veterans have also reported higher rates of physician-diagnosed CVD among veterans who suffer from PTSD.[9] Among US Civil War veterans, exposure to war trauma has been positively associated with post-service cardiovascular ailments.[10] There are studies suggesting that controlling for depression may weaken the association between veteran status and heart disease.[2]
Race and gender may complicate the link between veteran status and CVD risk and risk factors.[16] Although most previous studies have reported that a specific group of veterans (those with mental disorders such as PTSD) are at higher risk of cardiovascular morbidity and mortality,[1,2,7,8,9,10] the current study suggests that veteran status – per se – may be a risk factor for CVD.
This study showed that depressive symptoms also predict future heart disease. Prospective studies have consistently suggested that negative affect predicts CAD.[25,26,27,28,29] Depression has been reported to be associated with CAD morbidity and mortality, even after controlling for traditional CAD risk factors, such as cholesterol level, blood pressure and smoking.[27,30,31] Although multiple behavioral pathways have been proposed to explain the mechanism by which depression may be linked to the development and progression of CAD,[32,33] our study suggests that the link between depression and CAD may be independent of smoking, exercise and BMI.
Findings of the current study may have important clinical or public health implications. The results can be used for primary prevention of heart disease among veterans in the United States. One of five older adults in the US (aged ≥65 years) has CAD.[34,35] Future studies should investigate if interventions targeted at veterans will reduce morbidity and mortality associated with CAD in the general population or not.
We suggest that veterans with high BMI, those who smoke, have high depressive symptoms and have diabetes and hypertension but have not yet developed heart disease should receive interventions for prevention of heart disease. Based on our findings, independent of traditional CVD risk factors, veterans should be considered as a high-risk population for CVD and should receive targeted interventions to reduce their risk of heart disease. Understanding the link between veteran status, traditional CVD risk factors and CVD risk may need further research, and the information provided may collectively reduce the burden of CVD among veterans.[17]
The current study had a few limitations. First, the study did not use time to event analysis. Use of Cox regression and survival analysis could provide more information on differences in timing of development of CVD across veterans and non-veterans. In addition, the study used self-reported physician diagnosis of CVD as outcome. Although this outcome is valid, evaluation of heart disease could result in more accurate results. Furthermore, the study measured depressive symptoms, not clinical disorder for major depressive disorder. Finally, the study only controlled for baseline confounders. As socio-economic status, CVD risk factors, BMI and health behaviors such as smoking are subjected to change over time, future research can benefit from conceptualizing these confounders or mediators as time-varying covariates.
CONCLUSIONS
Among individuals older than 50 in the United States, veterans are at a higher risk of heart disease over the span of 20 years. This risk seem to be independent of baseline socio-economic characteristics, chronic medical conditions, health behaviors, BMI and depressive symptoms.
ACKNOWLEDGMENTS
We used public use dataset available at the study website at University of Michigan. The HRS is conducted by the Survey Research Center, Institute for Social Research, University of Michigan. The National Institute on Aging (NIA) provided funding for the Health and Retirement Study (U01 AG09740).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16:248–56. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Boscarino JA. A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: Implications for surveillance and prevention. Psychosom Med. 2008;70:668–76. doi: 10.1097/PSY.0b013e31817bccaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Findley P, Shen C, Sambamoorthi U. Multimorbidity and persistent depression among veterans with diabetes, heart disease, and hypertension. Health Soc Work. 2011;36:109–19. doi: 10.1093/hsw/36.2.109. [DOI] [PubMed] [Google Scholar]
- 4.Smith NL, Chen L, Au DH, McDonell M, Fihn SD. Cardiovascular risk factor control among veterans with diabetes: The ambulatory care quality improvement project. Diabetes Care. 2004;27(Suppl 2):B33–8. doi: 10.2337/diacare.27.suppl_2.b33. [DOI] [PubMed] [Google Scholar]
- 5.Hofmann SG, Litz BT, Weathers FW. Social anxiety, depression, and PTSD in Vietnam veterans. J Anxiety Disord. 2003;17:573–82. doi: 10.1016/s0887-6185(02)00227-x. [DOI] [PubMed] [Google Scholar]
- 6.O’Toole BI, Catts SV, Outram S, Pierse KR, Cockburn J. The physical and mental health of Australian Vietnam veterans 3 decades after the war and its relation to military service, combat, and post-traumatic stress disorder. Am J Epidemiol. 2009;170:318–30. doi: 10.1093/aje/kwp146. [DOI] [PubMed] [Google Scholar]
- 7.Boscarino JA, Chang J. Electrocardiogram abnormalities among men with stress-related psychiatric disorders: Implications for coronary heart disease and clinical research. Ann Behav Med. 1999;21:227–34. doi: 10.1007/BF02884839. [DOI] [PubMed] [Google Scholar]
- 8.Boscarino JA. Diseases among men 20 years after exposure to severe stress: Implications for clinical research and medical care. Psychosom Med. 1997;59:605–14. doi: 10.1097/00006842-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Schnurr PP, Spiro A, 3rd, Paris AH. Physician-diagnosed medical disorders in relation to PTSD symptoms in older male military veterans. Health Psychol. 2000;19:91–7. doi: 10.1037//0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- 10.Pizarro J, Silver RC, Prause J. Physical and mental health costs of traumatic war experiences among Civil War veterans. Arch Gen Psychiatry. 2006;63:193–200. doi: 10.1001/archpsyc.63.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kazis LE, Ren XS, Lee A, Skinner K, Rogers W, Clark J, et al. Health status in VA patients: Results from the Veterans Health Study. Am J Med Qual. 1999;14:28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 12.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160:3252–7. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 13.Johnson AM, Rose KM, Elder GH, Jr, Chambless LE, Kaufman JS, Heiss G. Military combat and risk of coronary heart disease and ischemic stroke in aging men: The Atherosclerosis Risk in Communities (ARIC) study. Ann Epidemiol. 2010;20:143–50. doi: 10.1016/j.annepidem.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmadi N, Hajsadeghi F, Mirshkarlo HB, Budoff M, Yehuda R, Ebrahimi R. Post-traumatic stress disorder, coronary atherosclerosis, and mortality. Am J Cardiol. 2011;108:29–33. doi: 10.1016/j.amjcard.2011.02.340. [DOI] [PubMed] [Google Scholar]
- 15.Jiang W, Glassman A, Krishnan R, O’Connor CM, Califf RM. Depression and ischemic heart disease: What have we learned so far and what must we do in the future? Am Heart J. 2005;150:54–78. doi: 10.1016/j.ahj.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Rose DE, Farmer MM, Yano EM, Washington DL. Racial/ethnic differences in cardiovascular risk factors among women veterans. J Gen Intern Med. 2013;28(Suppl 2):S524–8. doi: 10.1007/s11606-012-2309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vimalananda VG, Miller DR, Christiansen CL, Wang W, Tremblay P, Fincke BG. Cardiovascular disease risk factors among women veterans at VA medical facilities. J Gen Intern Med. 2013;28(Suppl 2):S517–23. doi: 10.1007/s11606-013-2381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hauser RM, Willis RJ. Survey design and methodology in the health and retirement study and the Wisconsin longitudinal study. In: Waite LJ, editor. Aging, Health, and Public Policy: Demographic and Economic Perspectives. New York: The Population Council, Inc; 2005. pp. 209–35. [Google Scholar]
- 19.Heeringa SG, Connor JH. Technical description of the health and retirement survey sample design. 1995. Available from: http://www.hrsonline.isr.umich.edu/sitedocs/userg/HRSSAMP.pdf .
- 20.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 21.Yang FM, Jones RN. Measurement differences in depression: Chronic health-related and sociodemographic effects in older Americans. Psychosom Med. 2008;70:993–1004. doi: 10.1097/PSY.0b013e31818ce4fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steffick DE, Wallace RB, Herzog AR. Survey Research Center, University of Michigan; 2000. [Last retrieved on 2008 Jan 08]. Documentation of affective functioning measures in the Health and Retirement Study. Available from: http://www.hrsonline.isr.umich.edu/docs/userg/dr-005.pdf . [Google Scholar]
- 23.Ayotte BJ, Yang FM, Jones RN. Physical health and depression: A dyadic study of chronic health conditions and depressive symptomatology in older adult couples. J Gerontol B Psychol Sci Soc Sci. 2010;65:438–48. doi: 10.1093/geronb/gbq033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dormann CF, Elith J, Bacher S, Buchmann C, Carl G, Carré G, et al. Collinearity: A review of methods to deal with it and a simulation study evaluating their performance. Ecography. 2013;36:27–46. [Google Scholar]
- 25.Chang PP, Ford DE, Meoni LA, Wang NY, Klag MJ. Anger in young men and subsequent premature cardiovascular disease: The precursors study. Arch Intern Med. 2002;162:901–6. doi: 10.1001/archinte.162.8.901. [DOI] [PubMed] [Google Scholar]
- 26.Kubzansky LD, Cole SR, Kawachi I, Vokonas P, Sparrow D. Shared and unique contributions of anger, anxiety, and depression to coronary heart disease: A prospective study in the normative aging study. Ann Behav Med. 2006;31:21–9. doi: 10.1207/s15324796abm3101_5. [DOI] [PubMed] [Google Scholar]
- 27.Hemingway H, Marmot M. Evidence based cardiology: Psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318:1460–7. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Booth-Kewley S, Friedman HS. Psychological predictors of heart disease: A quantitative review. Psychol Bull. 1987;101:343–62. [PubMed] [Google Scholar]
- 29.Penninx BW, Beekman AT, Honig A, Deeg DJ, Schoevers RA, van Eijk JT, et al. Depression and cardiac mortality: Results from a community-based longitudinal study. Arch Gen Psychiatry. 2001;58:221–7. doi: 10.1001/archpsyc.58.3.221. [DOI] [PubMed] [Google Scholar]
- 30.Kubzansky LD, Kawachi I. Going to the heart of the matter: Do negative emotions cause coronary heart disease? J Psychosom Res. 2000;48:323–37. doi: 10.1016/s0022-3999(99)00091-4. [DOI] [PubMed] [Google Scholar]
- 31.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychol Bull. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 32.Krantz DS, Manuck SB. Acute psychophysiologic reactivity and risk of cardiovascular disease: A review and methodologic critique. Psychol Bull. 1984;96:435–64. [PubMed] [Google Scholar]
- 33.Grippo AJ, Johnson AK. Biological mechanisms in the relationship between depression and heart disease. Neurosci Biobehav Rev. 2002;26:941–62. doi: 10.1016/s0149-7634(03)00003-4. [DOI] [PubMed] [Google Scholar]
- 34.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics - 2011 update: A report from the American Heart Association. Circulation. 2011;123:e18–209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.CDC. Behavioral risk factor surveillance system. [Last accessed on 2011 Oct 07]. Available from: http://www.cdc.gov/brfss .


