Abstract
Background:
The present study was aimed to evaluate the efficacy of acetaminophen plus dexamethasone on post-operative emergence agitation in pediatric adenotonsillectomy.
Methods:
A total of 128 patients were randomized and assigned among four groups as: Intravenous (IV) dexamethasone, oral acetaminophen, IV dexamethasone plus oral acetaminophen, placebo. Group 1 received 0.2 mg/kg dexamethasone plus 0.25 mg/kg strawberry syrup 2 h before surgery. Group 2 received 20 mg/kg oral acetaminophen (0.25 ml/kg) with 0.05 ml/kg IV normal saline. Group 3 received 20 mg/kg acetaminophen and 0.2 mg/kg dexamethasone intravenously. Group 4 received 0.25 ml/kg strawberry syrup and 0.05 ml/kg normal saline. Agitation was measured according to Richmond agitation sedation score in the post anesthetic care unit (PACU) after admission, 10, 20 and 30 min after extubation. Pain score was measured with FACE scale. Nurse satisfaction was measured with verbal analog scale. If agitation scale was 3 ≥ or pain scale was 4 ≥ meperidine was prescribed. If symptoms did not control wit in 15 min midazolam was prescribed. Patients were discharged from PACU according Modified Alderet Score. Data were analyzed with ANOVA, Chi-square, and Kruskal-Wallis among four groups. P < 0.05 was considered statistically significant.
Results:
A total of 140 patients were recruited in the study, which 12 of them were excluded. Thus, 128 patients were randomized and assigned among four groups. The four treatment groups were generally matched at baseline data. Median of pain score in 0, 10, 20 and 30 min after extubation were different between each study group with the control group (<0.001, 0.003 respectively). Also median of agitation score in 0, 10, 20 and 30 min after extubation were different between each study group with the control group (<0.001). Incidence of pain and incidence of agitation after extubation were not statistically identical among groups (P < 0.001 and P = 0.002 respectively). Mean of recovery time, duration of agitation and 1st time to agitation appearance, meperidine and midazolam consumption, nurse satisfaction and complication frequency were not statistically identical among groups (P < 0.001).
Conclusions:
Acetaminophen, dexamethasone and combination of them are superior to placebo for prevention of agitation after adenotonsillectomy in children. Furthermore combinations of both drugs are superior to acetaminophen or dexamethasone separately.
Keywords: Acetaminophen, adenotonsillectomy, dexamethasone, postoperative agitation
INTRODUCTION
Emergence from general anesthesia may be complicated with agitation in some children. This phenomenon which has incidence of 10-80%, also described with interchangeable term such as post anesthetic excitement and emergence delirium and may have deleterious effects in the post-operative period.[1] Children may harm themselves, site of surgery, dislodge monitoring or intravenous (IV) line and/or care providers who provide extra nursing care and additional sedatives and/or analgesics that may cause a delay in discharge from hospital.[1,2,3] Emergence agitation is an acute phenomenon, during which the patient exhibits no purposeful restlessness and agitation, thrashing, screaming crying or moaning, disorientation and incoherence.[4] Emergence agitation with its incidence of 10-80% may have deleterious effects in the postoperative period. Children may harm themselves and or care providers, increased nursing care in the post anesthetic care unit (PACU), delays reunion with parents, increase additional sedatives and/or analgesics that may cause a delay in discharge from PACU and hospital and may lead to adverse sequel in some cases.[1,4] An understanding of the risk factors for enterprise architecture (EA) is important to minimize contributory factors and to appropriately manage agitation when it occurs. In a Cohort Study identified multiple factors associated with EA in young children and found that the use of isoflurane, short time to awakening, and otorhinolaryngologic procedures were independent risk factors for this outcome.[5] In another study different factor such as rapid return of consciousness, pain, sore throat, airway obstruction and bladder distension suggested as possible etiologic factor for emergence agitation.[3] Then pain, edema and airway obstruction which appear after airway surgery are the two most probably etiologic factor in emergence agitation in otorhinolaryngologic procedures. Dexamethasone is the drug of choice for reducing edema. Acetaminophen also use frequently for relief of pain particularly in pediatric postsurgical patients. This study was designed to describe which, if dexamethasone or acetaminophen or combination of both with reducing of edema or pain or both can reduce post adenotonsillectomy agitation in pediatric patients.[5]
METHODS
In a double-blinded, randomized clinical trial study, after obtaining approval of Ethics and Research Committee and written informed consent from parents, all pediatric patients aged 3-7 year-old with American Society of Anesthesiologists I, II without liver, kidney, systemic disease or bleeding diathesis that a candidate for adenotonsillectomy in AL-Zahra Medical Center from 2010 to 2012 were enrolled in the study. A total of 140 patients were eligible, that twelve of them did not allocate in the study: Not meeting inclusion criteria (n = 8) and refused to participate (n = 4). Finally, 128 patients were randomized and assigned among four study groups. This sample size was selected according to the prevalence of agitation in Tom et al. study[6] and using the formula:
Z2:1.28, P1 and P2:0.57 and 0.2 respectively.
Exclusion criteria were intra-operative complications including bleeding and allergy to study drugs. All patients were fasted nothing per oral for 6 h before surgery and fluids were prescribed according 4.2.1. Rule for them with dextrose in saline. Patients were randomly enrolled in four study groups using randomization allocation software as: (1) IV dexamethason. (2) Oral acetaminophen, (3) IV dexamethasone plus oral acetaminophen, (4) placebo. Group 1 received 0.2 mg/kg dexamethasone plus 0.25 mg/kg strawberry syrup. Group 2 received 20 mg/kg oral acetaminophen (0.25 ml/kg) with 0.05 ml/kg IV normal saline. Group 3 received 20 mg/kg acetaminophen and 0.2 mg/kg dexamethasone intravenously. Group 4 received 0.25 ml/kg strawberry syrup and 0.05 ml/kg normal saline. These drug dosages received from Steward et al. and Rømsing et al. studies.[7,8] All premedication were prescribed 2 h before surgery by one anesthesiologist who did not participate in the course of study. None of researchers didn't know about patient groups until the study was finished and the codes were opened. In the operating room standard monitoring (contain: EKG, pulse oximetry, blood pressure) connected to patients. After preoxygenation with 100% oxygen through face mask, induction of anesthesia was done with atropine 0.01 mg/kg, fentanyl 2 micg/kg, sodium thiopental 5 mg/kg and atracurium 0.5 mg/kg. Trachea intubated and anesthesia was maintained with 66% N2O in 33% O2 and 1.2 MAC isoflurane. Ventilator respiratory rate was adjusted as end tidal CO2 was between 35 mmHg and 45 mmHg. 0.1 mg/kg morphine injected intravenously for all patients after tracheal tube fixation. Every 1 ml of blood loss was replaced with 3 ml lactated ringer. After completed of the surgery reversal of atracurium was done with neostigmine 0.04 mg/kg and 0.02 mg/kg atropine. When tidal volume received to 5 ml/kg patient transferred to post anesthesia care unit. When patient was able to open his or her eyes and able to hold head for 5 s trachea was extubated. Agitation was measured according to Richmond agitation sedation score in the PACU after admission, 10, 20 and 30 min after extubation.[9] (0: Alert and calm, 1: Restless, 2: Agitated, 3: Very agitated, 4: Combative). Pain score was measured with FACE scale.[10] Nurse satisfaction was measured with verbal analog scale from 0 (un satisfaction) to 10 (full satisfaction). If agitation scale was 3 ≥or pain scale was 4 ≥ meperidine was prescribed 1 mg/kg IV. If symptoms did not control wit in 15 min midazolam was prescribed 0.1 mg/kg IV. Patients was discharged from PACU when Modified Alderet Score 9 of 10 was achieved.[11] Pulse rate and SaO2 both measured in the PACU after admission, 10, 20 and 30 min later. Duration of anesthesia (from induction until discontinuation of anesthesia agents), extubation time (from discontinuation of anesthesia agents until extubation of trachea), recovery time (from entering to PACU until accepting of discharge criteria with modified Alderet score) and duration of agitation all measured and recorded.
Collected data entered into a computer and analyzed by Data were collected, edited and analyzed by Statistical Package for the Social Sciences software version 18 (SPSS version 18) software. ANOVA was used for comparison of demographic data, anesthesia, surgery and recovery times, duration of agitation, time to agitation appearance, meperidine and midazolam doses consumption, nurse satisfaction score and time to extubation among four groups. Sex distributions, frequency of pain, frequency of agitation and complication were measured with Chi-square test among four groups. In comparisons of median of agitation severity and median of pain severity because data did not normal distributions, we used nonparametric tests for comparison of them. Then median of agitation severity and pain severity were measured with Kruskal-Wallis among four groups. Mann-Whitney test was used for comparisons of data between each two groups in the study. P < 0.05 was considered to be statistically significant.
RESULTS
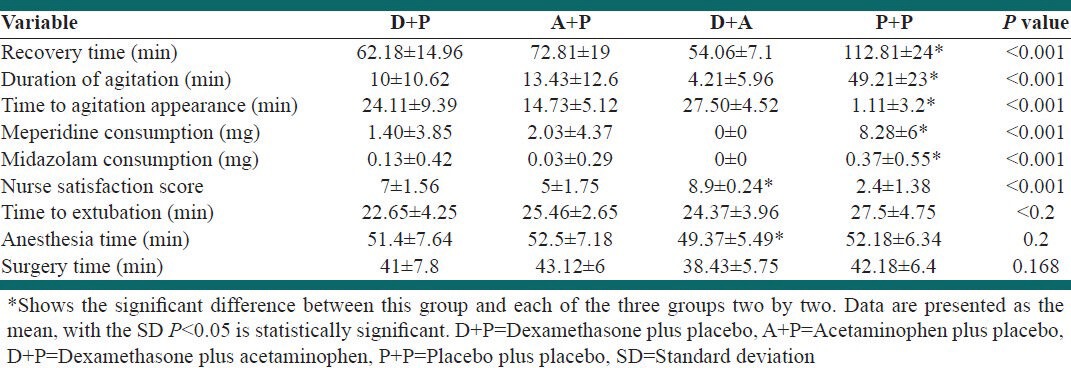
A total of 140 patients were recruited in the study. Four patients refused to participate and eight patients did not meet our study criteria. Thus, 128 patients were randomized and assigned among four groups, as described in Figure 1 and Table 1. The four treatment groups were generally matched at baseline in terms of age, gender, weight, duration of anesthesia and surgery and extubation. No differences were found in cardiorespiratory variables (systolic and diastolic blood pressure, heart rate, respiratory rate, or SpO2) among the groups during surgery. Median of pain score in 0, 10, 20 and 30 min after extubation were different between each study group with the control group, but there were no differences among study groups. Furthermore, median of agitation score in 0, 10, 20 and 30 min after extubation were different between each study group with the control group, but differences among study groups were not statistically different [Table 2]. Incidence of pain and incidence of agitation after extubation were statistically different among groups [Table 3]. Mean of recovery time, duration of agitation and 1st time to agitation appearance, meperidine and midazolam consumption, nurse satisfaction and complication frequency were not statistically identical among groups [Table 4].
Figure 1.
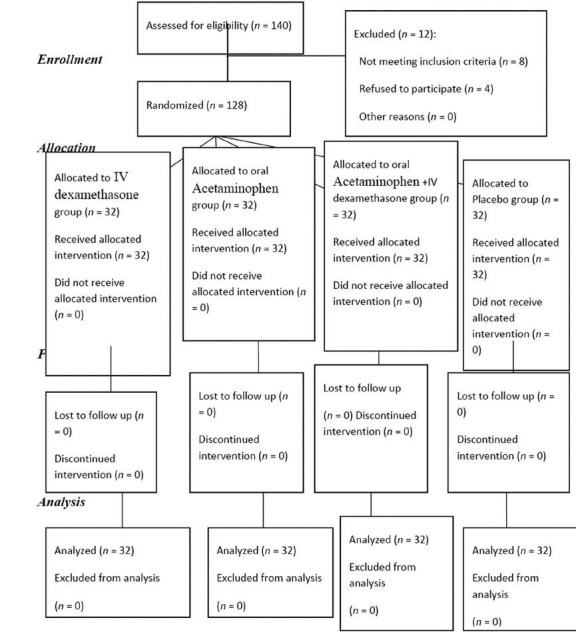
Consort diagram showing the flow of participants through each stage of the study
Table 1.
Characteristics of patients undergoing adenotonsillectomy who received dexamethasone, acetaminophen, dexamethasone plus acetaminophen or placebo
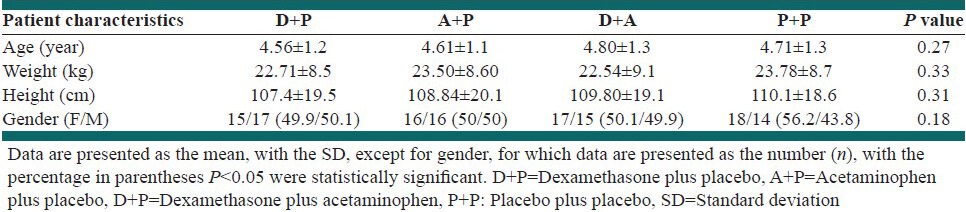
Table 2.
Median of agitation score and median of pain score in 0, 10, 20 and 30 min after extubation
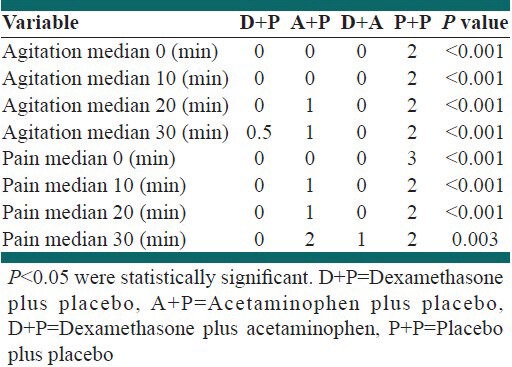
Table 3.
Incidence of agitation, incidence of pain and complications in PACU
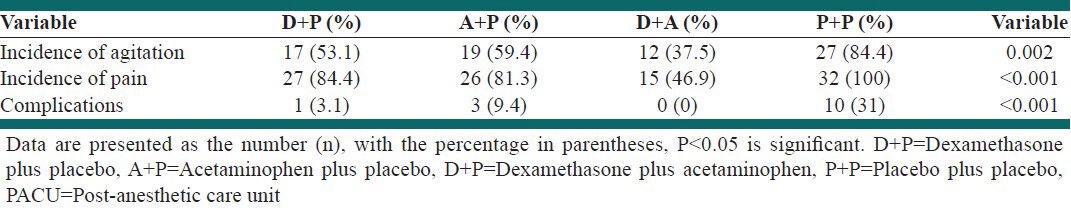
Table 4.
Recovery time, duration of agitation, time to agitation appearance, meperidine and midazolam consumption, nurse satisfaction score, extubation time, anesthesia time and surgery time anesthesia and complication frequency
DISCUSSION
This study showed that combination of acetaminophen and dexamethasone efficiently decreases both EA and post-operative pain in comparison with the placebo group and also with acetaminophen alone and dexamethasone alone groups separately. Post-operative complications also significantly decreased in acetaminophen plus dexamethasone group in comparison with the placebo group and also dexamethasone alone and acetaminophen alone groups separately. Dexamethasone is an anti-inflammatory agent and acetaminophen, also known as paracetamol, is a non-steroidal anti-inflammatory drug with potent antipyretic and analgesic actions but with very weak anti-inflammatory activity.[12]
Eckenhoff in the early 1960's at first described EA in children anesthetized with ether, cyclopropane and ketamine undergoing tonsillectomy, thyroidectomy and circumcision.[1] He considered that a “sense of suffocation “during emergence from anesthesia may contribute to increase the incidence of EA in otolaryngology procedure.[1,2,3,4] Later in, 2003, Voepel-Lewis in a prospective study has shown that the otolaryngology procedure are an independent risk factor for EA.[5] Postoperative pain is the most confounding variable for EA.[4] Then in this study we compared the efficacy of acetaminophen and dexamethason on EA base on the two most etiologic risk factors on otolaryngology procedure: Pain and sense of suffocation. Incidence of EA in the PACU significantly reduced in acetaminophen plus dexamethasone group in comparison with the placebo group (P = 0.002). This finding is accordance with Templeton et al. and Fan et al. studies.[13] Incidence of pain in the PACU also significantly reduced in the acetaminophen plus dexamethasone group in comparison with the placebo group (P < 0.001). Furthermore incidence of EA was lower in acetaminophen group and dexamethasone group compared with placebo but is higher in dexamethasone plus acetaminophen group. A study by LI et al. found that sufentanyl reduce EA in PACU.[14] This finding approved that pain is interfere with EA in Pediatric Tonsillectomy. Anghelescu et al. also found the co administration of ketamine in induction of anesthesia could prevent emergence agitation.[15] These finding is comparable with our study. However in our study, we found that the sense of suffocation also interferes with EA in adenotonsillectomy and dexamethasone was effective for reducing EA.
Median of agitation score in PACU was significantly lower in dexamethasone plus acetaminophen group in comparison with the placebo group in 0, 10, 20 and 30 min after extubation of trachea (P < 0.001). Duration time of EA was significantly different among groups and was higher in the placebo group (P < 0.001). This finding is accordance with Pikering and Templeton studies.[1,3] Mean time to appearance of EA was significantly longer in dexamethasone plus acetaminophen group in comparison with the placebo group (P < 0.001). This finding also is accordance with Kissen et al. study. Duration of PACU stay was significantly higher in Placebo group (P < 0.001). Prescription of meperidine and dexamethasone were lower significantly in acetaminophen and dexamethasone group (P <.001). Median score of caregiver satisfaction was significantly different among groups and was higher in dexamethasone plus acetaminophen group (P < 0.001). For the purpose of ethical considerations and study limitations, in this study drugs which are used were not usual, then, after obtaining written informed consent, we used study drugs, therefore, no ethical barrier or limitation has been determined.
CONCLUSIONS
Pain and edema suggested as etiologic factor in post-tonsillectomy agitation in the previous study. Acetaminophen plus dexamethasone decreased agitation after adenotonsilectomy in this study. Because dexamethasone reduce both pain and edema and acetaminophen reduce pain, then combination of them decreased agitation after adenotonsilectomy in our study. Then we concluded that acetaminophen plus dexamethasone is effective in prevention of post-adenotonsilectomy agitation.
Footnotes
Source of Support: Financial support by Research Department, Isfahan University of Medical Sciences, Isfahan, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Nasr VG, Hannallah RS. Emergence agitation in children – A view. Middle East J Anesthesiol. 2011;21:175–82. [PubMed] [Google Scholar]
- 2.Bortone L, Ingelmo P, Grossi S, Grattagliano C, Bricchi C, Barantani D, et al. Emergence agitation in preschool children: Double-blind, randomized, controlled trial comparing sevoflurane and isoflurane anesthesia. Paediatr Anaesth. 2006;16:1138–43. doi: 10.1111/j.1460-9592.2006.01954.x. [DOI] [PubMed] [Google Scholar]
- 3.Silva LM, Braz LG, Módolo NS. Emergence agitation in pediatric anesthesia: Current features. J Pediatr (Rio J) 2008;84:107–13. doi: 10.2223/JPED.1763. [DOI] [PubMed] [Google Scholar]
- 4.Vlajkovic GP, Sindjelic RP. Emergence delirium in children: Many questions, few answers. Anesth Analg. 2007;104:84–91. doi: 10.1213/01.ane.0000250914.91881.a8. [DOI] [PubMed] [Google Scholar]
- 5.Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg. 2003;96:1625–30. doi: 10.1213/01.ANE.0000062522.21048.61. [DOI] [PubMed] [Google Scholar]
- 6.Tom LW, Templeton JJ, Thompson ME, Marsh RR. Dexamethasone in adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 1996;37:115–20. doi: 10.1016/0165-5876(96)01388-2. [DOI] [PubMed] [Google Scholar]
- 7.Steward DL, Grisel J, Meinzen-Derr J. Steroids for improving recovery following tonsillectomy in children. Cochrane Database Syst Rev. 2011;8:CD003997. doi: 10.1002/14651858.CD003997.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rømsing J, Ostergaard D, Drozdziewicz D, Schultz P, Ravn G. Diclofenac or acetaminophen for analgesia in paediatric tonsillectomy outpatients. Acta Anaesthesiol Scand. 2000;44:291–5. doi: 10.1034/j.1399-6576.2000.440312.x. [DOI] [PubMed] [Google Scholar]
- 9.Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, et al. The Richmond agitation-sedation scale: Validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338–44. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 10.Garra G, Singer AJ, Taira BR, Chohan J, Cardoz H, Chisena E, et al. Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50–4. doi: 10.1111/j.1553-2712.2009.00620.x. [DOI] [PubMed] [Google Scholar]
- 11.Marshall SI, Chung F. Discharge criteria and complications after ambulatory surgery. Anesth Analg. 1999;88:508–17. doi: 10.1097/00000539-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Botting RM. Mechanism of action of acetaminophen: Is there a cyclooxygenase 3? Clin Infect Dis. 2000;31(Suppl 5):S202–10. doi: 10.1086/317520. [DOI] [PubMed] [Google Scholar]
- 13.Fan KT, Lee TH, Yu KL, Tang CS, Lu DV, Chen PY, et al. Influences of tramadol on emergence characteristics from sevoflurane anesthesia in pediatric ambulatory surgery. Kaohsiung J Med Sci. 2000;16:255–60. [PubMed] [Google Scholar]
- 14.Li J, Huang ZL, Zhang XT, Luo K, Zhang ZQ, Mao Y, et al. Sufentanil reduces emergence agitation in children receiving sevoflurane anesthesia for adenotonsillectomy compared with fentanyl. Chin Med J (Engl) 2011;124:3682–5. [PubMed] [Google Scholar]
- 15.Anghelescu DL, Rakes LC, Shearer JR, Bikhazi GB. Prevention of emergence agitation in seven children receiving low-dose ketamine and propofol total intravenous anesthesia. AANA J. 2011;79:238–42. [PMC free article] [PubMed] [Google Scholar]


