Abstract
Aphasia is prevalent in people following stroke, which can have a significant impact on the quality of life of the patients with stroke. One of the new methods for treatment of patients with aphasia is constraint-induced aphasia therapy (CIAT). The aim of this study was to investigate the efficacy of CIAT on naming deficits in individuals with chronic aphasia. This study had a prospective, single-subject study with A-B-A design. The CIAT was administered to two patients with chronic aphasia. Participants were a 57-year-old male and a 45-year-old female and had a stroke 60 and 36 months ago, respectively. In this study, the naming test was used as the outcome measure. The naming test was administered in three baseline sessions with 1 week interval between tests (phase A). Patients received CIAT for four consecutive weeks (3 days/week). Four measurements were taken during the treatment phase (phase B). In follow-up phase (phase A) two other measurements were performed. Visual analysis consisting of level, regression line, and variability were used to determine the effects of CIAT on naming. Both participants increased scores on naming test after phase A and B. The mean of the naming score improved from the baseline to the intervention phase in both participants. There was a positive trend in naming scores during the treatment phase compared with the trend in the baseline demonstrated by both participants. The results of this study showed that the CIAT can be effective in improving the naming deficit in patients with chronic post-stroke aphasia.
Keywords: Aphasia, constraint-induced aphasia therapy, naming deficit, prevention
INTRODUCTION
Aphasia is a language dysfunction that occurs in one-third of patients after stroke. Aphasia is a multifaceted disorder involving different modalities of language.[1] Naming deficit is commonly observed in patients with aphasia post-stroke.[2] Approximately, 30% of patients with post-stroke aphasia suffer from naming deficit.[3] There are a variety of treatment methods for patients with aphasia. One novel method for treating aphasia is constraint-induced aphasia therapy (CIAT). The CIAT is principally adapted from a movement rehabilitation approach used for the treatment of motor deficits in post-stroke hemiplegia called constraint-induced movement therapy (CIMT).[4] The CIMT is based on a notion that the motor disability after stroke involves a suppression of movement of the affected limb through a phenomenon labeled learned non-use. Consequently, limb disuse must be prevented by forcing patients to utilize the affected limbs, while avoiding compensatory strategies. Evidence indicates that CIMT can achieve its effects through neuroplasticity and use-dependent cortical reorganization.[5] In CIAT, first proposed by Pulvermüller and Roth,[6] patients with chronic aphasia receive short term, intensive speech therapy, and are forced to communicate with talking while all compensatory strategies (e.g. gesturing, writing, pointing) are restricted.[7] The CIAT uses the principles of massed practice, shaping and constraint of compensatory non-verbal strategies. Evidence from clinical trials supports the efficacy of CIAT in improving language of individuals with chronic aphasia to other current language interventions although, there is few studies to support it.[7,8] However, evidence for efficacy of CIAT in naming deficits of patients with chronic aphasia is not established. Therefore, the aim of this study was to investigate the effect of CIAT on naming deficit in patients.
CASE REPORT
This is a single-subject study with A-B-A design that was conducted on two patients with chronic aphasia. The protocol of this study was approved by Research Council, School of Rehabilitation, and Ethical Committee of Tehran University of Medical Sciences (TUMS). The participants signed an informed consent form before conducting the study. Total naming score (TNS) was the main outcome measure in this study. A total of 310 pictures with different frequencies were used to test naming.
Two patients with aphasia referred to the clinic of speech therapy, School of Rehabilitation, TUMS included in the study based on the following criteria; (1) Age 40-65 years old; (2) stroke resulted in aphasia; (3) history of stroke 12 ≥ months; (4) presence of naming deficit; (5) right handed; (6) normal vision, or corrected using glasses or contact lenses; (7) normal or corrected hearing; (8) intact auditory comprehension (score at least 25 on the Mississippi test) (9) ability to utter single words; (10) mono-language (Persian); (11) able to read and write. The exclusion criteria were: (1) History of drug abuse in the past 6 months; (2) history of mental illnesses; (3) history of psychotropic drug abuse; and (4) recurrent stroke. Since there was no protocol available to be used in the study, several pilot studies were performed to develop an appropriate treatment protocol. It therefore took 11 months to develop a protocol for use in this study. Then, the data collection started in January 2012 and completed in March 2012. The treatment and all measurements were taken at the clinic of speech therapy, School of Rehabilitation, TUMS. Participants were two adult patients with aphasia. Patient one was a 57-year-old male, and patient two was a 45-year-old female. They had a stroke 60 and 36 months ago, respectively.
Following a baseline interview to collect the demographic data, patients were screened by the first author, a speech-language pathologist (SLP). The Mississippi test[9] was administered to diagnose the aphasia, and the naming deficit was examined using the naming test.[10] Naming test included 310 pictures and was performed as naming picture, in which every picture had two points and if patient was not able to name the picture he/she was not receiving any point. If patient named the picture with phonological or semantic paraphasia, he/she was receiving one point. The screening process also included the determination of handedness. The baseline data were collected for 3 consecutive weeks (1 assessment each week). Then, patients went under treatment for 4 weeks, 3 days a week. Each treatment session took 2.5 h. Four assessments were performed during the treatment phase; again 1 assessment each week. The naming test was administered in two follow up sessions with 1 week interval between tests (phase A).
CIAT treatment sessions were conducted as a card game with both study patients treated simultaneously under supervision of SLP. The patients were forced to communicate only with talking, and were not allowed to use any compensatory strategies. Patients were encouraged if they named the pictures verbally.
A set of 120 picture cards was used for treatment. Each patient was asked to pick up a picture card and was forced to name it verbally. When named, the other patient was asked to find the similar card and name it verbally. At first, the SLP used phonological and visual clues to help patients, but it gradually decreased with improvements so that the patients were forced to name the picture independently At the first stage, pictures were used for treatment. Pictures used for treatment were associated with low frequency or high frequency words, minimal pairs, colors, and numbers.[10] At this stage, patients were forced to name the picture shown to them. At the second stage, written materials were also used. At this stage, pictures of words, categorized items, the written form of minimal pairs, and word puzzles were used for treatment. At the third stage, sentence stimulating pictures were used to enhance patients’ verbal outcome. The collected data were statistically analyzed using level, standard deviation (SD) range, mean, trend, and mean shift statistics to assess the treatment effects. Improvements of two points or more above the +2SD line have been considered as clinically significant indicating the treatment efficacy.[11]
Participant 1
The mean of total score on naming test was 33.66 at the baseline which was improved to 110.75 after treatment [Table 1]. The values of treatment phase was above the +2SD line as shown in Figure 1. The slope of regression line was positive which was indicative of improvement trend. The level statistic, the difference between the mean of score obtained in the last evaluation session and the first intervention session, was +65 showing the efficacy of the CIAT. The level statistic for the first and the last treatment sessions was +12. The mean shift statistic was 2.29.
Table 1.
The total naming score for participant 1
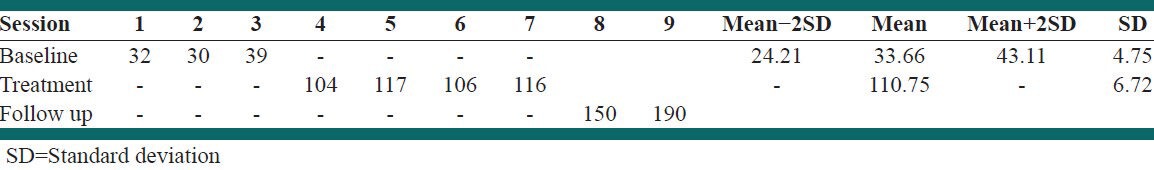
Figure 1.

The total naming score at baseline and after treatment for participant 1
Participant 2
The mean of total score on naming test was 308 at the baseline, which was improved to 405.75 after treatment [Table 2]. Again, the values of treatment phase was above the +2SD line as shown in Figure 2.
Table 2.
The total naming score for participant 2

Figure 2.
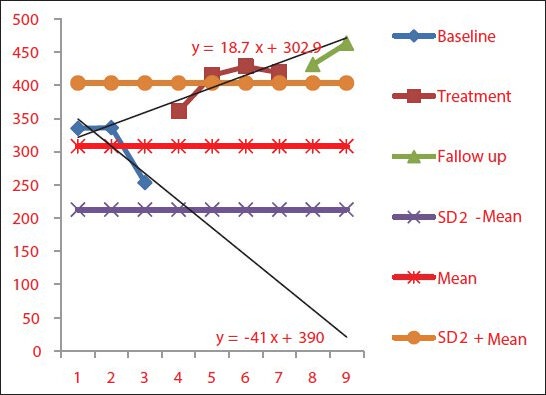
The total naming score at baseline and after treatment for participant 2
The slope of regression line for participant 2 was also positive which was indicative of improvement trend. The level statistic, the difference between the mean of score obtained in the last evaluation session and the first intervention session was +108. The level statistic for the first and the last treatment session was +58. The mean shift statistic was 0.31.
DISCUSSION
This study was undertaken to evaluate the effects of CIAT in two post-stroke individuals with naming deficits using single-subject design. The results of the present study appeared that the CIAT approach was effective in our study participants with aphasia. As far as we know, this is the first report on the effect of CIAT on naming ability of patients with aphasia post-stroke. Although speech therapy is widely used for managing language problems in patients with aphasia, there are concerns about the extent to which improvements may occur in chronic phase of the aphasia after the period of spontaneous recovery phase.[5] The results of the present study revealed that the CIAT approach using the intense and repetitive forced speech production is effective in improving naming deficit of patients with aphasia. Our finding is in consistent with the report of Kurland et al.[8] which showed that the CIAT has a positive effect even in patients with chronic moderate-to-severe aphasia. Furthermore, the CIAT has been shown that is more effective in improving verbal outcome in comparison with traditional treatments.[12,13,14,15,16,17,18,19] The possible explanation for improvements could be due to cortical reorganization and neuroplasticity.[7,8,20,21,22,23]
Authors have demonstrated that only intensive treatments may promote brain reorganization and therefore the improvement of language functionality in patients with aphasia.[24,25,26] The severity of a condition is an important factor for predicting the therapeutic effect of CIAT. An inverse relationship has been shown between the severity of language problems and the degree of improvement after the treatment.[27,28,29] In the present study, the participant 2, who had a severe of language problem, showed more improvement after the CIAT. The results demonstrated in the present study are in agreement with findings of Meinzer et al.[27] The results of this study showed that the CIAT is effective for treating naming deficit in stroke survivors with aphasia. Both patients responded well to the CIAT, as demonstrated by naming test scores. The data from this study suggest that the CIAT may be an effective treatment approach for naming disorders in patients with aphasia.
ACKNOWLEDGMENTS
We would like to thank Dr. Meinzer and Professor Nickels for their valuable comments.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Berthier ML. Poststroke aphasia: Epidemiology, pathophysiology and treatment. Drugs Aging. 2005;22:163–82. doi: 10.2165/00002512-200522020-00006. [DOI] [PubMed] [Google Scholar]
- 2.Wisenburn B, Mahoney K. A meta-analysis of word-finding treatment for aphasia. Aphasiology. 2009;23:1338–52. [Google Scholar]
- 3.Kohn SE, Goodglass H. Picture-naming in aphasia. Brain Lang. 1985;24:266–83. doi: 10.1016/0093-934x(85)90135-x. [DOI] [PubMed] [Google Scholar]
- 4.Taub E, Uswatte G, Mark VW, Morris DM. The learned nonuse phenomenon: Implications for rehabilitation. Eura Medicophys. 2006;42:241–56. [PubMed] [Google Scholar]
- 5.Taub E, Uswatte G, Elbert T. New treatments in neurorehabilitation founded on basic research. Nat Rev Neurosci. 2002;3:228–36. doi: 10.1038/nrn754. [DOI] [PubMed] [Google Scholar]
- 6.Pulvermüller F, Roth VM. Communicative aphasia treatment as a further development of PACE therapy. Aphasiology. 1991;5:39–50. [Google Scholar]
- 7.Balardin JB, Miotto EC. A review of constraint-induced therapy applied to aphasia rehabilitation in stroke patients. Dement Neuropsychol. 2009;3:275–82. doi: 10.1590/S1980-57642009DN30400003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurland J, Pulvermüller F, Silva N, Burke K, Andrianopoulos M. Constrained versus unconstrained intensive language therapy in two individuals with chronic, moderate-to-severe aphasia and apraxia of speech: Behavioral and fMRI outcomes. Am J Speech Lang Pathol. 2012;21:S65–87. doi: 10.1044/1058-0360(2012/11-0113). [DOI] [PubMed] [Google Scholar]
- 9.Khatoonabadi A, Piran A, Nakhostin Ansari N. Under Work; 2012. Assessing the reliability and validity of The Mississippi test for Persian language. [Google Scholar]
- 10.Tahanzadeh B, Soleymani Z, Seyyedeh KM, Mehri A, Jalaie S. Validity and reliability of oral picture-naming test in aphasic adults. Audiol. 2012;21:84–93. [Google Scholar]
- 11.Ottenbacher KJ. Interrater agreement of visual analysis in single-subject decisions: Quantitative review and analysis. Am J Ment Retard. 1993;98:135–42. [PubMed] [Google Scholar]
- 12.Lincoln NB, McGuirk E, Mulley GP, Lendrem W, Jones AC, Mitchell JR. Effectiveness of speech therapy for aphasic stroke patients. A randomised controlled trial. Lancet. 1984;1:1197–200. doi: 10.1016/s0140-6736(84)91690-8. [DOI] [PubMed] [Google Scholar]
- 13.Poeck K, Huber W, Willmes K. Outcome of intensive language treatment in aphasia. J Speech Hear Disord. 1989;54:471–9. doi: 10.1044/jshd.5403.471. [DOI] [PubMed] [Google Scholar]
- 14.Bhogal SK, Teasell R, Speechley M. Intensity of aphasia therapy, impact on recovery. Stroke. 2003;34:987–93. doi: 10.1161/01.STR.0000062343.64383.D0. [DOI] [PubMed] [Google Scholar]
- 15.Wertz RT, Weiss DG, Aten JL, Brookshire RH, García-Buñuel L, Holland AL, et al. Comparison of clinic, home, and deferred language treatment for aphasia. A Veterans Administration Cooperative Study. Arch Neurol. 1986;43:653–8. doi: 10.1001/archneur.1986.00520070011008. [DOI] [PubMed] [Google Scholar]
- 16.Marshall RC, Wertz RT, Weiss DG, Aten JL, Brookshire RH, Garcia-Bunuel L, et al. Home treatment for aphasic patients by trained nonprofessionals. J Speech Hear Disord. 1989;54:462–70. doi: 10.1044/jshd.5403.462. [DOI] [PubMed] [Google Scholar]
- 17.David R, Enderby P, Bainton D. Treatment of acquired aphasia: Speech therapists and volunteers compared. J Neurol Neurosurg Psychiatry. 1982;45:957–61. doi: 10.1136/jnnp.45.11.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartman J, Landau WM. Comparison of formal language therapy with supportive counseling for aphasia due to acute vascular accident. Arch Neurol. 1987;44:646–9. doi: 10.1001/archneur.1987.00520180064018. [DOI] [PubMed] [Google Scholar]
- 19.Prince RS, Schoonen R, Vermeulen J. Efficacy of two different types of speech therapy for aphasic stroke patients. Appl Psycholinguist. 1989;10:85–123. [Google Scholar]
- 20.Pulvermüller F, Hauk O, Zohsel K, Neininger B, Mohr B. Therapy-related reorganization of language in both hemispheres of patients with chronic aphasia. Neuroimage. 2005;28:481–9. doi: 10.1016/j.neuroimage.2005.06.038. [DOI] [PubMed] [Google Scholar]
- 21.Meinzer M, Elbert T, Wienbruch C, Djundja D, Barthel G, Rockstroh B. Intensive language training enhances brain plasticity in chronic aphasia. BMC Biol. 2004;2:20. doi: 10.1186/1741-7007-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breier JI, Maher LM, Schmadeke S, Hasan KM, Papanicolaou AC. Changes in language-specific brain activation after therapy for aphasia using magnetoencephalography: A case study. Neurocase. 2007;13:169–77. doi: 10.1080/13554790701448200. [DOI] [PubMed] [Google Scholar]
- 23.Berthier ML, Pulvermüller F. Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nat Rev Neurol. 2011;7:86–97. doi: 10.1038/nrneurol.2010.201. [DOI] [PubMed] [Google Scholar]
- 24.Meinzer M, Rodriguez AD, Gonzalez Rothi LJ. First decade of research on constrained-induced treatment approaches for aphasia rehabilitation. Arch Phys Med Rehabil. 2012;93(Suppl 1):S35–45. doi: 10.1016/j.apmr.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brindley P, Copeland M, Demain C, Martyn P. A comparison of the speech of ten chronic Broca’s aphasic following intensive and non-intensive periods of therapy. Aphasiology. 1989;3:695–707. [Google Scholar]
- 26.Pulvermüller F, Neininger B, Elbert T, Mohr B, Rockstroh B, Koebbel P, et al. Constraint-induced therapy of chronic aphasia after stroke. Stroke. 2001;32:1621–6. doi: 10.1161/01.str.32.7.1621. [DOI] [PubMed] [Google Scholar]
- 27.Meinzer M, Streiftau S, Rockstroh B. Intensive language training in the rehabilitation of chronic aphasia: Efficient training by laypersons. J Int Neuropsychol Soc. 2007;13:846–53. doi: 10.1017/S1355617707071111. [DOI] [PubMed] [Google Scholar]
- 28.Szaflarski JP, Ball A, Grether S, Al-Fwaress F, Griffith NM, Neils-Strunjas J, et al. Constraint-induced aphasia therapy stimulates language recovery in patients with chronic aphasia after ischemic stroke. Med Sci Monit. 2008;14:CR243–50. [PMC free article] [PubMed] [Google Scholar]
- 29.Faroqi-Shah Y, Virion CR. Constraint-induced language therapy for agrammatism: Role of agrammatism constraints. Aphasiology. 2009;23:977–88. [Google Scholar]


