Abstract
In this case report we aimed to present a patient with granulocytic sarcomaa, neutropenic fever, ARDS and Pneumocystis jirovecii pneumoniae that was hospitalized in our intensive care unit. The patient recovered and then developed vancomycin resistant enterococci (VRE) bacteremia due to port catheter during follow up. The patient had risk factors for VRE bacteremia and he was administered linezolide without removing the catheter. He was discharged with recovery.
Keywords: Granulocystic sarcoma, Pneumocystis jiroveci pneumoniae, vancomycin resistant enterococci, (VRE)
Introduction
Granulocytic sarcoma is a rare extramedullary tumor that originates from granulocytic cells. Granulocytic sarcoma may develop during acute myeloid leukemia, myelodysplastic syndrome and myeloproliferative disorders. It is usually detected on skin,bones, soft tissue and periost layer. It is common in children and adolescents and equally shown in both genders. This is a sign of bad prognosis [1]. Surgical excision, combined chemotherapy, and radiotherapy are treatment models [2]. Allogenic or autologous bone marrow transplantation are additional treatment to systemic chemotherapy in case of coexistence of acute leukemia and granulocytic sarcomae [1]. Recently immunosuppressed cases have increased due to an increment in cytotoxic and corticosteroid treatment (organ transplantation, systemic disorders, etc.) [3, 4]. Neutropenia is defined as neutrophil count less than 500/mm3or decreasing under 500/mm3 in 24-48 hours. Febril neutropenia, is defined as fever higher than 38.3°C or higher than 38°C during one hour [3]. Pulmonary complications are ictu causes of morbidity and mortality in immunosuppressed cases. In these cases mortality develops depending on underlying disorders, infectious agent and type of complication. Early diagnosis, and treatment are important and multidiciplinary approach is needed. Prematures, children with primary immunodefiency, hematological malignities, organ transplantation, immunosuppresive treatment are under risk of P.jirovecii infection other than AIDS. Pneumocystis jiroveci pneumoniae is a clinical icture with diffuse interstitial infiltration. Besides normal pulmonary X-ray, cystic form with increased risk of spontanous pneumothorax, paranchymal consolidation, multiple nodules, pleural fluid, and enlargement of lymph nodes may be other radiological images [5]. Enterococcal infections have increased due to increment in third generation cephalosporin use in 1970s. First isolation of VRE was in 1978 and then globally spreaded and became one of the most important reason of hospital infection. Enterecoccus feacalis and Enterecoccus faecium are the most common strains [6]. In this case report we aimed to present a patient with granulocytic sarcomae, neutropenic fever, acute respiratory distress syndrome (ARDS) and Pneumocystis jiroveci pneumoniae that was hospitalized in our intensive care unit.
Patient and observation
Nineteen year old male patient had left arm pain two months ago and afterwards he was diagnosed as granulocytic sarcoma. On the seventh day of his chemotherapy neutropenic fever developed. He was administered piperacillin/tazobactam, amikacin; but fever continued and teicoplanin was initiated. Then the antibiotics were stopped and amphothericin B and meropenem was begun. On the twentyfifith day of the chemotherapy regime neutropenic state ended. He developed fever, dyspnea and hypotension on the 27th day. His physical examination showed cyanosis, dyspnea, increased respiratory sound at the upper and middle lung level bilaterally. The arterial blood gas analysis revealed severe hypoxemia (PaO2/FiO2: 82.5) and he was entubated. The patient was transffered to intensive care unit and mechanical ventilation support was applied. The chest X-ray revealed bilaterally increased non-homogeneous density on all zones (Figure 1). High Resolution computerized tomography indicated frost glass appearance (Figure 2). No growth was reported on microbiological cultures. Pneumocytis jiroveci pneumoniae was not detected on broncho alveolar lavage sample by Giemsa stain and trimethoprim/sulfamethoxazole (TMP/SMX) 80mg/day was iniated. Clinical and radiological recovery was obtained (Figure 3). Mechanical ventilation support was stopped on the nineth day. Fever increased on twelveth day. Vancomycin resistant Enterecoccus feacalis was detected on blood culture taken from the port catheter and evaluated as hospital infection. Strict infection control measures were taken and the patient was administered linezolide. Peripheral and catheter blood cultures were drawn in 48-72 hours before the removal of the port catheter. The patient was discharged on the twentyfourth day with recovery.
Figure 1.
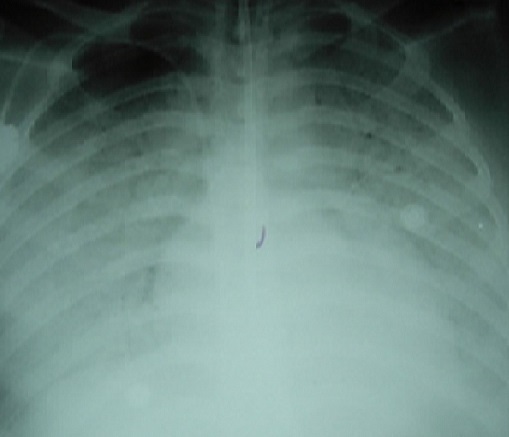
The chest X-ray image revealed bilaterally increased non-homogeneous density on all zones
Figure 2.

High resolution computerized tomography (HRCT) image of the patient
Figure 3.
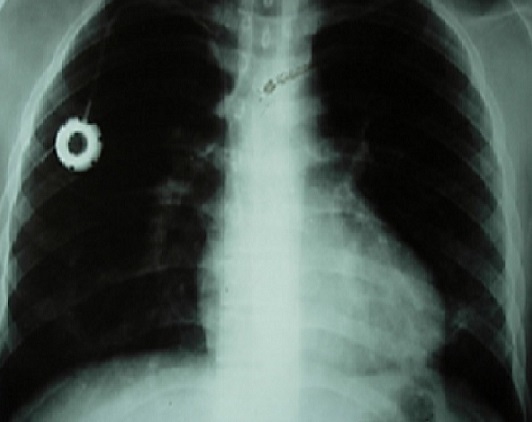
Radiological recovery of the patient on chest X-ray
Discussion
P. Jiroveci pneumoniae is a clinical picture in individuals with cellular immundeficiency and fever, cough, progressive hypoxemia and dyspnea develops. The clinical status of the patient may be severe. Diffuse interstitial and perihilar infiltration are typical on chest X-ray [7]. Fever and dyspneae may appear a few days earlier. P. jirovecicannot be detected on culture. The diagnosis can be done by direct microscopic examination of the lower respiratory tract samples with Giemsa and Wright stain and PCR. In our case report we could not show P. jiroveci on bronchoscopic samples and ampiric treatment was initiated considering hypoxemia and radiological image.
The treatment of P. jiroveci pneumoniae requires TMP/SMX (15 mg/kg/day) for 14-21 days as the first line agent. In cases with mild to severe hypoxemia (PaO2 < 70 mmHg) corticosteroid treatment potentiates oxygenation and decreases mortality. The recommended treatment requires 40 mg/day twice for 5 days, 40 mg/day for five days and 20 mg methylprednisolone for 11 days [3]. In our case TMP-SMX and methylprednisolone were iniated and clinical and radiological recovery were obtained. Also dyspnea healed.
Enterococci are a part of the gastrointestinal system and vaginal flora and infections are commonly due to endogeneous flora. The bacterial isolate is transferred to patients by contamianted hands and fomites. Recently there is an increment in nosocomial infections due to enterococci. VRE infections particulary increased in patients with underlying disorders. E. Faecium strains show 47% vancomycin resistance [8, 9]. The risk factors for VRE infection are immunsuppression, long duration of hospitalization, and broad spectrum antibiotic. Our patient had all of these risk factors. VRE was reported on port catheter which was used to administer chemotherapy [9]. Linezolid is the only member of synthetic oxyzolidone family and is active in-vitro against resistant Gram positive cocci such as vancomycin resistant Enterococcus faecalis and Enterococcus faecium and methicilin resistant Staphylococcus aureus [9, 10]. The approval was declared in our country in 2005. Our case was treated with linezolide without removing the catheter.
Conclusion
Chemotherapy and other treatment modalities have increased survey; but long duration of hospitalization, and broad spectrum antibiotic use increase the risk of resistant infections. Appropiate microbiological culture and multidiciplinary approach can decrease mortality.
Competing interests
The authors declare no competing interest.
Authors’ contributions
Celdir Emre and Oz were doctors responsible for this patient. Ece carried out microbiologycal analysis. Arda was the doctor from the department of Infectious Diseases who monitors us with this case. Celdir Emre, Baysak and Ece were major contributors to writing the manuscript and to the conception and design as well as drafting the article for publication. Bacakoglu supervised the redaction of this article. All the authors have read and approved the final version of the manuscript
References
- 1.Finnegan DPJ, Jones FGC, McMullin MF. Acute myeloid leukemia with concurrent myeloid sarcomaa treated with autologous bone marrow transplantion:two illustrative cases and a literature review. Hematol Oncol. 2005;23(3,4):133–135. doi: 10.1002/hon.759. [DOI] [PubMed] [Google Scholar]
- 2.Dutta Roy S, Stafford JS, Scally J, Selvachandran SN. Granulocytic sarcomaa of the breast antedating acute myelogenous leukemia. Breast. 2004;13(3):242–246. doi: 10.1016/j.breast.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Türk Toraks Dernegi Bagisikligi Baskilanmis Eriskinlerde Gelisen Pnömoni Tani ve Tedavi Rehberi; 2009. [Google Scholar]
- 4.Rano A, Agusti C, Sibila O, Torres A. Pulmonary infections in non-HIV immunocompromised patients. Curr Opin Pulm Med. 2005;11(3):213–7. doi: 10.1097/01.mcp.0000158728.14945.46. [DOI] [PubMed] [Google Scholar]
- 5.Franquet T, Gimenez A, Hidalgo A. Imaging of opportunistic fungal infections in immunocompromised patients. Eur J Radiol. 2004;51(2):130–8. doi: 10.1016/j.ejrad.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Akalin Erdal. Geçmisten Gelecege Yogun Bakim Infeksiyonlari. Yogun Bakim Dergisi. 2007;7(1):5–8. [Google Scholar]
- 7.De Pauw BE, Verweij PE. Infections in patients with hematologic malignancies. Principles and Practice of Infectious Diseases. In: Mandell GL, Bennett JE, Dolin R, editors. Elsevier Inc; 2005. pp. 3432–41. [Google Scholar]
- 8.Tasbakan IM. Vankomisine dirençli enterekok olgular? ANKEM Derg. 2010;24(Ek 2):82–4. [Google Scholar]
- 9.Usluer Gaye. Linezolid. ANKEM Derg. 2010;24(Ek 2):114–8. [Google Scholar]
- 10.Ulusoy Sercan. Yogun bakim ünitesinde Gram-pozitif mikroorganizmalar ve direnç sorunu. Yogun bakim Derg 3.2. 2003:118–128. [Google Scholar]


