Abstract
Psychological treatments for OCD are increasingly aimed at improving outcomes by directly incorporating family members to address family disruption, dysfunction, or symptom accommodation. Much remains to be learned about the pooled effects of “family-inclusive treatment” (FIT) for OCD and factors that may explain variation in response. Random-effects meta-analytic procedures were conducted to empirically evaluate the overall effect of FITs on OCD, and treatment moderators. Study search criteria yielded 29 studies examining FIT response in 1,366 OCD patients. Outcome variables included OCD symptoms and global functioning. Examined moderators included age group, gender, minority status, treatment length and format, and inclusion of specific family-focused treatment elements. FITs for OCD demonstrated a large overall effect on OCD symptoms (pooled d = 1.68, SE = 0.14) and global functioning (pooled d = 0.98, SE = 0.14). Moderator analyses found that individual family treatments (versus group) and FITs targeting family accommodation of symptoms (versus those that did not target accommodation) were associated with greater improvements in patient functioning. Results indicate a robust overall response to FITs for OCD and clarify key moderators that inform optimal circumstances for effective treatment. Findings underscore the need for continued momentum in the development, evaluation, and dissemination of FITs for OCD.
Keywords/Phrases: OCD, CBT, Meta-analysis, Family-based treatment, Accommodation
Introduction
Obsessive-compulsive disorder (OCD)—characterized by recurrent intrusive, anxiety-provoking thoughts and/or repetitive behaviors that cause marked distress or interference—is a highly debilitating mental disorder affecting between 1–3% of individuals in the United States in a given year and 2.7% of individuals across a lifetime (Kessler, Pethukhova, Sampson, Zaslavsky, & Wittchen, 2012). Onset often occurs in childhood or young adulthood (Ruscio, Stein, Chiu, & Kessler, 2010), and research on the effects of gender has generally reflected higher prevalence in females (e.g., Ruscio et al., 2010), though other studies have found mixed results (e.g., Steinhausen, Bisgaard, Munk-Jorgensen, & Helenius, 2013). Studies to date reflect higher rates of OCD in Caucasians, but historically low recruitment of racial and ethnic minorities in clinical trials suggests that documented prevalence rates may not be entirely accurate (Williams, Powers, Yun, & Foa, 2010). OCD is associated with high levels of functional impairment in academic, occupational, social, and family domains (Rosa et al., 2012); full remission without treatment is rare (Skoog & Skoog, 1999); and, accordingly, early and effective intervention is critical.
Current Treatment Models for OCD
Psychotropic medications and cognitive-behavioral therapy (CBT) have garnered the strongest empirical support in the treatment of OCD (Olatunji, Davis, Powers, & Smits, 2013; Watson & Rees, 2008). Among psychotropic medications, serotonin reuptake inhibitors (SRIs) have received the most support (e.g., Greist et al., 1995; Tollefson, Rampey, Potvin et al., 1994). Regarding psychological treatment, the efficacy of CBT for OCD has been well established in adults (Foa et al., 2005; Franklin et al., 2000) and in children and adolescents (Franklin et al., 2011; POTS Team, 2004; Thienemann et al., 2001). Recent meta-analytic work examining the pooled efficacy of CBT for OCD across clinical trials indicates a large and robust pooled effect size ranging from d = 0.998 to d = 1.45 (e.g., Olatunji et al., 2013; Watson & Rees, 2008). Meta-analytic work to date suggests that CBT for OCD is associated with somewhat larger effect sizes than pharmacologic interventions (Watson & Rees, 2008).
Despite the great support for CBT in the treatment of OCD, meta-analytic studies examining treatment moderators have failed to identify many factors that systematically explain variations in treatment response, with outcomes roughly comparable across group and individual treatment formats, and outcomes not systematically varying by patient (baseline severity, comorbidity, gender) or study characteristics (methodological rigor, number of sessions) (Olatunji et al., 2013). However, there is evidence that CBT response differs across age groups, with pooled estimates of treatment effects somewhat smaller in the treatment of adult OCD relative to pediatric OCD, even though outcomes do not significantly vary by age-of-onset or by duration of symptoms (Olatunji et al., 2013). This may speak to the greater malleability of OCD symptoms during earlier developmental stages, but may also speak to a key difference in treatment protocols targeting child versus adult OCD populations. Specifically, although behavioral and cognitive strategies are incorporated across patients of all developmental levels, CBT for OCD in youth more consistently includes an explicit focus on family functioning and direct involvement of family members in treatment (e.g., Freeman & Garcia, 2008).
Family Factors in OCD
Family reactions and coping strategies when confronted with symptoms may have important implications for the maintenance and amelioration of OCD (e.g., Abramowitz et al., 2013; Lebowitz, Panza, Su, & Bloch, 2012). Because OCD often revolves around activities of daily living (bathing, eating, being with family members), it can be particularly disruptive to functioning within a family context. The majority of research examining family processes in relation to OCD has focused on family symptom accommodation. Accommodation refers to changes in family members’ behavior in order to attempt to prevent or reduce the patient’s distress related to their OCD symptoms (Calvocoressi et al., 1995), or to reduce time associated with extended rituals. Examples include engaging in rituals on behalf of or with the patient (e.g., checking the stove for the patient), providing necessary supplies for rituals (e.g., cleaning products), or giving verbal reassurance.
For most family members, accommodation can offer a natural and sensitive response to their family member’s distress and immediately smooth family interactions. Indeed, family members often report that their efforts at accommodation are explicitly motivated by a desire to decrease the OCD-affected individual’s immediate distress, or to simply decrease the time associated with onerous rituals (Calvocoressi et al., 1999). Accommodation can be an effective strategy in the short term; in addition, OCD-affected individuals often explicitly request or demand accommodation, and can become upset or aggressive if family members decline (Calvocoressi et al., 1995). However, accommodating OCD symptoms also allows the individual to avoid confronting his/her obsessional thoughts (through continued engagement in compulsions) and strengthens associations between these obsessions and anxiety. Thus, in the longer term, such family responses can also yield a negative impact, legitimizing patients’ obsessional beliefs and creating an escalating cycle between family members’ accommodating responses and OCD symptoms.
Indeed, higher levels of family accommodation are associated with increased OCD symptoms, increased functional impairment, and poorer treatment outcome in both children and adults (Amir, Freshman, & Foa, 2000; Calvocoressi et al., 1999; Merlo, Lehmkuhl, Geffken, & Storch, 2009; Storch et al., 2010). In addition to its detrimental effects on patients, over time accommodation is also related to significant family member distress (e.g., depression, anxiety, personal burden), family dysfunction (e.g., poor problem-solving and communication, high affective involvement), and rejection of patients (Calvocoressi et al., 1995; Storch et al., 2009).
The high rates of impairment among OCD patients and their family members, and the reciprocal relationships among family behaviors and patients’ symptoms, indicate a pressing need to address these issues in the context of OCD treatment. CBTs for OCD are increasingly beginning to directly incorporate family members of affected individuals into treatment in hopes that such an approach will yield improved outcomes, stronger generalization and maintenance of gains, and improved overall family functioning. In addition to potentially reducing unhelpful patterns of interaction among patients and family members, if the OCD symptoms themselves have caused substantial conflict among the family members, then active involvement of family members in treatment activities can contribute to a “team approach” of family versus disorder, reducing negative feelings and empowering the group (Waters, Barrett, & March, 2001). OCD treatment can be quite challenging for patients, and family support and engagement has the potential for bolstering treatment effects and reducing family stress.
Family-Inclusive Treatments
Whereas individual-centered treatments of psychopathology typically frame the locus of the problem squarely within an “identified patient,” familial-contextual models approach the conceptualization, maintenance, and amelioration more broadly. Family models allow for engagement and integration of important potential resources within an individual’s environment while also considering how aspects of the environment may be contributing to maladaptive cycles that tend to perpetuate the problems.
Several approaches to family-inclusive treatment (FIT) for OCD have been described in the literature, with substantial variability across formats, the length and content of the FIT protocol, and age of the targeted patients. Regarding treatment format, FIT approaches can be separated into those that employ an individual family treatment approach (e.g., Storch, Geffken, et al., 2007), allowing the clinician to attend exclusively to the particular issues relevant for a given family, or a group approach (e.g., Farrell, Schlup, & Boschen, 2010), providing patients and families built in social support and opportunities to gather group feedback.
The treatment content of FITs for OCD also varies across treatment models. Some protocols provide only psychoeducation about OCD and CBT to families (Bolton & Perrin, 2008), whereas others also include more targeted information to families or skills training that are specific to family interactions in OCD (Freeman et al., 2008; Peris & Piacentini, 2013). Two such common targets include working with families to reduce symptom accommodation, based on the rationale described previously, and on exposure “coach” training. Exposures, during which patients are asked to deliberately provoke obsessive fears and then resist engaging in associated compulsions, are a critical element of CBT for OCD. They allow patients to learn to tolerate their anxiety, and ultimately reduce the urge to ritualize. Particularly early in treatment, it is often helpful for patients to have someone present during their exposures in order to ensure that they are not doing anything, even subtly, to avoid the distress provoked by the exercise, as this would defeat the intended function of the exposure. Training family members to act as coaches entails teaching them to guide exposure exercises outside of sessions; this training can enhance treatment compliance and may provide family members with a more sophisticated understanding of the principal of exposure.
Finally, the patient age targeted in FITs for OCD has varied, spanning a range from as young as 5 years old (Freeman et al., 2008) through adults (Mehta, 1990), and at present it is not clear whether patient age moderates the impact of FIT efficacy. Family relationships, patterns, and routines can have a substantial impact on OCD patient symptoms and functioning across the lifespan, and in turn family members are greatly affected by OCD behaviors and associated patient distress (Calvocoressi et al., 1995; Cooper, 1996; Lebowitz et al., 2012; Renshaw, Steketee, & Chambless, 2005). However, in younger aged patients family involvement may be particularly important given that children often have relatively lower levels of insight into their disorder and lower baseline motivation to change their behavior. Furthermore, parents often have a natural inclination to alleviate their children’s distress, which could lead to greater accommodation and negative reinforcement of OCD symptoms, and thus FITs may be associated with particularly large effects in pediatric relative to adult OCD.
The Present Study
Despite several revealing meta-analyses evaluating the overall efficacy of psychological treatments for OCD across the lifespan, little is known about the specific pooled effects of OCD treatments that take on a broader familial-contextual approach to intervention and include the family members of OCD-affected individuals in treatment (i.e., FITs). Similarly, much remains to be learned about factors that may explain systematic variation in outcomes associated with FIT for OCD across the lifespan.
In the present meta-analysis, we evaluated: (a) the overall effect of the range of FITs on OCD, as well as (b) moderators of treatment outcome that can inform for whom and under what circumstances FITs may be most effective for patients with OCD. Specifically, we first hypothesized that OCD treatments that included a family component would be associated with medium to large effect sizes across methodological designs (i.e., within-subjects designs and between-subjects designs) and across outcomes (i.e., OCD symptoms, general functioning) given the variety of designs and outcomes that have yielded robust treatment effects in prior meta-analyses. Second, we hypothesized that FIT would be associated with larger effects in younger, relative to older, patient populations. Third, given previous work suggesting comparability in outcomes across group and individual treatment formats (Olatunji et al., 2013), we did not expect treatment format to moderate FIT effects. Finally, we predicted stronger effects of FITs that targeted family accommodation and included coaching in exposure tasks than FITs that did not directly target these elements, given the medium to large effects often found in trials examining the efficacy of FITs for pediatric OCD (Freeman et al., 2008; Piacentini et al., 2011; Storch et al., 2010) and the fact that these treatments formally address family accommodation and coaching in exposure tasks above and beyond what is included in most FITs for adult OCD.
Method
All meta-analytic procedures were conducted in accordance with guidelines set forth by Field and Gillett (2010) and Field (2013).
Study selection
Clinical trials published prior to May 1, 2012 that satisfied six a priori selection criteria were included. First, OCD had to be the principal target of the treatment under study in order to ensure that none of the integrated findings were due to secondary impacts of treatments targeting non-OCD problems. For studies that involved multiple diagnostic groups (e.g., Chambless & Steketee, 1999), we required outcomes to be reported separately for the OCD group. Second, studies needed to include at least one treatment group that received a psychological intervention with some level of standardized family involvement described, specifically a clearly defined portion of the treatment which all family members received (e.g., “Parents attended sessions 4, 5, and 12”). As long as families were systematically included to some extent, no absolute minimum time requirement for family participation in treatment was required (as this was a specific variable of interest). Third, study sample sizes needed to be sufficient to afford statistical analyses (n≥10). Fourth, the studies had to provide sufficient statistical information for the authors to calculate or extract effect sizes necessary for meta-analysis. Fifth, for quality control, only studies that had undergone peer-review were included (no dissertations or data in book chapters). Lastly, consistent with most meta-analyses published in English-language journals, articles had to be written in English so that all study coders had equal facility extracting data for each article.
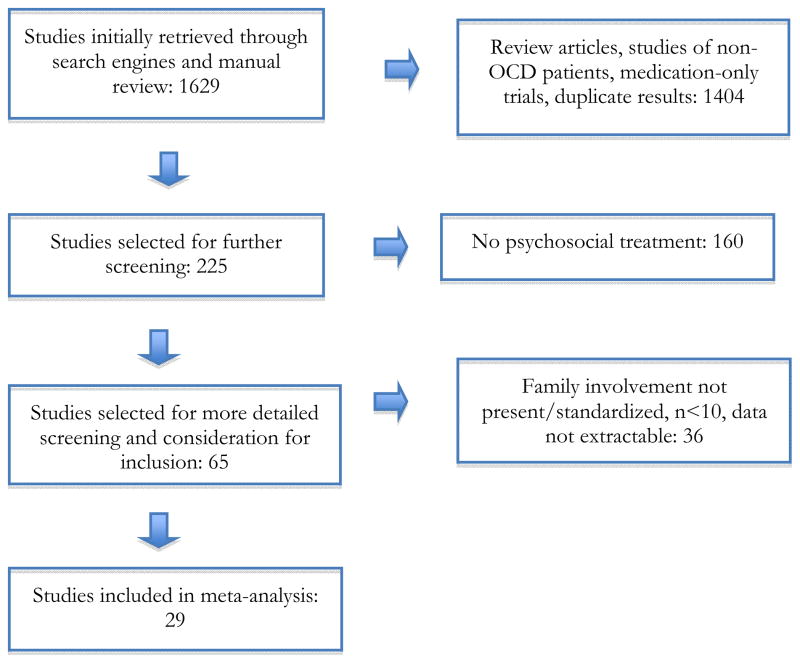
Following Field and Gillett (2010), several strategies were employed to identify eligible studies in the following order: (a) computer searches in PubMed and PsycINFO using search terms related to family, OCD, and treatment (a list of exact search terms used is available upon request); (b) examining the reference sections of the articles identified through the computer search; (c) manual search of the tables of contents since 2000 in relevant journals (a list of these journals is available upon request); and (d) review of the reference sections of existing meta-analyses examining OCD treatments. Figure 1 presents the flow of included studies.
Figure 1.
Flow chart of the study selection process
Variable coding
Eligible studies were coded independently by two separate coders. Individual effect sizes were extracted or computed for OCD symptoms and for general functioning.
Patient variables
We coded mean patient age, patient age group (youth: ≤ 17; adult: ≥ 18 years), percentage of racial/ethnic minority patients and percentage of male patients.
Treatment variables
Treatment format was classified as either (a) individual family treatment (patient/family was treated alone) or (b) group treatment (i.e., patient/family was treated with others concurrently), and treatment length (in mean number of weeks and sessions) was coded. Level of family involvement (regardless of specific content) was coded on a 1–5 scale, with 1 representing minimal involvement (e.g., family members were brought in for a portion of a single session and allowed to ask questions about the treatment) and 5 representing extensive involvement (e.g., a fully family-based treatment in which relatives were present for all sessions and were actively incorporated into treatment activities and discussions). We also coded the presence or absence of several specific family elements that treatment may have contained: (a) psychoeducation to the family about OCD and exposure-based treatment (identified in 100% of included studies), (b) instructions to family members to reduce accommodation (83% of included studies, and (c) family training as a “coach” for exposures (45% of included studies).
Study methodology variables
Acute effects referred to outcomes immediately at posttreatment. More than half of the included studies also included follow-up assessments.
Procedure
Coders were two graduate students specializing in the treatment of anxiety disorders across the lifespan under the direct supervision of a clinical psychologist (final author). Training included didactics and practice coding. Overall interrater reliability of coding was strong (intraclass correlation coefficient = .98).
Data Analysis
Random-effects (RE) analytic methods were used given their advantages over fixed-effect (FE) methods. RE methods are believed to be more accurate and realistic, given their assumption that population parameter values will vary across studies, whereas FE methods assume that analyzed studies have a homogenous population effect. In addition, regardless of whether population parameter values are heterogeneous or homogenous, RE methods reduce the likelihood that type 1 error rates may be inflated (see Field, 2001; Hedges, 1992; Hedges & Vevea, 1998; Lipsey & Wilson, 2000).
Effect sizes were calculated using Cohen’s d and a 95% confidence interval. For studies with multiple effects reported for one construct, effects were averaged within study to yield one effect size per construct per study prior to data synthesis. Z scores were also calculated to assess the significance of pooled effects, which was done by dividing the pooled effect by the standard error of that effect. To determine whether observed variability across effects was significant, the Q statistic was calculated for each effect to assess the effect homogeneity. Heterogeneity was expected across effects, due to the wide variety of patient demographics (e.g., the large age span within the sample), methodologies, and treatment outcomes across the FIT literature.
To evaluate potential moderators of effects for categorical variables, we employed Q-Between tests, which systematically evaluate the extent to which effects vary across different levels of each variable in question (e.g., adult versus youth samples). Significant Q-Between tests indicate moderation. In cases of significant moderation, pooled effect sizes across different levels of the moderator were compared for interpretation. Meta-regression was used to evaluate potential moderators that were continuous.
Moreover, to evaluate potential publication bias, fail-safe Ns (FSN) were calculated for significant results, which correspond to the number of null results that would be needed to overturn a significant result (i.e., the number of studies needed to make p > .05); an FSN greater than five times the number of studies in the analysis plus ten (i.e., FSN ≥ 5k + 10) is considered to be robust against the file-drawer effect (Rosenthal, 1991).
Results
The literature on family-inclusive treatment of OCD
A total of 29 studies evaluating 1,366 children and adults were identified that met selection criteria (see Table 1). The mean age of patients across studies was 17.89 (SD = 9.72; range 7.1–37.0); mean sample size was 47.10 (SD = 31.38; range 14–124). Twenty studies (69%) included single-group within-subjects analyses, while 12 studies (41%) included between-groups comparisons of two or more conditions (some studies included both within- and between-groups analyses). Twenty-six studies (90%) evaluated acute post-treatment outcomes, and 16 (55%) included follow-up outcomes. Nine (31%) of the studies included group treatment for patients. Seven (24%) studies evaluated adult patients (i.e., mean age of sample ≥18). Family interventions varied widely, ranging from family members attending a single session to fully family-based treatments. Twenty-two studies (76%) included families for at least a portion of all sessions with the patient; seven studies (24%) included families for the all sessions in full. Five studies (17%) included families for only one session. Of those studies that listed a manual for the family intervention (19 studies, 66%), the majority used or adapted the treatment manual by March and Mulle (1998).
Table 1.
Studies of family-inclusive treatments (FITs) for OCD
| Reference | Total n |
Mean pt age |
Family treatment format |
# sessions for patient:family |
Family treatment protocol |
Elements of family treatment
|
Comparison group(s) |
Description of family treatment | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Psycho- education |
Focus on reducing accommodation |
Exposure coach training |
||||||||
| Barrett, Farrell, Dadds, & Boulter, 2005 | 77 | 11.8 | Individual family | 16:16 | March & Mulle, 1998* | X | X | X | None | CBT. Separate parent skills training and family review of progress at each session.” |
| Group family | 16:16 | March & Mulle, 1998* | X | X | X | None | Group CBT. Separate parent skills training group and family review of progress at each session. | |||
| Barrett, Healy-Farrell, & March, 2004 | 77 | 11.8 | Individual family | 16:16 | March & Mulle, 1998* | X | X | X | None | CBT. Separate parent skills training and family review of progress at each session. |
| Group family | 16 :16 | March & Mulle, 1998* | X | X | X | None | Group CBT. Separate parent skills training group and family review of progress at each session. | |||
| Benazon, Ager, & Rosenberg, 2002 | 16 | 8–17 (range) | Individual family | 12 :12 | March & Mulle, 1998* and Schwartz, 1996* | X | X | None | CBT. Parents attended four sessions in full and a portion of all sessions. | |
| Bolton & Perrin, 2008 | 20 | 13.2 | Individual family | 12:1 | Not specified | X | Waitlist | ERP. Parents attended one session. | ||
| Chambless & Steketee, 1999 | 49 | 35 | Individual family | 22:1 | Unpublished | X | None | CBT. Family members attended one 90-minute session early in treatment. | ||
| de Haan et al., 1998 | 23 | 13.77 | Individual family | 12:12 | Not specified | X | X | Medication | BT. Parents attended the first and last session in full, and portions of all sessions. | |
| Farrell, Schlup, & Boschen, 2010 | 35 | 12.29 | Group family | 14:14 | March & Mulle, 1998* | X | X | X | None | CBT. Parents attended a group for 15–30 minutes following the patients’ group treatment. |
| Franklin et al., 2011 | 124 | 13.6 | Individual family | 14:14 | March & Mulle, 1998* | X | X | Medication management | CBT. Parents attended sessions 1, 7, and 11 in full, and portions of all sessions. | |
| Individual family | 7:7 | Not specified | X | Medication management | Instructions in CBT. Parents attended session 1 in full, and portions of all sessions. | |||||
| Freeman et al., 2008 | 42 | 7.11 | Individual family | 10:12 | Freeman & Garcia, 2009 | X | X | X | Family-inclusive relaxation | CBT. Parents attended two introductory sessions alone; all other sessions were conducted with child and parents. |
| Grunes, Neziroglu, & McKay, 2001 | 28 | 28.5 | Group family | 8:8 | Not specified | X | X | X | Individual CBT | CBT. Group intervention for family members. |
| Haland et al., 2010 | 54 | 35.9 | Group family | 14:1 | Krone et al., 1991 | X | X | None | ERP. Family members attended one session in full. | |
| Himle et al., 2001 | 113 | 37 | Group family | 8:1 | Krone et al., 1991 | X | None | ERP. Family members attended one session in full. | ||
| Group family | 13:1 | Krone et al., 1991 | X | None | ERP. Family members attended one session in full. | |||||
| Keeley et al., 2011 | 25 | 13.16 | Individual family | 14:14 | March & Mulle, 1998* | X | None | CBT. Parents attended sessions 1, 7, and 11 in full, and portions of all sessions. | ||
| March, Mulle, & Herbel, 1994 | 15 | 14.3 | Individual family | 17:17 | Unpublished | X | X | None | ERP and anxiety management training. Parents included for a brief “checkin” at all sessions, and attended sessions 1, 6, and 12 in full. | |
| Martin & Thienemann, 2005 | 14 | 11.3 | Group family | 14:14 | March & Mulle, 1998* | X | X | None | Group CBT. Parents met in a separate family group for 12 sessions, and together with patients for two sessions. | |
| Mehta, 1990 | 30 | 34.2 | Individual family | 24:24 | Not specified | X | X | X | Individual ERP | ERP. Family members attended all sessions in full. |
| O’Leary, Barrett, & Fjermestad, 2009 | 77 | 11.8 | Individual family | 16:16 | March & Mulle, 1998* | X | X | X | None | CBT. Separate parent skills training and family review of progress at each session. |
| Group family | 16:16 | X | X | X | None | Group CBT. Separate parent skills training group and family review of progress at each session. | ||||
| POTS Team, 2004 | 112 | 11.7 | Individual family | 14:3 | March & Mulle, 1998* | X | X | Medication alone, placebo | CBT. Parents attended sessions 1, 7, and 11 in full. | |
| Individual family | 14:3 | March & Mulle, 1998* | X | X | Medication alone, placebo | CBT plus medication. Parents attended sessions 1, 7, and 11 in full. | ||||
| Peris & Piacentini, 2012 | 20 | 12.35 | Individual family | 12:12 | Piacentini, Langley, & Roblek, 2007 | X | X | None | ERP. Parents attended a portion of all sessions. | |
| Individual family | 12:6 | Not specified | X | X | X | None | ERP and Positive Family Interaction Therapy. Parents attended sessions every other week. | |||
| Piacentini et al., 2011 | 71 | 12.2 | Individual family | 12:12 | Piacentini, Langley, & Roblek, 2007 | X | X | Relaxation | CBT. Parents attended a portion of all sessions. | |
| Piacentini et al., 2002 | 42 | 11.8 | Individual family | 12.5:9 | Piacentini et al., 1994* | X | X | None | CBT. Parents attended the first two sessions in full, and a portion of remaining sessions. | |
| Steketee & Chambless, 2001 | 49 | 35 | Individual family | 22:1 | Unpublished | X | None | CBT. Family members attended one 90-minute session early in treatment. | ||
| Storch et al., 2011 | 31 | 11.1 | Individual family | 14:14 | March & Mulle, 1998* | X | X | X | Waitlist | CBT. Parents attended all sessions in full. |
| Storch et al., 2007 | 40 | 13.3 | Individual family | 14:14 | March & Mulle, 1998 and Lewin et al., 2005 | X | X | X | None | CBT. Parents attended all sessions in full. |
| Individual family | 14:14 | March & Mulle, 1998 and Lewin et al., 2005 | X | X | X | None | Intensive CBT. Parents attended all sessions in full. | |||
| Storch et al., 2010 | 30 | 13.4 | Individual family | 14:14 | March & Mulle, 1998* | X | X | X | None | Intensive CBT. Parents attended all sessions. |
| Thienemann et al., 2001 | 18 | 15.2 | Group family | 14:14 | March & Mulle, 1998* | X | X | None | CBT. Parents attend one full session, and a portion of all other sessions. | |
| Valderhaug et al., 2007 | 28 | 13.3 | Individual family | 12:12 | Piacentini et al., 1998 | X | X | None | CBT. Parents attended the first two sessions in full, and a portion of all other sessions. | |
| Van Noppen et al., 1997 | 42 | 33 | Group family | 20:20 | Not specified | X | X | X | Group BT | BT. Families attended all sessions in full. |
| Wever & Rey, 1997 | 82 | 13.7 | Individual family | 12:12 | Unpublished | X | X | X | None | CBT. Parents attended sessions 1 and 2 in full; attend portion of all sessions. |
Note: Manuals indicated with an asterisk (*) were adapted by the study authors. ERP = Exposure and response prevention, CBT = Cognitive-behavioral therapy, BT = Behavior therapy.
Overall effect of family-inclusive treatment on OCD symptoms and functioning
Overall, FITs had a large effect on OCD symptoms (κ = 28, pooled d = 1.68, SE = .14, 95% CI = 1.41—1.95, z = 12.23, p < .001). This result was very robust against the file-drawer effect, with a fail-safe N of 9,038. When broken down by study methodology, the within-groups effect of FITs on OCD symptoms remained large (κ = 18, pooled d = 1.80, SE = .05, 95% CI = 1.50—2.10, z = 11.67, p < .001), as did the between-groups effects (κ = 12, pooled d = 1.45, SE = .29, 95% CI = .89—2.01, z = 5.06, p < .001). Acute and follow-up effects of FITs on OCD symptoms were not significantly different (Qbetween = .06, df = 1). Regarding the effects on general functioning, FITs for OCD were associated with a large overall effect (κ = 14, pooled d = .98, SE = .14, 95% CI = .70—1.26, z = 6.89, p < .001). Both within-subjects and between-subjects analyses demonstrated large effects on functioning (within-groups effects: κ = 9, pooled d = .87, SE = .11, 95% CI = .65—1.10, z = 7.63, p < .001; between-groups effects: κ = 6, pooled d = 1.21, SE = .32, 95% CI = .58—1.83, z = 3.77, p < .001). There was not a significant difference between the effect of FITs on functioning at acute versus follow-up assessments (Qbetween = .81, df = 1). Although these effect sizes were large, there was considerable heterogeneity in the magnitude of effects across studies on both OCD symptoms (Q = 593.3, τ2 = 95.4) and functioning (Q = 209.296, τ2 = 93.79), supporting examination of potential moderators that may explain variability.
Moderators of the effects of family-inclusive treatment on OCD symptoms and functioning
Tables 2 and 3 display the results of analyses examining potential moderators of treatment effects on OCD symptoms and functioning. Regarding moderators of OCD symptom outcomes, no patient characteristics evaluated (i.e., age group, ethnicity, and gender) significantly moderated the effect of FIT on OCD symptoms. The format of treatment (group versus individual family) was also not a significant moderator of OCD symptom outcomes, nor was FIT treatment content or treatment length in weeks. The level of family involvement in FIT was also not a significant moderator. However, the number of sessions did significantly moderate treatment effects on OCD symptoms, with more sessions producing superior outcomes (κ = 28, β = .09, SE = 0.04, 95% CI = .02—.16, z = 2.55, p < .01).
Table 2.
Results of analyses examining moderators of response on OCD symptoms (κ = 28, N = 1,324)
| Categorical Moderator/Subgroup | κ | Pooled d | SE | 95% C.I.(lower, upper) | Z | Test of moderation |
|---|---|---|---|---|---|---|
| Age group | Qbetween=0.27, df=1 | |||||
| Mean pt. age < 18 | 21 | 1.70 | .19 | 1.33, 2.07 | 9.01*** | |
| Mean pt. age ≥ 18 | 7 | 1.57 | .16 | 1.26, 1.88 | 9.94*** | |
|
| ||||||
| Format | Qbetween=0.15, df=1 | |||||
| Individual | 22 | 1.78 | .18 | 1.44, 2.12 | 10.13*** | |
| Group | 9 | 1.68 | .20 | 1.28, 2.08 | 8.27*** | |
|
| ||||||
| Family Accommodation | Qbetween=0.08, df=1 | |||||
| Not targeted | 6 | 1.73 | .30 | 1.14, 2.31 | 5.80*** | |
| Targeted | 23 | 1.64 | .16 | 1.32, 1.95 | 10.13*** | |
|
| ||||||
| Exposure training for family | Qbetween=3.38, df=1 | |||||
| Not targeted | 16 | 1.48 | .15 | 1.18, 1.78 | 9.78*** | |
| Targeted | 13 | 1.89 | .16 | 1.57, 2.22 | 11.50*** | |
|
| ||||||
| Continuous Moderator | κ | β | SE | 95% C.I. (lower, upper) | Z | Test of moderation |
|
| ||||||
| Treatment length (weeks) | 28 | 0.02 | .02 | −0.02, 0.06 | 1.12 | Q =1.25, df=1 |
| Treatment length (sessions) | 28 | 0.09 | .04 | 0.02, 0.16 | 2.55** | Q =6.50, df=1 |
| Level of family involvement | 28 | −0.05 | .12 | −0.28, 0.18 | −0.41 | Q =0.17, df=1 |
| % male patients | 28 | 0.01 | .01 | −0.01, 0.03 | 0.61 | Q =0.37, df=1 |
| % minority patients | 18 | −0.03 | .02 | −0.06, 0.00 | −1.74 | Q =3.04, df=1 |
Note:
p<.05,
p<.01,
p<.001
Table 3.
Results of analyses examining moderators of response to FIT on functioning (κ = 14, N = 649)
| Categorical Moderator/Subgroup | κ | Pooled d | SE | 95% C.I. | Z | Test of moderation |
|---|---|---|---|---|---|---|
| Age group | Qbetween = 1.21, df = 1 | |||||
| Mean pt. age<18 | 10 | 1.07 | .19 | 0.71, 1.44 | 5.76*** | |
| Mean pt. age≥18 | 4 | 0.77 | .21 | 0.35, 1.18 | 3.64*** | |
|
| ||||||
| Format | Qbetween = 8.52**, df = 1 | |||||
| Individual | 11 | 1.10 | .17 | 0.76, 1.43 | 6.41*** | |
| Group | 3 | 0.56 | .07 | 0.42, 0.70 | 7.79*** | |
|
| ||||||
| Family Accommodation | Qbetween = 7.14**, df = 1 | |||||
| Not targeted | 3 | 0.58 | .09 | 0.41, 0.76 | 6.52*** | |
| Targeted | 12 | 1.09 | .16 | 0.76, 1.41 | 6.58*** | |
|
| ||||||
| Exposure training for family | Qbetween = 1.12, df = 1 | |||||
| Not targeted | 7 | 0.83 | .15 | 0.54, 1.13 | 5.51*** | |
| Targeted | 7 | 1.14 | .24 | 0.66, 1.62 | 4.64*** | |
|
| ||||||
| Continuous Moderator | κ | β | SE | 95% C.I. | Z | Test of moderation |
|
| ||||||
| Treatment length (weeks) | 14 | −0.03 | .03 | −0.09, 0.03 | −0.84 | Q = 0.71, df = 1 |
| Treatment length (sessions) | 14 | −0.02 | .04 | −0.11, 0.06 | −0.50 | Q = 0.25, df = 1 |
| Level of family involvement | 14 | 0.05 | .13 | −0.20, 0.30 | 0.38 | Q =0.14, df=1 |
| % male patients | 14 | 0.03 | .01 | 0.01, 0.05 | 2.44* | Q = 5.96, df = 1 |
| % minority patients | 8 | 0.01 | .02 | −0.02, 0.04 | 0.86 | Q = 0.75, df = 1 |
Note:
p<.05,
p<.01,
p<.001
Regarding moderators of the effect of FIT on functioning outcomes, effects were robust across age groups and racial/ethnic groups; however, gender significantly moderated FIT effects, with samples containing a larger percentage of male patients demonstrating greater functional improvements. There was a significant effect of treatment format, with individual family treatments yielding larger effects on functioning than group treatments. Although the overall continuous extent of family involvement in the treatment was not a significant moderator, the inclusion within FITs of specific attention to reducing family accommodation resulted in significantly larger improvements in functioning relative to treatments that did not address family accommodation. No other potential moderators examined were significant.
Discussion
The present meta-analysis quantitatively synthesized the empirical literature on family-inclusive psychological treatments for OCD (FITs). Overall, FITs were associated with a large effect on OCD symptoms across studies utilizing both within-groups and between-groups designs. The effect was robust across acute and follow-up time points, indicating that these improvements in symptom levels are maintained over time. Findings regarding the impact of FITs on OCD symptoms were consistent across a range of patient and treatment protocol variables, suggesting that FITs are associated with highly robust effects on OCD psychopathology. FITs also had a large and robust effect on patient functioning across both acute and follow-up time points, although individual family treatments were associated with a larger effect on patient functioning than group treatments, as were samples with a higher proportion of male patients, relative to samples with lower proportions of male patients. Absolute level of family involvement did not moderate outcomes, however FITs that specifically addressed family accommodation of symptoms were associated with larger effects on functioning than treatments that did not include this element. Collectively, these findings add to the existing OCD treatment outcome literature by highlighting the very positive impact that FITs specifically have on OCD outcomes, and underscore the need to maintain a broadened focus on patient functioning, in addition to symptom response, in clinical decision-making.
Results from this analysis compare favorably with effect sizes reported in previous meta-analyses of psychological treatments for OCD that have not focused on family-inclusive treatments, which have ranged from 0.99 to 1.45 (between-groups pooled d; Olatunji et al., 2013; Watson & Rees, 2008). The results from the present study fall at the high end of these previous meta-analytic estimates, suggesting FITs likely result in enhanced outcomes relative to strictly individual-based treatments for OCD.
The present findings — along with burgeoning research demonstrating that families are highly involved in and impacted by OCD symptoms across the lifespan — highlight the importance of enhancing efforts to disseminate family-inclusive psychological treatments for OCD. Elsewhere in the literature, maladaptive family responses have been associated with poorer treatment outcomes and greater risk of relapse in adult samples (Amir, Freshman, & Foa, 2000; Chambless & Steketee, 1999); incorporating families into the treatment context provides the opportunity to help families develop more adaptive coping in addition to targeting the OCD symptoms themselves.
Group treatment formats may offer more resource-efficient dissemination of FITs, since they require fewer clinician hours than individual treatments. Studies comparing individual (non-FIT) OCD treatment to group treatment have demonstrated mixed results regarding any differences in outcomes between the two formats (Anderson & Rees, 2007). However, we found that individual FITs yield more impressive functional outcomes in comparison to group treatments. At this time, when targeting both OCD symptoms and overall functioning, as resources allow, individual FITs may be the preferred modality.
Attention to family accommodation behaviors in FIT moderated effects on functioning outcomes, although not on overall OCD symptoms. This result is consistent with previous findings suggesting parental accommodation mediates the relationship between children’s OCD symptom severity and their functional impairment (Storch et al., 2007) and reductions in family accommodation precede improvement in OCD symptoms (Piacentini et al., 2011). Assisting family members in strategies to gradually reduce accommodation, in the context of a broader treatment targeting the OCD pathology, appears to result in significant improvement in patients’ overall functional performance. Importantly, research into the effect of accommodation on both patients and family members has largely been conducted in Western cultures, where autonomous functioning is highly valued. In cultural contexts where community and inter-relatedness are more heavily emphasized, accommodation may not demonstrate the same inverse relationship with functioning that has been shown in research to date, and addressing accommodation in treatment may have a different relationship (or no relationship) with outcomes, in contrast to our findings.
The overall extent of family involvement across the FITs did not moderate symptom or functioning outcomes, although the inclusion or absence of treatment content related to family accommodation did. This may simply represent a floor effect, as all studies in the present meta-analysis included at least some level of family involvement. Alternatively, taken together with our finding that the inclusion of specific treatment content does moderate treatment response, it may be the quality of FIT elements, rather than the quantity, that matters. “More is better” may not be accurate when it comes to the benefits of family involvement; rather, specific attention to modifying maladaptive patterns of interaction and developing more effective family coping with symptoms may have a greater impact than sheer number of hours families spend in treatment. This latter interpretation would be useful information for clinicians and families for whom a fully family-based treatment may not always be practical. Indeed, a few focused sessions devoted to the right content may be sufficient to reap the benefits of family-inclusive treatment.
Moreover, it is not clear why FITs on samples with larger proportions of males fared better than FITs on samples with lower proportions of males. Perhaps the higher rates of disruptive behavior problems among males compared to females in the general population and the association between comorbid disruptive behavior disorders among OCD samples and greater family accommodation (Storch, Lewin, Geffken, Morgan, & Murphy, 2010) are relevant. Given the considerable efficacy of family-based treatments for disruptive behavior problems (Comer et al., 2013), it may be that gender distribution serves as a proxy for the rate of disruptive behavior problems in a sample, which in turn is linked with the need for a family-based approach.
The present study has several limitations. First, our results synthesized the available literature regarding family-inclusive psychological treatments for OCD, and cannot speak directly to those populations and interventions that are less well studied. Patient samples in the literature have been relatively homogeneous with regard to race and ethnicity. In addition, we chose a conservative approach to our selection criteria by operating under the assumption that not all studies of treatment for pediatric OCD inherently include family involvement. Therefore, only studies that explicitly reported family involvement were included. Second, relatively fewer eligible studies evaluated group treatment approaches rather than individual family approaches, and fewer studied adult patients rather than children. Although there were a sufficient number of studies in each of these categories to justify meta-analysis (see Field, 2013), a larger κ would increase confidence in the observed pooled effect size estimates. Third, given the great heterogeneity across FITs, as well as the small number of trials for many types of FITs, there was not sufficient power in the present work to examine the relative impacts of all of the possible manifestations of family involvement in OCD treatment (e.g., number of family-only sessions, number of conjoint sessions). Fourth, studies of FITs have generally neglected to include measures of potential mechanisms, such as actual rates of accommodation, family socioeconomic status, or levels of family dysfunction, limiting our ability to examine changes in these factors in the context of treatment response. Robust comparisons of change in these and other variables would help elucidate how FITs achieve their effects and how they might be optimized in response to the needs of particular patient and family presentations. Fifth, for quality control, only peer-reviewed studies were included in our analysis. Our results were quite robust against the “file drawer effect,” but nonetheless it is possible that our results would have been different if unpublished data had been included. Finally, the present study did not make direct comparisons between FITs and individual treatments for OCD, and as such the present findings cannot speak to the relative efficacy of FITs compared to individual treatments. Previous studies that have directly compared FIT and non-FIT approaches have generally found that FITs result in greater symptom improvement for patients, as well as better outcomes on secondary variables such as depression, anxiety, and family functioning (Grunes et al, 2001; Mehta, 1990; Van Noppen et al., 1997).
Adult OCD patients can pose particular challenges in terms of implementing FITs. These patients are less likely to be married than adults without OCD (Koran, 2000), though a sizable minority of adult OCD patients continues to live with their parents (Steketee & Pruyn, 1998). If the patient is unmarried and their parents are unable or unwilling to participate in treatment, finding another suitable participant may be difficult, and in the cases of some more reclusive patients may in fact be irrelevant. To our knowledge, no studies have examined the feasibility or efficacy of including non-family members or individuals who do not currently live with the patient into the treatment. It is possible that such adaptations would prove less efficacious than previously tested FIT protocols for adults, as these non-family members may have less exposure to the OCD pathology or may be less central to the maintenance of OCD symptoms due to living separately and/or reluctance on the part of the patient to disclose the extent of their symptoms. These difficulties may partially explain the relative dearth of non-pediatric samples in studies of FIT. As such, we recommend future work continue to explore the effects of FITs in adult populations, as OCD symptoms are associated with high levels of family distress across the lifespan (Renshaw, Steketee, & Chambless, 2005).
Family-based treatments offer the potential of increasing the effectiveness of existing interventions for OCD by broadening the context of treatment and providing family members with important information and skills to support recovery of affected individuals. The present study demonstrates that FITs are a highly effective form of OCD treatment, yielding large gains in symptom and functional response. Moreover, our quantitative synthesis supports the continued dissemination of FITs for OCD across the lifespan, not simply for affected child populations. Such findings bolster recent concerns regarding off-label psychotropic prescribing for OCD and other anxiety disorders (see Comer et al., 2011), particularly as first-line interventions, and call for the development of innovative methods to expand the availability and accessibility of FITs for OCD. New technologies will likely be central to these efforts. Recently, several research groups have begun to find success applying Internet-based methods for the delivery of FITs for OCD (e.g., Comer et al., in press; Storch, Caporino, et al., 2011). These Internet-based formats for the delivery of FIT use videoconferencing methods to deliver real-time cognitive-behavioral therapy for OCD to affected individuals and their families, regardless of the patient’s geographic proximity to a mental health facility. These preliminary findings are encouraging, and given the present meta-analytic findings it is clear that continued research is needed to examine how new technologies and other innovative methods can be harnessed to further promote the broad availability and accessibility of FITs for individuals suffering with OCD and their families.
Acknowledgments
We thank Dr. John Piacentini, Dr. Else De Haan, and Dr. Jennifer B. Freeman for providing additional study information for this analysis. This work was supported by the National Institutes of Health (NIH) and by the International OCD Foundation.
References
- Abramowitz JS, Baucom DH, Boeding S, Wheaton MG, Pukay-Martin ND, Fabricant LE, Paprocki C, Fischer MS. Treating obsessive-compulsive disorder in intimate relationships: A pilot study of couple-based cognitive-behavior therapy. Behavior Therapy. 2013;44(3):395–407. doi: 10.1016/j.beth.2013.02.005. [DOI] [PubMed] [Google Scholar]
- Amir N, Freshman M, Foa EB. Family distress and involvement in relatives of obsessive-compulsive disorder patients. Journal of Anxiety Disorders. 2000;14(3):209–217. doi: 10.1016/s0887-6185(99)00032-8. [DOI] [PubMed] [Google Scholar]
- Anderson RA, Rees CS. Group versus individual cognitive-behavioural treatment for obsessive-compulsive disorder: a controlled trial. Behaviour Research and Therapy. 2007;45(1):123–137. doi: 10.1016/j.brat.2006.01.016. [DOI] [PubMed] [Google Scholar]
- *.Barrett P, Farrell L, Dadds M, Boulter N. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: Long-term follow-up and predictors of outcome. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(10):1005–1114. doi: 10.1097/01.chi.0000172555.26349.94. [DOI] [PubMed] [Google Scholar]
- *.Barrett P, Healy-Farrell L, March JS. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: a controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(1):46–62. doi: 10.1097/00004583-200401000-00014. [DOI] [PubMed] [Google Scholar]
- *.Benazon NR, Ager J, Rosenberg DR. Cognitive behavior therapy in treatment naïve children and adolescents with obsessive-compulsive disorder: An open trial. Behavior Research and Therapy. 2002;40(5):529–539. doi: 10.1016/s0005-7967(01)00064-x. [DOI] [PubMed] [Google Scholar]
- *.Bolton D, Perrin S. Evaluation of exposure with response-prevention of obsessive compulsive disorder in childhood and adolescence. Journal of Behaviour Therapy and Experimental Psychiatry. 2008;39(1):11–22. doi: 10.1016/j.jbtep.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Calvocoressi L, Lewis B, Harris M, Trufan SJ, Goodman WK, McDougle CJ, Price LH. Family accommodation in obsessive-compulsive disorder. American Journal of Psychiatry. 1995;152:441–443. doi: 10.1176/ajp.152.3.441. [DOI] [PubMed] [Google Scholar]
- *.Chambless DL, Steketee G. Expressed emotion and behavior therapy outcome: a prospective study with obsessive-compulsive and agoraphobic outpatients. Journal of Consulting and Clinical Psychology. 1999;67(5):658–665. doi: 10.1037//0022-006x.67.5.658. [DOI] [PubMed] [Google Scholar]
- Comer JS, Chow C, Chan P, Cooper-Vince C, Wilson LAS. Psychosocial treatment efficacy for disruptive behavior problems in young children: A meta-analytic examination. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:26–36. doi: 10.1016/j.jaac.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince CE, Kerns CE, Chan PT, Edson AL, Freeman JB. Internet-delivered, family-based treatment for early-onset OCD: Rationale, considerations, and a preliminary case series. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Mojtabai R, Olfson M. National trends in the antipsychotic treatment of psychiatric outpatients with anxiety disorders. American Journal of Psychiatry. 2011;168(10):1057–1065. doi: 10.1176/appi.ajp.2011.11010087. [DOI] [PubMed] [Google Scholar]
- *.de Haan E, van Oppen P, van Balkom AJ, Spinhoven P, Hoogduin KA, Van Dyck R. Prediction of outcome and early vs. late improvement in OCD patients treated with cognitive behaviour therapy and pharmacotherapy. Acta Psychiatrica Scandinavica. 1998;96(5):354–361. doi: 10.1111/j.1600-0447.1997.tb09929.x. [DOI] [PubMed] [Google Scholar]
- *.Farrell LJ, Schlup B, Boschen MJ. Cognitive-behavioral treatment of childhood obsessive-compulsive disorder in community-based clinical practice: Clinical significance and benchmarking against efficacy. Behavior Research and Therapy. 2010;48(5):409–417. doi: 10.1016/j.brat.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Field AP. Meta-analysis of correlation coefficients. A Monte-Carlo comparison of fixed- and random-effects methods. Psychological Methods. 2001;6:161–180. doi: 10.1037/1082-989x.6.2.161. [DOI] [PubMed] [Google Scholar]
- Field AP. Meta-analysis in clinical psychology research. In: Comer JS, Kendall PC, editors. The Oxford Handbook of Research Strategies for Clinical Psychology. NY: Oxford University Press; 2013. [Google Scholar]
- Field AP, Gillett R. How to do a meta-analysis. British Journal of Mathematical and Statistical Psychology. 2010;63:665–694. doi: 10.1348/000711010X502733. [DOI] [PubMed] [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, Tu X. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162:151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Franklin ME, Abramowitz JS, Kozak MJ, Levine J, Foa EB. Effectiveness of exposure and ritual prevention for obsessive-compulsive disorder: A comparison of randomized and clinic patients. Journal of Consulting and Clinical Psychology. 2000;68:594–602. [PubMed] [Google Scholar]
- *.Franklin ME, Sapyta J, Freeman JB, Khanna M, Compton S, Almirall D, March JS. Cognitive behavior therapy augmentation of pharmacotherapy in pediatric obsessive-compulsive disorder: The Pediatric OCD Treatment Study II (POTS II) randomized controlled trial. Journal of the American Medical Association. 2011;306(11):1224–1232. doi: 10.1001/jama.2011.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman JB, Garcia AM. Family-based treatment for young children with OCD workbook. USA: Oxford University Press; 2008. [Google Scholar]
- *.Freeman JB, Garcia AM, Coyne L, Ale C, Przeworski A, Himle M, Compton S, Leonard HL. Early childhood OCD: Preliminary findings from a family-based cognitive-behavioral approach. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(5):593–602. doi: 10.1097/CHI.0b013e31816765f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia AM, Sapyta JJ, Moore PS, Freeman JB, Franklin ME, March JS, Foa EB. Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):1024–1033. doi: 10.1016/j.jaac.2010.06.013. quiz 1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greist JH, Jefferson JW, Kobak KA, Katzelnick DJ, Serlin RC. Efficacy and tolerability of serotonin transport inhibitors in obsessive-compulsive disorder: A meta-analysis. Archives of General Psychiatry. 1995;52(1):53–60. doi: 10.1001/archpsyc.1995.03950130053006. [DOI] [PubMed] [Google Scholar]
- *.Grunes MS, Neziroglu F, McKay D. Family involvement in the behavioral treatment of obsessive compulsive disorder. Behavior Therapy. 2001;32:803–820. [Google Scholar]
- *.Haland AT, Vogel PA, Lie B, Launes G, Pripp AH, Himle JA. Behavioural group therapy for obsessive-compulsive disorder in Norway. An open community-based trial. Behaviour Research and Therapy. 2010;48(6):547–554. doi: 10.1016/j.brat.2010.03.005. [DOI] [PubMed] [Google Scholar]
- Hedges LV. Meta-analysis. Journal of Educational Statistics. 1992;17:279–296. [Google Scholar]
- Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3:486–504. [Google Scholar]
- *.Himle JA, Rassi S, Haghighatgou H, Krone KP, Nesse RM, Abelson J. Group behavioral therapy of obsessive-compulsive disorder: Seven vs. twelve-week outcomes. Depression and Anxiety. 2001;13(4):161–165. [PubMed] [Google Scholar]
- *.Keeley ML, Geffken GR, Ricketts E, McNamara JP, Storch EA. The therapeutic alliance in the cognitive behavioral treatment of pediatric obsessive-compulsive disorder. Journal of Anxiety Disorders. 2011;25(7):855–863. doi: 10.1016/j.janxdis.2011.03.017. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koran LM. Quality of life in obsessive-compulsive disorder. Psychiatric Clinics of North America. 2000;23:509–517. doi: 10.1016/s0193-953x(05)70177-5. [DOI] [PubMed] [Google Scholar]
- Lebowitz E, Panza K, Su J, Bloch M. Family accommodation in obsessive compulsive disorder. Expert Review of Neurotherapeutics. 2012;12(2):229–238. doi: 10.1586/ern.11.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. In: Bickman L, Rog DJ, editors. Applied Social Research Methods Series. Vol. 49. Thousand Oaks, CA: Sage; 2000. pp. 1–240. [Google Scholar]
- Maher MJ, Huppert JD, Chen H, Duan N, Foa EB, Leibowitz MR, Simpson HB. Moderators and predictors of response to cognitive-behavioral therapy augmentation of pharmacotherapy in obsessive-compulsive disorder. Psychological Medicine. 2010;40(12):2013–2023. doi: 10.1017/S0033291710000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Mulle K. OCD in children and adolescents: A cognitive behavioral treatment manual. New York, NY: The Guildford Press; 1998. [Google Scholar]
- *.March JS, Mulle K, Herbel B. Behavioral psychotherapy for children and adolescents with obsessive-compulsive disorder: An open trial of a new protocol-driven treatment package. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(3):333–341. doi: 10.1097/00004583-199403000-00006. [DOI] [PubMed] [Google Scholar]
- *.Martin JL, Thienemann M. Group cognitive-behavior therapy with family involvement for middle-school-age children with obsessive-compulsive disorder: A pilot study. Child Psychiatry and Human Development. 2005;36(1):113–127. doi: 10.1007/s10578-005-3496-y. [DOI] [PubMed] [Google Scholar]
- *.Mehta M. A comparative study of family-based and patient-based behavioural management in obsessive-compulsive disorder. British Journal of Psychiatry. 1990;157:133–135. doi: 10.1192/bjp.157.1.133. [DOI] [PubMed] [Google Scholar]
- Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2009;77:355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.O’Leary EM, Barrett P, Fjermestad KW. Cognitive-behavioral family treatment for childhood obsessive-compulsive disorder: A 7-year follow-up study. Journal of Anxiety Disorders. 2009;23(7):973–978. doi: 10.1016/j.janxdis.2009.06.009. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Davis ML, Powers MB, Smits JAJ. Cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analysis of treatment outcome and moderators. Journal of Psychiatric Research. 2013;47:33–41. doi: 10.1016/j.jpsychires.2012.08.020. [DOI] [PubMed] [Google Scholar]
- *.Pediatric OCD Treatment Study (POTS) Team. Cognitive-behavioral therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: The Pediatric OCD Treatment Study (POTS) randomized controlled trial. Journal of the American Medical Association. 2004;292(16):1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- *.Peris TS, Piacentini J. Optimizing treatment for complex cases of childhood obsessive compulsive disorder: A preliminary trial. Journal of Clinical Child and Adolescent Psychology. 2012;42(1):1–8. doi: 10.1080/15374416.2012.673162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Sugar CA, Bergman RL, Chang S, Langley A, Piacentini J. Family factors predict treatment outcome for pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2012;80(2):255–263. doi: 10.1037/a0027084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Piacentini J, Bergman RL, Chang S, Langley A, Peris R, Wood JJ, McCracken J. Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:1149–1161. doi: 10.1016/j.jaac.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Piacentini J, Bergman RL, Jacobs C, McCracken JT, Kretchman J. Open trial of cognitive behavior therapy for childhood obsessive-compulsive disorder. Journal of Anxiety Disorders. 2002;16(2):207–219. doi: 10.1016/s0887-6185(02)00096-8. [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Steketee G, Chambless DL. Involving family members in the treatment of OCD. Cognitive Behavior Therapy. 2005;34(3):164–175. doi: 10.1080/16506070510043732. [DOI] [PubMed] [Google Scholar]
- Rosa AC, Diniz JB, Fossaluza V, Torres AR, Fontenelle LF, de Mathis AS, da Conceicāo Rosário M, Miguel EC, Shavitt RG. Clinical correlates of social adjustment in patients with obsessive-compulsive disorder. Journal of Psychiatric Research. 2012;46(10):1286–1292. doi: 10.1016/j,jpsychires.2012.05.019. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. Meta-analytic procedures for social research. London, England: Sage; 1991. [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15(1):53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoog G, Skoog I. A 40-year follow-up of patients with obsessive compulsive disorder. Archives of General Psychiatry. 1999;56(2):121–127. doi: 10.1001/archpsyc.56.2.121. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC, Bisgaard C, Munk-Jorgensen P, Helenius D. Family aggregation and risk factors of obsessive-compulsive disorders in a nationwide three-generation study. Depression and Anxiety. 2013;30(12):1177–1184. doi: 10.1002/da.22163. [DOI] [PubMed] [Google Scholar]
- *.Steketee G, Chambless DL. Effects of axis I and II comorbidity on behavior therapy outcome for obsessive-compulsive disorder and agoraphobia. Comprehensive Psychiatry. 2001;42(1):76–86. doi: 10.1053/comp.2001.19746. [DOI] [PubMed] [Google Scholar]
- *.Storch EA, Caporino NE, Morgan JR, Lewin AB, Rojas A, Brauer L, Larson MJ, Murphy TK. Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Research. 2011;189(3):407–412. doi: 10.1016/j.psychres.2011.05.047. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK, Grabill K. Family accommodation in pediatric obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psychology. 2007;36(2):207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- *.Storch EA, Geffken GR, Merlo LJ, Mann G, Duke D, Munson M, Adkins J, Grabill KM, Murphy TK, Goodman WK. Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: comparison of intensive and weekly approaches. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(4):469–478. doi: 10.1097/chi.0b013e31803062e7. [DOI] [PubMed] [Google Scholar]
- *.Storch EA, Lehmkuhl HD, Ricketts E, Geffken GR, Marien W, Murphy TK. An open trial of intensive family based cognitive-behavioral therapy in youth with obsessive-compulsive disorder who are medication partial responders or nonresponders. Journal of Clinical Child and Adolescent Psychology. 2010;39(2):260–268. doi: 10.1080/15374410903532676. [DOI] [PubMed] [Google Scholar]
- Storch EA, Lewin AB, Geffken GR, Morgan JR, Murphy TK. The role of comorbid disruptive behavior in the clinical expression of pediatric obsessive-compulsive disorder. Behaviour Research and Therapy. 2010;48:1204–1210. doi: 10.1016/j.brat.2010.09.004. [DOI] [PubMed] [Google Scholar]
- *.Thienemann M, Martin J, Cregger B, Thompson HB, Dyer-Friedman J. Manual-driven group cognitive-behavioral therapy for adolescents with obsessive-compulsive disorder: A pilot study. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(11):1254–1260. doi: 10.1097/00004583-200111000-00004. [DOI] [PubMed] [Google Scholar]
- Tollefson GD, Rampey HR, Potvin JH, et al. A multicenter investigation of fixed dose fluoxetine in the treatment of obsessive-compulsive disorder. Archives of General Psychiatry. 1994;51:559–567. doi: 10.1001/archpsyc.1994.03950070051010. [DOI] [PubMed] [Google Scholar]
- *.Valderhaug R, Larsson B, Gotestam KG, Piacentini J. An open clinical trial of cognitive-behaviour therapy in children and adolescents with obsessive-compulsive disorder administered in regular outpatient clinics. Behaviour Research and Therapy. 2007;45(3):577–589. doi: 10.1016/j.brat.2006.04.011. [DOI] [PubMed] [Google Scholar]
- *.Van Noppen B, Steketee G, McCorkle BH, Pato M. Group and multifamily behavioral treatment for obsessive compulsive disorder: A pilot study. Journal of Anxiety Disorders. 1997;11:431–446. doi: 10.1016/s0887-6185(97)00021-2. [DOI] [PubMed] [Google Scholar]
- Watson HJ, Rees CS. Meta-analysis of randomized, controlled treatment trials for pediatric obsessive-compulsive disorder. Journal of Child Psychology and Psychiatry. 2008;49(5):489–498. doi: 10.11111/j.1469-7610.2007.01875.x. [DOI] [PubMed] [Google Scholar]
- *.Wever C, Rey JM. Juvenile obsessive-compulsive disorder. Australian and New Zealand Journal of Psychiatry. 1997;31(1):105–113. doi: 10.3109/00048679709073806. [DOI] [PubMed] [Google Scholar]
- Williams M, Powers M, Yun YG, Foa E. Minority participation in randomized controlled trials for obsessive-compulsive disorder. Journal of Anxiety Disorders. 2010;24(2):171–177. doi: 10.1016/j.janxdis.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]