Abstract
Objective To investigate whether an early rehabilitation intervention initiated during acute admission for exacerbations of chronic respiratory disease reduces the risk of readmission over 12 months and ameliorates the negative effects of the episode on physical performance and health status.
Design Prospective, randomised controlled trial.
Setting An acute cardiorespiratory unit in a teaching hospital and an acute medical unit in an affiliated teaching district general hospital, United Kingdom.
Participants 389 patients aged between 45 and 93 who within 48 hours of admission to hospital with an exacerbation of chronic respiratory disease were randomised to an early rehabilitation intervention (n=196) or to usual care (n=193).
Main outcome measures The primary outcome was readmission rate at 12 months. Secondary outcomes included number of hospital days, mortality, physical performance, and health status. The primary analysis was by intention to treat, with prespecified per protocol analysis as a secondary outcome.
Interventions Participants in the early rehabilitation group received a six week intervention, started within 48 hours of admission. The intervention comprised prescribed, progressive aerobic, resistance, and neuromuscular electrical stimulation training. Patients also received a self management and education package.
Results Of the 389 participants, 320 (82%) had a primary diagnosis of chronic obstructive pulmonary disease. 233 (60%) were readmitted at least once in the following year (62% in the intervention group and 58% in the control group). No significant difference between groups was found (hazard ratio 1.1, 95% confidence interval 0.86 to 1.43, P=0.4). An increase in mortality was seen in the intervention group at one year (odds ratio 1.74, 95% confidence interval 1.05 to 2.88, P=0.03). Significant recovery in physical performance and health status was seen after discharge in both groups, with no significant difference between groups at one year.
Conclusion Early rehabilitation during hospital admission for chronic respiratory disease did not reduce the risk of subsequent readmission or enhance recovery of physical function following the event over 12 months. Mortality at 12 months was higher in the intervention group. The results suggest that beyond current standard physiotherapy practice, progressive exercise rehabilitation should not be started during the early stages of the acute illness.
Trial registration Current Controlled Trials ISRCTN05557928.
Introduction
Patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary disease and other chronic respiratory diseases, such as chronic asthma, bronchiectasis, and interstitial lung disease, are at increased risk of mortality, morbidity, and further episodes of unscheduled hospital admission. Acute exacerbation of chronic obstructive pulmonary disease is the second most common cause for unscheduled hospital admission in the United Kingdom, accounting for the largest component of health costs associated with the disease.1
Admission to hospital has negative effects on physical performance and health status from which the patient may not fully recover.2 3 Treatment of the acute episode is predominantly targeted at improvement of ventilatory function, with little attention paid to these wider systemic impacts. Consequently, physical performance and activity may be reduced for a prolonged period after hospital stay, increasing the risk of readmission.2 4 5
Pulmonary rehabilitation is of established efficacy in stable chronic respiratory diseases, and small scale trials of pulmonary rehabilitation delivered after discharge from hospital for chronic obstructive pulmonary disease have suggested a reduction in the short term risk of readmission. However, the effects of the acute episode on physical fitness and skeletal muscle function may occur rapidly during the inpatient phase4 6 suggesting that a rehabilitation intervention delivered at the time of the acute illness might preserve physical function and reduce the risk of subsequent admission to hospital. This is supported by previous small scale trials of exercise based therapy during acute exacerbation of chronic obstructive pulmonary disease, which have suggested such interventions are feasible and may be effective.7 8 9 An early exercise/mobility intervention is a component of wider enhanced recovery programmes, which have been successfully implemented for patients undergoing elective surgery but have not been widely applied to unscheduled medical admissions.10 11 12
We conducted a randomised clinical trial of a progressive, exercise based rehabilitation intervention delivered immediately after unscheduled admission to hospital for an acute exacerbation of chronic respiratory disease. The principles underpinning the intervention were that it should be delivered early in the admission with the aim of preventing decline in physical performance, should be provided intensively making best use of the time spent in hospital, and should be continued after discharge to maximise the restoration of physical performance and activity and obviate the need to extend the hospital stay to provide treatment. We hypothesised that this intervention would reduce the risk of readmission in the following year and accelerate recovery of physical functioning.
Methods
Study design
This was a prospective, parallel group, single blind randomised controlled trial conducted in two centres in the United Kingdom: an acute cardiorespiratory unit in a teaching hospital (Glenfield Hospital, University Hospitals of Leicester) and an acute medical unit in an affiliated teaching district general hospital (Kettering General Hospital).
We randomly allocated patients to one of two treatment groups: an early rehabilitation group and a usual care group. Participants randomised to the early rehabilitation group received a six week intervention.
Outcomes were measured at baseline, discharge from hospital, six weeks from randomisation, three months, and 12 months.
The nature of the intervention meant that blinding of the participants was not possible, but all investigators performing the outcome measures were blinded to treatment allocation.
Study population
Participants were recruited to the study and randomised within 48 hours of admission to hospital with an exacerbation of chronic respiratory disease. Inclusion criteria were diagnosis of chronic respiratory disease (chronic obstructive pulmonary disease, chronic asthma, bronchiectasis, or interstitial lung disease), self reported breathlessness on exertion when stable (Medical Research Council dyspnoea grade 3 or worse), and age 40 years or greater. Exclusion criteria were inability to provide informed consent; concomitant acute cardiac event; presence of musculoskeletal, neurological, or psychiatric comorbidities that would prevent the delivery of the rehabilitation intervention; and more than four emergency admissions to hospital for any cause in the previous 12 months.
Usual care group
Participants assigned to the usual care group received standard care from the ward clinical physiotherapy team as directed by the responsible clinical team. This included physiotherapist delivered techniques for airway clearance, assessment and supervision of mobility, and advice on smoking cessation. Nutritional status was assessed using the malnutrition universal screening tool score in all participants, and referral for dietetic advice and nutritional support was carried out if appropriate. No supervised or progressive exercise programme was provided during the admission or immediately after discharge, but outpatient pulmonary rehabilitation was offered to all participants three months after discharge as part of standard care.
Early rehabilitation group
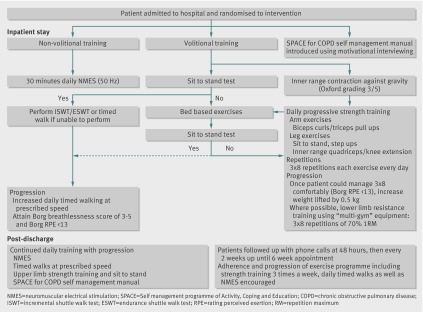
Participants allocated to the intervention group started early rehabilitation within 48 hours of hospital admission. In addition to usual care, they also received daily, supervised volitional (strength and aerobic training) and non-volitional (neuromuscular electrical stimulation) techniques. The pulmonary rehabilitation team, consisting of physiotherapists and nurses, delivered the early rehabilitation programme. The exercise programme was individually prescribed and progressed (fig 1). Early rehabilitation was performed on the acute medical ward and by the participants’ bedside. After discharge, participants underwent an unsupervised home based programme, supported by telephone consultations. Those who were readmitted after the six week intervention period did not receive a further early rehabilitation intervention.
Fig 1 Training intervention algorithm. Prescription protocol for progressive aerobic, resistance, and non-volitional training
Aerobic training
Daily walking was performed at a set walking speed predetermined by the endurance shuttle walk test at 85% oxygen consumption (VO2) max (calculated from the incremental shuttle walk test). If participants were not able to walk 10 m in 20 seconds (1.78 km/h) then they performed daily timed walks at a manageable speed. Walking time was progressed at the prescribed walking speed, maintaining a Borg breathlessness score of between 3 and 5 (from 0 for no breathlessness to 10 for the most severe breathlessness) and a Borg exertion score for rating perceived exertion <13 (from 6 for no exertion at all to 20 for maximal exertion).
Strength training
Patients completed daily strength training, comprising three sets of eight repetitions resistance training exercises with weights. This was performed for biceps curls, triceps curls, knee extension, sit to stand, and step-ups, which was based on the one repetition maximum. Once the rate of perceived exertion was <13 the weight was increased.
Non-volitional training
The intervention team initially supervised the neuromuscular electrical stimulation until participants were deemed able to use independently. Neuromuscular electrical stimulation (Empi 300PV, MN) was applied to both quadriceps synchronously for 30 minutes daily. The stimulation protocol consisted of a symmetrical biphasic pulse at 50 Hz, pulse duration of 300 ms, 15 seconds on and five seconds off. The intensity was increased by the therapist or patient according to tolerance. Neuromuscular electrical stimulation continued throughout both the inpatient and the outpatient intervention period.
Supported self management programme
The intervention team delivered education using the SPACE (Self management programme of Activity, Coping and Education) manual for chronic obstructive pulmonary disease, a structured programme of exercise, education, and psychosocial support. Motivational interviewing techniques were used to introduce patients to the manual and to familiarise them with the content. The manual was used throughout the participants’ inpatient stay and in the subsequent discussions during telephone calls.
Post-discharge training
After discharge we advised the participants to follow a progressive walking based home exercise programme and to continue daily neuromuscular electrical stimulation, and we encouraged them to follow the self management programme. The post-discharge training was supported by telephone consultations from the pulmonary rehabilitation intervention team, using motivational interviewing techniques, at 48 hours, two weeks, and four weeks. Participants were encouraged with adherence and progression of their exercise programme. Participants were also able to discuss any concerns that they may have and were given advice on ongoing management of their condition.
Primary and secondary outcomes
The primary endpoint was unplanned readmissions to hospital at 12 months for all causes, adjusted for site. We captured hospital admissions in the follow-up period using hospital databases and general practice records. Secondary analyses of healthcare utilisation included per protocol analysis (defined as retention within the trial during the six week intervention period), time to first readmission, total days spent in hospital, cause of admission (respiratory or non-respiratory), and mortality (including cause of death and time from primary admission). Secondary functional outcome measures were recorded at baseline (where feasible), discharge from hospital, six weeks, and three and 12 months. At baseline, the acute illness prevented the recording of physiological and exercise performance measures other than quadriceps strength.
Spirometry was measured to British Thoracic Society standards.13 Exercise performance was measured using the incremental shuttle walk test14 and endurance shuttle walk test.15 Maximal isometric quadriceps strength was measured using an isometric dynamometer.16 Disease specific health status was measured using the St George’s respiratory questionnaire.17
Statistical analysis
The clinical trials unit at the University of Leicester coordinated randomisation by an automated internet based service (www.sealedenvelope.com). Participants were randomly allocated in a simple 1:1 ratio.
We used an intention to treat analysis to assess the primary outcome. The study was powered to detect a difference in readmission rate of 15% (usual care 40%, early rehabilitation 25%), requiring 152 in each group (power 80%, two sided α=0.05). With the expected mortality (20%) we planned to recruit 190 participants to each group (380 in total). Analyses were performed using STATA version 13. We compared baseline measures using the t test for parametric data, Mann-Whitney U test for non-parametric data, and χ2 tests for categorical data. The rate of admission to hospital was calculated using a Fine-Gray competing risks analysis, with death as the competing risk (adjusted for site), presented as hazard ratios.18 We used negative binomial regression (offset by natural log of time to death) to calculate secondary outcomes of differences in number of hospital admissions and hospital days, presented as incident rate ratios. Binary logistic regression was used to calculate mortality odds ratios. Hazard and odds ratios are presented in comparison with the usual care group. Secondary healthcare utilisation measures are presented both unadjusted (other than for site) and adjusted for covariables known to affect the risk of hospital admission (site, age, diagnosis, Medical Research Council grade for dyspnoea, previous hospital stays, quadriceps strength at baseline, number of comorbidities). For the utilisation of healthcare we conducted a predefined per protocol analysis, defined as those who remained in the study during the intervention period. We analysed longitudinal changes in physiological outcomes using repeated measures analysis of variance (corrected for site). Bonferroni correction was applied for analyses at six weeks and three months.
We used multiple imputation by chained equations to replace missing data for the functional measures (incremental shuttle walk test, endurance shuttle walk test, maximal isometric quadriceps strength, St George’s respiratory questionnaire). Forty imputed datasets were created (see supplementary appendix).
Results
Recruitment and baseline characteristics
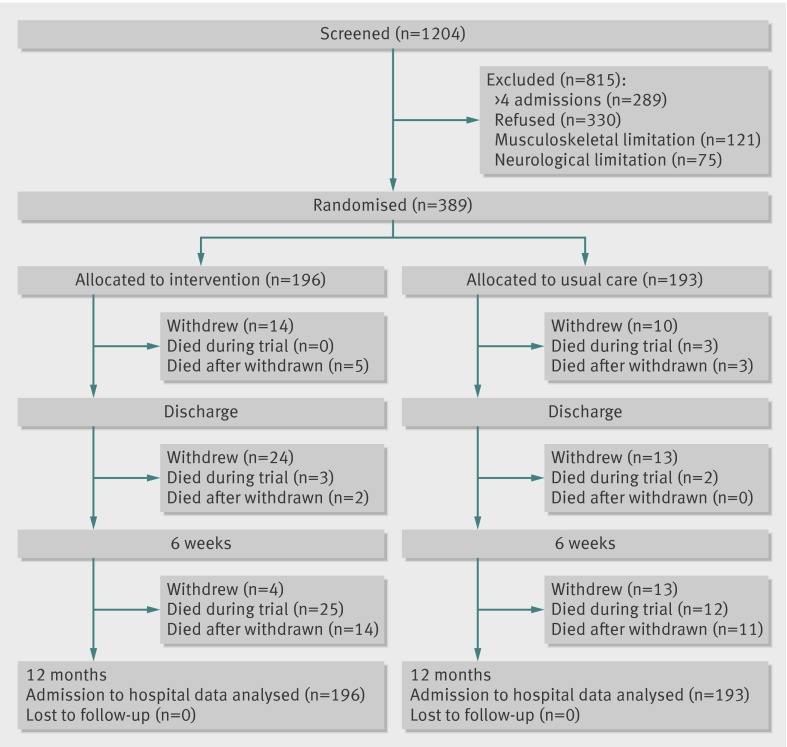
Overall, 389 participants were recruited between January 2010 and September 2011, with final follow-up in September 2012: 196 were randomised to early rehabilitation and 193 to usual care. Recruitment was similar at both sites (Glenfield n=200, Kettering n=189). Figure 2 shows the flow of screening, randomisation, and follow-up in the study. No statistically significant differences for personal characteristics and measures were observed between the intervention and usual care groups at baseline (table 1). The forced expiratory volume in one second recorded in the stable state before the index admission (available in 136 (69%) and 131 (68%) of the intervention and usual care groups, respectively) was significantly lower in the intervention group, although spirometry recorded at discharge did not differ significantly between the groups (n=332, P=0.1).
Fig 2 Flow of participants through study
Table 1.
Personal characteristics and baseline measures. Values are numbers (percentages) unless stated otherwise]
| Variables | Usual care (n=193) | Early rehabilitation (n=196) |
|---|---|---|
| Mean (SD) age (years) | 71.2 (10.0) | 71.1 (9.4) |
| Men | 85 (44) | 88 (45) |
| Mean (SD) body mass index | 26.3 (7.1) | 26.6 (6.9) |
| Median (interquartile range) baseline MRC dyspnoea grade | 4 (3-4) | 4 (3-4) |
| Median (interquartile range) No of comorbidities | 2 (1-3) | 2 (2-3) |
| Mean (SD) previous FEV1 (L)* | 1.28 (0.64) | 1.12 (0.61) |
| Mean (SD) previous FEV1/FVC (%)* | 52.9 (18.3) | 49.5 (16.4) |
| Previous FEV1 (% predicted)* | 57.4 (23.6) | 51.9 (25.1) |
| Mean (SD) pack years | 41 (30) | 46 (30) |
| Smoking: | ||
| Current | 40 (21) | 43 (22) |
| Former | 137 (71) | 136 (70) |
| Never | 16 (8) | 16 (8) |
| Previous pulmonary rehabilitation | 62 (32) | 73 (37) |
| Home oxygen | 50 (26) | 55 (28) |
| Hospital admissions in previous year: | ||
| None | 100 (52) | 105 (54) |
| 1 | 53 (27) | 48 (24) |
| 2-4 | 40 (21) | 43 (22) |
| Primary diagnosis: | ||
| Chronic obstructive pulmonary disease | 151 (78) | 169 (86) |
| Chronic asthma | 17 (9) | 11 (6) |
| Interstitial lung disease | 13 (7) | 8 (4) |
| Bronchiectasis | 12 (6) | 8 (4) |
| Mean (SD) quadriceps strength on admission (kg) | 13.4 (7.6) | 12.8 (6.8) |
| Median (interquartile range) St Georges respiratory questionnaire total on admission | 68.1 (33.9-90.7) | 67.7 (34.8-94.0) |
| Mean (SD) heart rate on admission (bpm) | 90.4 (15.0) | 92.7 (14.7) |
| Required non-invasive ventilation on admission | 9 (5) | 7 (4) |
MRC=Medical Research Council; FEV1=forced expiratory volume in one second; FVC=forced vital capacity.
*Available in 267 participants (usual care n=136, early rehabilitation n=131).
Index admission
The median length of hospital stay during the index admission was five days (range 1-33 days) for the intervention group and five days (range 1-31 days) for the usual care groups (P=0.9). On admission, 338 (87%) participants received systemic corticosteroids and 317 (82%) received antibiotics, with no significant differences between the groups (P=0.5 and P=0.6). Overall, 271 (70%) participants received supplemental oxygen on admission (no difference between groups, P=0.4). Eleven (3%) deaths occurred during the index admission (six (3%) in the usual care group and five (3%) in the early rehabilitation group, P=0.3), of whom eight of the 11 (73%) had withdrawn from the trial before death.
Adherence to early rehabilitation training
A total of 165 (86%) participants performed inpatient aerobic training, 176 (90%) inpatient resistance training, and 176 (90%) inpatient neuromuscular electrical stimulation training. The mean number of sessions during the inpatient training was 2.7 (SD 2.6) for aerobic training, 2.5 (SD 1.9) for resistance training, and 3.6 (SD 3.2) for neuromuscular electrical stimulation training. This was associated with increases in exercise training walk times (76 s, 95% confidence interval 56 to 96 s, P<0.001), intensity of neuromuscular electrical stimulation training (4 mA, 95% confidence interval 3 to 5 mA, P<0.001), and weight used in resistance training (100 g, 95% confidence interval 60 to 140 g, P<0.001).
After discharge further improvements were reported in walking time (304 s, 95% confidence interval 152 to 457 s, P<0.001) but the change in progression of resistance training was not significant. At the end of the intervention period, continued daily adherence to the home programme was reported by 54% of participants for aerobic training and 61% for resistance training.
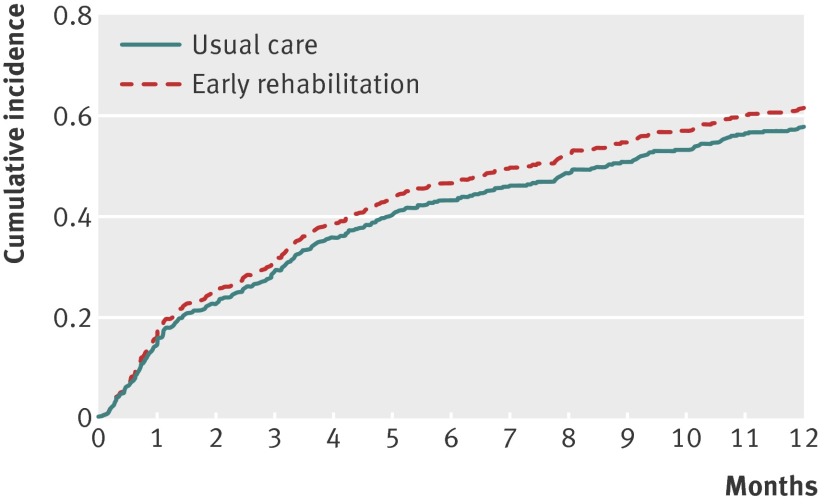
Hospital readmissions
During the follow-up period, 233 (60%) participants were readmitted, with 599 admissions. A respiratory cause accounted for 447 (75%) of these readmissions. The difference in the number of participants with at least one readmission was not significant; usual care 111/193 (58%), early rehabilitation 122/196 (62%): hazard ratio 1.1 (95% confidence interval 0.86 to 1.43), P=0.4. Figure 3 shows the risk of readmission over time. For each patient there was a mean of 1.54 (95% confidence interval 1.33 to 1.75) hospital admissions in the year after the index admission, with no difference between groups (P=0.9). Table 2 presents the data for admissions for respiratory and non-respiratory causes. The median time to the first hospital admission did not differ significantly (89 days for usual care and 93.5 days for early rehabilitation, P=0.4).
Fig 3 Cumulative incidence of hospital readmission, using competing risks regression analysis, in usual care and early rehabilitation groups. The groups did not differ (P=0.4)
Table 2.
Healthcare utilisation. Comparison of number of hospital admissions per patient and hospital days per patient in 12 months after admission. Values are means (standard deviations) unless stated otherwise
| Variables | Usual care | Early rehabilitation | Adjusted for site only* | Adjusted for covariates† | ||
|---|---|---|---|---|---|---|
| Incidence rate ratio (95% CI) | P value | Incidence rate ratio (95% CI) | P value | |||
| No of hospital admissions | ||||||
| Intention to treat: | ||||||
| Total | .1.60 (2.29) | 1.48 (1.89) | 1.02 (0.76 to 1.35) | 0.9 | 0.98 (0.74 to 1.30) | 0.9 |
| Respiratory | 1.20 (1.94) | 1.10 (1.64) | 1.02 (0.73 to 1.41) | 0.9 | 0.99 (0.72 to 1.37) | 1.0 |
| Non-respiratory | 0.39 (0.90) | 0.39 (0.81) | 1.04 (0.66 to 1.64) | 0.9 | 1.09 (0.71 to 1.70) | 0.7 |
| Per protocol: | ||||||
| Total | 1.67 (2.39) | 1.49 (1.87) | 0.92 (0.68 to 1.26) | 0.6 | 0.91 (0.67 to 1.22) | 0.5 |
| Respiratory | 1.28 (2.02) | 1.14 (1.65) | 0.95 (0.67 to 1.34) | 0.8 | 0.94 (0.67 to 1.33) | 0.7 |
| Non-respiratory | 0.39 (0.92) | 0.35 (0.75) | 0.87 (0.52 to 1.45) | 0.6 | 0.95 (0.58 to 1.56) | 0.9 |
| No of hospital days | ||||||
| Intention to treat: | ||||||
| Total | 14.8 (27.7) | 12.0 (18.0) | 0.95 (0.63 to 1.44) | 0.8 | 0.88 (0.58 to 1.34) | 0.6 |
| Respiratory | 11.2 (23.1) | 9.1 (18.5) | 0.97 (0.60 to 1.59) | 0.9 | 0.93 (0.56 to 1.53) | 0.8 |
| Non-respiratory | 3.6 (12.0) | 3.5 (9.3) | 1.24 (0.57 to 2.68) | 0.6 | 1.17 (0.55 to 2.46) | 0.7 |
| Per protocol: | ||||||
| Total | 15.4 (28.7) | 11.1 (16.2) | 0.81 (0.52 to 1.28) | 0.4 | 0.75 (0.48 to 1.19) | 0.2 |
| Respiratory | 11.9 (24.0) | 8.2 (13.7) | 0.83 (0.49 to 1.41) | 0.5 | 0.80 (0.47 to 1.38) | 0.4 |
| Non-respiratory | 3.5 (12.0) | 2.9 (8.0) | 0.95 (0.39 to 2.28) | 0.9 | 1.16 (0.50 to 2.73) | 0.7 |
Table shows both intention to treat and per protocol analyses, defined as participants who remained within the study during the six week intervention period. Analyses are shown both unadjusted and adjusted for covariates. Incident rate ratio is relative to the usual care group and offset for time exposed (time to death).
*Adjusted for site only.
†Adjusted for site, age, diagnosis, previous hospital admissions, quadriceps strength at baseline, Medical Research Council dyspnoea grade, and number of comorbidities.
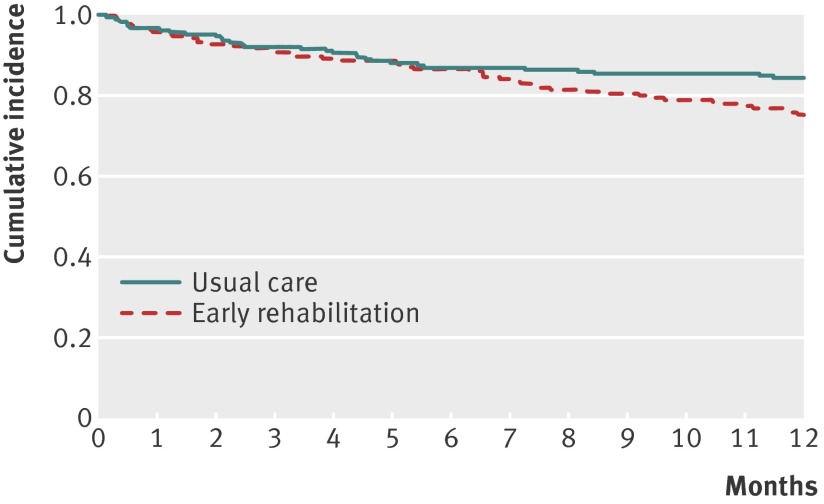
Mortality
Eighty deaths (21%) occurred in the study population during the follow-up period, 23 (29%) occurring without readmission (usual care n=11 (35%), early rehabilitation n=12 (24%)). Unadjusted and adjusted mortality rates were higher in the intervention group at 12 months (31 (16%) in the usual care group and 49 (25%) in the early rehabilitation group, odds ratio 1.74, 95% confidence interval 1.05 to 2.88, P=0.03, fig 4). See supplementary table S2 for causes of death.
Fig 4 Kaplan-Meier plots showing survival in follow-up period
Number of hospital days
During the follow-up period the number of hospital days was 5211 (usual care 2861 and early rehabilitation 2350 days, table 2). The total number of days spent in hospital was similar in the two groups (difference 18%, z=−0.5, P=0.6).
Per protocol analysis
Sixty one (16%) participants withdrew during the intervention period (usual care 12%, early rehabilitation 19%, P=0.04). Compared with those who completed the intervention, those who withdrew were older (P<0.001), had reduced muscle strength (P=0.01), and had higher Medical Research Council dyspnoea scores on admission (P=0.02). See supplementary table S3 for the reasons participants withdrew.
In the per protocol analysis the risk of hospital admission did not differ between the groups (hazard ratio 1.1, 95% confidence interval 0.83 to 1.45, P=0.5, table 2). The total number of days spent in hospital between the groups were similar (early rehabilitation 2616 days, usual care 1752, difference 33%, z=−0.2, P=0.8).
Participants who withdrew within the intervention period were more likely to die than those who completed the intervention, with death occurring in 25 of the 61 participants (41%): odds ratio 3.44 (95% confidence interval 1.91 to 6.19), P<0.001. The difference in mortality between the two groups did not differ at any time point in the per protocol analysis.
Post hoc analysis of subgroup with chronic obstructive pulmonary disease
Three hundred and twenty participants (82%) participants had a primary diagnosis of chronic obstructive pulmonary disease (table 1). Overall, 192 (60%) participants in the chronic obstructive pulmonary disease subgroup were readmitted, with 18 (6%) dying before readmission or the end of the study. Risk of readmission was similar in both groups (hazard ratio 1.19, 95% confidence interval 0.90 to 1.60, P=0.2). There was no difference in the primary and secondary outcomes in the chronic obstructive pulmonary disease subgroup compared with the whole population.
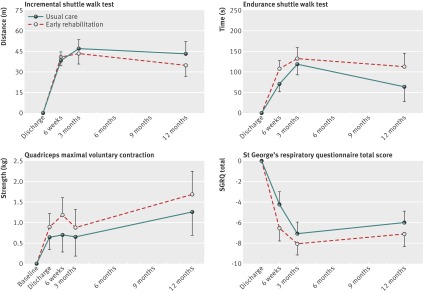
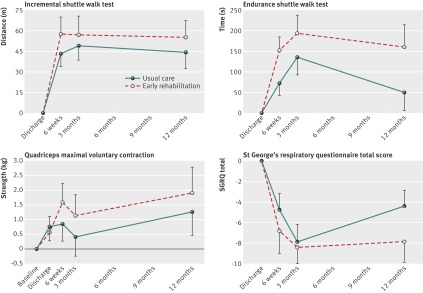
Exercise performance, quadriceps strength, and health related quality of life
Significant improvements in functional performance and health status were observed during the follow-up period in both groups, with the largest change seen in the first six weeks after the index admission (fig 5). No statistically significant between group differences in these measures was observed at 12 months. The measure for the endurance shuttle walk test was significantly higher in the early rehabilitation group at six weeks (P=0.03) but not at other time points during the follow-up period (fig 5).
Fig 5 Intention to treat analysis: change in functional measures (from first measure) in year after admission in all participants. Initial measures were taken at discharge for incremental and endurance shuttle walk tests and at baseline for quadriceps maximal voluntary contraction and St George’s respiratory questionnaire. *P<0.05
To account for the functional insult of further admissions to hospital, an additional reanalysis was conducted in those participants (n=133) who were not readmitted during the follow-up period. There was a trend for a difference in functional performance and health status in the early rehabilitation group compared with the intention to treat population (fig 6). This was statistically significant for the endurance shuttle walk test at six weeks (P=0.02), with a trend at 12 months (P=0.07). No difference was seen in other functional measures (incremental shuttle walk test, quadriceps maximal voluntary contraction, St George’s respiratory questionnaire).
Fig 6 Change in functional measures (from first measure) in year after admission in participants who were not readmitted in subsequent year (n=156) Initial measures were taken at discharge for incremental and endurance shuttle walk tests and at baseline for maximal voluntary contraction and St George’s respiratory questionnaire. *P<0.05
Uptake of pulmonary rehabilitation after three months
Participants were offered pulmonary rehabilitation from three months after recruitment. Uptake in the early rehabilitation group was significantly reduced (14% v 22%, P=0.04)
Discussion
We report a randomised clinical trial of a tailored early rehabilitation intervention aimed at enhancing recovery after unscheduled admission to hospital for acute exacerbation of chronic respiratory disease. The trial was adequately powered to determine the effect of the intervention on subsequent admission to hospital, but the results did not support our hypothesis that the intervention would reduce the number of readmissions in the subsequent 12 months. In addition, mortality was increased in the intervention group at 12 months. Significant within group recovery of muscle strength and walking performance was observed in both groups but, apart from the endurance shuttle walk test at six weeks, there was no significant improvement in physical performance in the intervention group over usual care.
Healthcare utilisation and comparison with previous studies
The lack of reduction in readmissions in the current study is in keeping with a smaller scale study from Hong Kong19 but contrasts with trials of peri-exacerbation pulmonary rehabilitation, where the rate was reduced over the shorter term.9 20 21 There are important differences in the population enrolled and the rehabilitation approach taken in the current trial, rendering comparison with these previous studies difficult. We delivered the intervention during the acute phase of the illness as well as during recovery, with the objective of preserving physical function and enhancing recovery from the episode. We did not provide pulmonary rehabilitation as defined in recent guidelines,22 23 but rather an exercise based intervention modified to suit the setting of the acute illness. This was by necessity lower in intensity, although it was provided daily during the hospital stay using both volitional and non-volitional training techniques. Supervision in the home recovery phase was also lighter but supported by a validated self management programme24 and follow-up telephone support. We recognise, however, that the relatively short length of hospital stay limited the number of supervised rehabilitation sessions undertaken and that the home segment of the intervention was unsupervised.
Participants in the current trial had a greater burden of disease and comorbidities and had lower muscle strength and exercise capacity than most reported pulmonary rehabilitation studies. This higher general level of ill health and frailty in the study population is in keeping with national and international trends for patients admitted to hospital with chronic obstructive pulmonary disease.25 Despite a robust, rigorously applied treatment algorithm (fig 1), it is likely that the intervention could not be delivered with sufficient intensity to produce a significant health benefit. This could have been either because of insufficient supervision or because the population was too unwell and frail to undertake progressive exercise in the circumstances under which they were enrolled.
Safety and mortality
Our finding of increased mortality at the 12 month time point in the intervention group was unexpected and cannot be explained directly from our results. We think it is unlikely that a six week exercise intervention that had no observed health benefit would directly increase the risk of death at 12 months and accept that this observation could have occurred by chance. However, we cannot exclude the possibility that the intervention resulted in alterations in health behaviour that might have modified the response to subsequent acute illness later during the follow-up period, such as delays in seeking medical advice. In keeping with this, the uptake of outpatient pulmonary rehabilitation later during the follow-up seems lower in the intervention group, suggesting that the intervention might have influenced health behaviour. Indeed it is possible that this reduced uptake was one of the mediating factors explaining the lack of reduction in the rate of admission to hospital and the increased mortality in the intervention group. The time course of change in health behaviour in response to an intervention is uncertain, but for conventional pulmonary rehabilitation we know the reverse is true and that the benefits diminish over the following 12 months.26
An increased mortality was seen in the intervention group in a recent trial of a self management intervention27 although as with the current study, the observation could not be explained from data obtained within the trial. The observations in the current trial and that of another trial27are a reminder that interventions such as self management and rehabilitation cannot be assumed to be free of risk. We suggest that future trials put data monitoring and the provision of patient safety in place when they are designed.
Physical performance and natural recovery
Our approach was informed by data from previous observational studies in chronic obstructive pulmonary disease, suggesting a negative short term effect of admission to hospital on muscle strength,4 limited improvement in walking performance after discharge,28 and a greater risk of readmission in patients who remained inactive in the month after discharge.2 However, we observed significant within group improvements in muscle strength, field walking performance, and health status in both groups in the three months after discharge, with limited additional gains observed in the intervention group. We did observe a more rapid recovery of endurance walking performance in the intervention group over usual care at six weeks, but this difference was not significant by three months. Some participants may have recovered naturally and achieved excellent reablement with the assistance of conventional hospital physiotherapy, which was part of usual care. Conversely, others in the early rehabilitation group may have not returned to baseline function because the intervention was insufficiently intense or they did not adequately adhere to the programme after discharge.29 Interestingly, the analysis of physical performance in the subgroup of patients who were not readmitted, indicated enhanced gains in performance in the intervention group. This might indicate that benefits from the intervention are conferred as long as the process is not disrupted by further unplanned admissions to hospital.
We observed an 18% difference in the total number of bed days in the intervention group compared with usual care, although this was not statistically significant, which is in keeping with trials of pulmonary rehabilitation in stable chronic obstructive pulmonary disease.26 This could suggest that an exercise intervention may not influence the number of subsequent exacerbations but might ameliorate their impact on the patient, facilitating recovery and earlier discharge. Conversely, the magnified effect on subsequent hospital bed days in those patients who completed the intervention may be indicative of the efficacy of the intervention or identified a group of patients in better health who were more able to comply with the programme and therefore spent fewer days in hospital in the subsequent year.
Comparison with other strategies after acute hospital stay
A feature of the intervention in the current trial was the shift from supervised inpatient therapy to unsupervised home exercise facilitated by the provision of a self management manual along with telephone support. Length of hospital stay was five days, which would be considered standard in the United Kingdom but relatively short compared with other healthcare systems, and this limited the opportunity for supervised rehabilitation in the current trial. In many respects our intervention resembles elements of post-surgical enhanced recovery programmes or supported self management programmes rather than conventional pulmonary rehabilitation. Our results suggest caution is needed in applying such programmes to recovery from acute illness, particularly exacerbation of chronic respiratory disease. A key element of enhanced recovery from surgery is preoperative preparation, which cannot be included in an acute illness intervention. We suggest, however, that better attention to chronic disease management and dovetailing with conventional stable state and post-exacerbation pulmonary rehabilitation may have a positive impact on clinical outcomes.
Limitations of this study
We acknowledge some limitations to the interpretation of the current trial. We enrolled patients with exacerbations of a variety of chronic respiratory diseases because it is increasingly accepted that patients with disabling respiratory disease (including those with different underlying lung diseases such as interstitial lung disease) benefit from pulmonary rehabilitation regardless of the nature of the pulmonary pathophysiology.22 23 Most of the participants had chronic obstructive pulmonary disease, and recruitment from two acute hospitals serving both urban and rural populations suggests that the participants were representative of UK clinical practice. Outcomes in the chronic obstructive pulmonary disease subgroup in the current trial were indistinguishable from that seen in the whole cohort. We recognise our conclusions are restricted to patients with fewer than five admissions in the preceding 12 months. We chose to exclude this population because admissions of this frequency are often influenced by physical and psychological comorbidity or social circumstances or are indicative of the proximity of end of life30 and as a result would be less modifiable by an exercise intervention.
Comparison with current guidelines
The recognition of the negative effects of admission to hospital and the positive outcome of recent trials of post-discharge pulmonary rehabilitation20 21 has led to recommendations that pulmonary rehabilitation should be offered to all patients after discharge,22 although more recently it has been appreciated that many patients decline the offer of pulmonary rehabilitation immediately after discharge.31 The current trial was undertaken before post-discharge pulmonary rehabilitation was considered “usual care” and therefore conventional post-discharge pulmonary rehabilitation was not offered to participants, although they could be enrolled in conventional outpatient pulmonary rehabilitation after three months if indicated. Our study therefore substantially extends these previous reports by testing a modified rehabilitation intervention delivered in a larger and more representative population in a clinical trial that was adequately powered to detect a reduction in readmissions at 12 months.
Conclusions and policy implications
Admission to hospital for acute exacerbations of chronic respiratory disease is an important event in the clinical course of disability, which in turn can be ameliorated by pulmonary rehabilitation. However, the current trial suggests that the acute admission is not the time to enrol patients in a progressive, rehabilitation process, which may be beyond the capabilities of many participants in this situation and moreover might cause harm.
We have conducted the largest trial to date of an early, tailored rehabilitation intervention aimed at enhancing recovery and reducing readmissions to hospital in patients with acute exacerbations of chronic respiratory disease. The lack of impact on physical function and readmissions and the observation of an increased mortality at 12 months in the intervention group indicate caution before implementing such programmes during the immediate recovery from acute illness.
What is already known on this topic
Admissions to hospital for exacerbations of chronic respiratory disease are associated with high readmission rates
Post-exacerbation pulmonary rehabilitation is recommended in current guidelines but may miss the early decline seen in physical performance associated with hospital stay, and uptake of treatment is poor
We hypothesised that an early rehabilitation intervention at the time of admission and immediately afterwards would prevent this physical decline and reduce the rate of hospital admission
What this study adds
The acute admission is not the time to enrol patients in a rehabilitation programme as the risk of readmission was not reduced and recovery of physical function was not enhanced during 12 months’ follow-up
Mortality at 12 months was higher in the intervention group
Rehabilitation at this time had no additional benefit to the rate of hospital admission or physical performance over standard physiotherapy and might cause harm
We thank the pulmonary rehabilitation and clinical physiotherapy departments at both Glenfield Hospital and Kettering General Hospital, and Collaboration for Leadership in Applied Health Research and Care in Leicestershire, Northamptonshire and Rutland (CLAHR-LNR), particularly Pam de Chazal, theme manager for the CLAHRC-LNR rehabilitation theme.
Contributors: SJS and MCS are joint senior authors. NJG, JEAW, TH-D, SFH, MJB, MDM, SJS, and MS contributed to study design. NG was chief investigator. NG and SFH were the site specific principal investigators. NJG, JEAW, THD, SFH, EJC, EEV, RC, SJS, and MCS undertook the recruitment and performed the study. All authors contributed to data analysis and interpretation. NJG, JEAW, TH-D, MJB, EJC, MDM, SJS, MCS drafted the report and all authors reviewed and approved the final manuscript. NG acts as guarantor of the data.
Funding: This study was funded by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care in Leicestershire, Northamptonshire and Rutland (CLAHRC LNR), and took place at the University Hospitals of Leicester NHS Trust and Kettering General Hospital NHS Foundation Trust. Support was also provided by the NIHR Leicester Respiratory Biomedical Research Unit and CLAHRC East Midlands. This trial was supported by the University of Leicester Clinical Trials Unit. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study was approved by the National Research Ethics Service, Nottingham REC 1 committee (09/H0403/76).
Data sharing: The technical appendix, statistical code, and dataset are available from the corresponding author at njg27@le.ac.uk.
Transparency: The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Cite this as: BMJ 2014;349:g4315
Web Extra. Extra material supplied by the author
Supplementary information
References
- 1.Commission for Healthcare Audit and Inspection. Clearing the air: a national study of chronic obstructive pulmonary disease. 2006.
- 2.Pitta F, Troosters T, Probst VS, Spruit MA, Decramer M, Gosselink R. Physical activity and hospitalization for exacerbation of COPD. Chest 2006;129:536-44. [DOI] [PubMed] [Google Scholar]
- 3.Donaldson GC, Wilkinson TM, Hurst JR, Perera WR, Wedzicha JA. Exacerbations and time spent outdoors in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005;171:446-52. [DOI] [PubMed] [Google Scholar]
- 4.Spruit MA, Gosselink R, Troosters T, Kasran A, Gayan-Ramirez G, Bogaerts P, et al. Muscle force during an acute exacerbation in hospitalised patients with COPD and its relationship with CXCL8 and IGF-I. Thorax 2003;58:752-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Aymerich J, Farrero E, Felez MA, Izquierdo J, Marrades RM, Anto JM, et al. Risk factors of readmission to hospital for a COPD exacerbation: a prospective study. Thorax 2003;58:100-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 2007;297:1772-4. [DOI] [PubMed] [Google Scholar]
- 7.Troosters T, Probst VS, Crul T, Pitta F, Gayan-Ramirez G, Decramer M, et al. Resistance training prevents deterioration in quadriceps muscle function during acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010;181:1072-7. [DOI] [PubMed] [Google Scholar]
- 8.Giavedoni S, Deans A, McCaughey P, Drost E, MacNee W, Rabinovich RA. Neuromuscular electrical stimulation prevents muscle function deterioration in exacerbated COPD: a pilot study. Respir Med 2012;106:1429-34. [DOI] [PubMed] [Google Scholar]
- 9.Eaton T, Young P, Fergusson W, Moodie L, Zeng I, O’Kane F, et al. Does early pulmonary rehabilitation reduce acute health-care utilization in COPD patients admitted with an exacerbation? A randomized controlled study. Respirology 2009;14:230-8. [DOI] [PubMed] [Google Scholar]
- 10.Ettinger WH. Can hospitalization-associated disability be prevented? JAMA 2011;306:1800-1. [DOI] [PubMed] [Google Scholar]
- 11.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [DOI] [PubMed] [Google Scholar]
- 12.Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, Lobo DN. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 2010;29:434-40. [DOI] [PubMed] [Google Scholar]
- 13.British Thoracic Society’s current guidance: Recommendations of the BTS & ARTP. Guidelines for the measurement of respiratory function. Respir Med 1994;88:165-94. [PubMed] [Google Scholar]
- 14.Singh SJ, Morgan MD, Scott S, Walters D, Hardman AE. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 1992;47:1019-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Revill SM, Morgan MD, Singh SJ, Williams J, Hardman AE. The endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax 1999;54:213-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edwards RH, Hyde S. Methods of measuring muscle strength and fatigue. Physiotherapy 1977;63:51-5. [PubMed] [Google Scholar]
- 17.Jones PW, Quirk FH, Baveystock CM. The St George’s Respiratory Questionnaire. Respir Med 1991;85(Suppl B):25-31; discussion 33-7. [DOI] [PubMed] [Google Scholar]
- 18.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496-509. [Google Scholar]
- 19.Ko FW, Dai DL, Ngai J, Tung A, Ng S, Lai K, et al. Effect of early pulmonary rehabilitation on health care utilization and health status in patients hospitalized with acute exacerbations of COPD. Respirology 2011;16:617-24. [DOI] [PubMed] [Google Scholar]
- 20.Seymour JM, Moore L, Jolley CJ, et al. Outpatient pulmonary rehabilitation following acute exacerbations of COPD. Thorax 2010;65:423-8. [DOI] [PubMed] [Google Scholar]
- 21.Puhan MA, Gimeno-Santos E, Scharplatz M, Troosters T, Walters EH, Steurer J. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2011:CD005305. [DOI] [PubMed]
- 22.Bolton CE, Bevan-Smith EF, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013;68(Suppl 2:ii):1-30. [DOI] [PubMed] [Google Scholar]
- 23.Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188:e13-64. [DOI] [PubMed] [Google Scholar]
- 24.Apps LD, Mitchell KE, Harrison SL, Sewell L, Williams JE, Young HM, et al. The development and pilot testing of the self-management programme of activity, coping and education for chronic obstructive pulmonary disease (SPACE for COPD). Int J Chronic Obstruct Pulmon Dis 2013;8:317-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buckingham RJL, Lowe D, Pursey NA, Roberts CM, Stone RA. Report of the national chronic obstructive pulmonary disease audit 2008: resources and organisation of care in acute NHS units across the UK. www.rcplondonacuk/resources/chronic-obstructive-pulmonary-disease-audit.
- 26.Griffiths TL, Burr ML, Campbell IA, Lewis-Jenkins V, Mullins J, Shiels K, et al. Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial. Lancet 2000;355:362-8. [DOI] [PubMed] [Google Scholar]
- 27.Fan VS, Gaziano JM, Lew R, Bourbeau J, Adams SG, Leatherman S, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med 2012;156:673-83. [DOI] [PubMed] [Google Scholar]
- 28.Man WD, Polkey MI, Donaldson N, Gray BJ, Moxham J. Community pulmonary rehabilitation after hospitalisation for acute exacerbations of chronic obstructive pulmonary disease: randomised controlled study. BMJ 2004;329:1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh SJ, Steiner MC. Pulmonary rehabilitation; what’s in a name? Thorax 2013;68:899-901. [DOI] [PubMed] [Google Scholar]
- 30.Suissa S, Dell’Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax 2012;67:957-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jones SE, Green SA, Clark AL, Dickson MJ, Nolan AM, Moloney C, et al. Pulmonary rehabilitation following hospitalisation for acute exacerbation of COPD: referrals, uptake and adherence. Thorax 2014;69:181-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information