Abstract
Growing evidence has linked posttraumatic stress disorder (PTSD) to insulin resistance and type-2 diabetes, but most previous studies were cross-sectional. We examined the association between PTSD and incidence of diabetes in a prospective study of middle-aged male twins from the Vietnam Era Twin Registry. Lifetime PTSD was diagnosed at baseline with the Diagnostic Interview Schedule (DIS) according to DSM-III-R criteria. Subthreshold PTSD was defined by meeting some, but not all, criteria for PTSD. A total of 4,340 respondents without self-reported diabetes at baseline were included. Of these, 658 reported a new diagnosis of treated diabetes over a median of 19.4 years of follow-up. At baseline, twins with PTSD showed more behavioral and metabolic risk factors such as overweight and hypertension. The age-adjusted cumulative incidence of diabetes was significantly higher in twins with PTSD (18.9%) than those without PTSD (14.4%), [odds ratio (OR)=1.4, 95% confidence interval (CI) 1.03-1.8], and intermediate in those with subthreshold PTSD (16.4%) (OR=1.2, 95% CI 0.9-1.5, p for trend=0.03). Adjustment for military, lifestyle and metabolic factors diminished the association. No significant association was found comparing twin pairs discordant for PTSD. In conclusion, PTSD was prospectively associated with a 40% increased risk of new-onset type-2 diabetes which was partially explained by a cluster of metabolic and behavioral risk factors known to influence insulin resistance. Shared biological or behavioral precursors which occur within families may lead to both PTSD and insulin resistance/diabetes. Thus, PTSD could be a marker of neuroendocrine and metabolic dysregulation which may lead to type-2 diabetes.
Keywords: Posttraumatic Stress Disorder, Diabetes, Twin Studies, Epidemiology, Stress
Objectives of the Study and Background
Posttraumatic stress disorder (PTSD) is a psychiatric condition that is common among Veterans and results from exposure to severe psychological stress, such as exposure to combat. Among Vietnam Veterans who served in the war zone, the lifetime prevalence is 15% to 19% (Dohrenwend et al., 2006; Thompson, Gottesman, & Zalewski, 2006). Reported prevalence estimates of PTSD are even higher in combat-exposed Veterans from the recent Iraq and Afghanistan wars (Hoge et al., 2004; Hoge, Terhakopian, Castro, Messer, & Engel, 2007).
Although the comorbidity of PTSD and other psychiatric disorders is well characterized, its impact on physical health is less well understood. Many studies have documented a higher prevalence of physical health problems among persons with PTSD, but most used cross-sectional designs and self-reported symptoms (Dedert, Calhoun, Watkins, Sherwood, & Beckham, 2010; Glaesmer, Brahler, Gundel, & Riedel-Heller, 2011; Schnurr & Jankowski, 1999). Evidence of a possible link between PTSD and type 2 diabetes—a growing public health problem and a major risk factor for cardiovascular disease and all-cause mortality (Danaei et al., 2011) —has received increased attention (Boyko et al., 2010; Goodwin & Davidson, 2005; Norman et al., 2006). PTSD has also been associated with the metabolic syndrome, a cluster of risk factors characterized by insulin resistance and elevated risk of diabetes (Heppner et al., 2009; Jin et al., 2009; Weiss et al., 2011). The mechanisms underlying these associations are ascribed to chronic perturbations of the hypothalamic-pituitary-adrenal (HPA) axis in those with PTSD, potentially leading to increased visceral adiposity, inflammation, and insulin resistance (Brunner et al., 2002; Chrousos, 2000; Friedman & McEwen, 2004). PTSD may also influence diabetes risk through adverse health behaviors, such as sedentary lifestyle, poor dietary habits, sleep problems, and excessive alcohol consumption (Breslau, Davis, & Schultz, 2003). Finally, genetic and familial factors may play a role. Genetic predisposition is substantial for obesity and other metabolic syndrome risk factors (Diamond, 2003; Jowett et al., 2009), as well as health behaviors, such as physical inactivity and diet (Heitmann, Harris, Lissner, & Pedersen, 1999; Lauderdale et al., 1997). Therefore, shared genetic pathways could potentially confound the association between PTSD and diabetes, as previously described for depression and cardiovascular disease (Kendler, Gardner, Fiske, & Gatz, 2009; Vaccarino et al., 2009).
A major limitation of most previous studies linking PTSD to type-2 diabetes and other metabolic risk factors is their cross-sectional design, which limits the ability to demonstrate a temporal relationship between PTSD and diabetes. Using a prospective twin study design, this study examines the association between PTSD and the incidence of treated type-2 diabetes.
Materials and Methods
Setting
The Vietnam Era Twin (VET) Registry is the source of Vietnam-era Veterans for this study. The Registry was constructed from computerized military discharge records and is a national sample of male twin pairs from all branches who served on active duty during the Vietnam era (1964-1975). Members of the Registry were born from 1939 through 1957. The process of identifying twin pairs involved a matching algorithm based on last name, date of birth, and similar Social Security numbers. A military record search confirmed an individual was a member of a twin pair by matching parental names and place of birth. The Registry was assembled in the 1980s and has subsequently seen extensive use as a platform for genetic epidemiological studies of both physical and mental health. A complete description of the VET Registry has been published previously (Goldberg, Curran, Vitek, Henderson, & Boyko, 2002).
Design
A Twin Study of the Course and Consequences of PTSD in Vietnam Era Veterans [Veterans Administration (VA) Cooperative Studies Program (CSP) #569) is a prospective, observational study of physical and mental health among Veterans who are members of the VET Registry. The study used data collected at the Registry’s inception that included socio-demographic data and military experience, as well as physical and mental health information collected in 1992 that included self-reported diabetes and PTSD. These measures constituted baseline data for the present study, and were combined with newly collected follow-up data from 2010 through 2012. In this analysis, we examined the association between PTSD assessed in 1992 and incident treated type-2 diabetes through 2012 among Veterans who were free of diabetes at the time PTSD was assessed.
Subjects
All members of the Registry who were known to be alive and had not withdrawn their Registry membership were recruited to participate in CSP #569. For these analyses, we restricted participants to those for whom PTSD was assessed in 1992 and who did not self-report diabetes at that time. Informed consent was obtained from all participating Registry members, and the VA Central Institutional Review Board approved the study protocol.
Measures
Socio-demographic and Military Service Factors
Information on socio-demographic and military service factors were available from the military service records of members of the VET Registry. These data were abstracted at the time the VET Registry was established in the 1980s and included date of birth, race, marital status at enlistment, educational attainment at the time of enlistment, date of enlistment, branch of service, and rank at enlistment.
Extensive additional information was obtained through a series of Registry-wide surveys that were conducted from 1987 through 1992. Education and marital status were updated, and information on occupational status and family income was obtained. Combat exposure was measured by asking each Veteran whether he engaged in 18 specific combat activities such as receiving incoming fire, serving as a “tunnel rat,” or checking enemy base camps, yielding a global index of combat exposure ranging from 0 to 18 (Janes, Goldberg, Eisen, & True, 1991).
Baseline Risk Factors and Medical Conditions
Registry-wide surveys conducted from 1987 through 1992 also provided extensive information about previous medical history and risk factors, including smoking history, alcohol consumption, anthropometric measurements, and dietary habits. Physical activity was determined by a series of questions about moderate everyday activities (6 questions) or intense sports-related physical activity (5 questions) (Lauderdale et al., 1997). Physical activity was classified as a 3-level ordinal variable of “no physical activity,” “moderate physical activity” (engaged in at least one moderate every day activity, such as taking the stairs, walking for exercise, etc.), and “vigorous physical activity” (engaged regularly in at least one vigorous or sports-related activity for at least the last 3 months, such as biking, running, swimming, etc.). Alcohol consumption was addressed with a series of questions asking the respondent on how many days, during the past 2 weeks, he drank beer, wine or hard liquor, and on the days he drank, how many drinks he had per day. From these questions, an average of drinks per day was calculated. Diabetes at baseline was assessed with the question: “Do you have diabetes?” which was asked in a 1992 survey. Veterans answering either affirmatively to or not answering this question were excluded from the analysis. In the same survey, previous history of cardiovascular diseases was assessed by a series of questions asking whether the respondent was ever told by a doctor that he had angina pectoris, congestive heart failure, coronary heart disease, damaged heart valves, heart attack or myocardial infarction, heart murmur, phlebitis or thrombophlebitis, or stroke, or whether the respondent ever had balloon angioplasty or coronary artery bypass surgery.
Psychiatric Diagnoses
In 1992, twins who participated in a Registry-wide study were administered the Diagnostic Interview Schedule (DIS) for the assessment of psychiatric disorders according to DSM-III-R criteria. Surveys were conducted using trained interviewers and a computer-assisted telephone version of the DIS (Eisen et al., 2004). Both lifetime and 12-month prevalence of PTSD, major depression, generalized anxiety disorder, and substance abuse disorder were assessed. In total, 8,169 Veterans were interviewed (3,516 twin pairs and 1,137 singletons), representing 79.7% of eligible twins who were still alive (Eisen et al., 2004). In addition to PTSD (meeting full diagnostic criteria), we examined subthreshold PTSD, defined as meeting both the A (exposure to traumatic stress) and B (re-experiencing symptoms) criteria and either the C (avoidance and numbing) or D (increased arousal) criteria. Lifetime PTSD diagnosis as of 1992 was the main exposure in our analysis.
Assessment of New-Onset Type-2 Diabetes
Between January 2010 and September 2012, Registry members were asked by questionnaire if they ever had a history of physician-diagnosed diabetes. A series of additional questions collected information on age at diagnosis and type of anti-diabetic treatment using a comprehensive list of generic and trade names for insulin and oral agents. If the Veteran responded positively to the medication treatment question and chose one or more anti-diabetic agents from a list provided, he was considered as having pharmaceutically-treated diabetes, which was the outcome used in this analysis. Given the age of the cohort, we assumed that all new diabetes cases were type-2. We validated this definition of diabetes against clinically-confirmed diabetes by comparison of all self-reported diabetes cases and a random sample of non-cases with health care provider checklists, and found an agreement of 97.5%.
Statistical Analysis
We examined baseline differences in socio-demographic, military service, and lifestyle factors according to PTSD status at baseline in 1992, the primary exposure, and according to whether participants developed diabetes through 2012, the primary outcome. We also compared baseline characteristics according to whether an individual completed the 2010-2012 mailed questionnaire in order to assess possible response bias. Formal testing for differences in response used Student’s t and chi-squared tests.
Based on PTSD status in 1992 (no PTSD, subthreshold PTSD, and PTSD) we calculated the risk of incident diabetes through 2012. We used multivariate logistic regression to adjust for potential confounding factors that could influence the association between PTSD and type-2 diabetes. Odds ratios (ORs) and 95% confidence intervals (CI) were estimated for participants with PTSD and for those with subthreshold PTSD compared to those without PTSD. ORs can be interpreted as an estimate of relative-risks for uncommon outcomes, generally those occurring in less than 20% of the cohort (Zhang & Yu, 1998). For the within-pair twin analysis we used logistic regression to estimate the ORs for the association between PTSD and diabetes within twin pairs discordant for PTSD. We also performed a sensitivity analysis where all self-reported diabetes was considered, not just treated diabetes. In all analyses, significance levels were two-sided and set at p = 0.05. All analyses accounted for the clustered data structure represented by twin pairs using robust variance estimators. Data analyses were performed with Stata software version 13.1.
All incidence estimates, means, and ORs were weighted to account for potential non-response bias affecting the original distribution of socio-demographic and military service factors in the VET Registry. Responses were weighted using a model-based reweighting approach (Rosenbaum, 1987). Briefly, this method fits a multivariable logistic regression model where the dependent variable (yi) is defined as a binary outcome for responder and the reference population (1 if responder, 0 if reference) and the socio-demographic, military service variables, and lifestyle factors are the independent variables (xi). Results from the fitted model are then used to generate inverse probability weights for response. This approach produces weighted estimates of parameters of interest, such as odds ratios, that account for all measured non-response differences from the living population of the VET Registry.
Results
Study Sample
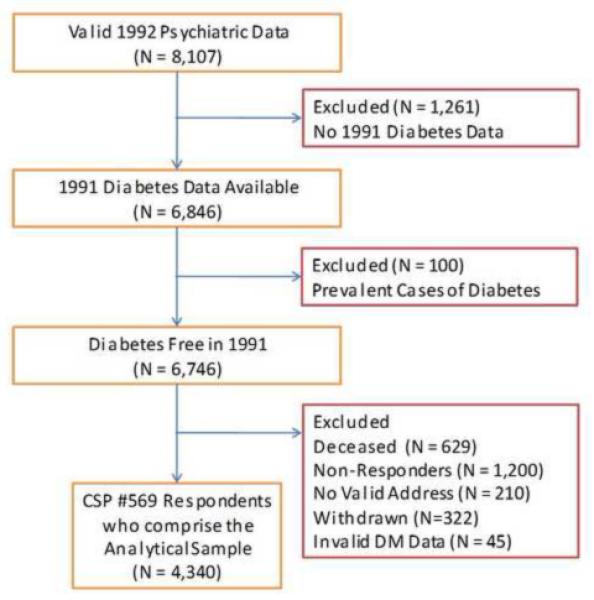
Of 8,169 Veterans interviewed in the 1992 survey, 8,107 had valid psychiatric data. From these we excluded 1,261 Veterans for whom no diabetes data were available, and 100 who reported a history of diabetes in or before 1992, leaving 6,746 diabetes-free Veterans who were eligible for outcome assessment. From this pool, 629 (9%) Veterans were found to be deceased, 1,004 (15%) refused to participate in the follow-up survey, 196 (3%) never responded, 210 (3%) could not be located, 322 (5%) had withdrawn their membership from the registry, and 45 (1%) failed to answer the diabetes questions, leaving 4,340 Veterans (64%) for this analysis. Figure 1 shows the construction of the sample for the current analysis.
Figure 1.
Eligibility for Prospective Cohort Study of the Association of PTSD and Incident Diabetes
Responders and non-responders were similar in most characteristics, except that non-responders tended more often to be non-white, not married, less educated and current smokers (Supplemental e-Table1). There were no differences in PTSD assessed in 1992 or other psychiatric diagnoses according to respondent status, nor were there differences in military service variables, including service in Southeast Asia, and cardiovascular risk factors, such as hypertension and BMI.
PTSD and Baseline Factors
In 1992, the prevalence of lifetime PTSD was higher among younger, unmarried, and less educated Veterans (Table 1). Those with PTSD were also more likely to be unemployed, to have served in the Army, and to have enlisted earlier. Veterans with PTSD tended to be less physically active, consume more alcohol, and smoke more. Overall they tended to have a higher rate of metabolic risk factors such as overweight and hypertension. In general, a gradation of association was noted for these risk factors, such that Veterans without PTSD had the lowest levels of risk factors, subthreshold PTSD intermediate levels, and full PTSD the highest levels. As expected, those with PTSD were more likely to have comorbid psychiatric diagnoses, such as major depression, generalized anxiety disorder, and substance abuse disorder.
Table 1.
Demographic, Military Service, Lifestyle, Clinical and Psychiatric Factors by PTSD Status.
| 1992 PTSD Diagnosis |
|||
|---|---|---|---|
| Factors at Baseline (1992) | No PTSD N=3,424 |
Subthreshold PTSD N=541 |
PTSD N=375 |
| Demographic Factors | |||
| Age | |||
| ≤39 | 18.6 | 20.4 | 21.8 |
| 40-41 | 19.0 | 19.2 | 22.9 |
| 42-43 | 33.5 | 33.9 | 35.4 |
| ≥44 | 28.9 | 26.5 | 19.9 |
| White Race | 91.0 | 90.7 | 90.1 |
| Hispanic Ethnicity | 2.6 | 2.5 | 4.1 |
| Married/Partnered/Widowed | 81.1 | 77.3 | 75.5 |
| Education | |||
| Less than H.S. Graduate | 2.6 | 5.0 | 4.9 |
| High School Graduate | 30.8 | 30.9 | 29.5 |
| Some College/Vocational | 40.3 | 42.6 | 46.0 |
| College Graduate or more | 26.4 | 21.5 | 19.6 |
| Employment Status | |||
| Full Time | 94.9 | 94.2 | 89.8 |
| Part Time | 1.1 | 1.7 | 3.4 |
| Unemployed | 4.0 | 4.1 | 6.8 |
| Military Service Factors | |||
| Branch of Service | |||
| Army | 49.0 | 52.3 | 55.3 |
| Navy | 26.0 | 20.6 | 19.8 |
| Air Force | 19.5 | 17.6 | 12.8 |
| Marines | 5.5 | 9.5 | 12.1 |
| Enlistment year | |||
| ≤1967 | 33.5 | 37.0 | 35.2 |
| 1968-69 | 33.1 | 33.9 | 33.1 |
| ≥1970 | 33.3 | 29.1 | 31.7 |
| Officer Military Rank at Enlistment | 3.6 | 1.7 | 1.4 |
| Service in Southeast Asia | 34.8 | 49.8 | 61.3 |
| Lifestyle and Cardiovascular Risk Factors | |||
| Cigarette Smoking | |||
| Current | 30.0 | 37.2 | 45.8 |
| Former | 33.3 | 37.6 | 31.5 |
| Never | 36.7 | 25.2 | 22.7 |
| Alcohol Consumption | |||
| Never Drinker | 6.7 | 5.7 | 5.3 |
| Former Drinker | 31.3 | 33.2 | 36.9 |
| <2 per day | 47.4 | 41.4 | 39.7 |
| ≥ 2 per day | 14.6 | 19.7 | 18.0 |
| Physical Activity | |||
| No Physical Activity | 11.0 | 10.0 | 7.9 |
| Moderate Physical Activity | 63.5 | 63.0 | 65.8 |
| Vigorous Physical Activity | 25.5 | 27.0 | 26.3 |
| BMI | |||
| < 25 | 40.6 | 43.4 | 35,4 |
| 25 – 30 | 48.1 | 44.9 | 53.3 |
| > 30 | 11.3 | 11.7 | 11.3 |
| Hypertension | 17.1 | 19.3 | 23.4 |
| Cardiovascular Disease | 11.3 | 10.9 | 17.4 |
| Psychiatric Conditions | |||
| Major Depressive Disorder | 5.5 | 13.3 | 32.7 |
| Generalized Anxiety Disorder | 0.9 | 3.1 | 10.6 |
| Alcohol Use Disorder | 48.6 | 62.8 | 72.2 |
| Substance Use Disorder | 6.3 | 12.5 | 27.1 |
All data weighed for non-response.
PTSD and Incidence of Type-2 Diabetes
A total of 658 new diabetes diagnoses were reported over a median of 19.4 years of follow-up. The cumulative incidence of diabetes was higher in non-white, Hispanic, and less educated Veterans (supplemental e-Table 2). As expected, those with higher BMI and hypertension at baseline were more likely to develop diabetes; however, there was no relationship between alcohol consumption, major depression, generalized anxiety disorder, and alcohol or drug abuse disorder in 1992 and diabetes onset through 2012.
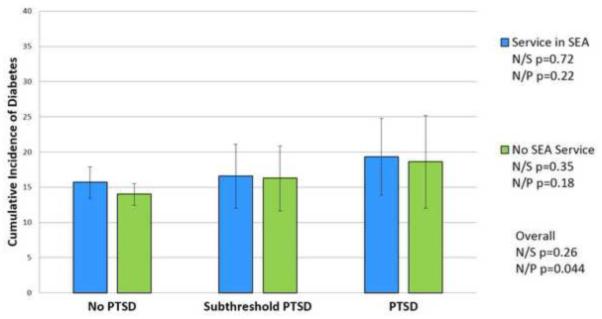
The age-adjusted cumulative incidence of type-2 diabetes was significantly higher in Veterans with PTSD at baseline (18.9%) than in those without PTSD (14.4%, p=0.044), and somewhat intermediate in those with subthreshold PTSD (16.4%) (p for trend=0.027). The results were similar in Veterans who served in Southeast Asia and in those who did not (Figure 2). The age-adjusted OR for new-onset diabetes was 1.2 (95% CI: 0.9-1.5) for subthreshold PTSD and 1.4 (95% CI: 1.0-1.9) for PTSD meeting full diagnostic criteria (Table 2, model 1). Adjustment for military service factors and by demographic characteristics diminished these associations (model 2). Further adjustment for BMI and other cardiovascular and behavioral factors assessed at or before 1992, brought the OR estimate close to the null (model 3), while the addition of other psychiatric conditions to the model had no impact (model 4).
Figure 2.
Association of PTSD with Age-Adjusted Incident Diabetes According to Vietnam Theater Service.
Footnotes to Figure 2:
N/S: No PTSD vs. Subthreshold PTSD
N/P: No PTSD vs. PTSD
No PTSD is defined as having no lifetime history of PTSD at the 1992 interview.
PTSD is defined as having a lifetime history of PTSD at the 1992 interview.
Subthreshold PTSD is defined as meeting both the A and B criteria and either the C or D criteria for PTSD according to the DSM-IIIR.
All estimates are weighted for non-response.
Table 2.
Association of PTSD with Incident Diabetes Among VET Registry Members, Unadjusted and Adjusted for Demographic, Military Service, Lifestyle, Clinical, and Psychiatric Factors
| Incident Diabetes |
|||||||
|---|---|---|---|---|---|---|---|
| Models | No PTSD n=3,424 |
Subthreshold PTSD n=541 |
PTSD n=375 |
P for Trend |
|||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | ||
|
Model 1:
Adjusted for Age |
1. 0 | (ref) | 1. 2 | (0.9 – 1.5) | 1. 4 | (1.03 – 1.8) | 0.027 |
|
Model 2:
Adjusted for Demographic and Military Service Factors * |
1. 0 | (ref) | 1. 1 | (0.8 – 1.4) | 1. 2 | (0.9 – 1.7) | 0.16 |
|
Model 3:
Adjusted for All Above Plus Lifestyle and Cardiovascular Risk Factors† |
1. 0 | (ref) | 1. 1 | (0.8 – 1.5) | 1. 1 | (0.8 – 1.5) | 0.41 |
|
Model 4:
Adjusted for All Above Plus Psychiatric Conditions‡ |
1. 0 | (ref) | 1.2 | (0.9 – 1.5) | 1.2 | (0.9 – 1.7) | 0.16 |
All data weighed for non-response.
No PTSD is defined as having no lifetime history of PTSD at the 1992 interview.
PTSD is defined as having a lifetime history of PTSD at the 1992 interview.
Subthreshold PTSD is defined as meeting both the A and B criteria and either the C or D criteria for PTSD according to the DSM-IIIR.
The model adjusted demographic and military service factors including age, race, ethnicity, marital status, education, branch of service, enlistment year, service in Southeast Asia, and military rank at enlistment.
In addition to the factors above, the model adjusted for baseline (1992) lifestyle and clinical factors including cigarette smoking, alcohol use, physical activity, BMI, hypertension, hypercholesterolemia, and history of cardiovascular disease.
In addition to the factors above, the model adjusted for baseline (1992) psychiatric factors including depression, generalized anxiety disorder, and alcohol or drug abuse disorder.
Table 3 shows the results of the twin-based within-pair analyses comparing brothers discordant for PTSD (370 pairs). In this analysis, no significant association was found between PTSD and diabetes onset.
Table 3.
Association of PTSD with Incident Diabetes Among VET Registry Twin Pairs Discordant for PTSD. Unadjusted and Adjusted for Selected Demographic, Military Service and Lifestyle Factors.
| Incident Diabetes |
|||||||
|---|---|---|---|---|---|---|---|
| Models | No PTSD n=3,424 |
Subthreshold PTSD n=541 |
PTSD n=375 |
P for Trend |
|||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | ||
|
Model 1:
Adjusted for Age |
1. 0 | (ref) | 1. 2 | (0.8 – 1.7) | 1. 0 | (0.6 – 1.7) | 0.68 |
|
Model 2:
Adjusted for Demographic and Military Service Factors * |
1. 0 | (ref) | 1. 2 | (0.8 – 1.8) | 1. 0 | (0.6 – 1.7) | 0.83 |
|
Model 3:
Adjusted for Selected Demographic, Military Service and Lifestyle Factors † |
1. 0 | (ref) | 1. 2 | (0.8 – 1.8) | 1. 0 | (0.6 – 1.8) | 0.75 |
All data weighed for non-response.
No PTSD is defined as having no lifetime history of PTSD at the 1992 interview.
PTSD is defined as having a lifetime history of PTSD at the 1992 interview.
Subthreshold PTSD is defined as meeting both the A and B criteria and either the C or D criteria for PTSD according to the DSM-IIIR.
Model 1 includes 370 twin pairs; Model 2 includes 352 twin pairs; and Model 3 includes334 twin pairs.
The model adjusted for demographic and military service factors including age, race, ethnicity, marital status, education, branch of service, enlistment year, service in Southeast Asia, and military rank at enlistment.
The model adjusted for selected demographic, military service and lifestyle factors including age, race, ethnicity, education, military rank at enlistment, service in Southeast Asia, physical activity, and BMI.
When all self-reported diabetes was considered as the outcome, results remained similar, although they were slightly more significant. In the within-pair analysis, the unadjusted OR for subthreshold PTSD was 1.3 (95% CI: 0.9-1.8), and for PTSD it was 1.4 (95% CI: 0.9-2.1, p=0.08 for trend). The estimates were unchanged after adjusting for other factors although the confidence intervals became somewhat wider.
Discussion
In this prospective study of Vietnam-era Veterans, PTSD was associated with a 40% increased risk of new-onset type-2 diabetes which was largely explained by a cluster of metabolic and behavioral risk factors known to influence insulin resistance. It is possible that PTSD leads to hormonal and metabolic abnormalities that influences insulin resistance and, in turn, increase the risk of diabetes. Based on the analysis of PTSD-discordant twin pairs, familial factors shared by the twins play a role in these associations, and suggest that there are common biological or behavioral factors for both PTSD and insulin resistance/diabetes.
This is the first prospective, long-term study to examine the association between a diagnosis of PTSD and incidence of treated diabetes mellitus. Although recent studies have reported an association between PTSD and diabetes (Boyko et al., 2010; Goodwin et al., 2005; Lukaschek et al., 2013; Norman et al., 2006), all except one (Boyko et al., 2010) were cross-sectional, and therefore limited in their ability to establish whether or not PTSD preceded the onset of diabetes. The only prospective study which found an association between PTSD and a self-report of physician-diagnosed diabetes (Boyko et al., 2010) is based on data from the Millennium Cohort Study that included 44,754 Veterans where PTSD was assessed by means of the PTSD Checklist, civilian scale. This is a young cohort (mean age approximately 36 years old) followed for 3 years, among whom the rate of new-onset diabetes was very low (<0.01%) but baseline PTSD was associated with a 2-fold increase in risk of new diabetes. Thus, differences in the two study populations likely account for the divergent findings. In addition, self-reported diabetes included any reported diabetes, while we focused on diabetes treated pharmacologically.
Several studies have linked psychological stress and depression to visceral fat, insulin resistance, and other components of the metabolic syndrome (Brunner et al., 2002; Capuron et al., 2008; Chrousos, 2000; Vaccarino et al., 2008). Enduring dysregulation of the HPA axis has been implicated, such that stressful experiences activate the HPA axis leading to excessive cortisol production, central adiposity, insulin resistance, and associated metabolic abnormalities (Friedman et al., 2004). Indeed, HPA axis dysregulation with excess cortisol production has been reported in persons with glucose intolerance or diabetes (Andrews, Herlihy, Livingstone, Andrew, & Walker, 2002; Liu, Bravata, Cabaccan, Raff, & Ryzen, 2005). However, the neurobiology of PTSD is complex, particularly as it relates to stress response and metabolic risk, since lower, rather than higher, cortisol levels in plasma and urine have been associated with PTSD during basic conditions, likely due to enhanced negative feedback sensitivity of the glucocorticoid receptors (Bremner, Southwick, & Charney, 1999; Yehuda, 2002).
Our results are consistent with an important role of metabolic and lifestyle factors in the association between PTSD and type-2 diabetes. Veterans with PTSD had a higher prevalence of cardiometabolic risk factors at baseline, such as sedentary behavior, smoking, alcohol consumption, hypertension and overweight. When these factors were accounted for, the association between PTSD and incident diabetes was weakened. Although the direct role of these risk factors in the PTSD-diabetes association, or in affecting insulin resistance, cannot be discerned from our analysis, it is plausible that they are the consequences of PTSD (mediators) rather than PTSD being a consequence of these risk factors (potential confounders).
Within twin pairs, no association was found even in unadjusted analysis, suggesting that familial influences shared by the twins are important in this association. There could be shared environmental factors or health behaviors that influence diabetes risk, such as socioeconomic and lifestyle factors, many of which are acquired in childhood and are known to strongly predict adult behaviors (Case, Fertig, & Paxson, 2005; Lauderdale et al., 1997; Ortega, Ruiz, Castillo, & Sjostrom, 2008). It is also possible that common biological precursors lead to both PTSD and insulin resistance/diabetes. Thus, PTSD could be a marker of neuroendocrine and metabolic dysregulation which may lead to increased risk of diabetes. Future studies should focus on the elucidation of cardiometabolic pathways that are associated with PTSD and also increase the risk of insulin resistance and diabetes. As many of these factors may be modifiable, this research has important clinical and public health implications that are especially relevant to the physical and mental health of our Veteran population.
This study has a number of limitations. The gold standard for the presence of diabetes is 2 measures of fasting measure of glucose that exceed 125 mg/dL; this assessment was not feasible. Instead we relied on self-report and a medication inventory to classify diabetes. We did a validation in a subsample and found an agreement of 97.5% between the definition of diabetes used in this analysis and clinically confirmed diabetes reported by health care providers. Although we have a good measure of clinically diagnosed diabetes, it likely underestimates the total burden of diabetes, since undiagnosed cases would not have been treated and therefore included. If PTSD status is associated with the likelihood of having diabetes diagnosed or treated among all those with diabetes, we may have failed to fully characterize the PTSD-diabetes association. However, when analyses were repeated with all self-reported diabetes as the outcome, conclusions did not change. Another limitation is that about 36% of eligible individuals at baseline were not included in this prospective analysis, primarily due to non-response. If the association between PTSD and diabetes were different in non-responders and responders, our findings would be biased. However, responders and non-responders were quite similar in their distribution of baseline risk factors and PTSD status, suggesting that bias due to non-response is unlikely in our results. Furthermore, we began our observation period in 1992, when PTSD status was assessed through the DIS, and excluded participants who reported diabetes prior to 1992. If diabetes in relationship with PTSD occurred earlier than 1992, we would have missed the association. Moreover, we were not able to provide insight into the temporal relationship at baseline between PTSD and cardiovascular and metabolic comorbidities associated with diabetes.
Another limitation is our lack of measures of insulin resistance, a major precursor and biological mechanism leading to diabetes. A direct measurement of either insulin action or insulin secretion would have been helpful in clarifying whether PTSD, directly or through other factors, affects the risk of diabetes by influencing insulin resistance. Additionally, we were unable to differentiate PTSD due to combat or to other types of trauma. Finally, our sample was all male and predominantly non-Hispanic whites; therefore, our findings are not generalizable to other demographic groups. Strengths of our study include the prospective design, the large sample size, and the availability of a clinical diagnosis of PTSD. In addition, the co-twin study design controls for potentially unmeasured confounding factors such as familial, genetic, and early environmental characteristics that may affect both the risk of PTSD and the risk of diabetes.
In conclusion, in a prospective study of Vietnam-era male Veterans, we found that PTSD was associated with a 40% increase in the risk of type-2 diabetes and with a cluster of metabolic and behavioral baseline risk factors that largely explained the association. Shared precursors to both PTSD and insulin resistance/diabetes may play a role in the link between PTSD and type-2 diabetes. Thus, PTSD could be a marker of hormonal and metabolic dysregulation which may lead to insulin resistance and increased risk of diabetes.
Supplementary Material
Highlights.
We examine whether PTSD is associated with incidence of type-2 diabetes.
We use a longitudinal twin study design.
PTSD is prospectively associated with a 40% increased risk of type-2 diabetes.
Twins discordant for PTSD do not differ in their risk of diabetes.
Common mechanisms may lead to both PTSD and insulin resistance/diabetes.
Acknowledgements
The authors gratefully acknowledge the continued cooperation and participation of the members of the VET Registry: without their contribution this research would not have been possible. We also owe great thanks to the members of the Department of Veterans Affairs Cooperative Study #569 Group (in addition to the authors): I. Curtis, A. Ali, B. Majerczyk, B. Harp, K. Moore, A. Fox, M. Tsai, A. Mori, J.Sporleder, P. Terry, Seattle, WA; D. Yeager, Charleston, SC. Executive Committee: S. Eisen, Washington, DC; A. Snodgrass, Albuquerque, NM. Data Monitoring Committee: J. Vasterling, Boston, MA; M. Stein, La Jolla, CA; B. Booth, Little Rock, AR; J. Westermeyer, Minneapolis,MN. Planning Committee: M. McFall, Seattle, WA; T. O’Leary, S. Eisen, Washington, DC; M. Smith, Palo Alto, CA; K. Swanson, Albuquerque, NM. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States Government.
Role of Funding Source
The Cooperative Studies Program (CSP) of the Office of Research and Development, Clinical Science Research and Development, of the United States Department of Veterans Affairs (VA), has provided financial support for Cooperative Study #569 and the development and maintenance of the Vietnam Era Twin (VET) Registry. Dr. Viola Vaccarino was supported in part by a National Institutes of Health award K24 HL077506.
Footnotes
Viola Vaccarino, MD, PhD, contributed to the study design, result interpretation and drafted the manuscript.
Jack Goldberg, PhD, contributed to the study design, result interpretation and manuscript revisions.
Kathryn M. Magruder, PhD, contributed to the study design, result interpretation and manuscript revisions.
Christopher W. Forsberg, MS, performed statistical analyses and helped with data interpretation and manuscript revisions.
Matthew J. Friedman, MD, PhD, contributed to the study design, result interpretation and manuscript revisions.
Brett T. Litz, PhD, contributed to the study design, result interpretation and manuscript revisions. Patrick J. Heagerty, PhD, supervised the statistical analyses and helped with data interpretation and manuscript revisions.
Grant D. Huang, MPH, PhD, contributed to result interpretation and manuscript revisions. Theresa C. Gleason, PhD, contributed to result interpretation and manuscript revisions. Nicholas L. Smith, PhD, contributed to the study design, result interpretation and manuscript revisions.
Conflicts of Interest
None of the authors report conflict of interest relevant to this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andrews RC, Herlihy O, Livingstone DE, Andrew R, Walker BR. Abnormal cortisol metabolism and tissue sensitivity to cortisol in patients with glucose intolerance. Journal of Clinical Endocrinology and Metabolism. 2002;87:5587–5593. doi: 10.1210/jc.2002-020048. [DOI] [PubMed] [Google Scholar]
- Boyko EJ, Jacobson IG, Smith B, Ryan MAK, Hooper TI, Amoroso PJ, Gackstetter GD, Barrett-Connor E, Smith TC. Risk of diabetes in US military service members in relation to combat deployment and mental health. Diabetes Care. 2010;33:1771. doi: 10.2337/dc10-0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Charney DS. The neurobiology of posttraumatic stress disorder: An integration of animal and human research. In: Saigh PA, Bremner JD, editors. Posttraumatic Stress Disorder: A Comprehensive Text. Allyn & Bacon; New York: 1999. pp. 103–143. [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Brunner EJ, Hemingway H, Walker BR, Page M, Clarke P, Juneja M, Shipley MJ, Kumari M, Andrew R, Seckl JR, Papadopoulos A, Checkley S, Rumley A, Lowe GDO, Stansfeld SA, Marmot MG. Adrenocortical, autonomic, and inflammatory causes of the metabolic syndrome: Nested case-control study. Circulation. 2002;106:2659–2665. doi: 10.1161/01.cir.0000038364.26310.bd. [DOI] [PubMed] [Google Scholar]
- Capuron L, Su S, Miller AH, Bremner JD, Goldberg J, Vogt GJ, Maisano C, Jones L, Murrah NV, Vaccarino V. Depressive symptoms and metabolic syndrome: is inflammation the underlying link? Biol Psychiatry. 2008;64:896–900. doi: 10.1016/j.biopsych.2008.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. Journal of Health Economics. 2005;24:365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Chrousos GP. The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: neuro-endocrine and target tissue-related causes. International Journal of Obesity and Related Metabolic Disorders. 2000;24:S50–55. doi: 10.1038/sj.ijo.0801278. [DOI] [PubMed] [Google Scholar]
- Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Annals of Behavioral Medicine. 2010;39:61–78. doi: 10.1007/s12160-010-9165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond J. The double puzzle of diabetes. Nature. 2003;423:599–602. doi: 10.1038/423599a. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313:979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen SA, Griffith KH, Xian H, Scherrer JF, Fischer ID, Chantarujikapong S, Hunter J, True WR, Lyons MJ, Tsuang MT. Lifetime and 12-month prevalence of psychiatric disorders in 8,169 male Vietnam War era veterans. Mil Med. 2004;169:896–902. doi: 10.7205/milmed.169.11.896. [DOI] [PubMed] [Google Scholar]
- Friedman MJ, McEwen BS. PTSD, Allostatic Load, and Medical Illness. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. American Psychological Association; Washington, DC: 2004. pp. 157–188. [Google Scholar]
- Glaesmer H, Brahler E, Gundel H, Riedel-Heller SG. The association of traumatic experiences and posttraumatic stress disorder with physical morbidity in old age: a German population-based study. Psychosom Med. 2011;73:401–406. doi: 10.1097/PSY.0b013e31821b47e8. [DOI] [PubMed] [Google Scholar]
- Goldberg J, Curran B, Vitek ME, Henderson WG, Boyko EJ. The Vietnam Era Twin Registry. Twin Research. 2002;5:476–481. doi: 10.1375/136905202320906318. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Davidson JR. Self-reported diabetes and posttraumatic stress disorder among adults in the community. Preventive Medicine. 2005;40:570–574. doi: 10.1016/j.ypmed.2004.07.013. [DOI] [PubMed] [Google Scholar]
- Heitmann BL, Harris JR, Lissner L, Pedersen NL. Genetic effects on weight change and food intake in Swedish adult twins. American Journal of Clinical Nutrition. 1999;69:597–602. doi: 10.1093/ajcn/69.4.597. [DOI] [PubMed] [Google Scholar]
- Heppner P, Crawford E, Haji U, Afari N, Hauger R, Dashevsky B, Horn P, Nunnink S, Baker D. The association of posttraumatic stress disorder and metabolic syndrome: a study of increased health risk in veterans. BMC medicine. 2009;7:1. doi: 10.1186/1741-7015-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. American Journal of Psychiatry. 2007;164:150–153. doi: 10.1176/ajp.2007.164.1.150. [DOI] [PubMed] [Google Scholar]
- Janes GR, Goldberg J, Eisen SA, True WR. Reliability and validity of a combat exposure index for Vietnam era veterans. Journal of Clinical Psychology. 1991;47:80–86. doi: 10.1002/1097-4679(199101)47:1<80::aid-jclp2270470112>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Jin H, Lanouette NM, Mudaliar S, Henry R, Folsom DP, Khandrika S, Glorioso DK, Jeste DV. Association of posttraumatic stress disorder with increased prevalence of metabolic syndrome. Journal of Clinical Psychopharmacology. 2009;29:210. doi: 10.1097/JCP.0b013e3181a45ed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jowett JB, Diego VP, Kotea N, Kowlessur S, Chitson P, Dyer TD, Zimmet P, Blangero J. Genetic influences on type 2 diabetes and metabolic syndrome related quantitative traits in Mauritius. Twin Res Hum Genet. 2009;12:44–52. doi: 10.1375/twin.12.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Fiske A, Gatz M. Major depression and coronary artery disease in the Swedish Twin Registry: phenotypic, genetic, and environmental sources of comorbidity. Archives of General Psychiatry. 2009;66:857–863. doi: 10.1001/archgenpsychiatry.2009.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Fabsitz R, Meyer JM, Sholinsky P, V Ramakrishnan, Goldberg J. Familial determinants of moderate and intense physical activity: a twin study. Medicine and Science in Sports and Exercise. 1997;29:1062. doi: 10.1097/00005768-199708000-00012. [DOI] [PubMed] [Google Scholar]
- Liu H, Bravata DM, Cabaccan J, Raff H, Ryzen E. Elevated late-night salivary cortisol levels in elderly male type 2 diabetic veterans. Clinical Endocrinology. 2005;63:642–649. doi: 10.1111/j.1365-2265.2005.02395.x. [DOI] [PubMed] [Google Scholar]
- Lukaschek K, Baumert J, Kruse J, Emeny RT, Lacruz ME, Huth C, Thorand B, Holle R, Rathmann W, Meisinger C, Ladwig KH, Investigators K. Relationship between posttraumatic stress disorder and type 2 diabetes in a population-based cross-sectional study with 2970 participants. Journal of Psychosomatic Research. 2013;74:340–345. doi: 10.1016/j.jpsychores.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Norman SB, Means-Christensen AJ, Craske MG, Sherbourne CD, Roy-Byrne PP, Stein MB. Associations between psychological trauma and physical illness in primary care. Journal of Traumatic Stress. 2006;19:461–470. doi: 10.1002/jts.20129. [DOI] [PubMed] [Google Scholar]
- Ortega FB, Ruiz JR, Castillo MJ, Sjostrom M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes (Lond) 2008;32:1–11. doi: 10.1038/sj.ijo.0803774. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR. Model-Based Direct Adjustment. Journal of the American Statistical Association. 1987;82:387–394. [Google Scholar]
- Schnurr PP, Jankowski MK. Physical health and post-traumatic stress disorder: review and synthesis. Seminars in Clinical Neuropsychiatry. 1999;4:295–304. doi: 10.153/SCNP00400295. [DOI] [PubMed] [Google Scholar]
- Thompson WW, Gottesman II, Zalewski C. Reconciling disparate prevalence rates of PTSD in large samples of US male Vietnam veterans and their controls. BMC Psychiatry. 2006;6:19. doi: 10.1186/1471-244X-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaccarino V, McClure C, Johnson BD, Sheps DS, Bittner V, Rutledge T, Shaw LJ, Sopko G, Olson MB, Krantz DS, Parashar S, Marroquin OC, Merz CN. Depression, the metabolic syndrome and cardiovascular risk. Psychosomatic Medicine. 2008;70:40–48. doi: 10.1097/PSY.0b013e31815c1b85. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Votaw J, Faber T, Veledar E, Murrah NV, Jones LR, Zhao J, Su S, Goldberg J, Raggi JP, Quyyumi AA, Sheps DS, Bremner JD. Major depression and coronary flow reserve detected by positron emission tomography. Archives of Internal Medicine. 2009;169:1668–1676. doi: 10.1001/archinternmed.2009.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss T, Skelton K, Phifer J, Jovanovic T, Gillespie CF, Smith A, Umpierrez G, Bradley B, Ressler KJ. Posttraumatic stress disorder is a risk factor for metabolic syndrome in an impoverished urban population. General Hospital Psychiatry. 2011 doi: 10.1016/j.genhosppsych.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R. Post-traumatic stress disorder. New England Journal of Medicine. 2002;346:108–114. doi: 10.1056/NEJMra012941. [DOI] [PubMed] [Google Scholar]
- Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


