Abstract
Objective: This meta-analysis was conducted to evaluate the efficacy of acupuncture on cognitive impairment (function) after a stroke.
Design: Randomized controlled trials (RCTs) comparing acupuncture with no acupuncture in addition to medicine or rehabilitation were identified from databases (PubMed, Cochrane Central Register of Controlled Trials, Chinese National Knowledge Infrastructure, VIP Chinese Periodical Database, Wangfang Chinese Periodical Database, Chinese Bio-medicine Database, Cochrane Library, and Chinese medical literature databases) and two relevant journals (Chinese Acupuncture and Moxibustion and the Journal of Shanghai Acupuncture and Moxibustion). Meta-analyses were conducted for the eligible RCTs.
Results: Twenty-one trials with a total of 1421 patients met inclusion criteria. Pooled random-effects estimates of the change in the Mini-Mental State Examination were calculated for the comparison of acupuncture with no acupuncture in addition to medicine or rehabilitation. Following 4 weeks and 8 weeks of intervention with acupuncture, the merged mean difference was 3.14 (95% confidence interval [CI], 2.06–4.21; p<.00001) and 2.03 (95% CI, 0.26–3.80; p=0.02), respectively. For the comparison of 3–4 weeks of acupuncture with no acupuncture in addition to medicine or rehabilitation groups, the merged MD in Neurobehavioral Cognitive State Examination total scores was 5.63 (95% CI, 3.95–7.31; p<.00001). For the comparison of 8–12 weeks of acupuncture with no acupuncture in addition to medicine or rehabilitation groups, the P300 latency merged MD was −12.80 (95% CI, −21.08 to −4.51; p<.00001), while the P300 amplitude merged MD was 1.38 (95% CI, 0.93–1.82; p<.00001). Overall, the study quality was rated as moderate on the basis of the Cochrane Handbook for Systematic Reviews of Interventions (part 2: 8.5).
Conclusions: This meta-analysis suggests that acupuncture had positive effects on cognitive function after stroke and supports the need for additional research on the potential benefits of this therapeutic approach.
Introduction
Stroke is a common cerebrovascular disease of the central nervous system whose occurrence increases dramatically with age. Stroke may lead to serious medical complications, resulting in a high mortality rate and increased disability rate. Approximately 70%–80% of stroke survivors experience long-lasting consequences, including motor dysfunction, sensibility dysfunction, and cognitive impairment. Evidence suggests ischemic stroke increases the risk of dementia or cognitive decline, particularly in the elderly. Cognitive impairment is a frequent consequence of stroke, with an estimated 35% of patients presenting with cognitive impairment within 3 months following a stroke1 and up to 32% of patients demonstrating persistent cognitive impairment for up to 3 years following the onset of their first stroke.2 Some patients may develop mild cognitive impairment following a stroke. A recent study provided evidence that vascular mild cognitive impairment is progressive, given that the incidence of dementia was diagnosed in 24.4% of individuals after 3 years, resulting in a mean rate of approximately 8% per year.3
To date, the definition and classification of cognitive impairment vary across studies. Cognition typically includes domains such as attention and concentration, memory, and executive function;4 some researchers also include visual-spatial perception and apraxia as cognitive impairments.5 Including patients who remain cognitively intact after an index stroke, hospital-based and population-based studies6,7 have revealed a significant risk of developing delayed dementia. However, physical handicaps often produce more profound symptoms compared with cognitive deficits following a stroke, and individuals who display slight cognitive deficits generally do not receive treatment. Considering that 40% of survivors are not able to take care of themselves, these cognitive deficits not only bring pain to the patients but also burden their family and society.
Stroke rehabilitation techniques develop rapidly. The World Health Organization8 reported that active rehabilitative therapy may help up to 60% of all surviving stroke victims to resume daily living activities without assistance; approximately 30% of working-age stroke survivors can return to work within 1 year after a stroke. In Western countries, treatments aimed at stroke rehabilitation typically include physiotherapy, occupational therapy, and speech therapy, in addition to the skilled medical and nursing care classified as conventional stroke rehabilitation. Considerable research efforts have focused on improving the many treatment technologies. However, no single rehabilitation intervention has been identified as unequivocally beneficial to recovery. This has led to more recent research on the use of other treatment approaches for stroke rehabilitation, such as acupuncture and Chinese herbal medicine.
Acupuncture is one of the most important treatments of Traditional Chinese Medicine and can be traced back more than 2000 years in China.9 A relatively simple, cheap, and safe treatment compared with other conventional interventions, acupuncture has been accepted by Chinese patients and is widely used to improve the neurologic functions of patients who have had a stroke, including motor function, sensation, and speech. As a therapeutic intervention, acupuncture has also become more frequently used among Western countries.10,11 The utility of acupuncture treatment remains under investigation, even with many lines of evidence supporting its use across diseases. Numerous studies12–15 support the clinical efficacy of acupuncture in stroke rehabilitation, especially in China; nevertheless, some conflicting evidence exists.16 Systematic reviews of trials of acupuncture in stroke rehabilitation have been conducted,13,17–21 including trials on stroke patients in acute, subacute, or chronic stages. One recent systematic review conducted by a Chinese research group indicated that acupuncture appeared to be safe but did not provide any additional benefit to patients with acute stroke.22
As a traditional therapeutic method, acupuncture therapy is a widely recognized alternative measure in current clinical practices. For decades, numerous clinical studies have evaluated the efficacy and safety of acupuncture in patients with cognitive impairment, more specifically with vascular dementia and cognitive impairment after stroke. Researchers designed randomized controlled trials (RCTs) to assess the efficacy of acupuncture on patients with cognitive impairment after stroke, but the results were inconsistent. Several review articles23,24 have summarized the use of acupuncture in patients who have had a stroke. Most of these reviews have highlighted the potential role of acupuncture as a promising treatment for patients with cognitive impairment after stroke, but no conclusions regarding its efficiency were drawn.
No systematic reviews have specifically examined the efficacy and safety of acupuncture on patients with cognitive impairment after stroke. To evaluate the effectiveness and safety of acupuncture therapy for impairment after stroke, a systematic review and meta-analysis were performed. This review used a standardized classification of cognitive impairment in high-quality RCTs of the effects of acupuncture on cognitive impairment after stroke. The purpose of this review was to systematically analyze all RCTs of acupuncture for cognitive impairment after stroke, with the goal of providing evidence-based treatment for clinical practice and assisting with future research.
Materials and Methods
Inclusion and exclusion criteria
Included in this review were original reports published in Chinese or English that described acupuncture as an intervention and provided sufficient methodologic details and specific data on cognitive function. The inclusion criteria for this meta-analysis were as follows: (1) RCT, 2) comparison of acupuncture of any kind with no acupuncture, (3) stroke diagnosis confirmed by computed tomography or magnetic resonance imaging; and (4) cognitive impairment and disability measures that are internationally recognized or nationally approved by an academic body in China. If studies contained three experimental groups with only one group receiving acupuncture, the acupuncture group and one additional treatment group consistent with interventions from other studies were chosen. If there were three experimental groups with two acupuncture groups, a routine acupuncture group was chosen as the intervention group and the nonacupuncture treatment group was chosen as the control group.
Trials were excluded if they met any of the following criteria: (1) no control group included in the original article; (2) acupuncture used in both the treatment group and the control group; (3) standardized indices of curative effect or detailed results of treatment not included; and (4) comparison of the intervention group with the control group in addition to treatment methods other than acupuncture, such as drugs or other forms of Traditional Chinese Medicine.
Search strategy
Electronic literature searches were performed in eight databases from their inception to February 2012 (PubMed, Cochrane Central Register of Controlled Trials, Foreign Medical Journal Service, Foreign Evidence-based Medicine, Vip Chinese Periodical Database, Chinese National Knowledge Infrastructure, Wangfang Chinese Periodical Database, and Chinese Bio-medicine Database) and two relevant journals (Chinese Acupuncture and Moxibustion and the Journal of Shanghai Acupuncture and Moxibustion). The search featured a wide coverage of reports and prospective studies within the field in order to provide sufficient data for analysis.
The search terms used were “acupuncture/electroacupuncture/auricular acupuncture, cognitive” AND “stroke/CVA/cerebrovascular accident/cerebral infarction/intracerebral hemorrhage/cerebral embolism (acupuncture OR acu*), cognitive” AND “(stroke OR apoplexy OR CVA OR cerebrovascular attack OR cerebrovascular accident OR cerebrovascular* OR cerebral infarction OR cerebral hemorrhage OR cerebral*).” One reviewer also manually searched Chinese Acupuncture and Moxibustion (2008–December 2012) and Journal of Shanghai Acupuncture and Moxibustion (2008–December 2012), which referenced trials and review articles, as well as acupuncture conference proceedings in China.
To include as many reports as possible on cognitive impairment, the publication date range was not limited and included all years for each individual database.
Study eligibility
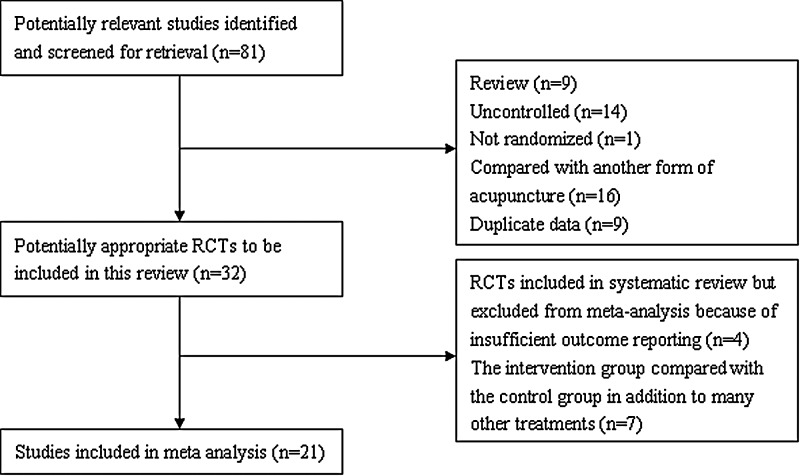
Information on patients, methods, interventions, outcomes, and results were extracted independently by two reviewers using a self-developed data extraction form. Disagreements were resolved by a third member or through discussion between reviewers. One researcher picked out duplications of these reports via NoteExpress and scanned the title and abstract of the citation retrieved by the selection search engine (first scanning). Another researcher then viewed the full text of all potentially eligible reports obtained, after which similar reports were marked as “suspicious duplications” and compared. If the similarity rate of these articles appeared at or above 80%, the report containing the most detailed information was included while the other articles were omitted. Disagreements between the two reviewers were resolved by the research team (Fig. 1).
FIG. 1.
Study flow diagram of selection of randomized, controlled trials (RCTs).
Data extraction
Two researchers compiled a table listing the general information of the final included reports. The table listed the report title, journal name, year of publication, type of control, number of participants, and country of publication. Any missing information was coded as “not reported,” and disagreements were resolved by consulting related references before the table was finalized. Two reviewers scanned the full text of all 21 reports and compiled the relevant data (Table 1).
Table 1.
Characteristics of Randomized, Controlled Trials Included in Meta-Analysis
| Treatment | ||||||
|---|---|---|---|---|---|---|
| Author, Year | Source of diagnostic criteria | Total sample size (intervention/control groups (n) | Intervention | Control | Intervention period (wk) | Outcome measurement for cognition |
| Xie et al., 2012 | FNACCVD confirmed by head CT or MRI | 66 (34/32) | Conventional treatment+rehabilitation+electroacupuncture | Conventional treatment+rehabilitation | 12 | P300 |
| Li et al., 2012 | CECS confirmed by head CT or MRI | 94 (48/46) | Conventional treatment+nimodipine+electroacupuncture | Conventional treatment+nimodipine | 12 | MMSE, HDS-R |
| Kang et al., 2011 | FNACCVD confirmed by head CT or MRI | 48 (24/24) | Conventional treatment+rehabilitation+electroacupuncture | Conventional treatment+rehabilitation | 8 | MMSE, P300 |
| Sun et al., 2011 | FNACCVD confirmed by head CT or MRI | 72 (36/36) | Conventional treatment+donepezil hydrochloride+acupuncture | Conventional treatment+donepezil hydrochloride | 4 | MMSE, MMSE efficiency |
| Jiang et al., 2011 | FNACCVD confirmed by head CT or MRI | 40 (20/20) | Conventional treatment+rehabilitation+electroacupuncture | Conventional treatment+rehabilitation | 8 | MMSE, P300 |
| Jia et al., 2011 | Unclear | 100 (50/50) | Conventional treatment+nimodipine+acupuncture | Conventional treatment+nimodipine | 12 | MoCA |
| Yang et al., 2011 | FNACCVD confirmed by head CT or MRI | 40 (20/20) | Conventional treatment+rehabilitation+electroacupuncture | Conventional treatment+rehabilitation | 8 | MMSE, P300 |
| Rao et al., 2010 | FNACCVD confirmed by head CT or MRI | 60 (30/30) | Conventional treatment+rehabilitation+electroacupuncture | Conventional treatment+rehabilitation | 4, 12 | FCA Improve Value |
| Wu et al., 2010 | Head CT or MRI | 40 (20/20) | Conventional treatment+xingnaojing+acupuncture | Conventional treatment+xingnaojing | 4 | MMSE |
| Lin et al.,. 2010 | FNACCVD confirmed by head CT or MRI | 82 (52/30) | Conventional treatment+xingnaojing+acupuncture | Conventional treatment+xingnaojing | 3 | MMSE |
| Zhu et al., 2010 | FNACCVD confirmed by head CT or MRI | 167 (83/84) | Conventional treatment+rehabilitation+acupuncture | Conventional treatment+rehabilitation | 4 | FCA |
| Wang et al., 2009 | FNACCVD confirmed by head CT or MRI | 68 (34/34) | Conventional treatment+rehabilitation+acupuncture | Conventional treatment+rehabilitation | 8 | LOTCA |
| Guo et al., 2009 | FNACCVD confirmed by head CT or MRI | 80 (40/40) | Conventional treatment+rehabilitation+acupuncture | Conventional treatment+rehabilitation | 6 | FIM, NIHSS |
| Chou et al., 2009 | Unclear | 33 (17/16) | Conventional treatment+rehabilitation+electroacupuncture | Conventional treatment+rehabilitation | 8 | LOTCA-G |
| Wang et al., 2008 | FNACCVD confirmed by head CT or MRI | 60 (30/30) | Conventional treatment+rehabilitation+acupuncture | Conventional treatment+rehabilitation | 2, 4, 8 | SECF |
| Huang et al., 2008 | Confirmed by head CT or MRI | 80 (40/40) | Conventional treatment+rehabilitation+acupuncture | Conventional treatment+rehabilitation | 4 | MMSE, CDT, block test |
| Li et al., 2008 | FNACCVD confirmed by head CT or MRI | 40 (20/20) | Conventional treatment+electroacupuncture | Conventional treatment | 4 | MMSE |
| Yu et al., 2007 | CECS confirmed by head CT or MRI | 51 (25/26) | Conventional treatment+nimodipine+electroacupuncture | Conventional treatment+nimodipine | 24 | MMSE efficiency, WMS |
| Guo et al., 2007 | FNACCVD confirmed by head CT or MRI | 80 (40/40) | Conventional treatment+acupuncture | Conventional treatment | 2 | NIHSS, FIM |
| Liu et al., 2006 | Clinical manifestations confirmed by head CT or MRI | 84 (43/42) | Conventional treatment+acupuncture | Conventional treatment | 3 | NCSE |
| Yang et al., 2006 | FNACCVD confirmed by head CT or MRI | 36 (18/18) | Conventional treatment+rehabilitation+acupuncture | Conventional treatment+rehabilitation | 4 | NCSE |
FNACCVD, Fourth National Academic Conference of Cerebral Vascular Diseases; CT, computed tomography; MRI, magnetic resonance imaging; CECS, Chinese expert consensus standards, proposed in 2005 for the prevention and treatment of cognitive dysfunction; MMSE, Mini-Mental State Examination; HDS-R, Revised Hasegawa's Dementia Scale; MoCA, Montreal Cognitive Assessment; FCA, Functional Comprehensive Assessment; LOTCA, Loewenstein Occupational Therapy Cognitive Assessment; FIM, Functional Independence Measure; NIHSS, National Institutes of Health Stroke Scale; SECF, Scale of Elderly Cognitive Function; CDT, Clock Drawing Task; WMS, Wechsler Memory Scale; NCSE, Neurobehavioral Cognitive State Examination.
Recorded data contained study characteristics, patient characteristics, and outcomes. An internationally recognized examination of cognitive impairment is generally composed of the following assessments: the Mini-Mental State Examination (MMSE), the Neurobehavioral Cognitive State Examination (NCSE), the Wechsler Memory Scale (WMS), the Functional Comprehensive Assessment (FCA), the National Institutes of Health Stroke Scale (NIHSS), the Functional Independence Measure (FIM), the Scale of Elderly Cognitive Function (SECF), the Montreal Cognitive Assessment (MoCA), the Loewenstein Occupational Therapy Cognitive Assessment (LOTCA), the Revised Hasegawa's Dementia Scale (HDS-R), the Clock Drawing Task (CDT), and the cognitive potential P300. Among these methods listed, P300 is the late component of an event-related potential (ERP) in the cerebral cortex and reflects the functioning of the neurochemical systems involved in cognitive processes.25
Statistical analysis
RevMan 5.02 (Cochrane Collaboration, Oxford, United Kingdom) was used to perform the meta-analysis. An odds ratio was used for enumeration data, and the weighted mean difference was used for continuous variables. For continuous data, two types of estimates were calculated. The measure of the treatment difference for any outcome was calculated as (1) the mean difference (MD) when the pooled trials used the same rating scale or test or (2) the standardized MD when the trials used a different rating scale or test. Both parameters were expressed with 95% confidence intervals (CIs). Heterogenous test results were expressed by using the random-effects model, and homogeneous test results were expressed with the fixed-effects model. Heterogeneous test results were analyzed with sensitivity and subgroup exploration. Homogeneity of weighted MD across studies was assessed by using the Cochrane Q statistic and the I2 statistic. A significant Q statistic (p<0.10) or I2>50% indicated heterogeneity across studies. The Begg rank correlation test and Egger linear regression test with p<0.10 indicated statistical significance.
Methodologic quality
The quality of clinical research articles was assessed via reference to the Cochrane Handbook for Systematic Reviews of Interventions, part 2: 8.5 (Table 2). The tool book consists of seven specific domains: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and “other issues,” such as early termination of the study and group differences at baseline that would impede data analysis. Each domain was evaluated as having low risk of bias high risk of bias, or unclear risk of bias in accordance with the judgment criteria. For each entry, a “yes” answer indicated a low risk of bias, “no” indicated a high risk of bias, and “unclear” indicated an unclear or unknown risk of bias. All test data were merged with the terminal index to obtain a positive result.
Table 2.
Risk of Bias in Included Randomized Controlled Trials
| Author, Year | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Binding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Xie et al., 2012 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | Unclear |
| Li et al., 2012 | Low risk | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Kang et al., 2011 | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Sun et al., 2011 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | High risk |
| Jiang et al., 2011 | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Jia et al., 2011 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Yang et al., 2011 | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Rao et al., 2010 | Unclear | Unclear | Unclear | High risk | Low risk | Low risk | Low risk |
| Wu et al., 2010 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | High risk |
| Lin et al., 2010 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Zhu et al., 2010 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | Unclear |
| Wang et al., 2009 | High risk | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Guo et al., 2009 | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk | Low risk |
| Chou et al., 2009 | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk | Low risk |
| Wang et al., 2008 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Huang et al., 2008 | Low risk | Unclear | Unclear | Unclear | Low risk | Low risk | Unclear |
| Li et al., 2008 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Yu et al., 2007 | High risk | Unclear | Unclear | Unclear | Low risk | Low risk | Unclear |
| Guo et al., 2007 | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk | High risk |
| Liu et al., 2006 | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk | Low risk |
| Yang et al., 2006 | Low risk | Low risk | Unclear | High risk | Low risk | Low risk | Low risk |
Based on Cochrane Handbook for Systematic Reviews of Interventions, Part 2: 8.5.
Results
Characteristics of included trials
The 21 included trials22,26–30,45–59 were conducted in China and included a total of 1421 patients ranging in age from 18 to 80 years. More male than female participants were included in 15 trials, while four trials did not describe the sex of the patients.26–27,46,50 The treatment period ranged from 2 to 24 weeks. Treatment sessions varied from 28 to 120 sessions, and the frequency of the sessions ranged from five sessions per week to two sessions per day. The acupuncture interventions varied significantly across the 21 trials. Nine trials were conducted by manual stimulation only, and 12 trials were conducted by electrical stimulation only. Acupuncture point prescriptions were also not consistent. Five trials24,28,47–49 involved only scalp acupoints, one trial29 contained only body acupoints, and the other trials contained both body and scalp acupoints. Moreover, in all included trials, the number of points varied considerably and the needle retention time ranged from 15 to 30 minutes.
The time interval between stroke onset and treatment varied. In 10 trials the time interval ranged from 48 hours to 1 month, and in nine trials, the time interval was 3 to 36 months. In two trials the time interval was unclear.50,51
The internationally recognized examination of cognitive impairment consisted of the MMSE, NCSE, WMS, FCA, NIHSS, FIM, SECF, MoCA, LOTCA, HDS-R, CDT, and cognitive potential P300.
Summary of meta-analysis
MMSE
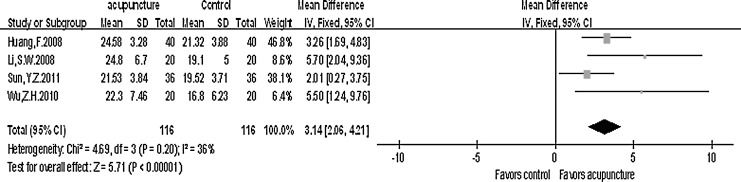
Four trials with a total of 116 patients30,46,50,51 measured improved MMSE total scores after 4-week acupuncture treatment. Heterogeneous tests were performed on the four referred trials. For the comparison of 4-week acupuncture with no acupuncture in addition to medicine or rehabilitation group, the MMSE total scores (chi-square=4.69; p=.20; I2=36%) indicated that the included studies were of clinical and statistical heterogeneity. The fixed-effects model was adopted in the meta-analysis; the merged MD value was 3.14 (95% CI, 2.06–4.21). The tests for overall effect (Z=5.71; p<.00001) revealed a statistically significant difference between the test and control groups on the MMSE after 4 weeks of treatment (Fig. 2).
FIG. 2.
Mini-Mental State Examination total scores after 4 weeks of treatment. CI, confidence interval; SD, standard deviation.
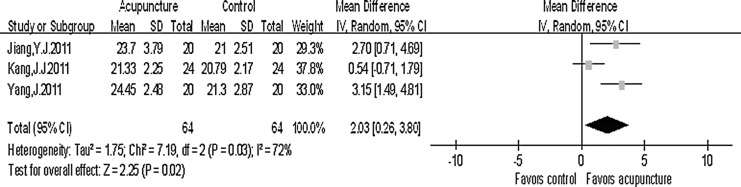
Three trials with a total of 64 patients47–49 measured improved MMSE total scores after an 8-week acupuncture treatment. For the comparison of 8-week acupuncture with no acupuncture in addition to medicine or rehabilitation group, the MMSE total scores (chi-square=7.19; p=0.03; I2=72%) indicated that included studies were of clinical and statistical heterogeneity. The random-effects model was adopted in the meta-analysis; the merged MD value was 2.03 (95% CI, 0.26–3.80). The tests for overall effect (Z=2.25; p=0.02) revealed a statistically significant difference between the test and control groups on the MMSE after 8 weeks of treatment (Fig. 3).
FIG. 3.
Mini-Mental State Examination total scores after 8 weeks of treatment.
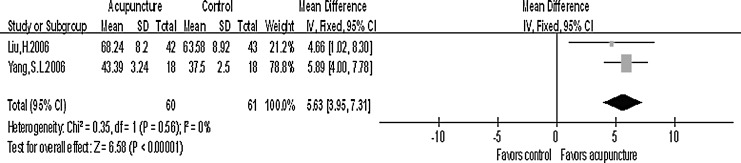
NCSE
Two trials with a total of 61 patients22,31 measured improved NCSE total scores after 3–4 weeks of acupuncture treatment. For the comparison of 3–4 weeks acupuncture with no acupuncture in addition to medicine or rehabilitation group, the NCSE total scores were compared (chi-square=0.35; p=0.56; I2=0%). The fixed-effects model was adopted in the meta-analysis; the merged odds ratio was 5.63 (95% CI, 3.95–7.31). The tests for overall effect (Z=6.58; p<.00001) revealed a statistically significant difference between the test and control groups on the NCSE after 3–4 weeks of treatment (Fig. 4).
FIG. 4.
Neurobehavioral Cognitive State Examination total scores after 3–4 weeks of treatment.
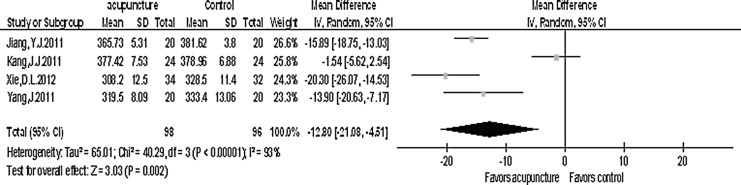
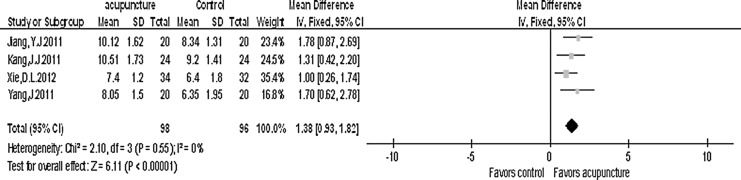
P300
Four trials with a total of 98 patients27,47–49 measured an improved P300 after acupuncture treatment. The P300 was measured by the key point electromyography/evoked potential instrument with auditory oddball paradigm. The main index consisted of latency and amplitude. For the comparison of 8–12 weeks of acupuncture with no acupuncture in addition to medicine or rehabilitation group, the P300 latency (chi-square=40.29; p<.00001; I2=93%) indicated that included studies were of clinical and statistical heterogeneity. The fixed-effects model was adopted in the meta-analysis; the merged MD value was −12.80 (95% CI, −21.08 to 4.51). The tests for overall effect (Z=3.03; p=.002) revealed a statistically significant difference between the test and control groups in latency (Fig. 5).
FIG. 5.
P300 latency after 8–12 weeks of treatment.
For the comparison of 8–12 weeks of acupuncture with no acupuncture in addition to medicine or rehabilitation group, the P300 amplitude was compared (chi-square=2.10; p=.55; I2=0%). The fixed-effects model was adopted in the meta-analysis; the merged MD value was 1.38 (95% CI, 0.93–1.82). The tests for overall effect (Z=6.11; p<.00001) indicated a statistically significant difference in amplitude between the test and control groups in amplitude (Fig. 6).
FIG. 6.
P300 amplitude after 8–12 weeks of treatment. CI=confidence interval; SD=standard deviation.
The other trials measured improved cognitive impairment after various acupuncture treatments for which the time interval was different; thus, the index was not merged.
Discussion
The conclusion drawn from the present data is that acupuncture may improve cognitive impairment after stroke. Numerous papers have discussed the effects of acupuncture on impaired cognitive function and have proposed the possible mechanisms of acupuncture that may lead to improved cognitive function after stroke. Litscher and colleagues32 reported that acupuncture may increase mean values of regional cerebral oxygen saturation and significantly increase mean blood flow velocity of the right middle cerebral artery. Lee and coworkers33 investigated the correlation between acupuncture and neuroimaging using single-photon emission computed tomography in patients with stroke. The results of their study suggested that postacupuncture images showed multiple activation sites in the periphery of the ischemic area or in the hypoperfused zone in the affected vascular territory.
The correlation between cognition and cerebral blood flow may partly explain the cognitive-enhancing effect of acupuncture.34 Dos Santos and colleagues35 suggested that electroacupuncture may prevent atrophy of some limbic structures, and thus improve cognitive deficits in pilocarpine-epileptic rats. The authors of that study postulated that this effect may depend on the serotonergic system.35 Wang and associates36 suggested that electroacupuncture may modulate the production and clearance of free radicals, as well as improve memory and the ability to learn in a rat model of vascular dementia. Furthermore, evidence from functional magnetic resonance imaging indicated that different acupoints on the same meridian may activate certain similar areas of the brain.26
The late component of the ERPs, the P300, is a marker for cognitive brain function. The hippocampus, thalamus, and frontal cortex are considered potential locations of the P300 generators,37 and these structures are important for learning and memory. P300 has been widely used to assess cognitive decline in various diseases affecting the central nervous system, especially in dementia-related disorders.38–41 P300 latency increases as dementia symptoms increase. It is considered a consequence of the attention process, speed of the reaction, and immediate memory. Shorter P300 latencies indicate a superior mental performance relative to longer latencies.42 Sufficient evidence suggests that the latency and amplitude of the P300 are altered in Alzheimer's disease. Furthermore, evidence indicates that the characteristics of the P300 wave are also compromised in individuals with mild cognitive impairment. Recent studies suggest that the latency and amplitude of the P300 wave might serve as a marker for monitoring the process through which mild cognitive impairment progresses to AD. Thus, the main indexes of P300 (1atency and amplitude) reflect complicated emotional activities, such as cognition, memory, and cognitive impairment. Evidence suggests that ERP is an objective, sensitive, and specific indicator in evaluating cognitive impairment, and P300 can be used to measure the severity of the impairment.37,38
Four trials with a total of 98 patients showed that acupuncture had a positive effect on restoring cognitive function after stroke. These findings suggest that the deleterious effects of cerebral infarction may improve with Traditional Chinese Medicine. Tang43 argued that scalp acupuncture should be the first choice in treating ischemic stroke. Scalp acupuncture activates the cerebral collateral circulation, increases blood volume in the brain, improves the velocity of blood flow, and repairs the ischemic condition in the affected area of the brain;27,44 thus, it provide a potential mechanism for the therapeutic effects of this approach. Therefore, P300 can be used as one of the objective indicators for evaluating the therapeutic effect of scalp acupuncture.
Two trials45,46 demonstrated that acupuncture did not improve cognitive impairment after stroke. Potential explanations for these discrepant findings include the short length of the intervention period, the differential placement of acupuncture points, the different methods of evaluation, and small sample size.
The outcome of this meta-analysis needs to be confirmed in future, prospective studies that include larger sample sizes. Limitations of this study that may have affected the results include small sample sizes, different criteria for evaluating cognitive function across studies, and the high risk of bias of the included studies. Furthermore, these analyses focused on comparing the overall effectiveness of combined treatment with acupuncture, without specifically analyzing the effects of acupuncture alone or the potential adverse incidents. It is difficult to comprehensively evaluate the differential effects of acupuncture from nonacupuncture interventions on cognitive impairment after stroke. In reference to the included trials, several different methods were selected for the assessment of cognitive impairment after stroke, and the intervention period varied across studies. Questions regarding how to achieve sensitive assessment methods and how long the treatment effects may last need to be resolved in future studies. Moreover, this study focused solely on cognitive function, and therefore future research is necessary to determine whether acupuncture can actively restore other functions of patients with stroke. Finally, the search was confined to reports written in Chinese or English because most journals on acupuncture are published in these languages. It is possible that additional reports may be included in non-Chinese databases or in other languages, which may have limited the results of our study.
The growing popularity of acupuncture, which is largely based on positive outcomes that are associated with less severe adverse effects and lower costs, clearly warrants additional research. Large-scale sham- or placebo-controlled trials are needed to confirm or refute the available evidence for acupuncture as an efficacious treatment for patients who have had a stroke. Future studies should clearly define the modality of acupuncture, use evidence-based acupuncture techniques and rigorous methods, adopt standard measures of assessment, and validate the outcomes. Future studies should also be reported according to the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) criteria in conjunction with the Consolidated Standards of Reporting Trials (CONSORT) criteria.
In conclusion, evidence from this meta-analysis suggests that acupuncture may improve cognitive function after stroke and supports the need for future research.
Acknowledgments
This study was supported by the Fujian University of Traditional Chinese Medicine. The authors are particularly indebted to Mr. Jing-Yu Tan for his review of the Chinese literature. They also thank Ms. Xue-Ping Lin for grammatical review of the manuscript.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Tatemichi T, Desmond D, Stern Y, et al. Cognitive impairment after stroke: frequency, patterns, and relationship to functional abilities. J Neurol Neurosurg Psychiatry 1994;57:202–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel M, Coshall C, Rudd AG, et al. Natural history of cognitive impairment after stroke and factors associated with its recovery. Clin Rehab 2003;17:158–166 [DOI] [PubMed] [Google Scholar]
- 3.Sachdev PS, Chen X, Brodaty H, et al. The determinants and longitudinal course of post-stroke mild cognitive impairment. J Int Neuropsychol Soc 2009;15:915–923 [DOI] [PubMed] [Google Scholar]
- 4.Unsworth C. Reflections on the process of therapy in cognitive and perceptual dysfunction. In: Cognitive and Perceptual Dysfunction: A Clinical Reasoning Approach to Evaluation and Intervention. Philadelphia: FA Davis; 1999:75–124 [Google Scholar]
- 5.Cicerone KD, Dahlberg C, Malec JF, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Arch Phys Med Rehab 2005;86:1681–1692 [DOI] [PubMed] [Google Scholar]
- 6.Tatemichi T, Paik M, Bagiella E, et al. Risk of dementia after stroke in a hospitalized cohort Results of a longitudinal study. Neurology 1994;44:1885–1891 [DOI] [PubMed] [Google Scholar]
- 7.Kokmen E, Whisnant J, O'Fallon W, et al. Dementia after ischemic stroke. A population-based study in Rochester, Minnesota (1960–1984). Neurology 1996;46:154–159 [DOI] [PubMed] [Google Scholar]
- 8.Recommendation on stroke prevention, diagnosis and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke 1989;20:1407. [DOI] [PubMed] [Google Scholar]
- 9.Wu J-N. A short history of acupuncture. J Alt Complement Med 1996;2:19–21 [DOI] [PubMed] [Google Scholar]
- 10.Johansson K, Lindgren I, Widner H, et al. Can sensory stimulation improve the functional outcome in stroke patients? Neurology 1993;43:2189–2192 [DOI] [PubMed] [Google Scholar]
- 11.NIH consensus conference: acupuncture. JAMA 1998;280:1518–1524 [PubMed] [Google Scholar]
- 12.Hu H-H, Chung C, Liu T-J, et al. A randomized controlled trial on the treatment for acute partial ischemic stroke with acupuncture. Neuroepidemiology 1993;12:106–113 [DOI] [PubMed] [Google Scholar]
- 13.Sze FK-H, Wong E, Yi X, et al. Does acupuncture have additional value to standard poststroke motor rehabilitation? Stroke 2002;33:186–194 [DOI] [PubMed] [Google Scholar]
- 14.Zhang X, Yuan Y, Kuang P, et al. [The changes of vasoactive intestinal peptide somatostatin and pancreatic polypeptide in blood and CSF of acute cerebral infarction patients and the effect of acupuncture on them]. Zhen Ci Yan Jiu 1996;21:10. [PubMed] [Google Scholar]
- 15.Sun H, Li X. [Clinical study on treatment of cerebral apoplexy with penetration needling of scalp acupoints]. Zhongguo Zhen Jiu 2001;21:275–278 [Google Scholar]
- 16.Johansson BB, Haker E, von Arbin M, et al. Acupuncture and transcutaneous nerve stimulation in stroke rehabilitation. A randomized, controlled trial. Stroke 2001;32:707–713 [DOI] [PubMed] [Google Scholar]
- 17.Ernst E, White A. Acupuncture as an adjuvant therapy in stroke rehabilitation? Wiener Medizin Wochenschr 1996;146:556. [PubMed] [Google Scholar]
- 18.Hopwood V. Acupuncture in stroke recovery: a literature review. Complement Ther Med 1996;4:258–263 [Google Scholar]
- 19.Park J, Hopwood V, White AR, et al. Effectiveness of acupuncture for stroke: a systematic review. J Neurol 2001;248:558–563 [DOI] [PubMed] [Google Scholar]
- 20.Smith LA, Moore OA, McQuay HJ, et al. Assessing the evidence of effectiveness of acupuncture for stroke rehabilitation: stepped assessment of likelihood of bias. Bandolier 2001 [Google Scholar]
- 21.Wu H, Tang J, Lin X, et al. Acupuncture for stroke rehabilitation. Cochrane Database Syst Rev 2009;1:1–24 [DOI] [PubMed] [Google Scholar]
- 22.Liu H, Wang Y, Ren H. An effect of acupuncture on ADL and cognitive function in patients with ischemic stroke. Chin J Rehab Med 2006;21:444–448 [Google Scholar]
- 23.Zhou X, Chen S, He J, et al. Clinical observations on treatment of post-cerebral infarction mild cognitive dysfunction by mind-regulating and meridian-unblocking acupuncture. Shang Hai Zhen Jiu Za Zhi 2008;27:3–4 [Google Scholar]
- 24.Guohui L, Xiuqun S, Xijun H, et al. Observation on therapeutic effect of acupuncture combined with cognitive training on cerebral arterial thrombosis patients with mild cognitive impairment. Chin Arch Trad Chin Med 2006;24:1759–1761 [Google Scholar]
- 25.Li L, Liu H, Li Y-Z, et al. The human brain response to acupuncture on same-meridian acupoints: evidence from an fMRI study. J Alt Complement Med 2008;14:673–678 [DOI] [PubMed] [Google Scholar]
- 26.Wang W, Fu JM, Gu XD, et al. Effect of scalp acupuncture combined with cognitive training on cognitive function of acute stroke patients. Chin J Rehab Theory Pract 2009;15:1046–1048 [Google Scholar]
- 27.Xie DL, Zhu LF, Liu HY, et al. Application of P300 in scalp acupuncture for cognitive disorder due to cerebral infarction. J Acupunct Tuina Sci 2012;10:26–28 [Google Scholar]
- 28.Chou P, Chu H, Lin JG. Effects of electroacupuncture treatment on impaired cognition and quality of life in Taiwanese stroke patients. J Alt Complement Med 2009;15:1067–1073 [PubMed] [Google Scholar]
- 29.Jia X, Meng L. Observation on the efficacy of lower point selection for upper disease in treating cognitive impairment after acute cerebral infarction. Shang Hai Zhen Jiu Za Zhi 2011;30:589–590 [Google Scholar]
- 30.Huang ZM, Prasad C, Britton FC, et al. Functional role of CLC-2 chloride inward rectifier channels in cardiac sinoatrial nodal pacemaker cells. J Molec Cell Cardiol 2009;47:121–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang X, Lai X, Zhang Y, et al. [siRNA-mediated silencing of ClC-2 gene inhibits proliferation of human U-87 glioma cells]. Chin J Cancer 2006;25:805. [PubMed] [Google Scholar]
- 32.Litscher G, Schwarz G, Sandner-Kiesling A, et al. Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res 1998;20:S28. [DOI] [PubMed] [Google Scholar]
- 33.Lee JD, Chon J, Jeong H, et al. The cerebrovascular response to traditional acupuncture after stroke. Neuroradiology 2003;45:780–784 [DOI] [PubMed] [Google Scholar]
- 34.Osawa A, Maeshima S, Shimamoto Y, et al. Relationship between cognitive function and regional cerebral blood flow in different types of dementia. Disabil Rehab 2004;26:739–745 [DOI] [PubMed] [Google Scholar]
- 35.Dos Santos JG, Tabosa A, do Monte FHM, et al. Electroacupuncture prevents cognitive deficits in pilocarpine-epileptic rats. Neurosci Lett 2005;384:234–238 [DOI] [PubMed] [Google Scholar]
- 36.Wang L, Tang C, Lai X. Effects of electroacupuncture on learning, memory and formation system of free radicals in brain tissues of vascular dementia model rats. J Trad Chin Med 2004;24:140. [PubMed] [Google Scholar]
- 37.Ball SS, Marsh JT, Schubarth G, Brown WS, Strandburg R. Longitudinal P300 latency changes in Alzheimer's disease. J Gerontol 1989;44:195–200 [DOI] [PubMed] [Google Scholar]
- 38.Ally BA, Jones GE, Cole JA, Budson AE. The P300 component in patients with Alzheimer's disease and their biological children. Biol Psychol 2006;72:180–187 [DOI] [PubMed] [Google Scholar]
- 39.Bennys K, Portet F, Touchon J, Rondouin G. Diagnostic value of event-related evoked potentials N200 and P300 subcomponents in early diagnosis of Alzheimer's disease and mild cognitive impairment. J Clin Neurophysiol 2007;24:405–412 [DOI] [PubMed] [Google Scholar]
- 40.Bonanni L, Franciotti R, Onofrj V, et al. Revisiting P300 cognitive studies for dementia diagnosis: early dementia with Lewy bodies (DLB) and Alzheimer disease (AD). Neurophysiol Clin. 2010;40:255–265 [DOI] [PubMed] [Google Scholar]
- 41.Donchin E, Coles M. Is the P300 component a manifestation of context updating? Behav Brain Sci 1988;11:357–374 [Google Scholar]
- 42.Polich J. P300 clinical utility and control of variability. J Clin Neurophysiol. 1998;15:14–33 [DOI] [PubMed] [Google Scholar]
- 43.Tang S. Clinical study on scalp acupuncture based treatment for ischemic stroke. Shang Hai Zhen Jiu Za Zhi 2001;20:6–7 [Google Scholar]
- 44.Ji R, Cui Y, Wang D, et al. Integrated scalp and body acupuncture for the elderly with paralysis due to cerebral hemorrhage after operation in early-stage. Zhong Guo Lin Chuang Kang Fu 2003;7:1610 [Google Scholar]
- 45.Guo R, Liu L, Ma X. [Long-term effect of acupuncture on quality of life in patients with early stage of stroke]. Chin J Integrat Trad Western Med 2007;27:708–709 [PubMed] [Google Scholar]
- 46.Li SW, Zhang ZX. The effect of acupuncture on patients with cerebral infarction. J Zhejiang Univ Trad Chin Med 2008;32:514–515 [Google Scholar]
- 47.Kang JJ. Clinical study of effect of electroacupuncture on GV20 and EX-HN1 on stroke patients with cognitive impairment [Thesis]. Fujian, China: Fujian University of Traditional Chinese Medicine; 2011 [Google Scholar]
- 48.Jiang YJ. Electroacupuncture DU20 and DU24 treatment on cognitive impairment after stroke 2011;Fujian University Of Traditional Chinese Medicine; Master's degree thesis [Google Scholar]
- 49.Yang J. The clinical study on cognitive impairment after stroke by using the treatment of electroacupuncture given at DU20 and GB20 [Thesis]. Fujian, China: Fujian University of Traditional Chinese Medicine; 2011 [Google Scholar]
- 50.Wu ZH. Observation on therapeutic effect of acupuncture combined with Xingnaojing injectio in the treatment of patients with multi-infarct dementia. Proceedings of the 7th National Rehabilitation Therapy Conference of Chinese Association of Rehabilitation Medicine2010;244–246 [Google Scholar]
- 51.Sun YZ, Wu WP. An effect of scalp acupuncture on cognitive function in 36 patients with cognitive impairment after ischemic stroke. J Clin Acupunct Moxibust 2011;27:11–13 [Google Scholar]
- 52.Rao J, Shao WB, Wang T. Effect of standardized tertiary rehabilitation and integrated Chinese and Western medicine on promoting of the cognitive function in acute stroke patients. Med J Chin Peoples's Health 2010;22:2008–2010 [Google Scholar]
- 53.Lin H, Ding XJ, Fu B. Effect of acupuncture and moxibusion combined with drug on cognitive impairment after stroke. Mod J Integr Trad Chin West Med 2010;19:36–37 [Google Scholar]
- 54.Wang B. Effect of acupuncture combined with cognitive craining on cognitive function and disability in elderly patients with cerebral apoplexy. Master's thesis, Hubei University of Traditional Chinese Medicine, 2008 [Google Scholar]
- 55.Zhu XJ, Wang T, Ouyang G, Zhang LX, Shen GY, Shao WB. Effects of upper-extremity rehabilitation on ADL and QOL in stroke patients. Chin J Trauma Disabil Med 2010;18:31–33 [Google Scholar]
- 56.Li W, Cheng YH, Yu XG. Observation on therapeutic effect of acupuncture combined with medicine on mild disorders in patients with post-stroke. Chin Acupunct Moxibustion 2012;32:3–7 [PubMed] [Google Scholar]
- 57.Guo RY, Su L, Liu LA, Wang CX. The Effects of Linggui Bafa acupuncture on the recovery and quality of life in patients with post-stroke depression. The third thromboembolic disease conference held by China Association of Chinese medicine 2009;167–173 [Google Scholar]
- 58.Yu XG, Sun SL, Cheng YH. Effect of Du Meridian acupuncture in patients with cognitive impairment after ischemic stroke. J Integr Med Cardio Cerebrovasc Dis 2007;12:1171–1173 [Google Scholar]
- 59.Yang SL. Effects of needing combined with cognitive function training on the cognitive function of stroke patients. Master's thesis, Fujian University of Traditional Chinese Medicine, 2006 [Google Scholar]