Abstract
Objective
Relations between interpartner psychological conflict (IPC) and the sleep of men and women were examined, and depression and anxiety symptoms were assessed as intervening variables of these associations.
Method
Participants were 135 cohabiting or married couples. The mean age was 36.50 (SD = 5.93) for women and 39.37 (SD = 7.33) for men. Most women (76%) and men (78%) were European American (EA) and the rest were predominantly African American (AA); there was a wide socioeconomic representation. Men and women reported on IPC used by their partner against them. Sleep was examined objectively with actigraphs, and multiple sleep quantity and quality measures were derived.
Results
Dyadic path analysis in which both actor and partner effects were assessed was conducted. For women, greater IPC by the partner was related to elevated levels of anxiety, which in turn was associated with shorter sleep duration and worse sleep efficiency; anxiety was an intervening variable. For men, IPC by the partner was related to greater symptoms of anxiety and depression; the latter was an intervening variable linking IPC with sleep quality (lower efficiency, longer latency). Some partner effects were observed and indicate that for both men and women, one’s perpetration of IPC is related to increased anxiety in the partner, which in turn is related to longer sleep latency for the actor.
Conclusion
Results build on this scant literature, and using objective well-validated measures of sleep highlight the importance of relationship processes and mental health for the sleep of men and women.
Keywords: sleep, conflict, actigraphy, interpartner psychological conflict, depression, anxiety
Interpartner psychological conflict (IPC), defined as the use of nonphysical but potentially hurtful behaviors during conflict such as yelling, name calling, and using verbal threats (Schumacher, Slep, & Heyman, 2001) is common in intimate relationships, with estimates of prevalence ranging from nearly 3 out of 4 couples in engaged and nonclinic married couples up to nearly all couples in a marital therapy clinic reporting at least one incidence of IPC (Murphy & Cascardi, 1999). Though most of IPC is relatively mild in comparison to physical aggression, IPC still has been associated with a wide range of negative consequences for its recipient, from increased drug use to poorer mental health to an increased risk of chronic diseases (Coker et al., 2002). In fact, some have even suggested that the effects of IPC are worse than those of physical violence in community samples (Lawrence, Yoon, Langer, & Ro, 2009), which is consistent with what victims of violence themselves report (Follingstad, Rutledge, Berg, Hause, & Polek, 1990).
A new line of work suggests the negative effects of IPC reverberate not only through the day but into the night, with recent work finding IPC impeded individual’s self-reported sleep quality (Rauer & El-Sheikh, 2012; Rauer, Kelly, Buckhalt, & El-Sheikh, 2010). Poor sleep has been associated with an increased risk of cardiovascular disease and mortality, in addition to exacerbating the negative effects of preexisting conditions, such as arthritis and cognitive impairment (Dew et al., 2003; Eguchi et al., 2008; Strine & Chapman, 2005). Given the well-documented costs of sleep problems for well-being and longevity, the finding that IPC leads to sleep problems may help explain why these same individuals are more vulnerable to serious health issues. However, to our knowledge, all existing studies of the effects of IPC on sleep have relied solely on subjective reports of sleep, which obscures a more nuanced view of how IPC is associated with objective sleep parameters, including quality and duration, which have unique antecedents and consequences for health (Friedman, 2011; Goldman et al., 2007). For example, sleep duration has been linked to a greater mortality risk (Patel et al., 2004), whereas sleep quality but not quantity has been linked to health complaints and mood disturbances (Pilcher, Ginter, & Sadowsky, 1997). Building on this scant literature, we examined relations between IPC and multiple actigraphy-based sleep parameters including duration and quality. Actigraphy provides a thorough objective assessment of sleep–wake patterns in naturalistic settings (Sadeh, Raviv, & Gruber, 2000) and is being used increasingly in studies that examine relations between sleep and health (Hanson & Chen, 2010). By understanding what aspects of sleep are most impeded by interpartner conflict and how, we can better identify how recipients of IPC may be at risk for later health problems.
Psychological Interpartner Conflict and Sleep
Findings on the effects of simply the presence of a partner on sleep have been mixed. Some studies reported that having a partner can be beneficial for sleep (e.g., Troxel et al., 2010), whereas others found that partners can be detrimental (Dittami et al., 2007), particularly if the cosleeping partner has different sleep–wake patterns (Larson, Crane, & Smith, 1991) or sleep apnea (McArdle, Kingshott, Engleman, Mackay, & Douglas, 2001). Where the small yet growing literature has been less equivocal is in the negative effects of having a bad relationship with that partner on an individual’s sleep. For example, unhappily married women reported greater sleep disturbances than their happily married counterparts (Troxel et al., 2009). Although these findings are important, the reliance on subjective reports of relationship satisfaction and sleep and the sole inclusion of women limits our ability to generalize findings, or, more important, to understand how specific relationship processes might affect sleep.
As to what relationship processes may underlie this link, interpersonal conflict may be particularly important for one’s ability to achieve a good night’s sleep. Looking at this broadly, Hasler and Troxel (2010) found women who reported the valence of their most recent interaction with their partner was of a negative nature had poorer actigraphy-based sleep efficiency. Focusing more on what might have contributed to the negative nature of a partner interaction but drawing from subjective reports of sleep, Hicks and Diamond (2011) found that greater quarreling during the daytime was linked to poorer sleep quality that night in a sample of 39 cohabiting men and women. A more persuasive story about the detrimental effects of interpartner conflict on sleep emerges from work on more severe forms of conflict, namely physical aggression. Studies have documented the high rate of sleep problems of women who have been the victims of interpartner physical violence (IPV), with some estimates of the incidence of sleep disturbances as high as 88% (Woods, Kozachik, & Hall, 2010). However, as many of these women were living in shelters at the time of assessment, this introduces a number of potential confounds as a shelter is not likely to have ideal sleeping conditions (crowded, noisy, uncomfortable beds). In community samples of women who have experienced IPV, it appears that although all forms of aggression (physical, sexual, psychological) are linked to greater sleep problems, psychological aggression is particularly detrimental to the quality of women’s sleep as assessed by subjective reports (Wijma, Samelius, Wingren, & Wijma, 2007). This finding is in line with previous work suggesting psychological aggression may be more damaging to individual’s well-being than physical violence in community samples (Lawrence et al., 2009).
One of the most critical limitations to this literature has been the nearly exclusive focus on women’s experiences of IPC and sleep, despite evidence that men are just as likely to be victims of IPC as women (Lawrence et al., 2009). To our knowledge, there have only been two published studies (both with the same sample) of the links between IPC and sleep in women and men; note that the present sample is independent from the one used in the Rauer et al., 2010 and the Rauer & El-Sheikh, 2012 studies. Rauer et al. (2010) found men and women who reported being the recipient of higher levels of IPC and increases in that conflict over time reported more sleep problems 2 years later. Rauer and El-Sheikh (2012) found women’s but not men’s perpetration of IPC was linked to an increase in their partners’ reports of sleep problems a year later. Although these studies are promising in linking IPC to the sleep of men and women, their reliance on subjective measures of sleep poses some limitations.
Objective sleep parameters have unique associations with relationship processes that are not captured by subjective assessments of sleep (Hasler & Troxel, 2010). Thus, in addition to having different associations between these sleep indices and overall health and well-being (Pilcher et al., 1997), the distinction between sleep quality versus quantity appears particularly pertinent when trying to understand how the social environment affects sleep (Galambos, Dalton, & Maggs, 2009). For example, Meadows, Arber, Venn, Hislop, and Stanley (2009) found that sleep latency and efficiency but not duration were clustered at the couple level, meaning that having a bed partner affected both how long individuals took to fall asleep and how often their sleep was disturbed, but not how long they actually slept. In light of these important distinctions, researchers have called for the integration of more objective measures of sleep in investigations linking the intimate relationship to sleep (Troxel, Robles, Hall, & Buysse, 2007). This study addresses this literature gap through using state-of-the-science objective measures of sleep quantity and quality to determine how more nuanced relationship processes, specifically IPC, affect multiple sleep parameters in men and women.
Mood Disturbances as the Mechanism? The Roles of Depression and Anxiety Symptoms in These Links
In their seminal review on the links between marriage and sleep, Troxel et al. (2007) stated that although the evidence does suggest intimate relationships affect sleep, it is through their influence on other systems. Perhaps the domain that has received the most attention is mental health whereby conflict-ridden hostile relationships are thought to contribute to impaired sleep by disturbing the individual’s mood. Marital conflict is a robust predictor of psychological distress, including depression and anxiety symptoms (Du Rocher Schudlich, Papp, & Cummings, 2004). Mood disturbances have, in turn, been strongly linked to sleep problems (Buysse & Kupfer, 1993; Fuller, Waters, Binks, & Anderson, 1997; Vahtera et al., 2007). Individuals who have greater anxiety and depression symptoms are not only more prone to sleep disturbances but may also be more sensitive to stress, which would engender greater sleep problems (Mezick et al., 2009). Given that IPC is a stressor, one would expect it to be linked with both mood disturbances and sleep problems.
Although there is substantial evidence linking IPC to mood disturbances and mood disturbances to sleep, there is surprisingly little research identifying mood disturbances as a mechanism through which IPC increases the risk of poor sleep. In a study of 121 women exposed to IPC, depressed women had more insomnia and nightmares than those without depression (Pigeon et al., 2011); depression was not examined as a mechanism of effects yet findings are supportive of this proposition. In the one study that reported such findings to our knowledge, depression and to a lesser extent anxiety symptoms mediated the link between initial levels and increases in IPC over time and later self-reported sleep problems for men and women (Rauer et al., 2010).
This Study
The primary aim was to examine relations between IPC and the sleep of couples. Sleep problems are indexed by reduced sleep duration and worse sleep quality on a continuum within the sample. Similarly, IPC was examined on a continuum. The use of objective measures of sleep derived through actigraphy and the assessment of multiple sleep domains including duration and quality add substantially to this young literature. Elucidating mechanisms of effects, depression and anxiety symptoms were examined as intervening variables or meditators of the link between IPC and sleep. To account for the linked nature of intimate partners’ interactions and sleep, as well as findings that individuals are more likely to aggress against their partners if they themselves are the victims of IPC (Leonard & Senchak, 1996), we examined partners simultaneously using the Actor-Partner Interdependence Model (APIM; Kashy & Kenney, 2000). We hypothesized that IPC perpetrated by both the person and his or her partner would be associated with reduced sleep duration and worse sleep quality. Depression and anxiety symptoms were expected to function as intervening variables or mediators in the association between IPC and sleep problems both within and across partners; although tentative, effects were expected to be more pronounced for actor versus partner pathways (e.g., one’s depression affecting one’s sleep more than partner’s sleep). In both a mediation and an intervening variable model, the predictor is related to the mediator or intervening variable, which in turn is associated with the outcome (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). Further, in a mediation model, the relation between the predictor and outcome is significant prior to the introduction of the mediator.
Method
Participants
Participants were 282 families with at least one school-aged child enlisted in a larger study examining biopsychosocial influences on children’s health (data collected during 2009–2010). Given the study’s focus, individuals without a cohabiting partner and couples with at least one night shiftworker or one with a diagnosed sleep disorder were excluded. The final analysis sample included 135 cohabiting couples (90% married) from a semirural community in the Southeastern United States; relationship duration M=12.03 years (SD=6.11). The mean age was 37 years (SD=5.93) for women and 39 (SD=7.33) for men. In relation to ethnicity, 76% of women and 78% of men were European American (EA), and 21% of women and 18.0% of men were African American (AA); the rest reported other ethnicities. Couples were from a wide range of socioeconomic backgrounds; the household income-to-needs ratio (family income/ the federal poverty threshold for that family size) had a M=2.56 and an SD=1.67.
Procedure
Families were recruited from letters sent home from schools with children, which explained that the study’s objective was to learn more about sleep and adaptation in families. Of families who contacted our lab in response to the letters, 90% participated. Couples completed questionnaires and wore actigraphs for one week to assess sleep. The University IRB approved the study, consent forms were completed, and individuals were compensated monetarily.
Interpartner conflict
Participants completed the eight-item Psychological/Verbal Aggression subscale of the Revised Conflict Tactics Scale (CTS2; Straus, 1995) in which they rated the frequency of acts used by their partner against them within the last year on a scale ranging from 0 (this has never happened) to 6 (more than 20 times in the past year). A sample item includes “my partner insulted or swore at me.” Items are summed to create a scale score. Research has suggested a bias in self-reports of partner aggression, whereby partners underreport their own perpetration (e.g., Ehrensaft & Vivian, 1996). Thus, ratings of the tactics used by the partner against the reporter were used in analyses. The range for psychological aggression toward women and men was 0 to 37 and 0 to 32, respectively; α = .79 for women and .76 for men. Further, physical aggression was assessed with the 12-item Physical Aggression subscale of the CTS2 (α = .95 for women and .92 for men) and given its co-occurrence with IPC (O’Leary et al., 1989) was controlled in analyses. The small percentages of couples endorsing physical aggression (8% and 12% against women and men, respectively) precluded its assessment as a primary variable.
Anxiety symptoms
Anxiety symptoms were assessed via the 21-item self-report Beck Anxiety Inventory (BAI; Beck & Steer, 1993). Participants rated the extent to which they were bothered by common symptoms of anxiety during the past month on a 4-point scale (not at all to severely). The BAI reliably discriminates symptoms of anxiety from depression in adults (Hewitt & Norton, 1993). In this study, α = .85 for both partners. Fifteen percent of women and 7% of men fell within the mild-to-moderate clinical range, and 4% of women fell within the moderate-to-severe range (scores from 0 to 9 = normal; 10 to 18 = mild to moderate; 19 to 29 = moderate to severe; 30 to 63 = severe).
Depression symptoms
Depression symptoms were assessed using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). Men and women rated the frequency of experiencing symptoms of depression during the past week on a 4-point scale (rarely to most or all of the time). The CES-D has well-established reliability and convergent validity with clinical and self-report measures of depression (Radloff, 1977) across ethnically and socioeconomically diverse samples (Canady, Stommel, & Holzman, 2009). In this sample, α = .89 for women and .84 for men. Eighteen percent of women and 4% of men surpassed the clinical cutoff score of 16, which indicates significant depression symptoms.
Sleep
Actigraphs were used to record sleep between bedtime and wake time; actigraphy-based sleep and wake times were cross-validated using daily sleep logs completed by men and women nightly. Actigraphy is considered a reliable tool for objectively indexing sleep in a naturalistic setting (Rupp & Balkin, 2011). Participants wore actigraph watches on the nondominant wrist to record nighttime activity for one week. The actigraphs were Octagonal Basic Motionloggers (Ambulatory Monitoring, Ardsley, NY) and measured motion in 1-min epochs using zero crossing mode. The analysis software package (AW2, 2002 Ambulatory Monitoring, Ardlesey, NY) used the established Cole-Kripke scoring algorithm (Cole, Kripke, Gruen, Mullaney, & Gillin, 1992) to derive sleep variables.
The assessment of multiple actigraphy-based parameters is endorsed to tap a wide range of sleep problems (Sadeh et al., 2000). To assess sleep amount, we derived Sleep Minutes, the number of minutes scored as sleep between sleep onset and wake time. Sleep onset time was determined by the first minute of three consecutive minutes scored as sleep and sleep wake time was considered the first minute of five consecutive minutes scored as being awake followed by a long period of movement. To examine sleep quality, we derived sleep efficiency, percentage of time between sleep onset and wake time scored as sleep, and sleep latency, amount of time between bedtime and sleep onset.
Women and men had an average of 5.84 nights (SD = 1.63) and 5.45 nights (SD = 1.91) of valid actigraphy data, respectively. Reasons for missing data included forgetting to wear the actigraph and mechanical problems. Intraclass correlations indicated good night-to-night stability over the week of assessment for both women and men: sleep minutes (α = .82 and .83), sleep efficiency (α = .92 and .93), and latency (α = .59 and .69); lower coefficients for latency are consistent with those reported in the literature (e.g., Knutson, Rathouz, Yan, Liu, & Lauderdale, 2007). To derive each sleep variable, data from all available nights were averaged.
Plan of Analysis
An APIM (Kashy & Kenney, 2000) was fit to examine whether symptoms of anxiety and depression served as process variables in the association between IPC and sleep problems (actigraphy measured sleep minutes, sleep efficiency, and sleep latency) among men and women. The APIM allows for an examination of both actor and partner effects (Kashy & Kenny, 2000). Here the actor effects capture the links between being the recipient of IPC and sleep, and the partner effects capture the links between being the perpetrator of IPC and sleep. The capability to simultaneously assess both actor and partner effects and to capture the interplay within dyads is a key strength of the APIM.
Analyses were conducted using Amos 17. Full information maximum likelihood (FIML) estimation was used to handle missing data (Acock, 2005). Depression and anxiety symptoms as well as all sleep parameters were included simultaneously in the same model. IPC against men and women were allowed to correlate and the residual variances among depression and anxiety symptoms were allowed to covary within and across partners. In addition, the residual variances among the sleep variables were allowed to correlate within and across partners.
Prior to examining indirect effects, we first examined the direct relations between IPC and sleep problems among men and women (i.e., anxiety and depression symptoms were excluded from the model). Next, men’s and women’s anxiety and depression symptoms were added to assess their roles as process variables. To evaluate potential indirect effects, we used Monte Carlo simulation (Preacher & Selig, 2012). This method produces confidence intervals of the hypothesized indirect effects by generating a large number of estimates (20,000 in this study) of an indirect effect by resampling from the distributions of each direct effect. Selig and Preacher’s (2008) interactive tool was used for creating confidence intervals to test indirect effects, with an indirect effect being demonstrated when the confidence intervals do not contain zero. Because analyses are based on cross-sectional data, reference to prediction pertains to statistical effects (MacKinnon et al., 2002). While examining one potential process variable, the pathways between the other potential process variables and the sleep outcome variable of interest were temporarily constrained to reduce potential for bias. In total, one dyadic path model was fit to the data (see Figure 1).
Figure 1.
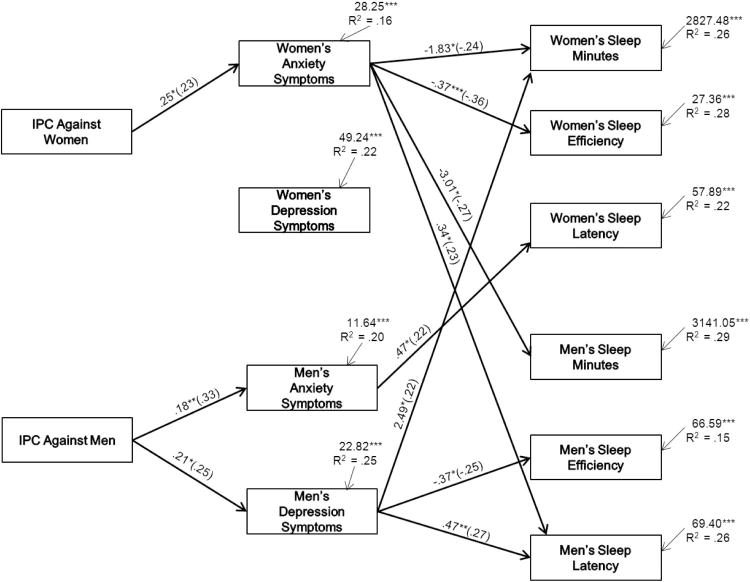
Dyadic path model used to examine anxiety and depression symptoms as process variables in the relation between interpartner psychological conflict (IPC) and sleep for romantic partners. Unstandardized and standardized coefficients (in parentheses) are provided. To improve the clarity of presentation, significant pathways are presented whereas non-significant pathways and correlations between variables and controls are not shown. IPC against women and men were allowed to covary. Residual variances among the depression, anxiety, and sleep variables were allowed to correlate within and across partners. Ethnicity, income-to needs ratio, age, medication use for chronic illness, sleep medication use, duration of cohabitation, and physical interpartner aggression directed toward men and women were controlled; control variables were allowed to correlate with exogenous variables and predict endogenous variables. Model fit: χ2(47) = 69, p < .05; χ2/df = 1.47; CFI = .97; RMSEA = .06 ns. †p < .10. * p < .05. ** p < .01. *** p < .001.
To reduce outlier effects, values ≥3 SDs were examined using histograms and values that fell beyond the tail end of the spectrum were set to missing (Cousineau, 2010; total n = 6). Men’s sleep onset latency was skewed and was log transformed. Variables associated with sleep and IPC in the literature were controlled: ethnicity, income-to-needs-ratio, age, duration of cohabitation, and physical aggression. Further, medication use for chronic conditions (38% of women and 28% of men including 13 women and 5 men who took antidepressants and 1 woman who took antianxiety medication) and for sleep (35% of women and 21% of men reported taking medication for sleep during the past month) were controlled.
Results
Preliminary Analyses
Descriptive statistics and correlations among study variables are presented in Table 1. Paired t tests indicated that, on average, women had greater symptoms of anxiety, t(104) = 5.46, p < .001, and depression, t(104) = 2.43, p < .05 than men; men and women did not differ on any sleep parameter. Average time in bed per night was 7.25 hr for women and 7 hr for men (i.e., minutes between bedtime and wake time). Further, women and men averaged 6.6 hr and 6.43 hr of actual sleep per night, respectively.
Table 1.
Correlations and Descriptive Statistics Among Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | M | SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Women’s ethnicity (1 = AA, 0 = EA) | — | — | — | |||||||||||||||||||||||
| 2. Men’s ethnicity (1 = AA, 0 = EA) | .81* | — | — | — | ||||||||||||||||||||||
| 3. Women’s age | −.22* | −.12 | — | 36.50 years | 5.93 | |||||||||||||||||||||
| 4. Men’s age | −.06 | −.08 | .61* | — | 39.37 years | 7.33 | ||||||||||||||||||||
| 5. Women’s medication use for chronic Illness | −.07 | .02 | .02 | .19* | — | — | — | |||||||||||||||||||
| 6. Men’s medication use for chronic illness | −.18* | −.17 | .04 | .07 | .09 | — | — | — | ||||||||||||||||||
| 7. Women’s sleep medication use | .08 | −.02 | .09 | .09 | .15 | .13 | — | — | — | |||||||||||||||||
| 8. Men’s sleep medication use | .08 | .03 | .03 | .23* | .09 | .42* | .13 | — | — | — | ||||||||||||||||
| 9. Income-to-needs ratio | −.09 | .01 | .31* | .07 | −.13 | −.11 | .07 | −.21 | — | 2.56 | 1.67 | |||||||||||||||
| 10. Duration of cohabitation | −.22* | −.12 | .50* | .36* | .04 | .15 | −.12 | .09 | .19 | — | 12.03 years | 6.11 | ||||||||||||||
| 11. Physical conflict toward women | −.10 | −.10 | .03 | −.08 | .29* | −.04 | −.02 | −.06 | .02 | .05 | — | 0.46 | 2.80 | |||||||||||||
| 12. Physical conflict toward men | −.06 | −.09 | −.03 | .07 | .40* | .08 | −.08 | .01 | −.18 | .00 | .75* | — | 0.81 | 3.92 | ||||||||||||
| 13. IPC toward women | −.26* | −.09 | .04 | −.05 | .13 | −.09 | .01 | −.08 | −.13 | .01 | .30* | .22* | — | 6.52 | 7.24 | |||||||||||
| 14. IPC toward men | −.23* | −.09 | −.05 | −.15 | .08 | −.06 | −.09 | −.13 | −.10 | .04 | .28* | .27* | .67* | — | 6.50 | 6.85 | ||||||||||
| 15. Women’s anxiety symptoms | −.20* | −.13 | .20* | .23* | .12 | −.11 | .10 | −.22* | −.03 | .05 | .00 | .00 | .32* | .27* | — | 6.00 | 5.96 | |||||||||
| 16. Men’s anxiety symptoms | −.05 | −.02 | .20* | .12 | .13 | −.01 | .05 | .05 | −.03 | .04 | .17 | .10 | .32* | .37* | .45* | — | 3.09 | 3.86 | ||||||||
| 17. Women’s depression symptoms | .03 | .17 | −.05 | .06 | .33* | −.08 | .06 | −.10 | −.09 | −.11 | .14 | .31* | .27* | .29* | .48* | .20* | — | 9.58 | 8.05 | |||||||
| 18. Men’s depression symptoms | .13 | .11 | −.10 | −.05 | .18 | −.07 | .12 | .08 | −.34* | −.12 | .13 | .11 | .25* | .30* | .15 | .36* | .18* | — | 7.37 | 5.53 | ||||||
| 19. Women’s sleep minutes | −.22* | −.12 | −.05 | −.13 | −.05 | .04 | .09 | −.15 | .27* | .09 | .01 | .02 | −.04 | .08 | −.07 | .02 | −.08 | .06 | — | 397 min | 62 min | |||||
| 20. Men’s sleep minutes | −.30* | −.21 | .23* | .16 | −.06 | −.02 | −.03 | −.14 | .14 | .11 | .03 | .02 | .01 | −.03 | −.08 | .09 | −.05 | −.19 | .26* | — | 384 min | 65 min | ||||
| 21. Women’s sleep efficiency % | −.15 | −.09 | −.04 | −.21* | −.12 | .05 | −.09 | −.18 | .31* | .18 | .09 | .04 | .08 | .12 | −.28* | −.08 | −.14 | −.05 | .54* | .27* | — | 93.49 | 6.34 | |||
| 22. Men’s sleep efficiency % | −.11 | −.08 | .07 | −.07 | −.13 | −.03 | −.02 | −.23* | .13 | −.01 | .07 | −.02 | −.07 | −.08 | −.11 | −.05 | −.10 | −.25 | .20* | .67* | .44* | — | 91.55 | 9.09 | ||
| 23. Women’s sleep onset latency (min) | .20* | .04 | −.07 | .04 | .21* | −.01 | .24* | .04 | −.22 | −.16 | .03 | .03 | .05 | −.02 | .19* | .22* | .07 | .11 | −.17 | −.18 | −.36* | −.25* | — | 11.68 | 8.70 | |
| 24. Men’s sleep onset latency (min) | .18 | .07 | −.17 | −.04 | −.03 | −.13 | −.01 | −.04 | −.20 | −.18 | −.01 | −.01 | .15 | .15 | .15 | .07 | .02 | .35* | −.10 | −.32* | −.18 | −.38* | .08 | — | 11.13 | 9.59 |
Note. Medication use for chronic illness and sleep medication use were dummy coded such that 1 = medication use and 0 = no medication use. IPC = Interpartner psychological conflict; AA = African American; EA = European American.
p < .05.
Dyadic Path Model
An APIM was fit to assess whether anxiety and depression symptoms served as process variables in the association between IPC and sleep. Control variables were allowed to correlate with exogenous variables and to predict endogenous variables. Prior to examining potential indirect effects, we assessed whether both received and perpetrated IPC were directly associated with men and women’s sleep, and no such effects were found. Next, anxiety and depression symptoms for women and men were entered in the model: model fit: χ2(47) = 69, p < .05; χ2/df = 1.47; CFI = .97; RMSEA = .06 ns; see Figure 1). For women, higher IPC was related to more symptoms of anxiety, which in turn was associated with fewer sleep minutes and reduced sleep efficiency. For men, being the recipient of greater IPC was related to having more symptoms of anxiety and depression. Further, increased levels of depression symptoms among men were related to reduced sleep efficiency and longer sleep onset latency.
Some partner effects were observed between mood disturbances and sleep (see Figure 1). Men had fewer sleep minutes and a longer sleep latency when their partners reported higher anxiety symptoms. Similarly, women had longer sleep latencies when their partners had more anxiety symptoms. Women also reported more sleep minutes when their partners reported greater symptoms of depression.
Tests of Indirect Effects
Next, the Monte Carlo simulation was used to explore possible indirect effects between IPC and sleep through mood disturbances. Given the lack of direct effects between IPC and any sleep parameter, significant indirect effects support intervening and not mediating pathways. For women, their anxiety symptoms served as an intervening variable in the relation between being the recipient of IPC and their sleep minutes (95% CI = −.18 to −.002) and sleep efficiency (95% CI = .−20 to −.003). Specifically, women exposed to higher levels of IPC had greater symptoms of anxiety, which were related to fewer sleep minutes and lower sleep efficiency. Further, for men, their depression symptoms served as a process variable linking IPC with their sleep efficiency (95% CI = −.19 to −.005) and sleep onset latency (95% CI = .01 to .25). Men who reported receiving more IPC experienced greater symptoms of depression, which in turn were related to reduced sleep efficiency and longer sleep onset latency.
Regarding the cross-partner effects, women who perpetrated more IPC (indicated by IPC against men in Figure 1) had partners who reported greater anxiety symptoms, which in turn was related to women having longer sleep onset latency (95% CI = .01–.20). On the other hand, looking at men’s depression symptoms as a process variable, women who perpetrated more IPC (IPC against men in Figure 1) had partners who reported more depression symptoms, which was, in turn, related to greater sleep minutes for women (95% CI = .01–.51). Finally, looking at the cross-partner effects of perpetration of IPC by men (IPC against women in Figure 1), women’s anxiety symptoms served as a process variable in the link between IPC against the partner and men’s sleep minutes (95% CI = −.39 to −.02) and sleep latency (95% CI = .002–.22). Men who perpetrated more IPC had partners who reported greater anxiety symptoms, which in turn was related to men having fewer sleep minutes and a longer sleep latency.
Further, we examined the magnitude of depression and anxiety effects on the various sleep parameters. For every one-point increase in women’s anxiety symptoms (range = 0–21), there was approximately (all numbers are rounded) a 2-min decrease in their sleep, a .50% decrease in their sleep efficiency, a 3-min decrease in men’s sleep duration, and a 1-min increase in men’s sleep latency. Further, for every one-point increase in men’s depression symptoms (range = 0–26), there was a .50% decrease in men’s sleep efficiency, a 1-min increase in men’s sleep latency, and a 3-min increase in women’s sleep duration. Finally, for every one-point increase in men’s anxiety symptoms (range = 0–15), there was about a 1-min increase in sleep latency among women.
Discussion
Building on a growing literature on the effects of relationship processes on sleep, relations between IPC and the sleep of couples were examined, and the intervening role of depression and anxiety symptoms in these associations was assessed. A dyadic model was used to examine research questions in which both actor and partner effects were evaluated. Findings contribute to the literature by illustrating that for women, anxiety symptoms were intervening pathways that were linking being the recipient of IPC with objectively derived sleep parameters, including shorter sleep duration and poorer sleep quality reflective of sleep fragmentation (low efficiency). Results were different for men and supported the role of depression symptoms as intervening variables in the association between exposure to IPC and sleep quality (poor efficiency and longer latency, which may reflect sleep onset insomnia). In addition, cross-partner effects were also evident. The general pattern of these effects illustrates that perpetration of IPC against the partner is associated with higher levels of internalizing symptoms for the partner, which in turn is related to poorer sleep for the perpetrator. Findings indicate that not all couples exposed to IPC are at equal risk for sleep problems. Rather, the individual’s and partner’s mental health are potential pathways of effects linking IPC and sleep problems. Results highlight the importance of contemporaneous assessments of intrapersonal and interpersonal factors in the prediction of sleep.
A number of recent studies have demonstrated that conflict plays a pivotal role in achieving adequate sleep among couples (Hicks & Diamond, 2011; Rauer & El-Sheikh, 2012; Troxel et al., 2007). Building on studies that have established direct associations, researchers have begun to investigate mechanisms of effects that may explain why interpartner conflict is related to disruptions in sleep. For instance, using self-reports of sleep problems and with an independent sample than that used in the present study, Rauer et al. (2010) found that higher levels of IPC among cohabiting and married couples were related to greater symptoms of depression and anxiety, which in turn were related to more sleep problems in men and women. This study extends this literature by demonstrating the intervening role of depression and anxiety symptoms in the relation between IPC and objectively measured sleep duration and quality. In addition, although analyses were conducted separately for men and women in the Rauer et al. (2010) study, this investigation used dyadic path analyses to account for the linked nature of intimate partners’ interactions and sleep. This statistical approach provides conservative model estimates, lends confidence in the findings, and allows for the assessment of how familial stressors uniquely influence men and women.
It is not clear why direct relations were not observed between IPC and sleep. This is the first study to examine these associations with actigraphy precluding comparison with similar investigations. In Rauer et al. (2010), men and women who were the recipients of higher IPC had more self-reported sleep problems 2 years later. Rauer and El-Sheikh (2012) found women’s perpetration of IPC was linked to an increase in their partners’ reports of sleep problems a year later, but men’s reports of perpetrating IPC were not linked to their partner’s later sleep problems. Sleep assessment methodologies and sample features may underlie the discrepant results. Associations between subjective and objective sleep parameters are frequently not observed (Sadeh, 2011), highlighting the importance of a multimethod approach.
Plausible explanations exist as to why anxiety and depression symptoms may intervene in the relations between the receipt of IPC and the quantity and quality of one’s sleep. The elevated levels of anxiety and depression symptoms that have been well-established outcomes of IPC (e.g., Haj-Yahia, 1999; Pico-Alfonso et al., 2006; Ratner, 1993; Sackett & Saunders, 1999) are often accompanied by increased vigilance, which is an antithesis of sleep (Dahl, 1996). Indeed, symptoms of depression, such as change in affect, ruminating thought processes, and increased emotional distress (Nolen-Hoeksema, 2000) may interfere with the relaxation needed to attain sleep (Dahl, 1996). Similarly, feelings of fear, worry, and alertness, the hallmarks of anxiety, may prevent individuals from being able to reduce arousal in order to sleep (Dahl, 1996). Further, from a biopsychosocial perspective, individuals who exhibit internalizing symptoms frequently have elevated cortisol levels (Pariante & Lightman, 2008), which is a risk factor for sleep problems (Vgontzas et al., 2003).
Although anxiety symptoms were intervening variables linking IPC and sleep minutes and efficiency for women, these findings were not observed for men. Conversely, depression symptoms served as a mechanism of effects in the association between IPC and sleep quality for men. It is plausible that differences in levels of anxiety and depression symptoms between men and women may account for some of the observed gender-related effects. For example, although IPC was related to higher levels of anxiety for both men and women, women reported higher levels of anxiety than men. The higher levels of anxiety among women may have surpassed the “tipping point” for sleep problems, whereas the lower levels of anxiety may have put men at less risk for sleep disruptions. For gender-related differences pertaining to the intervening role of depression symptoms, studies using polysomnography have demonstrated that symptoms of depression are linked to greater slow-wave sleep (i.e., increased delta wave counts or deep sleep) for women (Armitage & Hoffman, 2001). In contrast, men who exhibit depression symptoms show less slow wave sleep and extended wakefulness. Taken together, both men and women who have symptoms of depression show evidence of slow-wave sleep abnormalities but it is hyperresponsivity in women and hyporesponsivity in men (Armitage & Hoffmann, 2001; Reynolds et al., 1990). The women in our study who experienced depression symptoms may have experienced greater slow-wave sleep resulting in the actigraph detecting little night time movement. Obviously, these potential explanations about mechanisms of effects and gender-related differences are tentative until explored empirically. To explicate our findings, in additional analyses not reported here, we ran all the models separately for anxiety and depression symptoms, and the pattern of effects was almost identical to models that included both internalizing domains. Thus, entering anxiety and depression in the same model is not a potential explanation for the observed effects. Continued clarification of how interpartner conflict and internalizing symptoms differently influence the quantity and quality of sleep among men and women is warranted.
Women’s perpetration of IPC was associated with increased anxiety symptoms in men, which in turn were related to longer sleep latency for women. Cross-partner effects found for men’s sleep illustrate that perpetration of IPC by men is related to increased anxiety in women, which in turn is associated with longer sleep latency for men (and reduced sleep duration). Although tentative, men’s and women’s anxiety symptoms are likely to be outwardly expressed at least in part and to be apparent to the partner. This may lead to guilt, reflection, rumination about one’s aggressive behavior, which in turn leads to a longer sleep latency that is potentially indicative of sleep onset insomnia and associated with shorter sleep. One unexpected finding pertained to men’s depression being associated with longer sleep duration in women; interpretation would be too speculative and, thus, is not undertaken.
Findings from our study have important implications. The average amount of time spent in bed (7.25 hr for women and 7 hr for men) was on the lower end of the National Sleep Foundation’s (2011) recommendation of 7–9 hr allotted for sleep per night, and many participants were far below recommendations. Sufficient and adequate quality sleep is critical for physical and psychological health, and there is a continued need for researchers and health professionals to identify the sources of inadequate sleep. Findings demonstrate that IPC was directly related to depression and anxiety symptoms and indirectly related to sleep problems. Prevention efforts aimed at altering interpartner conflict tactics hold particular promise for minimizing health-related risks, including the reduction of sleep problems. Of course, intervention efforts should consider the clinical significance of the findings. For example, for every one-point increase in women’s anxiety symptoms, there was a 2-min decrease in their sleep duration and a .50% decrease in their sleep efficiency. Further, for every one-point increase in men’s depression symptoms, there was a .50% decrease in their sleep efficiency and a 1-min increase in their sleep latency.
Study limitations need to be considered. The cross-sectional nature of the study precludes inferences about causation. For example, although relationship conflict and aggression could impact sleep, the opposite direction of effects is also possible (Troxel et al., 2007). Similarly, sleep problems can influence one’s affect regulation and mood (Dinges, Rogers, & Baynard, 2005), which in turn could be a pathway of effects in the sleep–IPC link. Longitudinal studies are key for clarifying directionality of effects and the transactional nature of relations among model variables. Although a wide range of IPC was observed in this sample, and is similar to that reported in other community samples (El-Sheikh, Cummings, Kouros, Elmore-Staton, & Buckhalt, 2008) results may not translate to couples with more extreme aggression. Similarly, findings pertaining to anxiety and depression symptoms may not be generalizable to clinical samples. Further, although examining depression and anxiety symptoms as pathways of effects constitutes an advance in this young literature, there are many other plausible mechanisms of effects (e.g., chaotic home environment). Similarly, it is likely that several variables could function as moderators of the association between IPC and sleep including ethnicity, socioeconomic status, and period of cohabitation, and such investigations are warranted. It is unfortunate that our small sample size in the context of a complex model precluded assessment of such effects. In addition, actigraphy was examined during 1 week while reports of IPC pertained to 1 year. Even though both sleep and IPC are likely moderately stable, it is possible that more fine-grained analyses of daily conflict in relation to daily sleep could explicate relations further.
Acknowledgments
This research was supported by Grant Number R01-HL093246 from the National Heart, Lung, and Blood Institute awarded to Mona El-Sheikh. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. We thank our participants and the lab staff most notably Bridget Wingo and Lori Elmore-Staton for data collection and preparation.
References
- Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67:1012–1028. doi: 10.1111/j.1741-3737.2005.00191.x. [DOI] [Google Scholar]
- Armitage R, Hoffmann RF. Sleep EEG, depression and gender. Sleep Medicine Reviews. 2001;5:237–246. doi: 10.1053/smrv.2000.0144. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory manual. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Buysse DJ, Kupfer DJ. Sleep disorders in depressive disorders. In: Mann JJ, Kupfer DJ, editors. Biology of depressive disorders Part A: A systems perspective. New York, NY: Plenum Press; 1993. pp. 123–154. [Google Scholar]
- Canady RB, Stommel M, Holzman C. Measurement properties of the Centers for Epidemiological Studies Depression Scale (CES-D) in a sample of African-American and non-Hispanic White pregnant women. Journal of Nursing Measurement. 2009;17:91–104. doi: 10.1891/1061-3749.17.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Smith PH. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;23:260–268. doi: 10.1016/S0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification form wrist activity. Sleep. 1992;15:461–469. doi: 10.1093/sleep/15.5.461. [DOI] [PubMed] [Google Scholar]
- Cousineau D. Outliers detection and treatment: A review. International Journal of Psychological Research. 2010;3:58–67. [Google Scholar]
- Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology. 1996;8:3–27. doi: 10.1017/S0954579400006945. [DOI] [Google Scholar]
- Dew MA, Hoch CC, Buysse DJ, Monk TH, Begley AE, Houck PR, Reynolds CF. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosomatic Medicine. 2003;65:63–73. doi: 10.1097/01.PSY.0000039756.23250.7C. [DOI] [PubMed] [Google Scholar]
- Dinges DF, Rogers NL, Baynard MD. Chronic sleep deprivation. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 4. Philadelphia, PA: W. B. Saunders; 2005. p. 67. [Google Scholar]
- Dittami J, Keckeis M, Machatschke I, Katina S, Zeitlhofer J, Kloesch G. Sex differences in the reactions to sleeping in pairs versus sleeping alone in humans. Sleep and Biological Rhythms. 2007;5:271–276. doi: 10.1111/j.1479-8425.2007.00320.x. [DOI] [Google Scholar]
- Du Rocher Schudlich TD, Papp LM, Cummings EM. Relations of husbands’ and wives’ dysphoria to marital conflict resolution strategies. Journal of Family Psychology. 2004;18:171–183. doi: 10.1037/0893-3200.18.1.171. [DOI] [PubMed] [Google Scholar]
- Eguchi K, Pickering TG, Schwartz JE, Hoshide S, Ishikawa J, Ishikawa S, Kario K. Short sleep duration as an independent predictor of cardiovascular events in Japanese patients with hypertension. Archives of Internal Medicine. 2008;168:2225–2231. doi: 10.1001/archinte.168.20.2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrensaft MK, Vivian D. Spouses’ reasons for not reporting existing marital aggression as a marital problem. Journal of Family Psychology. 1996;10:443–453. doi: 10.1037/0893-3200.10.4.443. [DOI] [Google Scholar]
- El-Sheikh M, Cummings EM, Kouros CD, Elmore-Staton L, Buckhalt J. Marital psychological and physical aggression and children’s mental and physical health: Direct, mediated, and moderated effects. Journal of Consulting and Clinical Psychology. 2008;76:138–148. doi: 10.1037/0022-006X.76.1.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Follingstad DR, Rutledge LL, Berg BJ, Hause ES, Polek DS. The role of emotional abuse in physically abusive relationships. Journal of Family Violence. 1990;5:107–120. doi: 10.1007/BF00978514. [DOI] [Google Scholar]
- Friedman EM. Sleep quality, social well-being, gender, and inflammation: An integrative analysis in a national sample. Annals of the New York Academy of Sciences. 2011;1231:23–34. doi: 10.1111/j.1749-6632.2011.06040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller KH, Waters WF, Binks PG, Anderson T. Generalized anxiety and sleep architecture: A polysomnographic investigation. Sleep. 1997;20:370–376. doi: 10.1093/sleep/20.5.370. [DOI] [PubMed] [Google Scholar]
- Galambos NL, Dalton AL, Maggs JL. Losing sleep over it: Daily variation in sleep quantity and quality in Canadian students’ first semester of university. Journal of Research on Adolescence. 2009;19:741–761. doi: 10.1111/j.1532-7795.2009.00618.x. [DOI] [Google Scholar]
- Goldman SE, Stone KL, Ancoli-Israel S, Blackwell T, Ewing SK, Newman AB. Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep. 2007;30:1317–1324. doi: 10.1093/sleep/30.10.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haj-Yahia MM. Wife abuse and its psychological consequences as revealed by the first Palestinian National Survey on Violence Against Women. Journal of Family Psychology. 1999;13:642–662. doi: 10.1037/0893-3200.13.4.642. [DOI] [Google Scholar]
- Hanson MD, Chen E. Daily stress, cortisol, and sleep: The moderating role of childhood psychosocial environments. Health Psychology. 2010;29:394–402. doi: 10.1037/a0019879. [DOI] [PubMed] [Google Scholar]
- Hasler BP, Troxel WM. Couples’ nighttime sleep efficiency and concordance: Evidence for bidirectional associations with daytime relationship functioning. Psychosomatic Medicine. 2010;72:794–801. doi: 10.1097/PSY.0b013e3181ecd08a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewitt PL, Norton GR. The Beck Anxiety Inventory: A psychometric analysis. Psychological Assessment. 1993;5:408–412. doi: 10.1037/1040-3590.5.4.408. [DOI] [Google Scholar]
- Hicks AM, Diamond LM. Don’t go to bed angry: Attachment, conflict, and affective and physiological reactivity. Personal Relationships. 2011;18:266–284. doi: 10.1111/j.1475-6811.2011.01355.x. [DOI] [Google Scholar]
- Kashy DA, Kenny DA. The analysis of data from dyads and groups. In: Reis HT, Judd CM, editors. Handbook of research methods in social psychology. New York, NY: Cambridge University Press; 2000. pp. 451–477. [Google Scholar]
- Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Intra-individual daily and yearly variability in actigraphically recorded sleep measures: The CARDIA study. Sleep. 2007;30:793–796. doi: 10.1093/sleep/30.6.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson JH, Crane DR, Smith CW. Morning and night couples: The effect of wake and sleep patterns on marital adjustment. Journal of Marital and Family Therapy. 1991;17:53–65. doi: 10.1111/j.1752-0606.1991.tb00864.x. [DOI] [Google Scholar]
- Lawrence E, Yoon J, Langer A, Ro E. Is psychological aggression as detrimental as physical aggression? The independent effects of psychological aggression on depression and anxiety symptoms. Violence and Victims. 2009;24:20–35. doi: 10.1891/0886-6708.24.1.20. [DOI] [PubMed] [Google Scholar]
- Leonard KE, Senchak M. Prospective prediction of husband marital aggression within newlywed couples. Journal of Abnormal Psychology. 1996;105:369–380. doi: 10.1037/0021-843X.105.3.369. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle N, Kingshott R, Engleman HM, Mackay TW, Douglas NJ. Partners of patients with sleep apnoea/hypopnoea syndrome: Effect of CPAP treatment on sleep quality and quality of life. Thorax. 2001;56:513–518. doi: 10.1136/thorax.56.7.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meadows R, Arber S, Venn S, Hislop J, Stanley N. Exploring the interdependence of couples’ rest-wake cycles: An actigraphic study. Chronobiology International. 2009;26:80–92. doi: 10.1080/07420520802678452. [DOI] [PubMed] [Google Scholar]
- Mezick EJ, Matthews KA, Hall M, Kamarck TW, Buysse DJ, Owens JF, Reis SE. Intra-individual variability in sleep duration and fragmentation: Associations with stress. Psychoneuroendocrinology. 2009;34:1346–1354. doi: 10.1016/j.psyneuen.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy CM, Cascardi M. Psychological abuse in marriage and dating relationships. In: Hampton RL, editor. Family violence: Prevention and treatment. 2. Thousand Oaks, CA: Sage; 1999. pp. 197–226. [Google Scholar]
- National Sleep Foundation. How much sleep do we really need? 2011 Retrieved from http://www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need.
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109:504–511. doi: 10.1037/0021-843X.109.3.504. [DOI] [PubMed] [Google Scholar]
- O’Leary KD, Barling J, Arias I, Rosenbaum A, Malone J, Tyree A. Prevalence and stability of physical aggression between spouses: A longitudinal analysis. Journal of Consulting and Clinical Psychology. 1989;57:263–268. doi: 10.1037/0022-006X.57.2.263. [DOI] [PubMed] [Google Scholar]
- Pariante CM, Lightman SL. The HPA axis in major depression: Classical theories and new developments. Trends in Neurosciences. 2008;31:464–468. doi: 10.1016/j.tins.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Hu FB. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- Pico-Alfonso MA, Mastorci F, Ceresini G, Ceda GP, Manghi M, Pino O, Sgoifo A. Acute psychosocial challenge and cardiac autonomic response in women: The role of estrogens, corticosteroids, and behavioral coping styles. Psychoneuroendocrinology. 2007;32:451–463. doi: 10.1016/j.psyneuen.2007.02.009. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Cerulli C, Richards H, He H, Perlis M, Caine E. Sleep disturbances and their association with mental health among women exposed to intimate partner violence. Journal of Women’s Health. 2011;20:1923–1929. doi: 10.1089/jwh.2011.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: Relationships between sleep and measures of health, well-being and sleepiness in college students. Journal of Psychosomatic Research. 1997;42:583–596. doi: 10.1016/S0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Selig JP. Advantages of monte carlo confidence intervals for indirect effects. Communication Methods and Measures. 2012;6:77–98. doi: 10.1080/19312458.2012.679848. [DOI] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ratner PA. The incidence of wife abuse and mental health status in abused wives in Edmonton, Alberta. Canadian Journal of Public Health Revue canadienne de santé publique. 1993;84:246–249. [PubMed] [Google Scholar]
- Rauer AJ, El-Sheikh M. Reciprocal pathways between intimate partner violence and sleep in men and women. Journal of Family Psychology. 2012;26:470–477. doi: 10.1037/a0027828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauer AJ, Kelly RJ, Buckhalt JA, El-Sheikh M. Sleeping with one eye open: Marital abuse as an antecedent of poor sleep. Journal of Family Psychology. 2010;24:667–677. doi: 10.1037/a0021354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CF, III, Kupfer DJ, Thase ME, Frank E, Jarrett DB, Coble PA, Houck PR. Sleep, gender, and depression: An analysis of gender effects on the electroencephalographic sleep of 302 depressed outpatients. Biological Psychiatry. 1990;28:673–684. doi: 10.1016/0006-3223(90)90454-A. [DOI] [PubMed] [Google Scholar]
- Rupp TL, Balkin T. Comparison of Motionlogger Watch and Actiwatch actigraphs to polysomnography for sleep/wake estimation in healthy young adults. Behavior Research Methods. 2011;43:1152–1160. doi: 10.3758/s13428-011-0098-4. [DOI] [PubMed] [Google Scholar]
- Sackett LA, Saunders DG. The impact of different forms of psychological abuse on battered women. Violence and Victims. 1999;14:105–117. [PubMed] [Google Scholar]
- Sadeh A. Sleep assessment methods. In: El-Sheikh M, editor. Sleep and development: Familial and socio-cultural considerations. New York, NY: Oxford University Press; 2011. pp. 355–371. [Google Scholar]
- Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Developmental Psychology. 2000;36:291–301. doi: 10.1037/0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- Schumacher JA, Slep AMS, Heyman RE. Risk factors for male-to-female partner psychological abuse. Aggression and Violent Behavior. 2001;6:255–268. doi: 10.1016/S1359-1789(00)00025-2. [DOI] [Google Scholar]
- Selig JP, Preacher KJ. Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects [Computer software] 2008 Available from http://quantpsy.org/
- Straus MA. Manual for the Conflict Tactics Scale. Durham, NH: Family Research Laboratory, University of New Hampshire; 1995. [Google Scholar]
- Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Medicine. 2005;6:23–27. doi: 10.1016/j.sleep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Buysse DJ, Matthews KA, Kravitz HM, Bromberger JT, Sowers M, Hall MH. Marital/cohabitation status and history in relation to sleep in midlife women. Sleep. 2010;33:973–981. doi: 10.1093/sleep/33.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews. 2007;11:389–404. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahtera J, Kivimaki M, Hublin C, Korkeila K, Suominen S, Paunio T, Koskenvuo M. Liability to anxiety and severe life events as predictors of new-onset sleep disturbances. Sleep. 2007;30:1537–1546. doi: 10.1093/sleep/30.11.1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vgontzas AN, Zoumakis M, Bixler EO, Lin H-M, Prolo P, Vela-Bueno A, Chrousos GP. Impaired nighttime sleep in healthy old versus young adults is associated with elevated plasma Interleukin-6 and Cortisol levels: Physiologic and therapeutic implications. Journal of Clinical Endocrinology & Metabolism: Clinical and Experimental. 2003;88:2087–2095. doi: 10.1210/jc.2002-021176. [DOI] [PubMed] [Google Scholar]
- Wijma K, Samelius L, Wingren G, Wijma B. The association between ill-health and abuse: A cross-sectional population based study. Scandinavian Journal of Psychology. 2007;48:567–575. doi: 10.1111/j.1467-9450.2007.00553.x. [DOI] [PubMed] [Google Scholar]
- Woods SJ, Kozachik SL, Hall RJ. Subjective sleep quality in women experiencing intimate partner violence: Contributions of situational, psychological, and physiological factors. Journal of Traumatic Stress. 2010;23:141–150. doi: 10.1002/jts.20495. [DOI] [PubMed] [Google Scholar]


